Abstract
The objective of the present study was to determine whether whole blood carboxyhemoglobin (COHb) and plasma bilirubin, two indicators of hemolysis, are elevated in infants with severe Rh isoimmune hemolytic disease during the first months of life. Beginning at 2 wk of age and continuing monthly for 3 mo, serial blood samples were obtained for COHb, plasma bilirubin, Hb, reticulocyte count, plasma erythropoietin, plasma enzymes, and plasma iron. Because control infants (n = 13) and infants with ABO hemolytic disease (n = 5) did not differ from one another in any of the study parameters, these two groups were combined and compared with infants with the Rh isoimmunization. Infants with severe Rh isoimmune hemolytic disease(n = 13) were found to have significantly lower Hb and significantly higher bilirubin, the COHb fraction divided by the Hb concentration(COHb√Hb), and plasma erythropoietin levels at 2 and 6 wk of age, and reticulocyte counts at 6 wk. The remaining parameters were not different between the control-ABO group and Rhisoimmune group at any of the study intervals. The study's two primary indicators of hemolysis, plasma bilirubin and COHb√Hb, were significantly correlated with one another in the Rh-immunized group (r = 0.66, p < 0.0001), but not in the combined control-ABO group. Serial Rh antibody concentrations measured in the serum of four neonates with Rh isoimmunization demonstrated a mean half-life of 14.3 d. We speculate that, among infants with severe Rh isoimmune hemolytic disease, elevated total bilirubin levels and COHb√Hb ratios identified in the early weeks of life indicate continuing hemolysis due to persistence of maternal Rh antibodies.
Similar content being viewed by others
Main
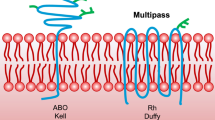
Despite improvements in the in utero diagnosis and treatment of severe Rh fetal isoimmune disease, postnatal anemia of a magnitude requiring RBC transfusions remains a common occurrence among affected infants(1). As a result of either, normal or pathologic hemolysis, Hb is degraded by the reticuloendothelial system to globin and heme(2). Degradation of the heme moiety in the heme pathway results in the cleavage of the porphyrin ring yielding equimolar amounts of iron, CO, and bilirubin(3). CO binds reversibly to Hb in circulating erythrocytes to form COHb. Although degradation of other heme proteins also contributes to endogenous CO and bilirubin production, this source contributes less than 25% to total CO production(4).
Previous reports of isoimmune hemolytic disease have documented increased concentrations of COHb and bilirubin in fetal blood at cordocentesis and at delivery, and/or in neonatal blood during the 1st wk of life(5–10). Although it has been presumed that the accentuation of early neonatal anemia, which regularly accompanies Coombs' test positive hemolytic disease, is the result of continued hemolysis(11, 12), data to substantiate this are lacking. Thus in the present study, we hypothesized that, during the early postnatal period when accentuated anemia occurs, severe Rh isoimmunization would result in increased COHb and bilirubin levels. To test this hypothesis, we compared biochemical and hematologic laboratory measurements in control subjects and in infants with ABO and severe Rh isoimmunization.
METHODS
Study subjects. Institutional review board approval for this protocol was obtained from the Ethics Committee at the University of Vienna, and informed consent was obtained from one or both parents.
Control neonates (n = 13) were eligible for enrollment if their mother's pregnancy was normal, if delivery occurred at term (i.e.≥37 wk), and if the infant's early neonatal course was normal. Infants with positive Coombs' tests or those with congenital abnormalities were excluded. Six control infants were studied while being monitored for congenital toxoplasma infection, which was eventually ruled out.
Entry criteria for infants with ABO immune hemolytic disease (n = 5) were identical to those of control infants. Because cord blood of infants of group O mothers is routinely Coombs' tested, ABO group infants were identified postnatally after this evaluation.
