Abstract
Fetal hepatic amino acid metabolism has unique features in comparison to postnatal life. Thus, it seemed likely that this metabolism might be changed by the endocrine changes which precede birth. To explore the changes in placental and fetal carbohydrate and amino acid metabolism that occur during parturition, labor was induced in six ewes at 131 ± 1 d gestation with a fetal infusion of dexamethasone. For purpose of chemical analysis, blood was withdrawn before and approximately 3 and 25 h from the start of the infusion from maternal arterial, uterine venous, umbilical venous, fetal arterial, and left hepatic venous catheters. Fetal oxygenation remained normal. At 25 h, both fetal and maternal arterial plasma glucose concentrations increased(p < 0.01 and p < 0.02, respectively) and umbilical glucose uptake decreased (p < 0.05). Fetal glutamate showed a significant reduction in its hepatic output (p < 0.05) with a concomitant reduction in fetal arterial plasma concentration (p < 0.05) and placental uptake (p < 0.01). Fetal plasma concentrations of several other amino acids were markedly increased. The reduction in placental glutamate uptake was temporally associated with a decline in progesterone release by the pregnant uterus. These data suggest the hypothesis that glutamate plays a role in integrating the complex changes in placental and fetal hepatic metabolism that occur during parturition.
Similar content being viewed by others
Main
Over the last few years, a number of studies have clearly demonstrated that the ovine placenta transports gluconeogenic amino acids such as glutamine, alanine, and glycine into the fetus at rates which exceed their rates of accretion in the fetal tissues(1–5). The fetal liver utilizes these amino acids, not for glucose production, but for the production of glutamate and serine(3, 4, 6–8) which are then released into the fetal hepatic circulation and become metabolic substrates for other organs. A large fraction of the glutamate released from the fetal liver is taken up by the placenta and oxidized(9).
Near the end of pregnancy, the activity of fetal hepatic gluconeogenic enzymes increases, and the fetal liver accumulates glycogen at a rapid rate(10). These events coincide with increased cortisol secretion by the fetal adrenals and can be induced prematurely by the fetal infusion of cortisol or other glucocorticoids, such as dexamethasone(11). In sheep, the fetal infusion of glucocorticoids is sufficient to trigger premature labor(12–14). There have been no previous studies which have examined fetal hepatic metabolism during normal or dexamethasone-induced parturition.
The above information suggests that, during parturition, there may be important changes in fetal hepatic and placental exchange and metabolism of gluconeogenic amino acids. Specifically, it suggests the hypothesis that glucocorticoids stimulate the diversion of gluconeogenic amino acid carbon from fetal hepatic glutamate and serine production to glycogen synthesis. A consequence of this would then be a decrease in the availability of fetal plasma glutamate for placental metabolism.
The present study was designed to test this hypothesis by exploring the changes in fetal amino acid uptake and release across the fetal hepatic and umbilical circulations that occur in response to a fetal infusion of dexamethasone. The study was carried out in a fetal sheep preparation with chronically implanted catheters for the sampling of maternal arterial, uterine venous, umbilical arterial, umbilical venous and fetal left hepatic venous blood.
METHODS
Surgery and animal care. Six Columbia-Rambouillet ewes with singleton time-dated pregnancies were used for this study. Ewes were fasted for 1-2 d before surgery with free access to water. They were operated at 120± 2 d of gestation under a combination of general pentobarbital sodium anesthesia (10 mg/kg initial dose) and spinal anesthesia (6 mg of Pontocaine, Winthrop). Polyvinyl catheters (1.4 mm OD) were inserted into each of the two uterine veins, with the catheter tip located 5 cm downstream from the level of the ovaries, in the maternal left femoral artery, a fetal pedal artery, a fetal brachial vein and the amniotic cavity. The common umbilical vein was catheterized using a technique described previously(26). The fetal left hepatic vein was catheterized via a right thoracotomy(7). A 15-gauge Angiocath (Becton Dickinson) was inserted in the thoracic inferior vena cava above the diaphragm and was used to guide the polyvinyl catheter into the left hepatic vein. The Angiocath was withdrawn, and the polyvinyl catheter was secured to the vena cava with a purse-string ligature. It was also secured to the fetal skin at the point of exit. The position of all sampling catheters was verified at autopsy. All catheters were tunneled s.c. through a flank incision and kept within a plastic pouch attached to the sheep's skin. All ewes recovered promptly from surgery. They were standing in their pen within 6 h and resumed normal food intake within 3 d. Ampicillin (500 mg) and gentamicin (80 mg) were given iintramuscularly to each ewe at the time of surgery. In addition, ampicillin (500 mg) was injected into the amniotic fluid at the end of the surgery and daily for the first 4 postoperative days. The animals were fedad libitum with an alfalfa pellet diet. Catheters were flushed daily with heparinized saline (35 U heparin/mL). The protocol for this study was approved by the University of Colorado Institutional Review Board for animal research.
