Abstract
The fetal liver is the main hematopoietic organ during intrauterine life. Morphometrical studies were performed on liver sections to detect changes occurring with intrauterine growth retardation and preeclampsia. Compared with the controls (n = 10), fetuses from preeclamptic mothers showed a severe reduction of erythroid cells by 60% on average (n = 18). Closer examination revealed that the erythroid cells at early stages of differentiation were more affected (80% reduction) than at later stages (55%). Seven out of 18 fetuses from preeclamptic mothers did not show growth retardation but exhibited severely reduced hepatic erythropoiesis. We suggest that the prime factor for impaired red blood cell production is preeclampsia itself rather than intrauterine growth retardation. Regulation of erythropoiesis in utero might depend on the interaction of many hematopoietic growth factors, and preeclampsia might alter the balance. To test this notion, we quantitated erythropoietin in fetal blood and various cytokines in the amniotic fluid. An elevation of erythropoietin and interleukin (IL)-3 levels was seen in babies born under the conditions of preeclampsia, whereas the concentrations of granulocyte/macrophage-colony-stimulating factor (CSF), granulocyte-CSF, and IL-1β were reduced, and the levels of IL-6 and IL-8 remained constant. With preeclampsia, a discrepancy between elevation of erythrocyte numbers in peripheral blood and depression of hematopoiesis at the main production site, the fetal liver, is seen. Concomitantly, there is elevation of some but reduction of other hematopoietic cytokines. We envision that during the course of preeclampsia quantitation of hematopoietic growth factors might allow to predict the deterioration of in utero life conditions.
Similar content being viewed by others
Main
Sudden and severe pathologic changes during pregnancy might result in fetal lethality. If changes occur more slowly, however, the fetus can suffer for a prolonged time and eventually die from starvation. Knowledge of the pathophysiologic mechanisms within the fetal organs might be useful to increase the chances of postpartum survival of the fetus. Furthermore, the pattern of morphologic changes in fetal tissues might give diagnostic hints to the cause of disturbances during pregnancy. On postmortem examination, fetal organs often do not show striking pathomorphologic features. The perception of mild changes in tissue morphology is further complicated by the fact that the increasing fetal age has a strong impact on tissue architecture, which is more pronounced in some organs such as brain, lungs, kidney, and skin, but less in others. However, there are organs such as lymphatic and hematopoietic tissue where reactive changes are readily displayed and which thus might mirror the quality of intrauterine life. During development, the fetal liver is the predominant site of hematopoiesis(1–3). In contrast to some animal species, the role of the spleen during fetal hematopoiesis is not significant in humans(4).
In the course of previous studies focused on elevated fetal granulopoiesis occurring with amniotic infection(5) we noted the reduction of erythropoiesis within the hepatic sinusoids in fetuses who had died as a consequence of a pregnancy disorder called preeclampsia. Typically, preeclamptic mothers suffer from hypertension, proteinuria, and edema. Their placentas are often small and exhibit signs of circulatory disturbance. Furthermore, the maternal vessels located at the implantation site of the placenta are often narrow and affected by “acute atherosis”(6). Etiologically, preeclampsia is often considered within the broad category of immunologic diseases(7). We previously reported that reduced levels of cytokines in fetal blood and amniotic fluid are characteristic for preeclampsia(8). In this report, we describe the hematopoietic alterations occurring in the fetal liver of affected fetuses and suggest that these alterations might be a consequence of preeclampsia rather than growth retardation.
METHODS
The experimental protocol was approved by the university ethical committee. In a first step, a total of 28 human fetuses of 23-34-wk gestational age were examined. In eight of them, pregnancy was terminated rather late because of a neural tube defect. The advanced fetal age, however, correlated well with the age of the fetuses from preeclamptic mothers (see below). In one case, advanced pregnancy ended due to severe maternal trauma in a car accident, and in another case, the fetus was delivered spontaneously after appendectomy of the mother (Table 1, nos. 1-10). The mean gestational age in this group, which was considered as the control (n = 10), was 26 wk (23-31 wk). “Normal appearing” fetuses with chromosomal anomalies were not included in the control group as it is known that,e.g. trisomy 21 exhibits anomalies during the development of lymphatic and hematopoietic tissues. In the remaining 18 cases (nos. 11-28), the respective mothers suffered from preeclampsia with maternal blood pressures higher than 140/90 mm Hg and proteinuria of over 0.3 g/d. Preeclampsia resulted either in intrauterine death (eight cases) or in a cesarean section followed by postpartum death within 24 h due to immaturity(10 cases). Intrauterine growth retardation had occurred in 11 fetuses (nos. 11-21). However, seven fetuses were not considered as growth-retarded, because total body weight as well as the weight of heart and kidney were appropriate for the corresponding gestational age (Table 1, nos. 22-28). Mean gestational age in the preeclamptic group was 28 wk (24-34 wk). In all cases, autopsy was performed within 36 h after death. Weights from the fetus and its organs were recorded and displayed as percentiles with respect to the corresponding fetal age (Table 1). A fetus was considered as growth-retarded if age-related body weights were below the 5th percentile. Normal weights were derived from a 10-y survey of our files comprising more than 3000 fetal and neonatal autopsies (T. Stallmach, unpublished data); percentiles had been established using a recently published method with standardized residuals(9).