Subjects with Rh isoimmune disease (n = 13) were all identified prenatally based on positive maternal indirect Coombs' testing. Only infants with severe hemolytic disease were included. These included infants whose hematocrit at cordocentesis fell below the fetal transfusion threshold of 30% and/or infants who received double volume RBC exchange transfusions for hyperbilirubinemia in the 1 st wk of life. During the neonatal period 15 mL/kg top-up RBC transfusions (small volume packed erythrocyte transfusions) were administered when Hct or Hb levels fell below 24% and 80 g/L, respectively.
Hospital charts were reviewed, and the infants' families were interviewed to ascertain information relevant to CO exposure and to factors perturbing plasma bilirubin levels. Information that was sought included whether the mother had breast-fed and whether the infant experienced passive exposure to CO. This exposure was quantitated as hours per week exposure to cigarette smoking or to home heating units generating significant amounts of CO. In ascertaining passive CO exposure parents were asked not only to report on the smoking habits of all individuals living at the home, but were also interrogated as to the mode of transportation, traffic situation, and possible smoke exposure of their infants, on the way to the outpatient clinic, to detect perturbations due to short time exogenous exposure to CO sources before blood sampling.
Protocol design. In addressing the study's objective, 1.1-mL samples of heparinized venous blood were obtained at each of four monthly intervals beginning at 2 wk of age. The blood measurements made were selected to include relevant biochemical and hematologic parameters indicative of hemolysis. The duration of observation was chosen to include the period when simple top-up packed RBC transfusions are commonly administered to Rh-isoimmunized infants(11). To avoid introducing factors perturbing bilirubin and COHb, blood testing was delayed until 2 wk of age(9, 10). In addition, blood sampling was not done within 3 d after a top-up blood transfusions. With the exception of whole blood saved for COHb analysis (see below) samples not analyzed immediately were centrifuged, and plasma was frozen at -20 °C.
Laboratory analysis. Erythrocyte, leukocyte, and reticulocyte counts were performed using automated blood counters (Sysmex NE-5500 Automated Hematology Analyzer, Toa Medical Electronics, Kobe, Japan, and Sysmex R-1000 Automated Reticulocyte Analyzer). Plasma total bilirubin, plasma iron, and liver enzymes were measured spectrophotometrically using an autoanalyzer(Kodak Ektachem 700XR Analyzer, Eastman Kodak Co., Rochester NY). Plasma Epo was measured in triplicate using a sensitive and specific double antibody RIA as previously described(13).
COHb concentrations were determined on whole blood samples (120-140 μL) shipped to Stanford University. This was done using a sensitive gas chromatographic method within 1 mo of storage at 4 °C(14, 15). Briefly, 2 μL of blood were injected in triplicate into 2-mL septum-sealed, CO-free vials with 20 μL of 10%(wt/vol) K3Fe(CN)6 in 0.1 M potassium phosphate buffer, pH 6.0, containing 1% (wt/vol) saponin. The vials were incubated at 0 °C for at least 30 min but not longer than 1 h. CO liberated into the vial head space was injected into the gas chromatograph with a reduction gas detector model RGA2 (Trace Analytical, Inc., Menlo Park, CA). The CO was then separated from other compounds on a 68 × 0.53-cm (inner diameter) 13X molecular sieve column at 125 °C with a carrier gas flow rate of 30 mL of CO-free air/min. The analyzer was standardized before and after each run with volumes of standard gas mixture containing 10.0 μL CO/L of N2 (Airco Air and Specialty Gases, Santa Clara, CA). The within-day and between-day coefficients of variation for reference blood samples using this method were 3 and 8%, respectively(10). The minimum detectable CO concentration was 0.00005, where the COHb concentration was expressed as the fraction of the total Hb saturation. There was no correction done for environmental CO.
