Abstract
The clinical significance of nutritional carnitine deficiency remains controversial. To investigate this condition under controlled conditions, an animal model was developed using the parenterally alimented, carnitine-deprived newborn piglet. Forty-five piglets received total parenteral nutrition for 2-3 wk that was either carnitine-free or supplemented with 100-400 mg/L L-carnitine. Blood and a muscle biopsy were taken at the initial surgery. Carnitine balance studies were performed at 11-14 d of age. Blood, liver, heart, and skeletal muscle were taken at sacrifice for analysis of carnitine, electron microscopy, and oxidation studies. Carnitine-deprived piglets were in negative carnitine balance and had lower blood, urine, and tissue levels of carnitine than carnitine-supplemented animals. There was a positive correlation between excretion and plasma concentrations of free carnitine with an apparent renal threshold between 15 and 35 μmol/L. Plasma levels were correlated with liver and heart, but not muscle, concentrations of total acid-soluble carnitine. Carnitine-deprived piglets had evidence of lipid deposition in liver and skeletal muscle and tended to have a higher incidence of muscle weakness and cardiac failure. Basal rates of oxidation of[14C]palmitate to 14CO2 and 14C-acid-soluble products were lower in liver homogenates from carnitine-deprived piglets than in those from carnitine-supplemented animals and increased in a dose-dependent fashion with the addition of L-carnitine (0, 50, and 500 μmol/L) in vitro. In summary, carnitine deprivation in the neonatal piglet resulted in low carnitine status and morphologic/functional disturbances compatible with carnitine deficiency. The described animal model appears to be suitable for the investigation of neonatal nutritional carnitine deficiency.
Similar content being viewed by others
Main
Primary systemic carnitine deficiency, an inborn error of carnitine transport, is a relatively rare, but well defined, autosomal recessive disease characterized by (cardio)myopathy and hepatic dysfunction, leading to episodic metabolic crises usually precipitated by fasting or infection(1). Serum and/or tissue levels of carnitine are reduced to 10-30% of controls. The ability to catabolize lipid is impaired, leading to lipid storage in muscle, heart, and liver.
The clinical significance of nutritional carnitine deficiency, on the other hand, remains controversial. Although hypocarnitinemia(2), reduced carnitine tissue levels(3), and biochemical evidence of impaired ability to handle an exogenous lipid load(4) have been reported in premature infants deprived of exogenous carnitine, documentation of physiologic dysfunction has remained anecdotal (for review, seeRefs. 5 and 6). The difficulties of studying this entity in a complex clinical setting have prompted efforts to develop an animal model for nutritionally induced carnitine deficiency. Attempts to induce carnitine deficiency in adult mammals by reducing exogenous carnitine intake generally have proven unsuccessful due to the mature animal's capacity to synthesize sufficient carnitine(7). It was recently reported that muscle and liver carnitine concentrations in juvenile rats fed enterally with carnitine-free TPN solutions for 6 wk were approximately 53% of those found in chow-fed controls(8). No functional disturbances were detected. Models based on feeding adult animals diets devoid of carnitine biosynthetic precursers, e.g. lysine(9), or cofactors, e.g. ascorbic acid(10), are limited in their usefulness for the study of carnitine deficiency because of the confounding deficiencies produced. More recent attempts to produce carnitine depletion by administering antibiotics conjugated with pivalic acid(11, 12) have proven unsatisfactory due to species' differences in the ability to form pivaloylcarnitine and confounding metabolic effects due to pivalic acid. We have previously induced carnitine deficiency in the artificially fed, carnitine-deprived newborn rabbit(13). This model is also of limited usefulness. Unlike in the human newborn, a renal carnitine leak was found in the rabbit pups, suggesting a more generalized malnutrition. Similar concerns were raised by a recent report of carnitine deficiency induced in the carnitine-deprived, artificially fed rat pup(14). The rat pups, fed a rat milk substitute via gastrostomy for 4 d beginning on the 1 st d of life, not only weighed less than dam-nursed control pups, but also less than their birth weight. Furthermore, there are considerable differences in neonatal metabolism between rabbit or rodent and human.
The newborn piglet has been considered a more appropriate model species than rodents or rabbits because of greater anatomic, physiologic, and metabolic similarities with the human neonate(15, 16). In particular, carnitine plasma and tissue concentrations during early development have been shown to be similar in both species(17). Successful TPN has been reported in the neonatal pig(18). The following describes the development of a model to study the pathophysiology of neonatal nutritional carnitine deficiency using the parenterally alimented, carnitine-deprived newborn piglet.