Histology. Tissues were fixed in formalin and later embedded in paraffin. Sections of the liver measuring 2 μm in thickness were stained using the naphthol-ASD-chloroacetate esterase reaction(10). This histochemical procedure marks brightly red neutrophilic granulopoietic cells, ranging from the promyelocyte stage to mature segmented granulocytes. The hematoxylin counterstain differentiates nuclear chromatin. Granulopoietic cells whose nuclei were indented and darkly stained, having about the appearance of metamyelocytes, were arbitrarily considered as “late stage,” together with the even more advanced stages of this lineage. Large cells with positive histochemical reactions and with large round nuclei were registered as “early stage” of granulopoiesis. More importantly, erythroid precursor cells were arbitrarily considered as late stage of differentiation, if nuclei were homogeneously darkly stained and small, having about the appearance of normoblasts. Large cells with negative histochemical reaction and with large round nuclei were registered as in the early stage of erythropoiesis. Immunohistochemical detection of the B and T cell markers CD20 and CD3, respectively, revealed that lymphocytes are very scarce within the liver of the investigated fetuses(not shown). This is in agreement with a previous report(11). Lymphocytes are thus quantitatively irrelevant and do not interfere with the quantitation of erythroid cells in the fetal liver.
Morphometry And Statistics. The average number of hematopoietic cells per mm2 from each fetal liver was determined by counting five different areas (1 mm2) of the liver's right lobe, strictly outside portal fields. Densities of hematopoietic cells within liver parenchyma were established by computer-assisted morphometry on a Zeiss microscopic system(Axiohome). Results are given as the mean of hematopoietic elements per area with standard deviations; results of individual cases are shown in Table 1. The level of significance of the obtained differences was determined by the use of the nonparametric Wilcoxon test.
Enzyme immunoassays for Epo and cytokines. In a second group of fetuses, which were all born via cesarean section, venous blood from the umbilical cord and amniotic fluid were examined. The 12 control fetuses were of adequate growth and derived from uncomplicated pregnancies (mean gestational age 36 wk), whereas 13 fetuses were growth-retarded and born under the conditions of preeclampsia (mean gestational age, 35 wk). Amniotic fluid was collected during the first minutes of surgery, and venous blood was taken from the umbilical cord. The fluids were centrifuged (4000 × g for 10 min) and the supernatants were stored at -70 °C. Epo concentration in fetal cord blood was determined using a RIA as described previously(12). Cytokines in the amniotic fluid were quantified by the use of commercially available enzyme immunoassay kits (Quantikine human G-CSF, Quantikine GM-CSF, Quantikine IL-1β, IL-2, IL-3, IL-6, and IL-8; R+D Systems, Minneapolis, MN). The results are given as means with the ranges. Significance of differences was established with the help of the nonparametric Mann-Whitney test.
RESULTS
In a first set of experiments, we analyzed alteration of hepatic hematopoiesis in fetuses born from preeclamptic mothers (n = 18) compared with similar aged controls (n = 10), the latter being mainly derived from late pregnancy terminations due to malformation of the fetal vertebral column (see Table 1 and“Methods”). With the mother suffering from preeclampsia, the number of erythroid cells within the liver parenchyma of the corresponding fetus was strongly reduced irrespective of whether the fetus was growth-retarded or not as exemplified in Figure 1. Histologic comparison of fetal liver sections from the control group (Fig. 1a) with the group suffering from the condition of maternal preeclampsia (Fig. 1c) revealed that in the latter erythropoiesis was reduced to small islands with most of the sinusoids cleared of nucleated cells. Morphometrical analysis showed that the total number of erythroid cells (combined “early” and“late”) in the affected liver parenchyma was 1346 ± 678 cells per mm2 (n = 18). Compared with the fetuses of the control group containing 3416 ± 480 cells per mm2 (n = 10), this represents a reduction of erythropoietic cells by about 60%(p < 0.001). To exclude that changes in density of the hematopoietic cells simply reflect alterations in the organ architecture such as hepatic edema, we determined the number of hepatocytes per mm2 and compared it with the total number of erythroid cells. We observed that the number of hepatocytes within the same area was about equal, being 1138± 206 cells per mm2 in the control group and 1081 ± 339 per mm2 in fetuses from preeclamptic mothers, thus excluding major alterations in hepatic architecture.