The concentration of Hb used for the COHb determinations was measured using a manual cyanmethemoglobin method (Kit No. 525, Sigma Chemical Co., St. Louis, MO)(16). Four microliters of blood, pipetted with a Hamilton gastight syringe in a Hamilton repeating dispenser (Hamilton Co., Reno, NV), was allowed to react with 2.0 mL of modified Drabkin's reagent for a minimum of 2 h at room temperature. The absorbance of the resultant cyanmethemoglobin was determined at 540 nm with a spectrophotometer (model UV-160, Shimadzu Scientific Instruments, Columbia, MD). The withinday and between-day coefficients of variation for reference blood samples using this method were 2.2 and 3.0%, respectively(10).
In a subset of Rh-isoimmunized patients, serial plasma samples were obtained for measurement of Rh antibody using a spectrophotometric autoanalyzer technique(17).
Data analysis. The mathematical expression, the fraction of COHb divided by the Hb concentration (COHb√Hb), was favored over that of COHb alone as it is a more informative indicator of the rate of hemolysis(18). This decision was based on the appreciation that the Hb to which CO binds forming COHb is not the Hb from which the CO was derived. Thus, the best way to assess the relative rate of hemolysis is to index CO production to Hb. Assuming similar CO elimination rates, individuals with the highest CO index can be understood to have produced the most CO relative to the immediate Hb for the interval up to that point in time.
Statistical analyses were performed using a microcomputer software program(StatView 4.5, Abacus Concepts, Inc., Berkeley, CA). Only two-tailed significance testing was used. Between-group comparisons were done using an unpaired t tests or the Mann-Whitney U test for normally and nonnormally distributed data as indicated. For within- and between-group comparisons over time, one-factor and two-factor ANOVA for repeated measures were used. Comparisons with significant ANOVA F values were subjected to post hoc examination using the Bonferroni procedure. Simple and multiple linear regression were used to examine for possible associations of study variables. Results are presented as the mean ± SEM. The α level selected for statistical significance was p< 0.05.
RESULTS
Control and ABO-isoimmunized infants did not differ in gestational age at birth, birth weight, breast-feeding, or exposure to environmental CO sources(Table 1). In contrast, infants with Rh isoimmunization had lower birth weights and were born at a younger gestational age. They tended to be bottle-fed and to have less exposure to passive CO from cigarette smoke or home heating units. None of the infants was exposed to exogenous CO or to medications known to perturb CO production in the hours immediately before blood sampling. Although the ratio of male to female infants was similar in the control and Rh-isoimmunized groups, the ABO group tended to include fewer female infants.
Peak bilirubin levels measured in the 1st wk of life before study enrollment tended to be higher in ABO and Rhisoimmunized infants when compared with the four control infants who were clinically jaundiced and therefore had plasma bilirubin levels measured. Nine of the 13 (69%) Rhisoimmunized infants received one or more postnatal top-up transfusions. One of the infants who underwent six in utero transfusions did not receive any transfusions postnatally. There were no deaths in any group.
Postnatal patterns of change for all study variables were compared among all three study groups for differences in absolute values (using ANOVA with post hoc testing) and for differences in postnatal patterns of change (using two-factor ANOVA for repeated measures). Because comparisons between control and ABO infants revealed no differences, data from these groups were combined for comparison with the Rh-isoimmunized group.
In examining the postnatal pattern of change in Hb concentration during the four study intervals, the combined control-ABO group differed significantly from the Rh-isoimmunized group (p < 0.0001)(Fig. 1a). Although there was a significant decline in Hb concentration in all groups from 2 to 6 wk of life (p < 0.05), Hb values at 2 and at 6 wk were significantly lower in the Rh isoimmune group relative to the combined control-ABO group. Lower Hb levels in the Rh-isoimmunized group at wk 2 and 6 occurred despite two-thirds of these infants having received simple RBC transfusions as treatment for anemia. By wk 10, Hb levels in the Rh-isoimmunized group increased to values that were similar to those of the combined control-ABO group.
