Abstract
This study examined the hypothesis that the cerebrovascular response to asphyxia of the late gestation sheep fetus is characterized by an increase in cerebrovascular resistance and a fall in cerebral blood flow (CBF) rather than the fall in resistance and increase in CBF which occurs in acute hypoxemia. In eight unanesthetized late gestation fetal sheep (123- to 125-d gestation) we evaluated continuous changes in carotid blood flow (CaBF) as an index of global CBF and total cerebral Hb concentrations as an index of global cerebral blood volume (CBV) using ultrasound flow probes and near infrared spectroscopy respectively. Asphyxia was induced by rapid and complete occlusion of the umbilical cord for 10 min. We also examined the fetal response to 1 h of acute 9% isocapnic hypoxia for comparison purposes. During hypoxia we observed a sustained increase in CaBF (p < 0.05) and CBV (p < 0.01) and a fall in carotid vascular resistance (p < 0.05). During asphyxia there was no significant rise in CBV, a fall in CaBF (p < 0.05), and a rise in carotid vascular resistance (p < 0.01). CaBF fell at a time when mean arterial pressure was elevated (p < 0.01). These data strongly suggest that fetal CBF does not increase and may even fall during severe asphyxia of rapid onset. Furthermore, our near infrared spectroscopy data show that the relative changes in total cerebral Hb concentrations may reflect the type and severity of the insult to which the fetus is exposed.
Similar content being viewed by others
Main
The cerebrovascular responses of the late gestation fetus to asphyxia, as opposed to moderate hypoxemia, have not been established unequivocally. It is widely reported that the fetus compensates, either partially or wholly, for hypoxia or asphyxia by increasing CBF, an increase that is mediated locally by a fall in cerebral vascular resistance and systemically by hypertension (1–6). This circulatory centralization thus maintains oxygen delivery to "essential" organs such as the brain, heart, and adrenals at the expense of the periphery (7–9). If asphyxia is prolonged, the compensatory mechanisms fail, with reduced cardiac contractility, hypotension, and a consequent fall in CBF (2,4). This hypotension has been strongly associated with neural injury (10). There is, however, contradictory evidence from a small number of previous studies of asphyxia that have reported either no early increase in CBF or a fall in CBF, although rapid initial changes were not determined (9,11,12). If there were indeed no increase, it would suggest that the fetal brain might be compromised much earlier than anticipated during some types of asphyxial insults. However, the factors determining whether cerebral centralization occurs are unknown. The specific experimental approach used may be important, for example with uterine artery occlusion versus umbilical occlusion (2). The severity of the insult is also important, and it has been suggested that failure of CBF to increase during asphyxia reflects cardiac compromise (11). Finally, we postulate that a key factor is likely to be the speed with which severe asphyxia is induced.
In this study we tested the hypothesis that CBF does not increase during rapidly induced severe asphyxia. We induced asphyxia by umbilical cord occlusion and used continuous NIRS and carotid blood flow measurements to assess continuous changes in total CBF and CBV. We compared the cerebrovascular response to asphyxia with the response to acute isocapnic hypoxia, an insult in which the nature of the cerebrovascular response has already been well established.
METHODS
Subjects and surgery. All procedures were conducted under license and in accordance with the Animals and Scientific Procedures Act, UK, 1986. Details about animal surgical preparation and maintenance have been previously described (8). Eight fetal sheep (Suffolk and Blue-faced Leicester Cross Mule) were instrumented at 117 to 121 d of gestation under general anesthesia using sterile techniques. Fetal catheters were placed in the right axillary vein and artery and the amniotic sac. Ultrasound blood flow probes (3R, Transonic Systems Inc., Ithaca, NY) were placed around either one or both carotid arteries above the vertebral anastomoses for the measurement of carotid blood flow. In two fetuses the vertebral-occipital anastomoses and lingual arteries were ligated bilaterally to maximize the proportion of cerebral blood flow in the carotid arteries (13). Stainless-steel electrodes were sewn across the chest and onto a hind limb to record the ECG. A pair of electrodes was implanted biparietally on the dura for ECoG recordings. Two flexible fiber optic probes, used for the NIRS recordings, were placed biparietally on the skull 3.5 cm apart, 1 cm anterior to bregma, and secured using rapid setting dental cement (Rocket Red, Dental Adventures of America, Inc., Corona, CA). An inflatable silicone occluder was placed around the umbilical cord. All leads were exteriorized through the maternal flank. Benzylpenicillin sodium (Crystapen, 600 mg) was administered into the amniotic sac before closure. A maternal femoral vein was catheterized and the ewes were given 5 mL of Streptopen intramuscularly.