Histologic analysis of extramedullary hematopoiesis within fetal liver: in liver sections of healthy fetuses, the dark staining nuclei of hematopoietic elements outnumber the pale staining nuclei of the hepatocytes (a); the nuclei of the erythroid blasts(arrows) have about the same size as hepatocyte nuclei(b). With preeclampsia, hematopoietic activity is reduced to isolated islands (c); erythroid blasts show cell death reminiscent of apoptosis (arrows) (d). Hematoxylin-eosin staining, enlarged ×175 (a and c) and ×500 (b and d).
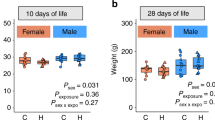
Closer histologic examination of the erythropoietic cells within the fetal liver revealed that the number of cells at early and late stages of differentiation (see “Methods”) was reduced by 80 and 50%, respectively, in fetuses from preeclamptic mothers (Fig. 2). In contrast to the control sections (Fig. 1b), the remaining hematopoietic islands contained about 30-50% of cells with clumped and fragmented chromatin (Fig. 1d). This was true not only for the late erythroid stages which are programmed to break down and expel their nuclei, but also for the early erythroid stages. Most probably these morphologic changes represent apoptosis of erythroid cells. With regard to granulopoiesis, the total number of granulopoietic cells (19.7 ± 15.3 per mm2 of liver parenchyma, outside portal tracts) was not altered. However, histologic quantitation revealed an up to 50% decrease of the early granulopoietic cells with preeclampsia (p < 0.01). Obviously, this reduction was made up by an increase in the number of more mature granulocytic cells.
Changes in numbers of erythroid precursor cells per mm2 of fetal liver tissue: with preeclampsia, erythropoiesis exhibits a highly significant (p < 0.001) reduction of both late and early cells. Boxes show median and contain 50% of all measurements, lines above and below represent 10th and 90th percentile, respectively.
What is the cause of reduced liver erythropoiesis in the growing fetus? Because growth retardation is known to occur in fetuses born from preeclamptic mothers, one might envision that reduced liver development (and thus reduced hepatic erythropoiesis) is a consequence of a general growth disturbance affecting the fetus as a whole. Indeed, 11 out of 18 affected fetuses were severely growth-retarded and the weight of the fetus and the corresponding placenta were both below the 5th percentile (Table 1, nos. 11-21). The corresponding placentas showed increased amounts of perivillous fibrin, and often more than 10% of the parenchyma was affected by infarction. Unexpectedly, seven fetuses, whose body weights were still above the 10th percentile at birth and which were thus considered as nongrowth-retarded(Table 1, nos. 22-28), exhibited the same severe reduction of erythropoiesis as observed in the growth retarded ones (Fig. 3). Therefore, in contrast to the hypothesis mentioned above, one might speculate that the cause for impaired red blood cell production might be preeclampsia itself rather than intrauterine growth retardation. In view that preeclampsia is considered an immunologic disease(7), one possible explanation might be that preeclampsia alters the concentration of a variety of growth factors known to support hematopoiesis. To test this notion, we quantitated Epo concentration in the umbilical cord blood and several cytokines in amniotic fluid taken from 12 premature newborns (considered as the control group) as well as from 13 growth-retarded babies born under the conditions of preeclampsia. The levels of Epo and IL-3 were elevated by 50 and 800%, respectively, in samples derived from premature babies born under the condition of preeclampsia compared with the control group (Table 2). The hematocrit of the premature newborns was 56 ± 4.4 (n = 9) and the one of babies born from preeclamptic mothers was 63 ± 3.2 (n = 6). In contrast to Epo and IL-3, GM-CSF, G-CSF, and IL-1β, all of which support mainly myelomonocytic lineages, were reduced by a factor of about 1.7-3.4. No statistical significant differences were found for IL-6 and IL-8, whereas the concentrations of IL-2 and interferon-γ were below the detection level in both groups.