Study design. The animals were allowed 4-10 d to recover from surgery before study. The induction of parturition started at 131 ± 1 d of gestation with a bolus of 0.2 mg of dexamethasone given into the fetal brachial venous catheter, followed by a continuous infusion at 0.07 mg·h-1. This dexamethasone dose has been used previously for parturition studies in our laboratory(14, 23). Blood was drawn simultaneously from the umbilical vein, fetal left hepatic vein, hind limb fetal artery, uterine artery, and uterine vein before and during the 50 h of the infusion. Four complete sets of samples were obtained at 20-min intervals from every fetus only during the control period and at 3(range 2-6 h) and 25 (22-28 h) h after the start of the infusion. Each set required 1.4 mL of blood from each fetal vessel for total of 4.2 mL of fetal blood per set. At the end of the four samplings in each of the three time periods, the fetus was transfused with 16 mL of fetal blood from a donor fetus. Fetal samples were analyzed for blood O2 content and plasma concentrations of lactate, glucose, and amino acids. Maternal blood samples from the uterine vein and maternal artery were also analyzed for progesterone.
Analytical methods. Blood O2 content was calculated from the Hb content and O2 saturation measured spectrophotometrically(OSM-3, Radiometer, Copenhagen, Denmark). Because glucose and lactate are the two carbohydrates delivered to the fetal circulation in significant amounts, plasma glucose and lactate concentrations were measured in duplicate by a glucose/lactate analyzer (YSI model 2700 Select and YSI Dual Standard). Within 5 min from collection, plasma samples for amino acid concentrations were frozen at -70°C until analysis. On the day of analysis, the samples were thawed quickly and deproteinized with 15% sulfosalicylic acid containing 0.3μmol·L-1 norleucine as an internal standard. The pH was adjusted to 2.2 with 1.5 N LiOH. After centrifugation, the supernatant was analyzed with a Dionex HPLC amino acid analyzer, (Dionix Corp, Sunnyvale, Calif). The same HPLC column was used for all samples from an individual animal. Reproducibility within the same column had a mean value of ± 2%. Samples from all vessels drawn simultaneously were loaded to run within 12 h. Amino acid concentrations were measured after reaction with ninhydrin at 570 nM wavelength except proline, and glutamate that were measured at 440 nM wavelength. This technique increases the sensitivity for detecting low plasma glutamate concentrations in the presence of high glutamine concentrations by increasing the glutamate/glutamine absorbance ratio (Fig. 1). Blood (0.5 mL) for progesterone determination was collected in syringes containing EDTA and centrifuged. The plasma was frozen at -70°C for later RIA of duplicate aliquots using the Coat-A-Count Progesterone RIA method of Diagnostic Product Corporation, Los Angeles, CA.
Calculations and statistical analysis. Net fetal uptakes of metabolic substrates via the umbilical circulation were normalized for fetal O2 uptake and expressed as fetal substrate/O2 uptake molar ratios according to the equation: where (Δ substrate)v-a is the umbilical venous-arterial blood molar concentration difference of the substrate and (Δ O2)v-a is the umbilical venous-arterial molar concentration difference of blood O2 content. Because net glutamate flux is from the fetus into the placenta(9), the equation calculates a“negative” fetal glutamate uptake, i.e. placental uptake of fetal glutamate.

The molar ratios of fetal hepatic substrate/O2 uptake were estimated according to the equation: where (Δ substrate)v-h and (Δ O2)v-h are the molar concentration differences between umbilical venous and fetal left hepatic venous blood for the substrate and for O2, respectively. This estimate is based on the knowledge that the left lobe of the fetal liver is perfused almost exclusively by umbilical venous blood(15). The contribution of portal venous blood to left hepatic blood flow is virtually zero and fetal arterial blood contributes approximately 10% of the total flow(15). Because glutamate and serine exit from the fetal liver, Equation 2 calculates negative uptakes(i.e. hepatic release) for these substrates.

