Abstract
As nitric oxide (NO) may be a particularly important vasodilator in early life, we investigated its role in the regulation of the gastrointestinal (GI) circulation at mid-gestation. Cardiac output and GI blood flow were measured by the radioactive microsphere technique in eight chronically instrumented and unanesthetized mid-gestation fetal sheep. Mean arterial pressure (MAP), heart rate, blood flow, oxygen delivery, and vascular resistance were determined before and after infusion of the specific NO synthase inhibitor,Nω-nitro-L-arginine (L-NNA) at doses of 10 and 25 mg/kg. In response to L-NNA infusion, MAP increased (p < 0.01) and combined ventricular output decreased (p < 0.001). GI blood flow and oxygen delivery decreased and vascular resistance increased in the stomach and all segments of the small and large intestine (all p< 0.001). The greatest reduction in blood flow was in the small intestine(p < 0.01) and the basal differential pattern of small intestinal blood flow exceeding large intestinal flow was completely abolished. These changes were much greater than those previously described in late-gestation fetuses. Our results suggest that, at mid-gestation, NO plays a major role in the regulation of blood flow and vascular tone across all segments of the fetal GI tract, with its effects being more pronounced than later in development.
Similar content being viewed by others
Main
Endothelium-derived NO is a potent vasodilator which, in the mature circulation, is a major determinant of intestinal blood flow, contributing to the characteristic low vascular resistance and high level of perfusion of this vascular bed(1). New information suggests that NO also plays a vasodilating role in the immature circulation, perhaps more powerful than that in the adult. NO synthesis is 9-fold greater in the fetus than the mother in sheep pregnancy(2), and NO plays a dominant role in maintaining the low vascular resistance and high perfusion of the umbilical-placental circuit(3,4). NO is also critical for maintaining the caliber of major arteries of the immature rat fetus(5) and thus is likely to be a powerful factor in determining blood flow in vascular beds other than the placenta. In the developing intestinal circulation of the lategestation sheep fetus, recent work has shown that NO plays an important role in contributing to low vascular resistance and high blood flow throughout the GI tract, as well as to the regional distribution of intestinal blood flow between intestinal segments, and across mucosal and muscular layers(6).
As yet no study has addressed the role of NO in the intestine at earlier gestations, though several indirect lines of evidence suggest that NO is likely to be important in the regulation of GI perfusion at mid-gestation and, indeed, that the role of NO at this time may be even more important than later in gestation. Gestational changes in umbilical-placental vessels suggest that the amount of NO released and its relaxant effect in vascular beds of the fetus may be more pronounced earlier in development(7), a possibility that is emphasized by the striking changes in major vessel caliber induced by altering NO synthesis in the very immature circulation of the rat fetus(5). The possibility that the regulatory role of NO in the GI circulation may be enhanced earlier in ontogeny is further supported by the greater NO-mediated intestinal vasodilation in newborn compared with older piglets(8,9). Supporting evidence for the concept that NO may be the dominant vasodilator early in development includes the observation that another important vasodilator, the neuropeptide CGRP, is poorly developed at mid-gestation and does not achieve maturity until the early postnatal period(10,11). Finally, NO appears to play a prominent role in maintaining flow at low perfusion pressures(12), an action which is likely to be of particular importance at the low arterial pressures present at mid-gestation(13).
Resolution of the role of NO in the maintenance of perfusion in the immature GI circulation has implications for understanding the pathogenesis of NEC. NEC has its highest incidence in the immature GI circulation(14) and compromised blood flow and oxygen transport to the intestine are prominent clinical findings in infants suffering NEC(15,16). Endogenous NO may be of critical importance for maintaining high levels of intestinal blood flow, particularly in the small intestine, which is most prone to NEC(6,17) and for preserving intestinal perfusion during hypoxia-ischemic insults that have been postulated to precipitate NEC(9).
The purpose of the present study was to test the hypothesis that NO plays a major role in the regulation of the intestinal circulation at mid-gestation(more powerful than later in development) that is critical to ensuring adequate blood flow and oxygenation of the immature GI tract. The role of NO in regulating GI hemodynamics at mid-gestation was assessed in studies of chronically instrumented fetal lambs before and after inhibition of NO synthase with the stereospecific inhibitor L-NNA. To test the hypothesis that NO has a greater regulatory role earlier in development, results from the mid-gestation fetus were compared with those obtained from late-gestation fetuses(6).
METHODS
All procedures and protocols used in these experiments were in accord with guidelines provided by the National Health and Medical Research Council of Australia and were approved by the Monash University Committee on Ethics in Animal Experimentation.