Reduction of erythroid cells in the livers of fetuses from preeclamptic mothers: early and late erythroid cells are compared in 10 control fetuses as well as 11 fetuses with and 7 fetuses without growth retardation; elements of erythroid lineage are less numerous per mm2 of liver tissue with preeclampsia, irrespective of the intrauterine growth stage.
DISCUSSION
A major proportion of intrauterine growth retardation and late fetal death in the Western world correlates with maternal preeclampsia. However, little is known about the involved pathophysiologic mechanisms. In the present study, we describe a severe reduction of hepatic erythropoiesis in human fetuses born from mothers suffering from preeclampsia. As affected fetuses often are growth-retarded, we investigated whether this intrauterine growth retardation represents the cause of altered hepatic erythropoiesis. It is known that, with intrauterine growth retardation, nucleated red blood cells are mobilized to the fetal peripheral blood, whereas there is no concomitant increase in the rate of cell division of the progenitors(13). At least in the guinea pig, it has been demonstrated that intrauterine growth retardation, which has been caused by cutting down maternal blood supply to the uterus, results in reduction of fetal hepatic erythropoiesis(14).
In our study, 7 out of 18 fetuses born from preeclamptic mothers were not growth-retarded at birth but, nevertheless, exhibited a reduced hepatic erythropoiesis similar to the growth-retarded ones. We considered all seven non-growth-retarded fetuses as such, because fetal body weights were indistinguishable compared with the control infants (Table 1, compare percentiles of the respective kidney and heart weights). It is recognized that there is no clear-cut distinction between“growth-retarded” and “normal-weighted” fetuses, as intrauterine growth retardation represents a continuous process. Thus, fetuses from preeclamptic mothers, whom we considered as normal weighted, might only be at the beginning of the dystrophic phase. Nevertheless, evidence could be presented that severe reduction of liver erythropoiesis can occur before a general growth retardation. Thus, we conclude that depression of red blood cell formation might be attributed to preeclampsia itself rather than to intrauterine growth retardation.
How does preeclampsia affect liver erythropoiesis? As mentioned in the results section, preeclampsia might alter the expression levels of hematopoietic growth factors. We thus quantitated Epo levels in the umbilical cord blood as well as the concentration of several cytokines, including IL-3 present in the amniotic fluid. Epo is known to regulate erythroid differentiation in the hematopoietic organs, including fetal liver, by preventing apoptosis of erythroid progenitor cells(15). We observed a moderate but significant elevation of Epo concentration by 50% in fetal cord blood, which can be explained by hypoxic exposure of the fetus(see below). IL-3 acts early during hematopoiesis by stimulating colony formation of erythroid lineages as well as megakaryocyte, neutrophil, eosinophil, basophil, mast cell, and monocytic lineages(16). In several ways, IL-3 also seems to prevent apoptosis in IL-3-dependent cells(17–19). Although Epo and IL-3 levels were increased in the blood of these fetuses, the remaining erythropoietic islands observed in fetal liver sections from the preeclamptic group showed dying cells containing clumped and fragmented chromatin characteristic for apoptosis. Most probably, this situation is another example demonstrating that activation of programmed cell death can be dominant to the suppression of apoptosis by Epo and IL-3(20). Examination of further colony-supporting and differentiation-inducing factors showed significant reductions of IL-1β, which has been defined as an apoptosis-inhibiting factor in hematopoiesis(21). Reduction was also found for the granulopoiesis-promoting factors GM-CSF and G-CSF. More factors are known that influence fetal hematopoiesis such as interferon-α(22), stem cell factor(23), IGF(15), and IL-2(21). In our series, IL-2 and interferon-γ concentrations were under the detection level for all tested samples. The inflammatory cytokines IL-6 and IL-8, known to influence hematopoiesis, were detected in amniotic fluid, but no significant difference in their concentrations was observed in normal growing or growth-retarded fetuses.
The observation that placentas from preeclamptic mothers are small and show infarction indicates that the resulting fetuses most probably are exposed to chronic hypoxia. Reduced oxygenation in turn is known to up-regulate Epo gene expression as well as a growing number of other genes including the vascular endothelial growth factor, glycolytic enzymes, and acute phase proteins(24, 25). Therefore, we postulate that hypoxia might alter fetal expression of certain genes involved in hematopoiesis. Indeed, hypoxically induced changes in immunoreactive Epo concentrations from human fetal blood samples(26–29) as well as increased mRNA levels of vascular endothelial growth factor and aldolase in an in vitro system of mouse embryogenesis(30) have been reported, indicating that the embryo/fetus is able to respond to changes in oxygen supply. In contrast to the expected effect of hypoxically induced Epo levels, fetal erythropoiesis was reduced in fetuses from preeclamptic mothers, suggesting that disturbances of red blood cell production occur at early stages of erythroid differentiation. This suggests that erythropoiesis in utero is dependent on many more factors than merely oxygen supply.