METHODS
Induction of carnitine deficiency. Forty-five 1-d-old mixed hybrid domestic piglets (Sus scrota domestica) that had received maternal colostrum were obtained from commercial sources. Placement of a central venous catheter was undertaken via the right or left external jugular vein under aseptic conditions and general anesthesia with halothane. This and subsequent catheters were tunneled under the skin to exit dorsally. A blood sample and open muscle biopsy from the quadriceps muscle were obtained at the time of surgery. The piglets were housed in neonatal incubators that provided a thermal neutral environment. They were given TPN (Table 1) that was either carnitine-free or supplemented with 100, 200, or 400 mg/liter L-carnitine (Sigma, Tau Chemical Co., Rome) for 2-3 wk. In some animals, at 1 wk of age, a bladder catheter to facilitate the collection of timed urine specimens was inserted directly into the bladder via an abdominal incision and threaded under the skin to exit dorsally. All piglets routinely received 3 d of antibiotics (cefazolin) after surgery and additional antibiotics if they developed fever. Fourteen piglets received prophylactic gentamicin daily. Animals with prolonged febrile illness (>3 d) or acute onset of fever within 72 h preceding a particular study were excluded from that study. Animals were weighed daily to assess their nutritional status. TPN was discontinued, and a saline infusion was infused for 12-14 h before initiation of most studies. The animals were usually killed by exsanguination under deep anesthesia with halothane. As a control group, farm-raised sow-fed piglets 2-3 wk of age were also studied. This study was approved by the Louisiana State University Medical Center Institutional Animal Care and Use Committee.
Carnitine excretion. The excretion (E) of FC was calculated from concentrations of FC and creatinine (Cr) in urine (U) and corresponding plasma (P) samples according to the following formula(19): where GF = glomerular filtrate.
Carnitine balance studies. Two or three consecutive 24-h urine collections were undertaken at 11-14 d of age for the measurement of total(TC), free (FC), and esterified (AC) carnitine and creatinine. Blood samples were obtained in the middle of the collection periods. TC was measured in aliquots of TPN solution and used for calculation of carnitine intake on the basis of daily TPN intake. Carnitine output was calculated from urinary concentrations and volume of urine. Carnitine balance was defined as intake minus urinary output of TC. Loss of carnitine through the stool was assumed to be negligible in these parentally alimented animals. Animals with diarrhea were excluded from this study.
Liver fat content(20). Approximately 1 g of liver was homogenized in 10 mL of modified Dole's extraction mixture(isopropanol/n-hexane/5.3% H2SO4: 40/10/1, vol/vol/vol). After centrifugation for 5 min at 2000 rpm, the supernatant was transferred to a clean glass tube, and the precipitate was washed with an additional 10 mL of extraction mixture. The combined supernatants were mixed with 10 mL each of hexane and water and centrifuged for 10 min at 2000 rpm. The upper layer was collected into a preweighed glass tube, and the lower layer was washed with 1 mL of hexane, which was also added to the glass tube. The combined upper layers were evaporated and dried at 37 °C until constant weight was obtained. Total fat weight was related to tissue wet weight.
Biochemical methods. TC and FC in plasma and urine were determined by a modification(21) of the radiochemical method of McGarry and Foster(22). AC was calculated from the difference between TC and FC. Total acid-soluble carnitine was measured in tissues as previously described(3) and related to dry weight and NCP(23). Creatinine(24) and total protein(25) in tissues were determined by standard methods.
Electron microscopy. Electron microscopy was performed at the Department of Anatomy, LSU Medical Center, using a JEOL JEM 1210 transmission electron microscope.