Surgical preparation. Eight Border-Leicester fetal lambs underwent surgery between 89 and 97 d of gestation (term = 147 d). After 24 h of fasting, general anesthesia was induced in pregnant ewes with 200 mg of i.v. propofol (Diprivan, ICI, Australia). The ewes were intubated and general anesthesia was maintained by positive pressure ventilation using 1-3% halothane, 30% oxygen, and the remainder nitrous oxide.
During surgery, maternal blood gases were monitored at regular intervals via a femoral arterial catheter. Under sterile conditions the fetal lamb's head, left forelimb, and upper thorax were delivered through a uterine incision. A left lateral thoracotomy was performed in the fourth interspace, and the fourth rib was removed to increase exposure of the heart and the pulmonary trunk. After incision of the pericardium, a polyvinyl catheter inserted into the left atrium and a 6- or 8-mm diameter ultrasonic flow transducer (Transonic Systems Inc., Ithaca, NY) was implanted around the main pulmonary trunk. A modified 18-gauge Teflon cannula connected to a polyvinyl catheter was inserted into the pulmonary trunk distal to the flow probe, and the pericardial incision over the left atrium was then closed. Nonocclusive polyvinyl catheters were advanced through the left axillary artery and vein into the brachiocephalic trunk and the superior vena cava, respectively.
The chest incision was closed and a wide bore catheter was sutured to the anterior chest wall for measurement of amniotic fluid pressure. Through a second uterine incision, both fetal groins were exposed, and catheters were inserted into a femoral artery bilaterally and a femoral vein, and advanced into the abdominal aorta and inferior vena cava, respectively.
The fetus was returned to the uterus, amniotic fluid losses were replaced with warm isotonic saline, antibiotics administered into the amniotic cavity(1 g of procaine penicillin, 1 g of dihydrostreptomycin sulfate), and the uterine incisions then closed. The catheters and flow transducer cable were exteriorized through a s.c. tunnel and protected in a pouch located above the ewe's right flank. Each day thereafter antibiotics were administered to the amniotic cavity, catheters were flushed, and the dead space filled with heparinized saline (1000 U/mL).
Experimental protocol. After 72-h recovery from surgery, the ewe was brought to the laboratory and placed in a study cage with free access to food and water. Pulmonary trunk flow was measured continuously by an ultrasonic volume flowmeter (model T208, Transonic Systems). Abdominal aortic blood pressure and amniotic fluid pressure were measured by pressure transducers (model CDX-111, COBE, Lakewood, CO). Hemodynamic variables were displayed on a Neotrace 800ZF chart recorder (Neomedix Systems, Sydney, Australia), recorded on computer at a sampling rate of 200 Hz with an analog to digital converter, and analyzed off-line with interactive software.
After recording of baseline hemodynamics and blood gas variables, ventricular outputs and regional blood flows were measured with radioactive microspheres. NOS was then inhibited with the specific NOS inhibitor L-NNA(Sigma Chemical Co., St. Louis, MO). L-NNA was dissolved in saline to a concentration of 5 mg/mL and infused into the inferior vena caval catheter at a rate of 0.68 mL/min to achieve cumulative doses of approximately 10 and 25 mg/kg of estimated fetal body weight. After a period of stabilization, hemodynamic, blood gas, and blood flow measurements were repeated at each L-NNA dose. On completing the experiment, the ewe and fetus were killed with an overdose of pentobarbitone sodium (150 mg/kg), and an autopsy was performed on the fetus to verify catheter placement.
Blood flow and resistance measurements. Blood flows were measured with radioactive microspheres (141Ce, 113Sn,85 Sr, 95Nb, and 46Sc, New England Nuclear, Boston, MA) using the reference sample technique(18). After ultrasonication, approximately one million 15-µm diameter microspheres were injected per microsphere label. At baseline and at an L-NNA dose of 25 mg/kg, two different microsphere labels were injected simultaneously, one into the left atrium to measure LV output and the other into the superior vena cava to measure RV output(19), whereas reference samples were drawn simultaneously from the pulmonary trunk, axillary artery, and descending aorta. At an L-NNA dose of 10 mg/kg, LV output was obtained with a single microsphere label injected into the left atrium, whereas reference samples were withdrawn from the axillary artery and descending aorta. Reference samples were withdrawn at a rate of 2.06 ml·min-1 using a mechanical pump (Harvard Apparatus, South Natick, MA). Reference sample withdrawal was commenced 10 s before microsphere injection and terminated 1.5 min after its completion. Fetal blood withdrawn during reference sampling was simultaneously replaced with maternal blood.