Erythropoietic laboratory parameters determined at the four study intervals during the early postnatal weeks of life. Shown are:(a) Hb concentration, (b) plasma erythropoietin concentration, and (c) reticulocyte count. The three infant study groups are illustrated separately in each panel. The pattern of change over time in the Rh-isoimmunized group was significantly different from the other two groups for all three study variables (p < 0.001). Because there were no differences between control and ABO-isoimmunized groups, statistical data shown at the four intervals indicate comparisons made between the Rh-isoimmunized infants and a combined control and ABO-isoimmunized group. Mean ± SEM values are shown.
Although in all groups the postnatal patterns of plasma Epo levels and reticulocyte counts were reciprocal to that of Hb, the greatest excursions were observed in the Rh-isoimmunized group (Fig. 1,b and c). At wk 6 of age when the Rh-isoimmunized infants' Hb levels were at their nadir, this group had significantly higher plasma Epo levels and reticulocyte counts than either the ABO or control infants. Although plasma Epo levels in the Rh-isoimmunized group were significantly higher at wk 2, the tendency of these infants to have higher reticulocyte counts at wk 2 did not achieve statistical significance (p < 0.10).
The pattern of change in COHb√Hb among the three groups was significantly different over the four study intervals (p < 0.0001) (Fig. 2a). During wk 2 and 6, COHb√Hb was significantly greater in the Rh-isoimmunized group compared with the combined control-ABO group.
Laboratory indicators of hemolysis determined at the four study intervals during the early weeks of life. Shown are: (a) COHb√Hb and (b) total bilirubin concentration. The three infant study groups are illustrated separately in each panel. The pattern of change over time in the Rh-isoimmunized group was significantly different from the other two groups for both study variables (p < 0.001). Because there were no differences between control and ABO-isoimmunized groups, statistical data shown at the four intervals indicate comparisons made between the Rh-isoimmunized infants and a combined control and ABO-isoimmunized group. Mean ± SEM values are shown.
Although the pattern of change in total bilirubin during the period of study did not quite achieve statistical significance among the three groups(p < 0.07) (Fig. 2b), mean plasma bilirubin concentrations in the Rh group were significantly elevated at wk 2 and 6 compared with that of the combined control-ABO group. We cannot unequivocally rule out developmental causes as the explanation for the differences in bilirubin concentrations between the groups. Based on previous work demonstrating mean bilirubin levels of 94 μmol/L at wk 2 and 3 of age in immature infants, this is unlikely(19).
Examination of the remaining laboratory measurements between the groups failed to reveal any significant differences. These variables included plasma iron, lactate dehydrogenase, serum glutamic-oxaloacetic transaminase, and serum glutamicpyruvic transaminase. With the exception of a progressive decline in plasma iron concentration noted in all groups (p < 0.01), none of the other laboratory variables demonstrated a significant change.
Correlation analysis of pooled laboratory data from all four study intervals was used to examine the relationships of study variables within individual groups (Table 2). There was no association observed of Hb with COHb for either the Rh isoimmune group or the combined control-ABO group (data not shown). Total plasma bilirubin and COHb√Hb, however, were significantly associated in the Rh isoimmune group, but not in the combined control-ABO group. No significant relationship between Hb and bilirubin levels was observed in the Rh-isoimmunized infants (data not shown), most likely as a result of the RBC transfusions these infants received. In the combined control-ABO group, plasma Epo levels and Hb were inversely correlated. Significant relationships in this group were also observed between Hb and reticulocytes and between plasma Epo and reticulocyte counts.
After completion of the above laboratory measurements, four Rh-isoimmunized infants had serial plasma samples available for determination of Rh antibody concentrations. None had received an exchange transfusion during the postnatal period. The half-life of the Rh antibody calculated from the slope elimination curves of these four infants was consistent among them (14.3 d ± 4.3) and similar to the 12.5 d reported for Rh-negative pregnant women given i.v. Rh immune globulin(20) (Fig. 3).
Decline in Rh antibody concentration among four Rh isoimmunization infants (μg/mL) and mean data for a group of pregnant Rh-negative women treated antenatally with intravenous Rh immune globulin(percentage of the initial antibody concentration)(20). The lines represent the least square regression plots for individual infants and for mean maternal data.