After surgery, the sheep were housed together in separate metabolic cages with access to water and food ad libitum. A period of 3 to 4 d postoperative recovery was allowed, during which time antibiotics were administered daily to the ewe (600 mg Crystapen i.v. for 4 d and 80 mg Gentamicin i.v. daily for the first 3 d) and fetal arterial blood was taken for blood gas analysis for assessment of fetal health. Catheters were maintained patent by continuous infusion of heparinized saline (50 U·mL-1 at 0.2 mL.h-1).
Physiological data measurements. Fetal ECoG, ECG, mean FHR (derived from ECG), arterial and venous blood pressure, and carotid blood flows were monitored continuously throughout the protocols using a Graphtec chart recorder (Linearcorder FWR 3701, Graphtec, UK). Concentration changes in fetal cerebral [Hb], [HbO2], and [THb] data were collected using the NIR 500 spectrophotometer (Hamamatsu Photonics KK, Hamamatsu City, Japan), and data were recorded by computer for off-line analysis.
The principles of NIRS have been described previously (14–16) and used in the fetal sheep (17,18). Near infrared light, at 3 different wavelengths between 775 and 908 nm, was carried to the fetal head through a fiber optic bundle. Emerging light was collected by the second optode and transmitted to the spectrophotometer. Changes in the cerebral [HbO2] and [Hb] were calculated from the modified Lambert-Beer law using a previously established algorithm and assuming a pathlength factor of 4.39 ± 0.28 (mean ± SD) (15,19). The absorption coefficients of HbO2 and Hb are known (19). Changes in [THb] were obtained as the sum of changes in [HbO2] and [Hb] and are related to CBV by the cerebral hematocrit: CBV (mL·100 g brain-1) = [THb]/(H.R) where H is the arterial Hb and R the cerebral-to-large vessel hematocrit ratio assumed to be 0.69 (15). The NIRS measures obtained are relative changes from zero, not absolute changes. CBV was not quantitatively measured, but [THb] was used as an index of CBV. NIRS data were collected with a temporal resolution of 10 s. All data were then averaged over 1-min intervals for asphyxia and 5-min intervals for hypoxia.
Experimental procedures. Four fetuses underwent hypoxia then asphyxia experiments on consecutive days, one experienced hypoxia only, and three experienced asphyxia only (5 hypoxia experiments and 7 asphyxia experiments).
Asphyxia protocol. After a control period of 30 min, fetal asphyxia was induced by rapid inflation of the umbilical occluder for 10 min (20). The occluder was inflated sufficiently to produce an immediate sharp rise in arterial blood pressure and an isoelectric ECoG (<5 µv2, 1-20 Hz). Fetal arterial blood was taken at 15 min before asphyxia, at 5 min of asphyxia, and at 15 postasphyxia for determination of pH, PaO2, PaCO2, oxygen saturation, oxygen content, hematocrit, and Hb (Instrumentation Laboratories blood gas analyzer, model IL 1301 and co-oximeter, model IL 482, Italy) and for glucose and lactate measurements (YSI model 2300, Yellow Springs, OH).
Hypoxia protocol. After a control period of 30 min, during which time the ewe breathed air, fetal isocapnic hypoxemia was induced for 1 h by reduction of the maternal FiO2 to 9 to 10% (inspirate 16 L·min-1 air; 22 L·min-1 nitrogen; 1.2 L·min-1 carbon dioxide) (8). After hypoxia, the ewe was returned to air for an additional 30 min. Fetal arterial blood was taken at 30 and 15 min before hypoxia; 5, 15, and 45 min during hypoxia; and 15 and 30 min after hypoxia for the measurements described above.
Data analysis. Data are presented as means ± SEM. CaVR (mm Hg·mL-1·min) was calculated using the formula (mean arterial pressure-mean venous pressure)/carotid blood flow. When two flows were measured, the data were averaged. Data were analyzed using one-way repeated-measures analysis of variance. When statistical changes over time were found, Dunnett's post hoc test was used to determine individual changes during and postinsult with baseline. A t test was used to analyze the blood composition data. Statistical significance was accepted when p < 0.05.