At the end of the experiment, the GI tract was totally removed, fixed in 10% formalin for a period of 1 wk, and then dissected into its major anatomical segments, namely the stomach, duodenum, jejunum, ileum, cecum, colon, and rectum. Each GI segment was blotted dry, weighed, and packed into plastic counting vials to a height of ≤ 2 cm. Radioactivity in tissue and reference blood samples was counted using a well type scintillation counter(model 1282 Compugamma, LKB-Wallac, Turku, Finland), with windows set at the appropriate energy levels.
Blood flows were calculated from the general relation Qtissue = [Qreference ×Rtissue]/Rreference, where Q is flow (mL/min) and R is radioactivity (counts/min). Ventricular outputs were calculated using an adaptation of this general relation for the fetal circulation as previously described(19). Thus, fetal LV output (QLV) was calculated as [Qreferennce ×RLA]/RLA≫CA, where RLA is the radioactivity of the label injected into the left atrial cavity and RLA≫CA is the radioactivity of the same label in the carotid arterial reference sample. Fetal RV output(QRV) was equal to [Qreference ×RRV]/RV≫PT, where RRV is the radioactivity of venous label passing into the right ventricle, calculated as the injected radioactivity of this label minus that portion crossing the foramen ovale to appear in the LV output, and RV≫PT is the radioactivity of the venous label in the pulmonary reference sample(19). RV output at an L-NNA dose of 10 mg/kg was obtained by interpolation from the measured pulmonary trunk flow, using baseline and 25 mg/kg L-NNA measurements of pulmonary trunk obtained with the ultrasonic flow probe and RV output obtained with radioactive microspheres. Global and regional GI vascular resistance(RGI, mm Hg·mL-1·min-1·100 g-1) was calculated as MAP/QGI, where MAP is mean abdominal aortic blood pressure and QGI is the appropriate GI blood flow.
Blood gas measurements. Blood gas tensions and pH corrected to 40°C (Radiometer ABL 500 blood gas analyzer, Radiometer, Copenhagen, Denmark), as well as Hb concentration ([Hb]) and Hb oxygen saturation(Sao2) (Radiometer OSM-2 hemoximeter) were measured in abdominal aortic blood. Abdominal aortic oxygen content (CAo2, mL/dL) was calculated as (0.0136 × [Hb] × SaO2) + (0.003 × PO2) and GI oxygen delivery (DO2, mL O2·min-1·100 g-1) was calculated as QGI × CAO2.
Statistics. All data are presented as mean ± SE. Data were compared with one-way and two-way repeated measures ANOVA and a post hoc Newmann-Keuls test as appropriate. All analyses were performed using the computer statistical package Statistica (StatSoft), and p < 0.05 was considered significant.
RESULTS
Systemic hemodynamics and blood gas changes. Baseline hemodynamics (Table 1) and blood gases(Table 2) in the mid-gestation fetal lambs were comparable to those reported in previous studies(13,20,21). After administration of 10 mg/kg L-NNA, arterial pressure rose by 13 ± 3 mm Hg (p < 0.01), the combined LV and RV output (CVO) fell by 145 ± 25 mL·min-1·kg-1 (p < 0.001), whereas heart rate was unchanged. At 25 mg/kg L-NNA, the CVO fell by a further 105 ± 39 mL·min-1·kg-1(p < 0.01), but MAP and heart rate were not significantly different from 10 mg/kg L-NNA (Table 1). Apart from an increase in Hb concentration (p < 0.001), blood gas variables were unchanged between baseline and 10 mg/kg L-NNA. However, the dose of 25 mg/kg L-NNA was associated with decreases in pH (p < 0.05) and SaO2 (p < 0.05), a rise in PCO2 (p< 0.05) and a further increase in Hb concentration (p < 0.001), but no change in arterial oxygen content (Table 2).
GI blood flow responses. Under baseline conditions, average GI blood flow was 93 ± 7 mL·min-1·100 g-1. Moreover, a substantive differential pattern of regional blood flow was evident along the GI tract with stomach and small intestinal and large intestinal blood flows being significantly different from one another(p < 0.001) and the highest flow occurring in the small intestine (Table 3).
After the infusion of 10 mg/kg L-NNA, average GI blood flow decreased to 41 ± 8 mL·min-1·100 g-1 (p< 0.001). Significant flow reductions occurred in all regions of the GI tract (p < 0.01 to 0.001), and blood flow to the stomach was still lower than to either the small or large intestine (Table 3). However, the extent of the flow reduction in the small intestine (59± 12 mL·min-1·100 g-1) was more pronounced than in the large intestine (27 ± 7 mL·min-1·100 g-1, p < 0.01) and, as a result, small and large intestinal flows were not significantly different from one another at 10 mg/kg L-NNA. Neither average GI blood flow nor regional blood flows to the stomach, small intestine or large intestine changed significantly between 10 and 25 mg/kg L-NNA (Table 3).