In vitro oxidation studies(26). Approximately 1 g of liver tissue was weighed, diced, and homogenized in 8 mL of ice-cold buffer (0.25 mol/L sucrose and 10 mmol/L Tris-HCl, pH 7.4) using a homogenizer (Virtishear Cyclone Sentry Microprocessor, Virtis, Gardiner, NY) set at 15,000 rpm for 60-90 s. After centrifugation at 700 × g to remove cellular debris, 200 μL of the resulting supernatant were incubated with 1 mL of incubation buffer (100 mmol/L sucrose, 8 mmol/L NaH2PO4, 0.4 mmol/L EDTA, 0.4 mmol/L MgCl2, 80 mmol/L KCl, 0.1 mmol/L malate, 2 mmol/L ATP, 0.04 mmol/L CoA, 1 mmol/L NAD, and 0.04 mmol/L palmitate labeled with 0.4 μCi/mL [14C-U]palmitate (DuPont NEN, Boston, MA) complexed with essentially fatty acid-free BSA) for 60 min in a shaking water bath at 37 °C. Each glass incubation vial was sealed with a rubber stopper fitted with a capsule suspended above the medium containing strips of filter paper (1 × 2 cm) drenched with 100 μL of 0.3 N Ba(OH)2. After termination of the incubation by injection of 100 μL of concentrated perchloric acid into the medium, the tubes were kept in the shaking water bath for an additional hour to trap the 14CO2 formed. The filter paper was then placed in scintillation fluid, and the inside of the trap was washed twice with scintillation fluid before counting in a liquid scintillation counter (1219 Rackbeta, LKB, Wallac).14 C-Labeled acid-soluble products were determined by counting the radioactivity in an aliquot of supernatant after centrifugation of the perchloric acid-treated homogenate. Results were related to homogenate protein. The oxidation studies were performed in triplicate under basal conditions, without addition of exogenous L-carnitine, and in duplicate with addition of increasing amounts of L-carnitine (50 and 500 μmol/L) added to the incubation media.
Statistical analysis. The data were evaluated by parametric and nonparametric analytical methods including the t test, Mann-Whitney test for independent samples, Wilcoxon test for paired samples, Kruskal-Wallis nonparametric analysis of variance test for evaluation of three groups, and the Friedman nonparametric repeated measures test. Certain aspects of the clinical data were evaluated by a 2 × 2 contingency table (Fisher's exact test, including Yate's continuity correction). Correlations between parameters were determined by regression analysis. The acceptable probability for an error of the first kind was defined a priori at α < 0.05.
RESULTS
Clinical data. The clinical data are presented in Table 2. There were no significant differences in mean initial weight or weight gain/d. Between 20 and 30% of the parenterally alimented piglets developed a secretory diarrhea that usually started in the 2nd wk of life and persisted for up to 4 d. The diarrhea was generally mild and not associated with weight loss. Two piglets in each group developed fever(>40 °C, >24 h) either associated with diarrhea or with a catheter site infection. There was no difference in incidence of fever or diarrhea between the two groups. Six of the 23 carnitine-deprived piglets developed symptoms compatible with carnitine deficiency. Four exhibited muscle weakness(diagnosed by splaying of the rear legs, difficulty or inability to stand up or walk), and three developed heart failure (diagnosed clinically by presence of tachycardia, tachypnea, rales, edema, response to diuretics). In contrast, muscle weakness was found in only one of the carnitine-supplemented piglets; none developed heart failure.
Carnitine values in plasma and urine. There were no differences in plasma carnitine values (Table 3) between the carnitine-deprived and -supplemented piglets on the 1st d of life. Two to three weeks of carnitine-free parenteral alimentation led to a fall in plasma TC, FC, and AC to levels that were 19, 15, and 32% of those found in carnitine-supplemented animals. They were also lower than those found in sow-fed piglets of the same age. The mean ratio of esterified to free carnitine (AC/FC) was higher in carnitine-deprived than in carnitine-supplemented piglets (p = 0.042). Carnitine supplementation led to an increase of plasma TC and FC to levels that were higher than those found in sow-fed piglets.
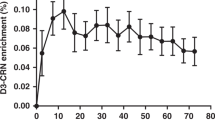
TC, FC, and AC concentrations in urine (Table 4) were 27-56 times lower in carnitine-deprived than in carnitine-supplemented piglets. The percent contribution of AC to TC was over 2-fold higher in the carnitine-deprived animals. There was a significant positive correlation(r2 = 0.843, n = 15, p < 0.0001) between excretion and plasma concentrations of FC with clear separation of the two study groups (Fig. 1). The apparent renal threshold for FC was between 15 and 35 μmol/L.
Carnitine-deprived animals were in negative carnitine balance, losing 6.0± 4.1 μmol/d (mean ± SD, n = 6). Carnitine-supplemented piglets were in positive balance retaining 47.6± 11.1% (mean ± SD, n = 6) of their administered dose.