RESULTS
Blood Composition Measurements
Values and statistical comparisons for blood gases, Hb, hematocrit, glucose, and lactate during hypoxia and asphyxia are presented in Table 1. During hypoxia the fetal PaO2 fell to 1.59 ± 0.48 kPa from 2.96 ± 0.2 kPa (p < 0.005), but there were no significant changes in pH and PaCO2. During asphyxia the fetal PaO2 fell to 0.85 ± 0.2 kPa (p < 0.001), the pH fell to 7.001 ± 0.0 (p < 0.001), and the PaCO2 increased to 13.79 ± 1.1 kPa (p < 0.001) (Table 1).
Fetal Heart Rate, Blood Pressure, Blood Flow, and ECoG Activity
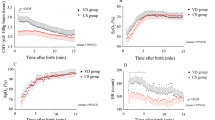
Asphyxia. FHR fell rapidly after the start of asphyxia and bradycardia (99.4 ± 3 bpm) was sustained throughout the period of occlusion (p < 0.01). After occlusion the fetuses became tachycardic (225.8 ± 2.2 bpm, p < 0.01) (Fig. 1). MAP rose significantly at the start of occlusion, peaking at 69.4 ± 5.0 mm Hg by 4 min (p < 0.01). MAP then progressively fell until the end of occlusion. During recovery MAP rose significantly and peaked at 61.2 ± 3.7 mm Hg by 6 min (p < 0.01), MAP then returned to control (Fig. 1). There was a progressive fall in carotid blood flow during asphyxia. Carotid blood flow had fallen significantly by 3 min of asphyxia (p < 0.05). Post occlusion there was a large significant rise in carotid blood flow between 2 and 5 min (p < 0.01) peaking at 128 ± 22.05 mL/min at 4 min. Thereafter, carotid blood flow returned to control values. No differences were seen in the carotid blood flow responses in the fetuses in which collateral blood flow was ligated compared with the nonligated group. There was a significant increase in carotid vascular resistance during asphyxia; values more than doubled (p < 0.01). Postasphyxia carotid vascular resistance fell rapidly to control values. During asphyxia ECoG activity became isoelectric 1.02 ± 0.3 min after the start of occlusion and remained isoelectric throughout asphyxia and during recovery (data not shown).
Effect of 10 min of severe asphyxia induced by umbilical cord occlusion on FHR, MAP, CaBF, and CaVR. The shaded region denotes the period of asphyxia. Values are means ± SEM (black bars, # p < 0.05; p < 0.01). Note the progressive fall in CaBF and the associated rise in CaVR at a time when MAP is significantly elevated.
Hypoxia. At the onset of hypoxia there was a significant fall in FHR. FHR remained significantly lower during the first 15 min (Fig. 2; p < 0.05) but gradually returned to baseline values by the end of the hypoxic period. Sustained tachycardia (198 ± 7.5 bpm) developed with reoxygenation (p < 0.005) (Fig. 2). MAP rose significantly during hypoxia by 10 min (p < 0.05) and remained significantly elevated during recovery (p < 0.05) (Fig. 2). Carotid blood flow rose significantly during hypoxia by 10 min (p < 0.05), and there was a significant fall in carotid vascular resistance by 10 min (p < 0.05). Carotid blood flow and vascular resistance returned to baseline values by 10 min after hypoxia (Fig. 2). ECoG activity switched from low-voltage to high-voltage ECoG within 2.6 ± 0.4 min of the start of hypoxia and switched back to low-voltage ECoG activity after 36.2 ± 3.7 min of hypoxia. In 2 animals this return to low-voltage ECoG activity was sustained; in the other 3 animals the ECoG activity continued to cycle between low- and high-voltage activity (data not shown).
Effect of 1 h of isocapnic hypoxia on FHR, MAP, CaBF, and CaVR. The shaded region denotes the period of hypoxia. Values are means ± SEM, # p < 0.05; ** p < 0.005, for individual time points or intervals of data (black bars). There is a significant rise in CaBF during hypoxia, which is associated with a fall in CaVR and a rise in MAP.