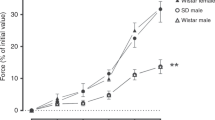
As illustrated in Fig. 1, similar degrees of blood flow reduction occurred at 10 mg/kg L-NNA in the duodenal (46 ± 16 mL·min-1·100 g-1), jejunal (61 ± 17 mL·min-1·100 g-1), and ileal (58 ± 10 mL·min-1·100 g-1) portions of the small intestine. Likewise, blood flow decrements in the cecum (28 ± 8 mL·min-1·100 g-1), colon (28 ± 9 mL·min-1·100 g-1), and rectum (20 ± 8 mL·min-1·100 g-1) did not differ significantly from one another. No further change in blood flow to regions of the small and large intestine occurred at 25 mg/kg L-NNA, apart from a further reduction in blood flow to the rectum (p< 0.05;Fig 1).
GI vascular resistance. Under baseline conditions, average GI vascular resistance was 0.41 ± 0.06 mm Hg·mL-1·min-1·100 g-1. In similar manner to blood flow, a substantial differential pattern of regional vascular resistance was evident along the GI tract, with small and large intestinal vascular resistances being significantly different from the stomach (p < 0.001), but not from one another(Fig. 2).
Vascular resistance (R) of stomach, small intestine, and large intestine (A) and regional vascular resistance (B) under baseline conditions (open bars) and after L-NNA infusion at 10 mg/kg i.v. (solid bars) and 25 mg/kg i.v. (hatched bars). Values are means ± SE; n = 8 fetal lambs. *p < 0.01 vs baseline; †p < 0.05 vs L-NNA (10 mg/kg).
In conjunction with the blood flow changes, vascular resistance in all major regions of the GI tract increased significantly after 10 mg/kg L-NNA(p < 0.01), with increments of 181 ± 28% in the stomach, 194 ± 37% in the small intestine and 120 ± 25% in the large intestine (Fig. 2A). No further change in vascular resistance occurred at 25 mg/kg L-NNA.
Regional vascular resistance increased dramatically in all segments of the small intestine at 10 mg/kg L-NNA, with increments ranging from 174 ± 44% for the duodenum to 199 ± 44% for the jejunum (Fig. 2B). Increases in regional vascular resistance were less marked for the large intestine, ranging from 92 ± 24% for the rectum to 166 ± 49% for the colon. No significant change in regional vascular resistances occurred between 10 and 25 mg/kg L-NNA, apart from a further small rise within the rectum (p < 0.05;Fig. 2B).
GI oxygen delivery. Under baseline conditions, average GI oxygen delivery was 5.0 ± 0.4 mL O2·min-1·100 g-1. A substantial differential pattern of regional oxygen delivery was evident along the GI tract with stomach and small and large intestinal oxygen delivery being significantly different from one another (p < 0.001) and the highest oxygen delivery occurring in the small intestine (Fig. 3A). After 10 mg/kg L-NNA, oxygen delivery decreased by 44 ± 3% to the stomach (p < 0.001), 44 ± 4% to the small intestine (p< 0.001), and 26 ± 10% to the large intestine (p < 0.05). Oxygen delivery to the small and large intestine did not change significantly between 10 and 25 mg/kg L-NNA, but fell further by 22% in the stomach(p < 0.05; Fig. 3A).
Oxygen delivery of stomach, small intestine, and large intestine (A) and regional oxygen delivery(B) under baseline conditions (open bars) and after L-NNA infusion at 10 mg/kg i.v. (solid bars) and 25 mg/kg i.v.(hatched bars). Values are means ± SE; n = 8 fetal lambs. Note that oxygen delivery to the small intestine significantly exceeded that to the large intestine in the baseline conditions, but not after L-NNA infusion. **p < 0.001; *p < 0.05vs baseline; †p < 0.05 vs L-NNA (10 mg/kg).
Regional oxygen delivery decreased significantly in all segments of the small intestine after 10 mg/kg L-NNA, amounting to reductions of 37 ± 6% in the duodenum (p < 0.001), 43 ± 5% in the jejunum by (p < 0.001) and 45 ± 3% in the ileum (p< 0.001). Regional oxygen delivery also fell in the cecum (33 ± 8%; p < 0.01) and colon (41 ± 4%, p < 0.05), but did not change significantly in the rectum (Fig. 3B). No further change in regional oxygen delivery to the small and large intestine occurred between 10 and 25 mg/kg L-NNA, apart from the rectum which was 38 ± 12% lower than baseline (p < 0.05).