DISCUSSION
This is the first study to report and to compare COHb and plasma bilirubin data measured consecutively over the first months of life in control infants and in infants affected by maternal Rh isoimmunization. Consistent with our hypothesis we observed that COHb and bilirubin determinations during the first 6 wk of life were elevated in infants with severe Rh isoimmunization. More specifically, this coincided with the period during which top-up RBC transfusions are commonly administered. Together these findings support speculation that the late anemia associated with Rh isoimmunization reflects a continuation of the low grade hemolytic process resulting from transplacentally acquired maternal anti-Rh IgG antibodies.
The hallmark of Rh isoimmune hemolytic disease in the fetus, and the primary pathophysiologic factor leading to fetal compromise and death, is anemia(1, 11). The severity of fetal anemia in Rh-isoimmunized pregnancies is directly associated with the elevated levels of fetal COHb and plasma bilirubin measured at cordocentesis(10). A significant association of the two latter indicators of hemolysis has also been reported among affected fetuses(6, 7, 10).
During the 1st wk of life, plasma bilirubin and whole blood COHb levels remain elevated in infants with hemolytic disease of the newborn(5, 6, 8, 21). In a study by Fällström and Bjure(22), elevated COHb levels noted in infants with Rh hemolytic disease on d 1 of life declined progressively over the subsequent 4 d. Of note, at the end of this period COHb levels in this group remained elevated relative to that of controls, 1.45%± 0.18 versus 0.77% ± 0.03, respectively. In the present study, we have extended the period of observation to the first several months of life. We observed that COHb levels in such infants continue their postnatal decline until becoming equivalent to control infants by 6-10 wk.
Because environmental CO exposure can have a profound influence COHb levels, the potential effect of exogenous CO sources was examined. Based on parental reporting, the Rh group of isoimmunized infants experienced less environmental exposure to CO than the control-ABO group, thus making it unlikely that exogenous CO sources were responsible for the higher COHb levels found in the Rh-isoimmunized group. Finding no differences in HbCO levels between the groups at the final two study intervals further suggests that exogenous CO was not the source of the HbCO differences.
Several features of the present study suggest that the differences observed in plasma bilirubin levels between the Rh-isoimmunized and control-ABO groups were conservative approximations. At wk 2 of study, plasma bilirubin levels in the combined control-ABO group were slightly elevated relative to values reported for term infants i.e., 30 versus 60 μmol/L(9). This slight discrepancy many have been due to a greater proportion of these infants being breast-fed. The observation that fewer of the Rh-isoimmunized infants were breast-fed would predispose this group to have lower bilirubin levels, leading to an underestimate of an already significant difference between the two groups at wk 2 and 6. Another factor that likely resulted in a lowering of the plasma bilirubin levels observed in the Rh-isoimmunized group was the postnatal exchange transfusions that nine of these infants received as therapy for icterus praecox.
The clinical course of late anemia associated with Rh isoimmunization in our study population was variable. A clear relationship between the number of intrauterine transfusions, the need for postnatal blood exchange transfusion, and the necessity for subsequent top-up transfusions was not evident. Nonetheless, it is notable that all nine postnatal top-up RBC transfusions administered for treatment of anemia were given before 7 wk of age, an interval consistent with reports of others(23–25). This period coincided precisely with that during which the study's primary indicators of hemolysis, COHb√Hb, and bilirubin, were significantly increased. If confirmed by others in a larger group of Rh isoimmune infants, this finding may be of value in defining the postnatal period after birth during which late anemia associated with Rh immunization is likely to require top-up transfusions.