To calculate substrate/O2 uptake ratios, the plasma concentrations of glucose and glutamate were converted to blood concentrations of exchangeable substrate using previously established formulas. For glucose:Equation (3) where PG is plasma glucose(mg·dL-1) and H is the fractional hematocrit. This equation was derived from paired measurements of blood and plasma glucose(25). Equation (4)


Equation 4 is based on the finding that the exchange of glutamate between blood and tissues is limited to the plasma compartment(9). Serine concentration differences were assumed to be equal in plasma and whole blood(4).
Net progesterone output by the pregnant uterus was normalized for uterine O2 uptake, using the equation: where (Δ progesterone)V-A is the molar concentration difference of plasma progesterone between uterine venous and arterial blood, and (Δ O2)A-V is the molar concentration difference of O2 between uterine arterial and venous blood.

For each animal the means of each sample period were calculated and were used in subsequent calculations. Statistical significance (p < 0.05) was tested for amino acid and carbohydrate concentrations by analysis of varianceusing SAS PROC Mixed software for the control (before infusion) and either study periods (3 and 25 h after the start of the infusion). The significance of the results was also assessed by the Wilcoxon matched-pairs signed-ranks test. Linear regression was calculated by the least-squares method. ANOVA was also used to test the significance of the differences in uptake and release of glucose and amino acids among the three time periods.
RESULTS
The six fetuses underwent uncomplicated vaginal deliveries at 47 ± 4 h after the start of dexamethasone infusion (133 ± 1 d of gestational age) which represented delivery approximately 2 wk before term. Birth weight was 2827 ± 213 g.
Concentrations in fetal and maternal arterial plasma. Three hours after starting the dexamethasone infusion there were no significant differences in most amino acid concentrations and in glucose and lactate concentrations compared with the control period. Only phenylalanine increased significantly (p < 0.02) at 3 h. At 25 h there were small increases in fetal blood O2 saturation and O2 content of fetal blood which attained statistical significance for umbilical vein O2 saturation and content and fetal arterial O2 content(Table 1). Fetal and maternal glucose concentrations and fetal lactate concentrations increased significantly (Table 2). Of the 18 amino acids measured in fetal arterial blood(Table 3) only one, glutamate, had a significant reduction to 57% of control. All essential amino acids, except lysine, increased their arterial concentration significantly. The branched chain amino acids increased by approximately 40%. Seven nonessential amino acids(tyrosine, glycine, proline, glutamine, asparagine, citrulline, and alanine) also increased significantly by 25 h. Figure 2 shows the concentration changes for proline, alanine, and glutamine. In contrast with the changes in fetal arterial plasma, there were relatively few changes in maternal arterial plasma amino acid, only glutamate and histidine changed significantly (Table 4).
Concentration differences across the fetal hepatic circulation. No significant changes in the umbilical venous-left hepatic venous O2 content differences were found between the control and 3- and 25-h periods(p = 0.06). There was a small but significant hepatic glucose uptake during the control period (31 ± 14 μmol/mmol O2, p< 0.05) and at 25 h a net glucose release which was not significantly different from zero (-22 ± 25 μmol/mmol O2, p = 0.1). A large net hepatic uptake of lactate was observed both before (310± 50 μmol/mmol O2) and during dexamethasone infusion (320± 40 μmol/mmol O2), with no significant difference between the two periods (p = 0.94). The amino acids which are normally taken up by the fetal liver(6) did not show significant changes in uptake. Conversely a marked reduction in the hepatic output was observed for glutamate (from 180 ± 56 to 45 ± 18 μmol/mmol O2, p < 0.001), which, at 25 h. was not significantly different from zero (p < 0.31). Fetal hepatic serine release was also significantly reduced (from 147.5 ± 41.7 to 71.1 ± 22.7μmol/mmol O2, p < 0.05).