DISCUSSION
NO has been shown to exert a powerful vasodilatory influence in GI circulation of mature animals(22–24). However, it was not until recently that endogenous NO was shown to be a significant contributor to the modulation of vascular tone in the GI circulation of late-gestation fetal lambs(6). In this study, we have extended our investigation to the mid-gestation fetus, and shown that NOS substantially affects GI vascular tone at this age. Moreover, our data indicate that a characteristic in utero pattern of basal intestinal blood flow favoring the small intestine is dramatically altered by the administration of L-NNA. As we elaborate below, our results suggest that NO plays a substantially greater role in the regulation of intestinal vascular tone in the mid-gestation fetus than it does later in gestation.
The baseline values we obtained for MAP, blood gas values, and CVO for the mid-gestation fetal sheep are consistent with values published in other studies(13,20). In accord with previously published gestational data(21), average blood flow was less at mid-gestation (93 mL·min-1·100 g-1) than at late-gestation (136 mL·min-1·100 g-1)(6). Values of blood flow in different regions of the GI tract ranged between 39 and 134 mL·min-1·100 g-1, levels that are comparable to those previously reported for fetal lambs at this stage of gestation(13,21). In a manner similar to the late-gestation fetal sheep(6), the mid-gestation fetus also displayed a differential pattern of blood flow between the small and large intestine, with much higher blood flows directed to the small intestine (Table 3).
An important feature of our experimental design was to evaluate the response to incremental doses of L-NNA, as it is known that specific effects of NOS inhibition in the mature circulation are dose related(24). In a manner similar to the late-gestation fetus, some of the systemic variables in the mid-gestation fetus, specifically arterial blood gases, pH, and Hb showed dose-related changes. Although changes in SaO2 and PCO2 which occurred after L-NNA were statistically significant, they were small in magnitude, so that values remained within normal ranges reported in other studies(13,20). pH at 10 mg/kg L-NNA was within the normal range but a mild acidosis was evident at 25 mg/kg L-NNA. This was most likely a consequence of significantly reduced placental blood flow causing reduced oxygen transport to the fetus, or of increased systemic vascular resistance leading to inadequate oxygen delivery. Hb rose progressively with increasing L-NNA concentration, probably reflecting increases in vascular permeability and promotion of plasma leakage that accompanies NOS inhibition(25,26).
Although basal arterial blood pressure at mid-gestation was lower than at late-gestation(6), the increase in blood pressure at both the 10 and 25 mg/kg doses of L-NNA were similar to those observed in late-gestation fetuses(6). That no accompanying bradycardia occurred after NOS inhibition in mid-gestation animals is probably related to the immaturity of vagal effects upon heart rate at this early stage of fetal development(27). One explanation for the progressive decrease in CVO after L-NNA is that the substantial increase in blood pressure associated with NOS inhibition may have exceeded the compensatory capacity of the immature fetal heart to maintain output in the face of the increased afterload. An alternative factor which may have contributed to the decreased CVO was a reduction in circulating blood volume accompanying the hemoconcentration observed after NOS inhibition(6,26).
The major finding of our study was that NOS inhibition in the mid-gestation fetus was associated with a substantial decrease in GI blood flow. As in the late-gestation fetal lambs(6), responses to NOS inhibition achieved steady state in the mid-gestational GI circulation between the 10 and 25 mg/kg doses of L-NNA (Table 3). In the regional GI vascular beds, the substantial blood flow reduction evoked by L-NNA largely abolished the basal differential pattern of higher blood flow in the small intestine compared with that in the large intestine. Particularly remarkable was the blood flow reduction evident in segments of the small intestine, where an average blood flow fell by 73 mL·min-1·100 g-1 overall. This flow reduction was twice that of the large intestine overall(Table 3), and in specific segments was much greater in magnitude than across the segments of the large intestine(Fig. 1). By contrast, in the late-gestation fetus, the differential pattern of blood flow between the small and large intestine was attenuated, but not entirely abolished by NOS inhibition(6).
We ascribe the powerful vasoconstriction in the immature GI circulation directly to the loss of the vasodilating effect of NO. No baroreflex-induced vasoconstriction would be expected under the conditions of our study as MAP rose, and as this would promote vasodilation rather than vasoconstriction. In any case, reflex responses would be expected to produce less vasoconstriction in the immature circulation(5,28), not greater vasoconstriction as we observed. It is also unlikely that the GI blood flow changes accompanying NOS inhibition in this study were related to the induction of a migratory motor complex(29), a pattern of electrical and contractile activity that is associated with cyclical increases in intestinal blood flow in the mature animal(30), as the migratory motor complex is absent or quiescent at mid-gestation(31).