Tissue carnitine concentrations. Mean total acid-soluble carnitine concentrations in muscle, heart, and liver from 2-3-wk-old carnitine-deprived piglets were 45.2, 45.6, and 23.5%, respectively, of those found in carnitine-supplemented animals (Table 5). Muscle concentrations were 42.8% of those found in sow-fed controls. Serial muscle biopsies taken from the same animal on d 1 and after 2-3 wk of TPN revealed that carnitine-deprived piglets decreased their muscle carnitine concentrations to about 47.8% of initial levels (from 10.03 ± 7.64 to 4.79 ± 2.53 μmol/g of NCP, n = 8, p < 0.03). In contrast, carnitine-supplemented piglets did not significantly change their carnitine muscle concentrations over the duration of TPN (8.14 ± 2.65versus 10.87 ± 5.87 μmol/g of NCP, n = 9, on the 1st d and after 2-3 wk of TPN, respectively).
Regression analysis testing the relationship between plasma TC and tissue total acid-soluble carnitine concentrations (related to NCP) revealed a strongly positive exponential correlation for liver (r2 = 0.728, n = 21, p < 0.0001), a weaker one for heart(r2 = 0.350, n = 16, p < 0.02), and none for muscle (r2 = 0.107, n = 20, p = 0.159).
Lipid deposition in tissues. The total fat content of liver determined gravimetrically was about 2-fold higher (p = 0.003) in carnitine-deprived (58.7 ± 5.3 mg/g of wet weight, n = 8) than in carnitine-supplemented animals (26.5 ± 5.3 mg/g of wet weight,n = 7). Electron microscopy was performed in muscle from two carnitine-deprived piglets and one carnitine-supplemented control. A representative electron micrograph of muscle from a carnitine-deprived piglet revealed multiple fat droplets distributed as a “string of pearls” between the myofibrils in close proximity to mitochondria. The picture was quite different in muscle from the carnitine-supplemented animal where only a few scattered droplets were seen (Fig. 2).
(a) Electron micrograph of skeletal muscle from a 16-d-old, parenterally alimented piglet that had not been supplemented with L-carnitine revealed the presence of multiple fat droplets(magnification, 6750×). (b) Skeletal muscle from an age-matched, carnitine-supplemented piglet (magnification, 6250×). The measure bars indicate 5 μm.
In vitro hepatic fatty acid oxidation. Under basal conditions, without addition of L-carnitine to the media, 14CO2 production and incorporation of 14C into acid-soluble products from[14C-U]palmitate were lower in liver homogenates from carnitine-deprived than in those from carnitine-supplemented animals (Fig. 3). Addition of increasing amounts of L-carnitine to the incubation media resulted in a dose-dependent increase of14 CO2 production and formation of 14C-acid-soluble products in liver tissue from both groups of animals. However,14 CO2 production was lower in liver homogenates from carnitine-deprived than in those from carnitine-supplemented animals at any concentration of carnitine in the media. The rate of formation of14 C-acid-soluble products was lower in the carnitine-deprived than in the carnitine-supplemented piglets at 50 μmol/L. However, this difference was no longer significant at the highest carnitine concentration in the media.
(a) 14CO2 production and(b) formation of 14C-acid-soluble products in liver homogenates from 2-3-wk-old piglets receiving TPN with (▪) or without(□) L-carnitine supplementation. Homogenates were incubated with[14C-U]palmitate and various amounts of added L-carnitine (basal or without added L-carnitine, 50 and 500 μmol/L). Each column represents the mean ± SEM of homogenates from four to five piglets. p values indicate differences between the two groups (unpaired t test).
DISCUSSION
Carnitine deprivation of the parenterally alimented newborn piglet for 2-3 wk decreased plasma concentrations of all carnitine fractions to levels that were lower than those on the 1st d of life, lower than those in carnitine-supplemented or sow-fed controls, and in a similar range to those seen in human infants receiving carnitine-free TPN(2, 27, 28). Urinary excretion decreased correspondingly, indicating an intact renal conservation mechanism. Nonetheless, carnitine-deprived piglets were in negative carnitine balance suggesting an obligatory loss of carnitine similar to that seen in the human(19). The apparent renal threshold for FC was estimated to lie between 15 and 35 μmol/L, which is similar to that estimated for the human(19, 29).