Together with our previous observations of high constitutive cytokine production in fetus and placenta and changes occurring with amniotic infection and with preeclampsia(8, 31), we propose that normal fetal hematopoiesis requires the coordinated interaction of many(hematopoietic) growth factors. Changes in oxygen concentrations might interfere in this network by up- or down-regulating genes involved in fetal hematopoiesis. From a clinical point of view, quantitation of various cytokines present in the amniotic fluid might help to detect the impact of developing preeclampsia on fetal well being or, if no such changes can be observed, reassure that the in utero life conditions are not as yet severely affected. This could help in determining the time point of therapeutic interventions that can be of critical importance for a very immature newborn. This notion might hold true regardless of the poor correlation found between cytokine concentration in fetal serum and amniotic fluid(32). To verify our suggestion, we are currently performing further prospective studies.
Abbreviations
- Epo:
-
erythropoietin
- G:
-
granulocyte
- GM:
-
granuloctye/macrophage
- CSF:
-
colony-stimulating factor
References
Sohn DS, Kim KY, Lee WB, Kim DC 1993 Eosinophilic granulopoiesis in human fetal liver. Anat Rec 235: 453–460
Tavassoli M 1991 Embryonic and fetal hemopoiesis: an overview. Blood Cells 1: 269–281
Thomas DB, Yoffey JM 1964 Human foetal haematopoiesis. II. Hepatic haematopoiesis in the human foetus. Br J Haematol 10: 193–197
Wilkins BS, Green A, Wild AE, Jones DB 1994 Extramedullary haemopoiesis in fetal and adult human spleen: a quantitative immunohistological study. Histopathology 24: 241–247
Stallmach T, Karolyi L 1993 Augmentation of fetal granulopoiesis with chorioamnionitis during the second trimester of gestation. Hum Pathol 25: 244–247
Khong TY, Robertson WB 1992 Spiral artery disease. In: Coulam CB, Faulk WP, McIntyre JA (eds) Immunological Obstetrics. Norton Medical Books, New York, pp 492–501
Galstian A, Beer AE, Roberts JM, Coulam CB, Faulk WP 1992 Immunology of preeclampsia. In: Coulam CB, Faulk WP, McIntyre JA (eds) Immunological Obstetrics. Norton Medical Books, New York, pp 502–516
Stallmach T, Hebisch G, Joller HI, Kolditz P, Engelmann M 1995 Expression pattern of cytokines in the different compartments of the feto-maternal unit under various conditions. Reprod Fertil Dev 7: 1573–1580
Altman DG 1993 Construction of age-related reference centiles using absolute residuals. Stat Med 12: 917–924
Moloney WC, McPherson L, Fliegelmann L 1960 Esterase activity in leukocytes demonstrated by the use of naphthol ASD chloroacetate substrate. J Histochem Cytochem 8: 200–207
Kamps WA, Timens W, De Boer GJ, Spanjer HH, Poppema S 1989 In situ study of haemopoiesis in human fetal liver. Scand J Immunol 30: 399–408
Eckardt KU, Kurtz A, Hirth P, Scigalla P, Wieczorek L, Bauer C 1988 Evaluation of the stability of human erythropoietin in samples for radioimmunoassay. Klin Wochenschr 66: 241–245
Thilaganathan B, Stagiannis K, Meher-Homji NJ, Plachouras N, Nicolaides KH 1994 Fetal blood mononuclear cell division in normal and pathological pregnancies. Fetal Diagn Ther 9: 79–83
Ernst LM, Salafia CM, Carter AM, Pezzullo JC 1993 Hepatic histology in intrauterine growth retardation following uterine artery ligation in the guinea pig. Pediatr Pathol 13: 763–772
Koury MJ, Bondurant MC 1992 The molecular mechanism of erythropoietin action. Eur J Biochem 210: 649–663
Ihle JN 1992 Interleukin 3 and hematopoiesis. Chem Immunol 51: 65–106
Athanasiou M, Mavrothalassitis GJ, Yuan CC, Blair DG 1996 The Gag-Myb-Ets fusion oncogene alters the apoptotic response and growth factor dependence of interleukin-3 dependent murine cells. Oncogene 12: 337–344