Comparison of blood flow decreases with previously published data from late-gestation fetuses(6) indicates that percentage decreases in blood flow and increase in vascular resistance were significantly greater at mid-gestation (Fig. 4). These observations suggest that endogenous NO exerts a much greater influence on the regulation of GI vascular tone at this early stage of gestation than it does later in fetal life. That NO should have a prominent role in the mid-gestation GI circulation of the lamb is supported by recent evidence that NOS is critical in maintaining the caliber of the ductus arteriosus and great vessels of the immature fetal rat(5). Interestingly, our findings complement those in the postnatal intestinal circulation(8,32), where the role of NO in promoting vasodilation is enhanced at the younger age of 3 d compared with 35 d.
Illustrations of the substantially greater effects of L-NNA infusion upon the GI circulation of the mid-gestation fetal lamb compared with the late-gestation fetal lamb. (A) Decrease in blood flow and (B) increase in vascular resistance after L-NNA infusion (25 mg/kg i.v.) in stomach, small intestine and large intestine of mid-gestation (open bars, n = 8) and late-gestation (solid bars, n = 11) fetal lambs. Values are means ± SE; **p < 0.001; *p < 0.05vs mid-gestation.
A possible explanation for the dominant vasodilator role of NO in the mid-gestation GI circulation may lie in a different pattern of interaction with other vasoactive influences(33–36) determining the balance of vascular tone in the immature circulation. Specifically, the vasodilatory effects of NO may operate in the presence of limited opposing vasoconstricting effects of the sympathetic nervous system which is poorly developed at this age(20,27,28,37). Importantly, when NO production is inhibited in the more mature intestinal circulation, there is a compensatory vasodilation effected by release of the neuropeptide CGRP(11,38–41). Although present by mid-gestation(10) CGRP does not attain peak activity until the early neonatal period(11,39). This suggests that NO may be the dominant vasodilator at mid-gestation, with CGRP assuming a greater role as the neonatal period is approached. Whether compensatory vasodilation due to other factors is also less pronounced in the GI circulation at mid-gestation remains to be determined; prostaglandins, which support NO-induced vasodilation in mature mesenteric vessels(42), may also contribute to vasodilation in the immature circulation, though perhaps to a lesser extent than NO(4).
In the present study, resting oxygen delivery to the GI circulation (5.0± 0.4 mL O2·min-1·100 g-1) was approximately half that of the near term fetus (8.6 ± 1.0 mL O2·min-1·100 g-1), presumably reflecting lesser requirements for growth and metabolic demand at mid-gestation. After NOS inhibition in the mid-gestation fetus, oxygen delivery was substantially decreased, particularly in the small intestine (Fig. 3), where the basal pattern of higher oxygen delivery compared with the large intestine was completely abolished. Compared with mid-gestation, changes in the regional pattern of GI O2 delivery in the late-gestation were less pronounced and confined to the small intestine, with O2 delivery to some segments of the large intestine being unaffected by L-NNA infusion(6). The late-gestation fetal GI circulation is more sensitive to hypoxia-ischemia than the neonate(43). In this respect, the mid-gestation GI circulation may be even more susceptible than the late-gestation GI circulation to hypoxia-ischemic insult because of the greater role of NO-mediated vasodilation in maintaining basal flow, and the sensitivity of NO production to hypoxia-ischemic insult(9).
The substantial dependence upon NO production of the immature ruminant GI circulation has important implications for the pathogenesis of NEC, which has a high incidence in premature infants. Although the human GI tract differs anatomically and physiologically from that of the ruminant, both species have high blood flow levels in the small intestine(44,45) that may be dependent upon NO production. As our study shows, endogenous NO is in large measure responsible for maintaining high levels of blood flow in the immature GI tract, particularly in the small intestine, a site at which NEC occurs at high frequency(17). Endothelium dysfunction resulting from damage by factors such as hypoxia-ischemia, may act as trigger events leading first to disruption of the key vasodilating role of NO and eventually to significant intestinal necrosis(9).
In summary, the inhibition of endogenous NO in the midgestation fetal sheep, results in substantial blood flow reductions across all segments of the GI tract. These effects are substantially greater at mid-gestation than later in fetal development and after birth. We speculate that if the synthesis and activity of NO were to be impaired, the immature GI circulation would be particularly vulnerable to ischemic insult.