Tissue levels were also lower in the carnitine-deprived than in the carnitine-supplemented piglets. Serial muscle measurements revealed that carnitine-deprived piglets decreased their muscle concentrations after 2-3 wk of carnitine-free TPN. However, it cannot be assumed that this decrease indicates absent carnitine biosynthesis. Estimated changes of carnitine body pool calculated from muscle carnitine concentrations and body weight on d 1 and at 2-3 wk of life (assuming that skeletal muscle contains about 95% of body carnitine and contributes about 25% to body weight) indicate that carnitine-deprived piglets may actually increase their total body carnitine, suggesting that carnitine biosynthesis was occurring during the first 2-3 wk of life. However, as in the human, endogenous carnitine biosynthesis was obviously not enough to maintain tissue levels, emphasizing the importance of an exogenous carnitine supply for the neonate. There was no difference in mean muscle carnitine levels between carnitine-supplemented and sow-fed animals. However, muscle concentrations from animals receiving the lowest level of carnitine intake (17 mg/kg/d) averaged 73% of those found in sow-fed controls, suggesting that higher i.v. doses may be needed to achieve optimal carnitine accretion in the muscle of a rapidly growing animal. The carnitine content of mature sow-milk has been reported to be 150 μmol/L(30). Assuming that a piglet drinks 300 mL/kg/d (G. Gomez, North Carolina State University, personal communication), carnitine intake would be approximately 7.3 mg/kg/d which is less than half of that received by our parenterally alimented piglets on low dose carnitine. Because plasma levels of total and FC were higher in the low dose carnitine-supplemented piglets (TC 52.3 ± 10.3, FC 45.0 ± 8.4μmol/L, n = 5) than in the sow-fed animals (p < 0.002), the data suggest that there might be a difference in carnitine uptake by muscle tissue between parenterally alimented and sow-fed piglets. This may be related to the form of carnitine offered to the tissues. The carnitine content of sow's milk is overwhelmingly esterified with a large contribution by isovalerylcarnitine(31), whereas the i.v. solution contained only FC. Furthermore, i.v. administration circumvents “first pass” through intestinal mucosa and liver which may also affect the form of carnitine available to peripheral tissues. On the other hand, there may be other, currently unrecognized factors associated with TPN or sow's milk affecting muscle transport. The muscle carnitine concentrations of animals receiving low (100 mg/L) versus high dose (400 mg/L) carnitine supplementation do show a tendency for higher mean carnitine levels in the latter. Administration of i.v. L-carnitine 34-68 mg/kg/d appears to approach muscle accretion rates of the sow-fed piglet.
Plasma carnitine levels, although strongly correlated with liver and heart tissue concentrations, did not reflect carnitine status in skeletal muscle. This is probably due to tissue-specific differences in carnitine uptake and turnover(32), e.g. human muscle has a much slower turnover than does liver. It is unknown whether prolonged carnitine deprivation affects the plasmalemmal carnitine transporter in various tissues. The retention of i.v. administered carnitine in our piglets was similar to that reported in human infants(33).
A deficiency state implies functional disturbance that can be ameliorated by administration of the substance in question. There is evidence that such a functional disturbance occurred in the described model. Assuming that the plasma AC/FC ratio reflects the relationship between esterified and free CoA within the cell(34), the higher mean AC/FC ratio in the plasma of carnitine-deprived compared with carnitine-supplemented piglets may reflect a sequestration of tissue CoA in the esterified form with potential inhibitory effects on metabolism. Four of 20 carnitine-deprived piglets had a plasma AC/FC > 1.5, whereas none of the carnitine-supplemented or sow-fed piglets exhibited an AC/FC ratio > 0.8. Electron microscopic demonstration of fat deposition in the muscle and increased liver fat content of carnitine-deprived piglets suggest impaired fatty acid oxidation with subsequent deposition of neutral lipid. Such findings have been observed in patients with myopathic carnitine deficiency(35), in those with the carnitine transporter defect(1) and in juvenile visceral steatosis (jvs) mice(36) that have an inborn error of carnitine transport. In addition, in spite of a similar incidence of fever and diarrhea, more carnitine-deprived than carnitine-supplemented animals exhibited clinical symptoms compatible with carnitine deficiency, e.g. muscle weakness and heart failure.