NIRS Measurements
Asphyxia. There was no significant change in [THb] during asphyxia compared with control. There was a significant rise in [THb] starting at 19 min postocclusion (p < 0.05) (Fig. 3). During asphyxia there was a substantial and rapid rise in [Hb] (p < 0.001) and a rapid and significant fall in [HbO2] (p < 0.005) (Fig. 3). Postinsult the changes in [HbO2] and [Hb] were variable. The rise in [HbO2] was gradual; [HbO2] remained significantly lower for the first 4 min (p < 0.01). [HbO2] then became transiently elevated (p < 0.05) before returning to control values by 11 min. [HbO2] rose again at approximately 21 min and remained elevated (p < 0.05). [Hb] remained significantly elevated, but fell to control values by 6 min (p < 0.05). There was a transient significant elevation in [Hb] starting at 13 min and lasting for 6 min (p < 0.05); [Hb] then fell to control values.
Changes from an arbitrary baseline in fetal cerebral HbO2 (#), Hb (f), and THb (*) during 10 min of severe asphyxia induced by umbilical cord occlusion. The shaded region denotes the period of asphyxia. Values are means ± SEM, * p < 0.05; fff p < 0.005; #### p < 0.001, for individual time points or intervals of data (black bars). Note the reciprocal changes in [HbO2] and [Hb] without a rise in [THb] indicating cerebral blood volume did not increase.
Hypoxia. At the onset of hypoxia there was a substantial and rapid rise in [Hb] (p < 0.01), a fall in [HbO2] (p < 0.005), and a significant rise in [THb] (p < 0.001) (Fig. 4). The largest increase in [Hb] was observed during the first 10 min of hypoxia; thereafter the rise in Hb was small and gradual. During recovery there was a rapid fall in [Hb], and values returned to baseline values by 15 min of recovery. The fall in [HbO2] reached a nadir at around 10 min; thereafter there was a slight rise in [HbO2], but [HbO2] remained significantly lower compared with baseline values throughout hypoxia (p < 0.005). The nadir of the fall in [HbO2] and peak in the rise in [Hb] during hypoxia were significantly less than those observed during asphyxia (p < 0.05). During recovery [HbO2] significantly increased during the first 15 min (p < 0.05), thereafter returning to baseline values. Overall there was a substantial and rapid increase in [THb] during the first 15 min of hypoxia; thereafter values continued to increase gradually throughout hypoxia (p < 0.001). [THb] fell on reoxygenation, remaining significantly elevated during the first 10 min (p < 0.05) before returning to baseline values by 15 min.
This figure shows the changes from an arbitrary baseline in fetal cerebral HbO2 (#), Hb (166), and THb (*) before, during, and after 1 h of isocapnic hypoxia. The shaded region denotes the period of hypoxia. Values are means ± SEM (black bar, #, f, *, p < 0.05; ff p < 0.01; ### p < 0.005; **** p < 0.001). Note the reciprocal changes in [HbO2] and [Hb] and the significant rise in [THb] during hypoxia indicating that cerebral blood volume has increased.
DISCUSSION
It was the purpose of this study to evaluate the hypothesis that CBF does not increase during acute severe asphyxia of rapid onset in the late gestation sheep fetus and that this is caused by a substantial increase in cerebral vascular resistance rather than a reduction in blood pressure. The present results support this hypothesis. We observed no increase in CBV, measured by NIRS, and an immediate fall in carotid blood flow. The fall in carotid blood flow was associated with a substantial increase in carotid vascular resistance that occurred rapidly after the onset of asphyxia and at a time when MAP had increased substantially. Thus carotid blood flow fell before the fall in MAP. Our data demonstrate that the fetal cerebrovascular response to asphyxia is more complex than is commonly proposed. Under some conditions of oxygen deprivation there is clearly a failure of circulatory centralization to the fetal brain from the outset of the insult. Cerebral protection may then only depend on regional redistribution of blood toward important brain structures, such as the brainstem, and a significant reduction in cerebral metabolism and oxygen consumption (2).
Methodological considerations. The accuracy of NIRS for detecting alterations in cerebral [THb], [HbO2], and [Hb] has been described previously (21) and has been extensively demonstrated as an applicable method for the continuous real-time measurement of changes in cerebral vascular tone pre- and postnatally (14,17,18,22). The differences in fetal Hb do not appear to alter NIRS measurements and interpretation of vascular tone (17,18,23), and it is unlikely that minor shifts in arterial Hb and hematocrit alter the validity of the NIRS measurements. Undoubtedly a current technical problem in the application of NIRS technology is the inability to quantify the area or volume of tissue being interrogated, and this technique must be refined further to allow monitoring of more discrete areas. However, the global [THb] data we obtained are consistent with other NIRS studies (24–27).