Quash G, Roch AM, Chantepie J, Michal Y, Fournet G, Dumontet C 1995 Methional derived from 4-methylthio-2-oxobutanoate is a cellular mediator of apoptosis in BAF3 lymphoid cells. Biochem J 305: 1017–1025
Crompton T 1991 IL3-dependent cells die by apoptosis on removal of their growth factor. Growth Factors 4: 109–116
Askew DS, Ihle JN, Cleveland JL 1993 Activation of apoptosis associated with enforced myc expression in myeloid progenitor cells is dominant to the suppression of apoptosis by interleukin-3 or erythropoietin. Blood 82: 2079–2087
Kaminski M 1994 Processes of cell necrosis-apoptosis-and their modification by toxic substances. Med Pr 45: 267–277
Tarumi T, Sawada K, Sato N, Kobayashi S, Takano H, Yasukouchi T, Takashashi T, Sekiguchi S, Koike T 1995 Interferon-α-induced apoptosis in human erythroid progenitors. Exp Hematol 23: 1310–1318
Muta K, Krantz SB, Bondurant MC, Wickrema A 1994 Distinct roles of erythropoietin, insulin-like growth factor I, and stem cell factor in the development of erythroid progenitor cells. J Clin Invest 94: 34–43
Wenger RH, Rolfs A, Marti HH, Bauer C, Gassmann M 1995 Hypoxia, a novel inducer of acute phase gene expression in a human hepatoma cell line. J Biol Chem 46: 27865–27870
Wenger RH, Gassmann M 1997 Oxygen(es) and the hypoxia-inducible factor-1. Biol Chem 378: 609–616
Ruth V, Widness JA, Clemons G, Raivio KO 1990 Postnatal changes in serum immunoreactive erythropoietin in relation to hypoxia before and after birth. J Pediatr 116: 950–954
Georgieff MK, Schmidt RL, Mills MM, Radmer WJ, Widness JA 1992 Fetal iron and cytochrome c status after intrauterine hypoxemia and erythropoietin administration. Am J Physiol 262: 485–491
Maier RF, Bohme K, Dudenhausen JW, Obladen M 1993 Cord blood erythropoietin in relation to different markers of fetal hypoxia. Obstet Gynecol 81: 575–580
Snijders RJ, Abbas A, Melby O, Ireland RM, Nicolaides KH 1993 Fetal plasma erythropoietin concentration in severe growth retardation. Am J Obstet Gynecol 168: 615–619
Gassmann M, Fandrey J, Bichet S, Wartenberg M, Marti HH, Bauer C, Wenger RH, Acker H 1996 Oxygen supply and oxygen-dependent gene expression in differentiating embryonic stem cells. Proc Natl Acad Sci USA 93: 2867–2872
Stallmach T, Hebisch G, Joller HI, Orban P, Schwaller J, Engelmann M 1995 Cytokine production and visualized effects in the feto-maternal unit: quantitative and topographic data on cytokines during intrauterine disease. Lab Invest 73: 384–392
Westgren M, Sverker EK, Remberger M, Ringden O, Stangenberg M 1995 Cytokines in fetal blood and amniotic fluid in Rh-immunized pregnancies. Obstet Gynecol 86: 209–213
Acknowledgements
The authors thank R. Tihic and W. Baier-Kustermann for performing the chloroacetate esterase stainings and the Epo RIA, respectively.
Author information
Authors and Affiliations
Additional information
Supported by the Hartmann-Müller-Stiftung Grant 626 (to T.S.) and by the Swiss National Science Foundation (31-47111.96) (to M.G.).
Rights and permissions
About this article
Cite this article
Stallmach, T., Karolyi, L., Lichtlen, P. et al. Fetuses from Preeclamptic Mothers Show Reduced Hepatic Erythropoiesis. Pediatr Res 43, 349–354 (1998). https://doi.org/10.1203/00006450-199803000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199803000-00007
This article is cited by
-
Reduced angiovasculogenic and increased inflammatory profiles of cord blood cells in severe but not mild preeclampsia
Scientific Reports (2021)
-
Preeclampsia in pregnancy affecting the stemness and differentiation potency of haematopoietic stem cell of the umbilical cord blood
BMC Pregnancy and Childbirth (2020)
-
Erythropoietin concentration among patients with and without preeclampsia
Archives of Gynecology and Obstetrics (2005)