In vitro oxidation studies with homogenates have long been used clinically(35) and in animal experiments(37) for the investigation of carnitine's role in oxidative metabolism. Their interpretation must be viewed with caution. The findings may not reflect fatty acid oxidation rates in vivo, because the organism has the ability to compensate deficiencies through hormonal or other homeostatic mechanisms. Furthermore, homogenization implies disruption of normal subcellular compartmentalization with subsequent loss of regulation, as well as significant dilution of substrate and cofactor pools. Nonetheless, our findings are suggestive of functional disturbances due to carnitine deprivation. Liver homogenates from the carnitine-deprived piglets oxidized radiolabeled palmitate less well than those from carnitine-supplemented animals. Both basal production of 14CO2 and formation of14 C-acid-soluble products were lower in carnitine-deprived than in carnitine-supplemented piglets suggesting that carnitine concentrations in the incubation media were rate-limiting for β-oxidation. Addition of L-carnitine to the incubation media increased the production of both14 CO2 and 14C-acid-soluble products in a dose-dependent fashion. However, a difference in 14CO2 production between carnitine-deprived and -supplemented animals was found even at concentrations of greater than 500 μmol/L L-carnitine in the incubation. This observation is difficult to interpret. In the liver, CPT I is thought to be a major regulatory enzyme for fatty acid oxidation(38). Assuming that the Km of porcine liver CPT I is similar to that found in adult rat liver, (i.e. ≈30 μmol/L)(39), a carnitine concentration of ≥500 μmol/L should exceed the Km for CPT I by over 10-fold and therefore not be rate-limiting. The lower 14CO2 production found in the carnitine-deprived versus -supplemented piglets at this higher concentration suggests an altered hepatic oxidative capacity. The explanation for this finding is unclear. Although it is possible that prolonged carnitine-deprivation down-regulates CPT I, this would be unlikely because other conditions associated with low carnitine levels are characterized by increased CPT I activity(40) and CPT I gene expression(41). The finding that there was no difference in the rate of formation of 14C-acid-soluble products at ≥500 μmol/L L-carnitine in the incubation suggests that the entry rate of[14C]palmitate into the mitochondrial β-oxidative pathway was similar between the two groups and that the impairment of oxidative metabolism in the carnitine-deprived piglets occurred at a more distal point in the pathway. This may represent a secondary change due to nutritional carnitine deprivation during neonatal development, the nature of which is unclear at this time and currently under study.
In summary, parenterally alimented piglets deprived of carnitine for 2-3 wk exhibited decreased blood, urine, and tissue levels of carnitine, as well as morphologic, biochemical, and clinical changes suggestive of metabolic and functional disturbances due to the lack of carnitine intake. The described animal model appears to be a suitable tool to help clarify the controversy that exists concerning the clinical relevance of neonatal nutritional carnitine deficiency. Although hypocarnitinemia is relatively easy to detect, carnitine deficiency, i.e. an abnormal clinical presentation correctable by carnitine administration(6), is not easily recognized in infants receiving TPN and indeed has not been convincingly demonstrated in any population not afflicted with an inborn error of metabolism. Evidence concerning potential functional disturbance is limited to biochemical perturbations. Clinically relevant functional disturbances(such as the muscle, myocardial, or hepatic dysfunction seen in patients with more severe carnitine depletion due to the inborn carnitine transport defect) have been only anecdotally reported in patients with nutritional carnitine deprivation.
The difficulty of documenting carnitine deficiency in the human newborn may be due to: 1) the multiplicity of confounding factors that could produce clinical symptoms similar to those of carnitine deficiency in the complex patients at risk; 2) the inappropriateness of using provocative maneuvers necessary to elicit disturbances due to carnitine deficiency in the sick human infant; and 3) the moderate degree of deficiency. This model was developed to study the effects of carnitine deprivation on vital organs and systems under controlled conditions and during provocative testing with various stressors,e.g. cold exposure, hypoxia or sepsis. It will allow the use of invasive techniques in vivo to look for subtle pathophysiologic changes and will facilitate repeated blood and tissue sampling allowing longitudinal follow-up. The parenterally alimented, carnitine-deprived piglet presents certain advantages over previous attempts to create a model of nutritional carnitine deficiency. From many aspects, including metabolism, anatomy, organ development, and level of maturity, it is more similar to the human neonate than other model animals used. Moreover, in this model, carnitine deprivation is the only factor involved in the induction of carnitine deficiency, thus eliminating confounding factors present in many previous attempts.

Abbreviations
- TC:
-
total carnitine
- FC:
-
free carnitine
- AC:
-
esterified (acyl)carnitine
- NCP:
-
noncollagenous protein
- TPN:
-
total parenteral nutrition
- CPT:
-
carnitine palmitoyltransferase
References
Treem WR, Stanley CA, Finegold DN, Hale DE, Coates PM 1988 Primary carnitine deficiency due to a failure of carnitine transport in kidney, muscle, and fibroblasts. N Engl J Med 319: 1331–1336.