Currently the microsphere technique remains the only direct measure of CBF, and further studies using microspheres will be required to examine in greater detail the observations made in this article. However, the microsphere technique is limited because only a few time points may be studied and it is difficult to obtain samples quickly enough to determine initial rapid changes in blood flow. For these reasons we used carotid blood flow measurements as a measure of global CBF changes. This method permits continuous real-time measures of blood flow. Carotid blood flow measurements have been shown to correlate closely with CBF as measured by microspheres (r = 0.97), and this relationship is reportedly true for the pressures obtained in our study (28). We did not observe any differences in carotid blood flow between the ligated and nonligated animals before, during, or after asphyxia, suggesting that our carotid blood flow measurements provided a good index of cerebral blood flow. Our carotid blood flow data are consistent with previous microsphere data during hypoxia and asphyxia (2,9,11,12,29).
Hypoxia. The fetal cardiovascular response to hypoxia has been well described (1,9), although we present, for the first time, data obtained by NIRS during hypoxia in the fetus. A number of studies have shown that the late gestation sheep fetus, at an age approximately equivalent to the term human with regard to brain maturation (30), is capable of responding to a reduction in oxygenation with a complex series of local vascular and neuronal reflexes which act to protect vital organs, including the brain (7–9). The acute cardiovascular response to hypoxemia is mediated via predominantly carotid chemoreflexes, which are rapid in onset, and via endocrine responses, which develop more slowly (1,7,8). An initial bradycardia is followed by an increase in FHR; MAP also increases (Fig. 2). Combined ventricular output is redistributed favoring essential organs such as the brain, as can be seen from the observed rise in carotid blood flow and carotid vascular resistance in our study (Figs. 2 and 4). This increase in cerebral perfusion was facilitated by a decrease in carotid vascular resistance. (Fig. 2) and probably the loss of cerebral autoregulation, which is known to occur during hypoxia and which allows blood flow to follow pressure (31,32). Thus the fetus compensates well during an insult of this nature; it has been demonstrated that despite reductions of the PaO2 to 1.6 kPa or of oxygen content to 1 mmol/mL-1, cerebral oxygen consumption is changed little because CBF and oxygen extraction are increased and oxygen demands are reduced, as demonstrated by the switch to high-voltage ECoG activity in our study (33,34).
The NIRS data are consistent with a number of studies, which report reciprocal changes in [Hb] and [HbO2], with a fall in [HbO2] and a rise in [Hb] (24–26,35–38). This represents a fall in arterial saturation and can occur with or without changes in [THb] (24,39). The mechanisms underlying the different changes in [THb] are debated in the clinical literature (14,22,35), but our hypoxia data would suggest that cerebral desaturation associated with a rise in [THb] indicates fetal compensation. Conversely, the asphyxia data suggest that a fall in cerebral saturation with no change or a fall in [THb] indicates a more severe insult during which the fetus cannot compensate. This would be consistent with the clinical findings where profound changes in fetal heart rate, which denote fetal distress (variable, late, and prolonged decelerations), are associated with a failure of [THb] to rise (38–40). This has also been observed in neonates during bradycardia and marked arterial desaturation (36). Clinically, more moderate hypoxia would appear to be associated with rises in [THb] (25,36).
Asphyxia. The asphyxial insult used in this study was severe, as seen by the rapid switch to an isoelectric ECoG and profound changes in blood gases. It is an insult during which the fetus cannot compensate to maintain sufficient cerebral oxygen delivery, leading to a fall in oxygen consumption (2,3,11). Our study demonstrates that during a severe asphyxial insult of rapid onset, carotid blood flow never increased, even during the initial period of asphyxia, indicating that there was no rise in global CBF (Fig. 1). Instead, carotid blood flow fell and this fall occurred at a time when MAP was significantly increased; it therefore occurred before evidence of hypotension. The failure of [THb] to rise, indicating no change in cerebral perfusion, further supports this finding (Fig. 3). This contrasts with the milder hypoxic insult in which CBV rose substantially. The failure of [THb] and carotid blood flow to rise during asphyxia appears to be caused primarily by a significant increase in cerebral vascular resistance, as reflected in the carotid vascular resistance values, which more than doubled. Again this was not seen in hypoxia, in which there was a significant fall in carotid vascular resistance. The after asphyxial elevation of [THb], at a time when carotid blood flow had returned to normal, suggests the rise is not associated with hyperemia, but rather may be caused by venous congestion. Similar findings have been observed in piglets after reperfusion after cardiac arrest (24).