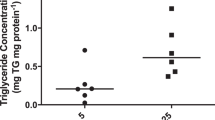
Concentration differences across the uterine and umbilical circulation. The uterine O2 content arterial-venous difference was significantly reduced at 25 h compared with the control period (from 1.15± 0.1 mM to 0.92 ± 0.06 mM, p < 0.01) whereas the umbilical O2 content venous-arterial difference was virtually unchanged(1.69 versus 1.83 mM, p > 0.1). No significant placental uptake or release of serine was found in all three time periods. The reduction of fetal hepatic glutamate release was associated with a significant reduction in placental glutamate uptake from 18.0 ± 3 to 2.0 ± 3μmol/mmol O2, p < 0.01 (Fig. 3). With dexamethasone infusion, there was a significant reduction in the progesterone output by the pregnant uterus (from 91.1 ± 13.0 to 36.3± 9.8 nmol/mmol O2, p < 0.01). At 25 h, concomitant with the increase in glucose concentration in maternal and fetal plasma, there was a significant (p < 0.001) reduction of the fetal glucose/O2 uptake molar ratio across the umbilical circulation (Fig. 4). No significant change in the fetal lactate/O2 uptake molar ratio was observed (70 ± 10versus 80 ± 10 μmol/mmol O2, p = 0.85).
DISCUSSION
During parturition there are endocrine changes in the fetal circulation including changes in cortisol, which attains peak concentrations in the last 48-72 h(12, 13). We have shown that the fetal liver and placenta serve as an integrated organ system with respect to serine-glycine exchange(3) and glutamate-glutamine exchange(7). We hypothesized that the release of serine and glutamate from the fetal liver might be an accommodation to hepatic amino acid oxidation in the absence of hepatic glucose release(3, 7). Cortisol stimulates fetal hepatic gluconeogenesis(11) and thus it may alter serine and glutamate output by the fetal liver. These considerations led us to the present study. A fetal dexamethasone infusion was used because it had been used previously in our laboratory to initiate parturition in sheep(14, 23).
Umbilical and fetal hepatic blood flows were not measured. Therefore the concentration differences of substrates across these circulations could not be used to calculate absolute uptakes. However, we were able to scale umbilical uptakes to fetal O2 consumption and hepatic uptakes to hepatic O2 consumption. The O2 saturation and content of fetal arterial, umbilical venous, and fetal hepatic venous bloods were virtually constant during the experiments, strongly suggesting that fetal and hepatic O2 consumptions either did not change or had small percent changes. For this reason, any large change in substrate/O2 uptake ratio induced by dexamethasone could be interpreted as a change in substrate uptake.
During fetal dexamethasone infusion there was a reduction in fetal hepatic glutamate output to 25% of control and serine output to 48% of control, a decrease in fetal arterial plasma glutamate concentration from 56 to 32 μM and a decrease in placental glutamate uptake to only 20% of control. The reduction in hepatic glutamate output accounts for the decrease in plasma glutamate concentration, because glutamate production by the fetal liver is the major source of glutamate appearance in the fetal plasma(7). In turn, the lower fetal arterial plasma glutamate concentration could account for the decrease in placental glutamate uptake. Under normal physiologic conditions, the placenta clears ≈90% of fetal glutamate from the umbilical circulation(9). This indicates that placental glutamate uptake is limited by the rate at which glutamate is delivered to the placenta by umbilical blood flow. Hence, a decrease in fetal arterial glutamate concentration would decrease placental uptake, even in the absence of any direct dexamethasone effect on placental glutamate transport and metabolism.
Glucocorticoids increase the activity of fetal hepatic gluconeogenic enzymes and promote glycogen synthesis(11). Therefore, the decrease in hepatic glutamate and serine output during dexamethasone infusion is likely to represent diversion of gluconeogenic amino acid carbon from glutamate and serine production to glycogen synthesis. Fetal dexamethasone infusion induced an increase of maternal and fetal plasma glucose concentration coincident with a decrease in glucose uptake by the umbilical circulation. The decreased fetal glucose uptake was caused by a decrease in the transplacental glucose concentration gradient as demonstrated by the following calculation.