Penn D, Schmidt-Sommerfeld E, Wolf H 1980 Carnitine deficiency in premature infants receiving total parenteral nutrition. Early Hum Dev 4: 23–34.
Penn D, Ludwigs B, Schmidt-Sommerfeld E, Pascu F 1985 Effect of nutrition on tissue carnitine concentrations in infants of different gestational ages. Biol Neonate 47: 130–135.
Schmidt-Sommerfeld E, Penn D, Wolf H 1983 Carnitine deficiency in premature infants receiving total parenteral nutrition: effect of L-carnitine supplementation. J Pediatr 102: 931–935.
Schmidt-Sommerfeld E, Penn D 1992 Role of carnitine in children receiving total parenteral nutrition. In: Ferrari R, Dimauro S, Sherwood G (eds) L-Carnitine and Its Role in Medicine: From Function to Therapy. Academic Press, New York, pp 117–136.
Rebouche CJ 1992 Carnitine functions and requirements during the life cycle. FASEB J 6: 3379–3386.
Boehles H, Michalk D, Brandl U, Fekl W 1983 Tissue carnitine concentrations after total parenteral nutrition with and without L-carnitine supplementation. Clin Nutr 2: 47–49.
Heinonen OJ, Takala J 1994 Moderate carnitine depletion and long chain fatty acid oxidation, exercise capacity, and nitrogen balance in the rat. Pediatr Res 36: 288–292.
Tanphaichitr V, Broquist HP 1973 Lysine deficiency in the rat: concomitant impairment in carnitine biosynthesis. J Nutr 103: 80–87.
Sandor A, Kispal G, Kerner J, Alkonyl I 1983 Combined effect of ascorbic acid deficiency and underfeeding on the hepatic carnitine levels in guinea pigs. Experientia 39: 512–513.
Diep QN, Bohmer T, Schjerven L 1992 Reduced carnitine and ketogenesis in the pivampicillin treated rat. Biochem Pharmacol 44: 1226–1228.
Davis AT 1995 The alterations in fat metabolism caused by pivalate administration occur independently of carnitine depletion. FASEB J 9:A156.
Penn D, Schmidt-Sommerfeld E 1988 The carnitine-deprived newborn rabbit: a potential model to study carnitine deficiency. J Nutr 118: 1535–1539.
Flores C, Hu C, Edmond J, Koldovsky O 1996 Milk carnitine affects organ carnitine concentration in newborn rats. J Nutr 126: 1673–1682.
Moughan PJ, Rowan AM 1989 The pig as a model animal for human nutrition research. Proc Nutr Soc NZ 14: 116–123.
Book SA, Bristad LK 1974 The fetal and neonatal pig in biomedical research. J Anim Sci 38: 997–1002.
Baltzell JK, Beser FW, Miguel SG, Borum PR 1986 The neonatal piglet as a model for human neonatal carnitine metabolism. J Nutr 117: 754–757.
Wykes LJ, Ball RO, Pencharz PB 1993 Developmental and validation of a total parenteral nutrition model in the neonatal piglet. J Nutr 123: 1248–1259.
Schmidt-Sommerfeld E, Penn D, Bieber LL, Kerner J, Rossi TM, Lebenthal E 1990 Carnitine ester excretion in pediatric patients receiving parenteral nutrition. Pediatr Res 28: 158–165.
Radin NS 1969 Preparation of lipid extracts. Methods Enzymol 14: 245–254.
Schmidt-Sommerfeld E, Werner D, Penn D 1988 Carnitine plasma concentrations in 353 metabolically healthy children. Eur J Pediatr 147: 356–360.
McGarry JD, Foster DW 1976 An improved and simplified radioisotopic assay for the determination of free and esterified carnitine. J Lipid Res 17: 277–281
Liliental JL, Zeirler KL, Folk BP, Buka R, Riley MJ 1950 A reference base and system for analysis of muscle constituents. J Biol Chem 183: 501–508.
Heinegard D, Tiderstrom G 1973 Determination of serum creatinine by a direct colorimetric method (Sigma Diagnostic Kit no. 555A). Clin Chim Acta 43: 305
Lowry OH, Rosebrough NJ, Fair AL, Randall RJ 1951 Protein measurement with the Folin phenol reagent. J Biol Chem 183: 501–508.