Our NIRS and carotid blood flow findings are consistent with those demonstrated by others who have shown that CBF, measured by microspheres, fell after the onset of asphyxia and that there was a doubling of resistance in the cerebral vasculature (9,11,12). The differences between these data and that of others showing an increase in CBF during asphyxia (5,6) may be due to the partial or slower nature of the insult used in the latter studies. This suggests that the severity and/or speed of onset of the insult may be very important in determining the cerebral vascular response. Our data suggest that in the face of a rapid, severe insult, the fetus actively initiates a response because there is a fast increase in vascular resistance at a time when perfusion pressure is elevated. Under these conditions, the response is contrary to the commonly held concept that cerebral hyperperfusion and hypertension characterize the initial phase of asphyxia. The eventual fall in blood pressure during severe asphyxia is likely to be largely mediated by a diminution of combined ventricular output, probably secondary to an effect on the myocardium (4). Although we have not measured combined ventricular output, we speculate that the initial fall in CBF is not caused by a failure of combined ventricular output because blood pressure was elevated at this time. Further work is required to elucidate these effects.
SUMMARY
Our data demonstrate that during severe asphyxia of rapid onset there is a failure of blood flow redistribution in favor of the brain, even during the initial phases of asphyxia when blood pressure is maintained. This appears to be caused by an active increase in cerebral vascular resistance. Further studies are required to determine the mechanisms mediating the initiation of this type of cerebrovascular response. The rapidity of the vasoconstriction during asphyxia and the immediate vasodilation postasphyxia suggests involvement of locally acting vasoactive substances, particularly because it has been shown that chemoreflexes do not play a role in the majority of the cerebrovascular responses of the fetus to asphyxia (29). Our NIRS findings show that a reciprocal fall in [HbO2] and rise in [Hb], accompanied by a failure of [THb] to rise, is associated with severe asphyxia and a failure of fetal compensatory mechanisms. Conversely, similar changes in [HbO2] and [Hb], in which [THb] rose, were observed during more moderate hypoxia, an insult where it has been extensively demonstrated by us and others that the fetus is able to compensate. These findings are of relevance to the clinical interpretation of NIRS.
Abbreviations
- ECoG:
-
electrocorticogram
- ECG:
-
electrocardiogram
- NIRS:
-
near infrared spectroscopy
- [THb]:
-
concentration of total cerebral Hb
- [HbO2]:
-
concentration of oxyhemoglobin
- [Hb]:
-
concentration of deoxyhemoglobin
- CaBF:
-
carotid blood flow
- CaVR:
-
carotid vascular resistance
- CVR:
-
cerebral vascular resistance
- MAP:
-
mean arterial blood pressure
- CBF:
-
cerebral blood flow
- CBV:
-
cerebral blood volume
- FHR:
-
fetal heart rate
- PaCO2:
-
partial pressure of arterial carbon dioxide
- PaO2:
-
partial pressure of arterial oxygen
- FiO2:
-
fraction of inspired oxygen
- bpm:
-
beats per minute
References
Giussani DA, Spencer JAD, Hanson MA 1994 Fetal cardiovascular reflex responses to hypoxaemia. Fetal Matern Med Rev 6: 17–37
Jensen A, Berger R 1991 Fetal circulatory responses to oxygen lack. J Dev Physiol 16: 181–207
Parer JT 1994 Fetal cerebral metabolism: the influence of asphyxia and other factors. J Perinatol 14: 376–385
Volpe JJ 1995 Hypoxic-ischemic encephalopathy: neuropathology and pathogenesis. In: Saunders WB, (ed) Neurology of the Newborn, 3rd Ed. WB Saunders, Philadelphia, 279–313.