Abbreviations
- NO:
-
nitric oxide
- NOS:
-
nitric oxide synthase
- GI:
-
gastrointestinal
- MAP:
-
mean arterial pressure
- L-NNA:
-
Nω-nitro-L-arginine
- NEC:
-
necrotizing enterocolitis
- >LV:
-
left ventricular
- RV:
-
right ventricular
- CVO:
-
combined ventricular output
- SaO2:
-
arterial oxygen saturation
- CAO2:
-
aortic oxygen content
References
Pawlik WW, Gustaw P, Thor P, Sendur R, Czarnobilski K, Hottenstein OD, Konturek SJ 1993 Microcirculatory and motor effects of endogenous nitric oxide in the rat gut. J Physiol Pharmacol 44: 139–146.
Yang D, Lang U, Greenberg SG, Myatt L, Clark KE 1996 Elevation of nitrate levels in pregnant ewes and their fetuses. Am J Obstet Gynecol 174: 573–575.
Chang J, Roman C, Heymann MA 1992 Effect of endothelium-derived relaxing factor inhibition on the umbilical-placental circulation in fetal lambs in utero. Am J Obstet Gynecol 166: 727–734.
Chaudhuri G, Cuevas J, Buga GM, Ignarro LJ 1993 NO is more important than PGI2 in maintaining low vascular tone in feto-placental vessels. Am J Physiol 265: H2036 H2043
Bustamante SA, Pang Y, Romero S, Pierce MR, Voelker CA, Thompson JH, Sandoval M, Liu X, Miller MJS 1996 Inducible nitric oxide synthase and the regulation of central vessel caliber in the fetal rat. Circulation 94: 1948–1953.
Fan WQ, Smolich JJ, Wild J, Yu VYH, Walker AM 1996 Nitric oxide modulates regional blood flow differences in the fetal gastrointestinal tract. Am J Physiol 271:G598–G604.
Izumi H, Garfield RE, Makino Y, Shirakawa K, Itoh T 1994 Gestational changes in endothelium-dependent vasorelaxation in human umbilical artery. Am J Obstet Gynecol 170: 236–245.
Nankervis CA, Nowicki PT 1995 Role of nitric oxide in regulation of vascular resistance in postnatal intestine. Am J Physiol 268:G949–G958.
Nowicki PT 1996 The effects of ischemia-reperfusion on endothelial cell function in postnatal intestine. Pediatr Res 39: 267–274.
Barajas L, Liu L, Nishiyama C 1991 Prenatal and postnatal development of the CGRP-immunoreactive innervation in the rat kidney. Neurosci Lett 133: 219–224.
Whittle BJR, Tepperman BL 1991 Role of the endogenous vasoactive mediators, nitric oxide, prostanoids and sensory neuropeptides in the regulation of gastric blood flow and mucosal integrity. In: Gardiner A, O'Brien PE (eds) Mechanisms of Injury, Protection and Repair of the Upper Gastrointestinal Tract. John Wiley & Sons, Chichester, UK, 127–137.
Smith TP, Canty JM 1993 Modulation of coronary autoregulatory responses to nitric oxide. Evidence for flow-dependent resistance adjustments in conscious dogs. Circ Res 73: 232–240.
Iwamoto HS, Kaufman T, Keil LC, Rudolph AM 1989 Responses to acute hypoxemia in fetal sheep at 0.6-0.7 gestation. Am J Physiol 256:H613–H620.
Kliegman RM 1990 Neonatal necrotizing enterocolitis: bridging the basic science with the clinical disease. J Pediatr 117: 833–835.
Hopkins GB, Gould VE, Stevenson JK, Oliver TK 1970 Necrotizing enterocolitis in preterm infants: a clinical and pathological evaluation of autopsy material. Am J Dis Child 120: 229–232.
Tait RA, Kealy WF 1979 Neonatal necrotizing enterocolitis. J Clin Pathol 32: 1090–1099.
Santulli TV, Schullinger JN, Heird WC, Gongaware RD, Wigger J, Barlow B, Blanc WA, Berdon WE 1975 Acute necrotizing enterocolitis in infancy: a review of 64 cases. Pediatrics 55: 376–387.
Heymann MA, Payne BD, Hoffman JIE, Rudolph AM 1977 Blood flow measurements with radionuclide-labeled particles. Prog Cardiovasc Dis 20: 55–79.
Smolich JJ, Woods RL 1995 Regional systemic ANP differences in fetal lambs: role of coronary sinus outflow distribution. Am J Physiol 269:H669–H675.
Iwamoto HS, Stucky E, Roman CM 1991 Effect of graded umbilical cord compression in fetal sheep at 0.6-0.7 gestation. Am J Physiol 261: H1268 H1274
Rudolph AM, Heymann MA 1970 Circulatory changes during growth in the fetal lamb. Circ Res 26: 289–299.
Greenblatt EP, Loeb AL, Longnecker DE 1993 Marked regional heterogeneity in the magnitude of EDRF/NO-mediated vascular tone in awake rats. J Cardiovasc Pharmacol 21: 235–240.