Passeron S, Savageau MA, Harary I 1968 Optimal conditions for palmitate oxidation by rat heart homogenates. Arch Biochem Biophys 128: 124–128.
Helms RA, Whitington PF, Mauer EC, Cataran EM, Christensen ML, Borum PR 1986 Enhanced lipid utilization in infants receiving oral L-carnitine during long term parenteral nutrition. J Pediatr 109: 984–988.
Bonner CM, DeBrie KL, Hug G, Landrigan E, Taylor BJ 1995 Effect of parenteral L-carnitine supplementation on fat metabolism and nutrition in premature infants. J Pediatr 126: 287–292.
Engel AG, Rebouche CJ, Wilson DM, Glasgow AM, Romshe CA, Cruse RP 1981 Primary systemic carnitine deficiency. II. Renal handling of carnitine. Neurology 31: 819–835.
Coffey MT, Shireman RB, Herman DL, Jones EE 1991 Carnitine status and lipid utilization in neonatal piglets fed diets low in carnitine. J Nutr 121: 1047–1053.
Kerner J, Froseth JA, Miller ER, Bieber LL 1984 A study of the acylcarnitine content of sow's colostrum, milk and newborn piglet tissues. J Nutr 114: 854–861.
Rebouche CJ, Engel AG 1984 Kinetic compartmental analysis of carnitine metabolism in the human carnitine deficiency syndromes. Evidence of alterations in tissue carnitine transport. J Clin Invest 73: 857–67.
Helms RA, Mauer EC, Hay WH, Christensen ML, Storm MC 1990 Effect of intravenous L-carnitine on growth parameters and fat metabolism during parenteral nutrition in neonates. J Parenter Enteral Nutr 14: 448–453.
Brass EP 1994 Overview of coenzyme A metabolism and its role in cellular toxicity. Chem-Biol Interact 90: 203–214.
Engel AG, Angelini C 1973 Carnitine deficiency of human skeletal muscle with associated lipid storage myopathy. Science 179: 899–902.
Miyagawa J, Kuwajima M, Hanafusa T, Ozaki K, Fujimura H, Ono A, Uenaka R, Narama I, Oue T, Yamamoto K, Kaidoh M, Nikaido H, Hayakawa J, Horiuchi M, Saheki T, Matsuzawa Y 1995 Mitochondrial abnormalities of muscle tissue in mice with juvenile visceral steatosis associated with systemic carnitine deficiency. Virchows Archiv 426: 271–279.
Long CS, Haller RG, Foster DW, McGarry JD 1982 Kinetics of carnitine-dependent fatty acid oxidation: Implications for human carnitine deficiency. Neurology 32: 663–666.
McGarry JD 1995 Ketogenesis and lipogenesis: metabolic integration in health and disease. Biochem Soc Trans 23: 481–485.
Weiss BC, Cowan AT, Brown N, Foster DW, McGarry JD 1994 Use of a selective inhibitor of liver carnitine palmitoyltransferase I (CPT I) allows quantification of its contribution to total CPT I activity in rat heart. J Biol Chem 269: 26443–26448.
Tsoko M, Beauseigneur F, Gresti J, Niot I, Demarquoy J, Boichot J, Bezard J, Rochette L, Cluoet P 1995 Enhancement of activities relative to fatty acid oxidation in the liver of rats depeleted of L-carnitine by D-carnitine and a γ-butyrobetaine hydroxylase inhibitor. Biochem Pharmacol 49: 1403–1410.
Uenaka R, Kuwajima M, Ono A, Matsuzawa Y, Hayakawa J-i, Inohara N, Kagawa Y, Ohta S 1996 Increased expression of carnitine palmitoyltransferase I gene is repressed by administering L-carnitine in the hearts of carnitine-deficient juvenile visceral steatosis mice. J Biochem 119: 533–540.
Acknowledgements
The authors thank Cathy Veil for her assistance with the electron microscopic examinations and Pamela Hilliard and Shelinda Harris for their secretarial assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by U.S. Public Health Service Grant HD29273 and by a grant from the American Heart Association-La Affiliate, Inc.
Rights and permissions
About this article
Cite this article
Penn, D., Bobrowski, P., Zhang, L. et al. Neonatal Nutritional Carnitine Deficiency: A Piglet Model. Pediatr Res 42, 114–121 (1997). https://doi.org/10.1203/00006450-199707000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00018