Ball RH, Parer JT, Caldwell LE, Johnson J 1994 Regional blood flow and metabolism in ovine fetuses during severe cord occlusion. Am J Obstet Gynecol 171: 1549–1555
de Haan HH, Van Reempts JL, Vles JS, de Haan J, Hasaart TH 1993 Effects of asphyxia on the fetal lamb brain. Am J Obstet Gynecol 169: 1493–1501
Bartelds B, Van Bel F, Teitel DF, Rudolph AM 1993 Carotid, not aortic, chemoreceptors mediate the fetal cardiovascular response to acute hypoxemia in lambs. Pediatr Res 34: 51–55
Giussani DA, Spencer JA, Moore PJ, Bennet L, Hanson MA 1993 Afferent and efferent components of the cardiovascular reflex responses to acute hypoxia in term fetal sheep. J Physiol 461: 431–449
Jensen A, Hohmann M, Kunzel W 1987 Dynamic changes in organ blood flow and oxygen consumption during acute asphyxia in fetal sheep. J Dev Physiol 9: 543–559
Gunn AJ, Parer JT, Mallard EC, Williams CE, Gluckman PD 1992 Cerebral histological and electrophysiological changes after asphyxia in fetal sheep. Pediatr Res 31: 486–491
Field DR, Parer JT, Auslender RA, Cheek DB, Baker W, Johnson J 1990 Cerebral oxygen consumption during asphyxia in fetal sheep. J Dev Physiol 14: 131–137
Yaffe H, Parer JT, Block BS, Llanos AJ 1987 Cardiorespiratory responses to graded reductions of uterine blood flow in the sheep fetus. J Dev Physiol 9: 325–336
de Haan HH, Gunn AJ, Williams CE, Heymann MA, Gluckman PD 1997 Magnesium sulfate therapy during asphyxia in near-term fetal lambs does not compromise the fetus but does not reduce cerebral injury. Am J Obstet Gynecol 176: 18–27
Hamilton RJ, Hodgett SG, O'Brien PMS 1996 Near infrared spectroscopy applied to intrapartum fetal monitoring. Baillieres Clin Obstet Gynaecol 10: 307–324
Wyatt JS, Cope M, Delpy DT, Richardson CE, Edwards AD, Wray S, Reynolds EO 1990 Quantitation of cerebral blood volume in human infants by near-infrared spectroscopy. J Appl Physiol 68: 1086–1091
Wyatt JS 1993 Near-infrared spectroscopy in asphyxial brain injury. Clin Perinatol 20: 369–378
Marks KA, Mallard EC, Roberts I, Williams CE, Sirimanne ES, Johnston BM, Gluckman PD, Edwards AD 1996 Delayed vasodilation and altered oxygenation following cerebral ischemia in fetal sheep. Pediatr Res 39: 48–54
Marks KA, Mallard EC, Roberts I, Williams CE, Gluckman PD, Edwards AD 1996 Nitric oxide synthase inhibition attenuates delayed vasodilation and increases injury following cerebral ischemia in fetal sheep. Pediatr Res 40: 185–191
Wray S, Cope M, Delpy DT, Wyatt JS, Reynolds EOR 1988 Characterisation of the near infrared absorption spectra of cytochrome aa3 and haemoglobin for the non-invasive monitoring of cerebral oxygenation. Biochim Biophys Acta 933: 184–192
Mallard EC, Gunn AJ, Williams CE, Johnston BM, Gluckman PD 1992 Transient umbilical cord occlusion causes hippocampal damage in the fetal sheep. Am J Obstet Gynecol 167: 1423–1430
Cope M, Delpy DT 1988 System for long-term measurement of cerebral blood and tissue oxygenation on newborn infants by near infra-red transillumination. Med Biol Engl Comput 26: 289–294
du Plessis AJ 1995 Near-infrared spectroscopy for the in vivo study of cerebral hemodynamics and oxygenation. Curr Opin Pediatr 7: 632–639
Wickramasinghe YA, Palmer KS, Houston R, Spencer SA, Rolfe P, Thorniley MS, Oeseburg B, Colier W 1993 Effect of fetal hemoglobin on the determination of neonatal cerebral oxygenation by near-infrared spectroscopy. Pediatr Res 34: 15–17
Nomura F, Naruse H, Duplessis A, Hiramatsu T, Forbess J, Holtzman DX, Volpe JJ, Jonas R, Tsuji M 1996 Cerebral oxygenation measured by near infrared spectroscopy during cardiopulmonary bypass and deep hypothermic circulatory arrest in piglets. Pediatr Res 40: 790–796