Loeb AL, Longnecker DE 1992 Inhibition of endothelium-derived relaxing factor-dependent circulatory control in intact rats. Am J Physiol 262:H1494–H1500.
Pique JM, Whittle BJR, Esplugues JV 1989 The vasodilator role of endogenous nitric oxide in the rat gastric microcirculation. Eur J Pharmacol 174: 293–296.
Kubes P 1992 Nitric oxide modulates epithelial permeability in the feline small intestine. Am J Physiol 262:G1138–G1142.
Kubes P, Granger DN 1992 Nitric oxide modulates microvascular permeability. Am J Physiol 262:H611–H615.
Walker AM, Cannata JP, Dowling MH, Ritchie BC, Maloney JE 1979 Age-dependent pattern of autonomic heart rate control during hypoxia in fetal and newborn lambs. Biol Neonate 25: 198–208.
Walker D 1994 Development of the autonomic nervous system, including adrenochromaffin tissue. In: Thorburn GD, Harding R (eds) Textbook of Fetal Physiology. Oxford University Press, Oxford, UK, 287–300.
Rodriguez-Membrilla V, Martinez V, Jimenez M, Gonalons E, Vergara P 1995 Is nitric oxide the final mediator regulating the migrating myoelectric complex cycle? Am J Physiol 268:G207–G214.
Fioramonti J, Bueno L 1984 Relation between intestinal motility and mesenteric blood flow in the conscious dog. Am J Physiol 246:G108–G113.
Bueno L, Ruckebusch Y 1979 Perinatal development of intestinal myoelectrical activity in dogs and sheep. Am J Physiol 237:E61–E67.
Nowicki PT, Nankervis CA 1994 The role of the circulation in the pathogenesis of necrotizing enterocolitis. Clin Perinatol 21: 219–234.
Gryglewski RJ 1995 Interactions between endothelial mediators. Pharmacol Toxicol 77: 1–9.
Modin A, Weitzberg E, Lundberg JM 1994 Nitric oxide regulates peptide release from parasympathetic nerves and vascular reactivity to vasoactive intestinal polypeptide in vivo. Eur J Pharmacol 261: 185–197.
Shimokawa H, Takeshita A 1995 Endothelium-dependent regulation of the cardiovascular system. Intern Med 34: 939–946.
Yamamoto R, Asada Y, Yuhi T, Yanagita T, Niina H, Sumiyoshi A 1994 Functional relation between nitric oxide and noradrenaline for the modulation of vascular tone in rat mesenteric vasculature. Naunyn Schmiedebergs Arch Pharmacol 349: 362–366.
Lebowitz EA, Novick JS, Rudolph AM 1972 Development of myocardial sympathetic innervation in the fetal lamb. Pediatr Res 6: 887–893.
Chen RYZ, Guth PH 1995 Interaction of endogenous nitric oxide and CGRP in sensory neuron-induced gastric vasodilation. Am J Physiol 268:G791–G796.
Dhall U, Cowen T, Haven AJ, Burnstock G 1986 Perivascular noradrenergic and peptide-containing nerves show different patterns of changes during development and ageing in the guinea-pig. J Auton Nerv Syst 16: 109–126.
Saito A 1994 Vasodilator nerves. Yakugaku Zasshi 114: 765–774.
Zygmunt PM, Ryman T, Högestätt ED 1995 Regional differences in endothelium-dependent relaxation in the rat: contribution of nitric oxide and nitric oxide-independent mechanisms. Acta Physiol Scand 155: 257–266.
Dezsi L, Dornyei G, Szentivanyi MJ, Tulassay T, Monos E 1997 Somatostatin induces vasodilation in the cat mesenteric artery via endothelium-derived nitric oxide and prostaglandins. Pflugers Arch 433: 536–538.
Edelstone DI, Holzman IR 1984 Regulation of perinatal intestinal oxygenation. Semin Perinatol 8: 226–233.
Hulten L, Jodal M, Lindhagen J, Lundgren O 1976 Blood flow in the small intestine of the cat and man as analysed by an inert gas washout technique. Gastroenterology 70: 45–51.
Hulten L, Jodal M, Lindhagen J, Lundgren O 1976 Colonic blood flow in cat and man as analysed by an inert gas washout technique. Gastroenterology 70: 36–44.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fan, W., Smolich, J., Wild, J. et al. Major Vasodilator Role for Nitric Oxide in the Gastrointestinal Circulation of the Mid-Gestation Fetal Lamb. Pediatr Res 44, 344–350 (1998). https://doi.org/10.1203/00006450-199809000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199809000-00013