Results of the regression analyses in the present study lend further support to the mechanism for the late anemia experienced by Rh-isoimmunized infants being the persistence of maternal IgG-induced hemolysis. The highly significant association observed between COHb and total bilirubin and between COHb√Hb and total bilirubin in the Rh group, but not in the combined control-ABO group, is evidence to support this. Although the anticipated increase in reticulocyte counts occurring as a normal response to anemia was observed among control and ABO infants, this was not found among Rh-isoimmunized infants. This was most likely attributable to the presence of maternally acquired anti-Rh IgG antibodies resulting in ineffective erythropoiesis(23, 24, 26). Although the rate of decline in anti-Rh antibodies from the plasma is consistent with maternally acquired antibodies as the etiology of neonatal hemolysis, it does not provide definitive proof. For ethical reasons, direct proof of this is not likely to be forthcoming in studies of human fetuses and infants. Indirect evidence from in vitro studies evaluating the effect of Rh antibody concentration and its binding affinity for fetal Rh-positive erythrocytes may be useful in addressing this issue.
In summary, increased COHb and plasma bilirubin levels were found among neonates with severe Rh isoimmune hemolytic disease during the first 6 wk of life. The close direct association of plasma bilirubin with COHb and COHb√Hb in the first 3-4 mo suggests that continued low grade hemolysis is the primary etiology for the accentuated late anemia commonly experienced by such infants. We speculate that the duration and severity of the late neonatal anemia associated with Rh isoimmune disease is determined by the concentration and affinity characteristics of transplacentally acquired maternal anti-erythrocyte IgG and the immunologic capacity for removing Rh antibody-coated erythrocytes.
Abbreviations
- CO:
-
carbon monoxide
- COHb:
-
carboxyhemoglobin
- COHb√Hb:
-
carboxyhemoglobin fraction divided by Hb concentration
- Epo:
-
erythropoietin
- RBC:
-
red blood cell
- Rh:
-
rhesus
- ANOVA:
-
analysis of variance
References
Weiner CP 1994 Fetal hemolytic disease. In: James DK, Steer PJ, Weiner CP, Gonik B (eds) High Risk Pregnancy: Management Options. WB Saunders, London, pp 783–801
Coburn RF, Williams WJ, White P, Kahn SB 1967 The production of carbon monoxide from hemoglobin in vivo. J Clin Invest 46: 346–356
Tenhunen R, Marver HS, Schmid R 1968 The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc Natl Acad Sci USA 61: 748–755
Berk PD, Blaschke TF, Scharschmidt BF, Waggoner JG, Berlin NI 1976 A new approach to quantitation of the various sources of bilirubin in man. J Lab Clin Med 87: 767–780
Ergaz Z, Gross D, Bar-Oz B, Arad I 1995 Carboxyhemglobin levels in neonatal jaundice treated with intravenous gammaglobulin. Vox Sang 69: 95–99
Fällström SP, Bjure J 1967 Endogenous formation of carbon monoxide in newborn infants. Acta Paediatr Scand 56: 365–373
Wranne L 1969 Studies on erythro-kinetics in infancy. XIV. The relation between anaemia and haemoglobin catabolism in Rh-haemolytic disease of the newborn. Acta Paediatr Scand 58: 49–53
Uetani Y, Nakamura J, Okamoto O, Yamazaki T, Vreman HJ, Stevenson DK 1989 Carboxyhemoglobin measurements in the diagnosis of ABO hemolytic disease. Acta Paediatr Jpn 31: 171–176
Maisels MJ 1994 Jaundice. In: Avery GB, Fletcher MA, Macdonald MG (eds) Neonatology: Pathophysiology and Management of the Newborn. JB Lippincott, Philadelphia, pp 630–725
Widness JA, Lowe LS, Stevenson DK, Vreman HJ, Weiner CP, Hayde M, Pollak A 1994 Direct relationship of fetal carboxyhemoglobin with hemolysis in alloimmunized pregnancies. Pediatr Res 35: 713–719