The net glucose flux to the fetus from the placenta, (Rf,p), expressed as mg·min-1·(kg fetus)-1, is related to maternal arterial plasma glucose concentration, (GA), and the fetal arterial plasma glucose concentration, (Ga), both expressed as mg·dL-1, by the empirical equation(16):Equation (6) Using the concentration values in Table 2, for the control period:Equation (7) and for the 25-h dexamethasone period:Equation (8)



According to this calculation, there was a decrease in the transplacental glucose gradient which would reduce the glucose uptake per kg fetus to ≈43% of control (i.e. {1.67/3.89}·100). The reduction in uptake predicted by this calculation, agrees with the finding that fetal glucose/O2 uptake ratio decreased to about 54% of control (Fig. 4). Because the calculation assumes no change in the glucose transport properties of the placenta, there is no evidence for a dexamethasone effect upon placental glucose transport capacity. The data indicate the primary effect of dexamethasone was to increase fetal glucose production and/or decrease fetal glucose utilization. Either one of these effects would cause the fetal glucose concentration to increase, reducing the transplacental gradient and thus, in turn, reducing fetal glucose uptake. Given the ability of glucocorticoids to stimulate gluconeogenesis, an increase in fetal glucose production seems most likely. However, fetal hepatic glucose output did not attain a measurable level during dexamethasone infusion. The absence of a significant dexamethasone effect on hepatic glucose output is in agreement with a previous study of fetal cortisol infusion(17). It suggests that dexamethasone may have had dual effects on the fetus, increasing gluconeogenesis and decreasing peripheral glucose utilization. This is not dissimilar from studies in adult mammals. For example, during 5-d cortisol infusion into adult dogs, there was a large increase in hepatic glycogen content and a decrease in net hepatic glucose output(18). The latter suggests decreased utilization by extrahepatic tissues of the glucose released by the liver. In addition to its effect on fetal glucose, the fetal dexamethasone infusion increased by about 20% maternal glucose concentration. This could represent an effect of dexamethasone entering the maternal circulation and/or a response of the mother to some of the changes in substrate flux that were induced by the hormone in the fetus and placenta. The reduction in fetal uptake of maternal glucose is likely to have been one of the changes that contributed to the increase in maternal glucose concentration.
Fetal dexamethasone infusion induced a marked increase in fetal plasma concentration of many amino acids, including essential amino acids. This finding was unexpected because dexamethasone given to normal adult men for several days causes no significant changes in amino acid concentrations, with the exception of a relatively small increase in alanine(19). We could not establish whether the increased concentration was related to metabolic changes in the placenta, fetal liver or both because an increase in amino acid concentration in the fetal circulation increases the analytical error of measuring arteriovenous differences and, thus, increases the variance of uptake estimates. In postnatal life, glucocorticoids increase proteolysis(20). One might hypothesize that dexamethasone reduced fetal growth rate leading to an imbalance between fetal amino acid uptake via the placenta and amino acid disposal via protein accretion.
The present study confirms that dexamethasone infusion in fetal sheep causes a marked decrease in progesterone output by the pregnant uterus(12–14) and demonstrates that the decline in progesterone output coincides with a decrease in placental uptake of fetal glutamate. The oxidation of glutamate generates NADPH(21), which is necessary for steroidogenesis. Synthesis of progesterone by human placental mitochondria is stimulated by the addition of glutamate to the incubation medium(21). It is possible that the decrease in placental glutamate uptake and uterine progesterone output may not be coincidental but the importance, if any, of placental glutamate deprivation upon the decrease in placental progesterone synthesis cannot be assessed at this time.
To our knowledge these are the first data concerning fetal hepatic and placental exchange of amino acids during parturition. Further information is needed to establish the meaning of the present observations with respect to spontaneous parturition. It seems likely that the induction of parturition by fetal dexamethasone infusion simulates some, but not all, of the events that precede natural birth. It is important to note that the effect of dexamethasone on fetal metabolism is of interest per se, because large doses of this glucocorticoid are used for inducing lung maturation in human fetuses(22).