D'Antona D, Aldrich CJ, Delpy DT, Reynolds EOR, Wyatt DT 1995 Effect of nuchal cord on fetal cerebral haemodynamics and oxygenation measured by near infrared spectroscopy during labour. Eur J Obstet Gynecol Reprod Biol 59: 205–209
Faris F, Doyle M, Wickramasinghe Y, Houston R, Rolfe P, O'Brien S 1994 A non-invasive optical technique for intrapartum fetal monitoring: preliminary clinical studies. Med Engl Phys 16: 287–291
Aldrich CJ, Dantona D, Wyatt JS, Spencer JAD, Peebles DM, Reynolds EOR 1994 Fetal cerebral oxygenation measured by near-infrared spectroscopy shortly before birth and acid-base status at birth. Obstet Gynecol 84: 861–866
Van Bel F, Roman C, Klautz RJM, Teitel DF, Rudolph AM 1994 Relationship between brain blood flow and carotid arterial flow in the sheep fetus. Pediatr Res 35: 329–333
Jensen A, Hanson MA 1995 Circulatory responses to acute asphyxia in intact and chemodenervated fetal sheep near term. Reprod Fertil Dev 7: 1351–1359
McIntosh GH, Baghurst KI, Potter BJ, Hetzel BS 1979 Foetal brain development in the sheep. Neuropathol Appl Neurobiol 5: 103–114
Papile L, Rudolph AM, Heymann MA 1985 Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 19: 159–161
Tweed WA, Cote J, Pash M, Lou H 1983 Arterial oxygenation determines autoregulation of cerebral blood flow in the fetal lamb. Pediatr Res 17: 246–249
Jones M Jr, Sheldon RE, Peeters LL, Meschia G, Battaglia FC, Makowski EL 1977 Fetal cerebral oxygen consumption at different levels of oxygenation. J Appl Physiol 43: 1080–1084
Richardson BS, Patrick JE, Abduljabbar H 1985 Cerebral oxidative metabolism in the fetal lamb: relationship to electrocortical state. Am J Obstet Gynecol 153: 426–431
O'Brien PMS, Doyle P, Rolfe P 1993 Near infrared spectroscopy in fetal monitoring. Br J Hosp Med 49: 483–487
Livera LN, Spencer SA, Thorniley MS, Wickramasinghe YA, Rolfe P 1991 Effects of hypoxaemia and bradycardia on neonatal cerebral haemodynamics. Arch Dis Child 66: 376–380
Peebles DM, Edwards AD, Wyatt JS, Bishop AP, Cope M, Delpy DT, Reynolds EO 1992 Changes in human fetal cerebral hemoglobin concentration and oxygenation during labor measured by near-infrared spectroscopy. Am J Obstet Gynecol 166: 1369–1373
Aldrich CJ, D'Antona D, Spencer JAD, Delpy DT, Reynolds EOR, Wyatt JS 1996 Fetal heart rate changes and cerebral oxygenation measured by near-infrared spectroscopy during the first stage of labour. Eur J Obstet Gynecol Reprod Biol 64: 189–195
Peebles DM, Spencer JA, Edwards AD, Wyatt JS, Reynolds EO, Cope M, Delpy DT 1994 Relation between frequency of uterine contractions and human fetal cerebral oxygen saturation studied during labour by near infrared spectroscopy. Br J Obstet Gynaecol 101: 44–48
Aldrich CJ, D'Antona D, Spencer JAD, Peebles D, Delpy DT, Reynolds EOR 1995 Late fetal heart decelerations and changes in cerebral oxygenation during the first stage of labor. Br J Obstet Gynaecol 102: 9–13
Acknowledgements
The authors thank the Wellcome Trust for support.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bennet, L., Peebles, D., Edwards, A. et al. The Cerebral Hemodynamic Response to Asphyxia and Hypoxia in the Near-term Fetal Sheep as Measured by Near Infrared Spectroscopy. Pediatr Res 44, 951–957 (1998). https://doi.org/10.1203/00006450-199812000-00022
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199812000-00022
This article is cited by
-
Validation of Cerebral Venous Oxygenation Measured Using Near-Infrared Spectroscopy and Partial Jugular Venous Occlusion in the Newborn Lamb
Journal of Cerebral Blood Flow & Metabolism (2008)