Zipursky A, Bowman JM 1993 Isoimmune hemolytic disease. In: Nathan R, Oski F (eds) Hematology of Infancy and Childhood. WB Saunders, Philadelphia, pp 44–73
Bowman JM 1989 Hemolytic disease (erythroblastosis fetalis). In: Creasy R, Resnik R (eds) Maternal-Fetal Medicine. WB Saunders, Philadelphia, pp 613–655
Georgieff MK, Landon MB, Mills MM, Hedlund BE, Faassen AE, Schmidt RL, Ophoven JJ, Widness JA 1990 Abnormal iron distribution in infants of diabetic mothers: spectrum and maternal antecedents. J Pediatr 117: 455–461
Vreman HJ, Kwong LK, Stevenson DK 1984 Carbon monoxide in blood: an improved microliter blood-sample collection system, with rapid analysis by gas chromatography. Clin Chem 30: 1382–1386
Vreman HJ, Stevenson DK, Zwart A 1987 Analysis for carboxyhemoglobin by gas chromatography and multicomponent spectrophotometry compared. Clin Chem 33: 694–697
Eilers RJ 1967 Notification of final adoption of an international method and standard solution for hemoglobinometry specifications for preparation of standard solutions. Am J Clin Pathol 47: 212–214
Bowman JM, Pollock JM, Biggins KR 1988 Antenatal studies and management of hemolytic disease of the neoborn. In: Greenwalt TJ(ed) Hematology: Blood Transfusion. Churchill Livingstone, New York, pp 163–212
Vreman HJ, Mahoney JJ, Stevenson DK 1995 Carbon monoxide and carboxyhemoglobin. Adv Pediatr 42: 303–334
Cohen RS, Durand DJ, Stevenson DK 1986 Serum bilirubin levels in very low birth weight infants during the first two months of life. J Perinatol 6: 259–261
Bowman JM, Pollock JM 1987 Failures of intravenous Rh immune globulin prophylaxis: an analysis of the reasons for such failures. Transfus Med Rev 1: 101–112
Maisels MJ, Pathak A, Nelson NM, Nathan DG, Smith CL 1971 Endogenous production of carbon monoxide in normal and erythroblastotic newborn infants. J Clin Invest 50: 1–8
Fällström SP, Bjure J 1968 Endogenous formation of carbon monoxide in newborn infants. III. ABO incompatibility. Acta Paediatr Scand 57: 137–144
Hyman CB, Sturgeon P 1955 Observations on the convalescent phase of erythroblastosis fetalis. Pediatrics 16: 15–23
Millard DD, Gidding SS, Socol ML, MacGregor SN, Dooley SL, Ney JA, Stockman JA 1990 Effects of intravascular, intrauterine transfusions on prenatal and postnatal hemolysis and erythropoiesis in severe fetal isoimmunization. J Pediatr 117: 447–454
Ebbesen F 1979 Late anemia in infants with rhesus haemolytic disease treated with intensive phototherapy. Eur J Pediatr 130: 285–290
Giblett ER, Varela JE, Finch CA 1956 Damage of the bone marrow due to Rh antibody. Pediatrics 17: 37–44
Acknowledgements
The authors express their appreciation to Mark Hart and G. Hatlauf for secretarial assistance, Birgit Panzenböck and Robert Schmidt for laboratory assistance, to Maria Babich for chart review and interaction with families, to Dr. Leon Burmeister for statistical advice, and to Dr. John M. Bowmann and Janet Pollock of the Rh Laboratory, Health Science Centre, Winnipeg, Canada, for the Rh antibody measurements.
Author information
Authors and Affiliations
Additional information
Supported in part by National Institutes of Health Grants HD14426, RR00070, and HL46925, and by The Mary L. Johnson Research Fund.
Rights and permissions
About this article
Cite this article
Hayde, M., Widness, J., Pollak, A. et al. Rhesus Isoimmunization: Increased Hemolysis during Early Infancy. Pediatr Res 41, 716–721 (1997). https://doi.org/10.1203/00006450-199705000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199705000-00018
This article is cited by
-
Jack Widness: the importance of connections
Pediatric Research (2018)
-
Effect of Hematocrit on Exhaled Carbon Monoxide in Healthy Newborn Infants
Journal of Perinatology (2005)