References
Lemons JA, Adcock EW, Jones MD Jr, Naughton MA, Meschia G, Battaglia FC 1976 Umbilical uptake of amino acids in the unstressed fetal lamb. J Clin Invest 58: 1428–1434
Bell AW, Kennaugh JM, Battaglia FC, Meschia G 1989 Uptake of amino acids and ammonia at mid-gestation by the fetal lamb. Q J Exp Physiol 74: 635–643
Cetin I, Fennessey PV, Sparks JW, Meschia G, Battaglia FC 1992 Fetal serine fluxes across the fetal liver, hindlimb and placenta in late gestation. The role of fetal serine in placenta glycine production. Am J Physiol 263:E786–E793
Cetin I, Sparks JW, Quick AN Jr, Marconi AM, Meschia G, Battaglia FC, Fennessey PV 1991 Glycine turnover and oxidation and hepatic serine synthesis from glycine in fetal lambs. Am J Physiol 260:E371–E378
Guyton TS, DeWilt H, Fennessey PV, Meschia G, Wilkening RB, Battaglia FC 1993 Alanine umbilical uptake, disposal rate and decarboxylation rate in the fetal lamb. Am J Physiol 265:E497–E503
Marconi AM, Battaglia FC, Meschia G, Sparks JW 1989 A comparison of amino acid arteriovenous differences across the liver and placenta of the fetal lamb. Am J Physiol 257:E909–E915
Vaughn PR, Lobo C, Battaglia FC, Fennessey P, Wilkening R, Meschia G 1995 Glutamine-glutamate exchange between placenta and fetal liver. Am J Physiol 268:E705–E711
Guyton TS, Fennessey PV, Battaglia FC, Meschia G, Wilkening RB 1994 Plasma lactate disposal, decarboxylation rate and entry into the tricarboxylic acid cycle in the fetal lamb. FASEB J 8: A918(abstr 320)
Moores RR, Vaughn PR, Battaglia FC, Fennessey PV, Wilkening RB, Meschia G 1994 Glutamate metabolism in fetus and placenta of late gestation. Am J Physiol 267:R89–R96
Girard J 1986 Gluconeogenesis in late fetal and early neonatal life. Biol Neonate 50: 237–258
Barnes RJ, Comline RS, Silver M 1978 Effect of cortisol on glycogen concentrations in hypophysectomized, adrenalectomized and normal foetal lambs during late or prolonged gestation. J Physiol 275: 567–579
Liggins GC, Grieves SA, Kendall JZ, Knox BS 1972 The physiological roles of progesterone, oestradiol-17b and prostaglandin F2a in the control of ovine parturition. J Reprod Fert 16: 85–103
Liggins GC 1969 Premature parturition after infusion of corticothrophin or cortisol into foetal lambs. J Endocrinol 45: 515–523
Burd LI, Lemons JA, Makowski EL, Meschia G, Niswender G 1976 Mammary blood flow and endocrine changes during parturition in ewe. Endocrinology 98: 748–754
Bristow J, Rudolph AM, Itskovitz J 1981 A preparation for studying liver blood flow, oxygen consumption and metabolism in the fetal lamb in utero. J Dev Physiol 3: 255–266
Hay WW, Molina RA, Di Giacomo JE, Meschia G 1990 Model of placental glucose consumption and glucose transfer. Am J Physiol 258:R569–R577
Rudolph CD, Roman C, Rudolph AM 1989 Effect of cortisol on hepatic gluconeogenesis in the fetal lamb. J Dev Physiol 11: 219–223
Goldstein RE, Wasserman DH, McGuiness OP, Lacy DB, Cherrington AD, Abumrad NN 1993 Effects of chronic elevation in plasma cortisol on hepatic carbohydrate metabolism. Am J Physiol 264:E119–E127
Wise JK, Hendler R, Felig P 1973 Influence of glucocorticoids on glucagon secretion and plasma amino acid concentrations in man. J Clin Invest 52: 2774–2782
Simmons PS, Miles GM, Gerich JE, Haymond MW 1984 Increased proteolysis. An effect of increases in plasma cortisol within the physiologic range. J Clin Invest 73: 412–420
Klimek J, Makarewicz W, Swierczynski J, Bossy-Bukato G, Zelewski L 1993 Mitochondrial glutamine and glutamate metabolism in human placenta and its possible link with progesterone biosynthesis. Troph Res 7: 77–86
Maher JE, Cliver SP, Goldenberg RL, Davis RO, Copper RL the March of Dimes Multicentric Study Group 1994 The effect of corticosteroid therapy in the very premature infant. Am J Obstet Gynecol 170: 869–873
Stys SJ, Clewell WH, Meschia G 1978 Changes in cervical compliance at parturition independent of uterine activity. Am J Obstet Gynecol 130: 414–418
Deleted in proof
Wilkening RB, Battaglia FC, Meschia G 1985 The relationship of umbilical glucose uptake to uterine blood flow. J Dev Physiol 7: 313–319
Schreiner RL, Burd LI, Jones MD Jr., Lemons JA, Sheldon RE, Simmons MA 1978 Fetal metabolism in fasting sheep. In: Longo LD and Reneav DD (eds) Fetal and Newborn Cardiovascular Physiology, Vol. 2. Garland STPM Press, New York, pp 197–222
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Grants HD-01866, HD-29374, and HD-29188.
Rights and permissions
About this article
Cite this article
Barbera, A., Wilkening, R., Teng, C. et al. Metabolic Alterations in the Fetal Hepatic and Umbilical Circulations during Glucocorticoid-Induced Parturition in Sheep. Pediatr Res 41, 242–248 (1997). https://doi.org/10.1203/00006450-199702000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199702000-00015