Abstract
In utero breathing activity is present periodically, but it must become continuous at birth. We investigated the effect of hypercapnia and of hypercapnia combined with central cooling on fetal breathing in seven chronically instrumented fetal lambs of 131-134-d gestation, using an extracorporeal membrane oxygenation (ECMO) system to control fetal blood gases and fetal temperature. During fetal hypercapnia (from a partial pressure of arterial CO2 (Paco2) 6.18 ± 0.11 kPa to Paco2 7.39± 0.15 kPa) frequency, amplitude, and incidence of fetal breathing movements during low voltage electrocortical activity (LV ECoG) increased significantly compared with isocapnic control on ECMO, but breathing remained absent during high voltage electrocortical activity (HV ECoG). During hypercapnia accompanied by central cooling (Paco2 7.90 ± 0.13 kPa, temperature decreased by 2.1°C) there were similar changes in fetal breathing movements during LV ECoG, but in four out of seven fetuses fetal breathing movements continued throughout HV ECoG. Hypercapnia accompanied by central cooling can thus override the inhibitory effects of HV ECoG on fetal breathing movements. This may be due to changes in sensitivity to CO2 produced by an increase in afferent input to the CNS.
Similar content being viewed by others
Main
In the sheep fetus in utero, after maturation of electrocortical activity in late gestation, breathing activity is present during LV ECoG and is inhibited during HV ECoG(1, 2). This inhibition must be removed or overridden at birth to allow the establishment of continuous breathing. The mechanisms involved in the initiation of continuous breathing at birth are not completely understood. It is known that Paco2 increases after cord occlusion at birth and that this is important for the initiation of breathing(3, 4). Fetal hypercapnia, obtained by increasing maternal Paco2, produces an increase in incidence, amplitude, and frequency of fetal breathing movements, but they still remain associated with LV ECoG. During HV ECoG associated with sustained contractions of nuchal muscles, breathing movements are inhibited(5–9). Also, in human fetuses during hypercapnia there is an increase in fetal breathing activity, but it is still present only periodically(10, 11).
Mechanisms involved in the inhibition of breathing during HV ECoG are not known. One possibility is that changes in sensitivity to CO2 play a role. Johnston et al.(12) described continuous breathing activity during hypercapnia, but not during normocapnia, in fetal lambs with lesions in the rostral lateral pons. It could be speculated that these lesions liberated the respiratory centers from inhibitory influences present during HV ECoG. Thus it may be that a decrease in sensitivity to CO2 occurs during HV ECoG in intact animals, resulting in the loss of respiratory drive and apnea. An extension of this idea is that an increase in CO2 sensitivity occurs at birth, allowing breathing to occur in both low voltage and high voltage states. The effect on CO2 sensitivity may be initiated by a decrease in fetal skin temperature, increasing afferent input to the CNS. This idea is supported by the continuous breathing activity observed after a decrease in cutaneous fetal temperature(13). This mechanism could play a role at birth when there is a combination of hypercapnia and an increased afferent input, including that from a decrease in temperature.
A previous study showed that a decrease in fetal core temperature produced by a cooling coil passed down the fetal esophagus failed to produce continuous breathing(13). In that study there was no change in fetal Paco2 and we speculated that the cold internal coil passing through the pharynx and larynx could have stimulated upper airway receptors, inhibiting breathing. We therefore decided to adopt a different approach by using an ECMO system with which blood gases and blood temperature can be changed. We tested the hypothesis that the association of hypercapnia with central cooling could override the central inhibition of fetal breathing normally occurring during HV ECoG, resulting in continuous breathing activity. In this report we provide evidence that supports this hypothesis. Hence, the combination of cooling and hypercapnia is an important mechanism involved in the initiation of continuous breathing at birth.
METHODS
This project was reviewed and approved by the animal care committee of University of Limburg. Experiments were performed on unanesthetized chronically instrumented fetal sheep in utero. With sterile technique, seven pregnant sheep were operated at 128-132-d gestational age after 48-h fasting, under general anesthesia (thiopentone 1 g/70 kg i.v. for induction, and 0.8% halothane in 50% nitrous oxide and 50% oxygen for maintenance). A midline laparotomy was performed, and the uterus was partly exteriorized to allow access to the fetal head. The uterus was opened, and the fetus was exteriorized to perform a thoracotomy at the level of the 10th intercostal space. A pair of wire electrodes (AS 632 Cooner Wire, Chatsworth, CA) were sewn into the diaphragm for recording EMG activity. Thermistors (PT 100 sensors, Murata, Nijkerk Electronics, The Netherlands) were placed in the pleural cavity to measure fetal core temperature. Catheters were placed in the right axillary artery and right carotid artery (directed toward the head) to measure blood pressure and heart rate and for fetal blood sampling (Radiometer ABL3, Copenhagen), and a catheter was placed in the right axillary vein to infuse antibiotics and fluids. Wire electrodes for recording ECoG activity were implanted bilaterally on the fetal parietal dura through holes drilled in the skull. A common electrode was sewn in adjacent tissue. Wire electrodes were sewn into a nuchal extensor muscle to record nuchal EMG and into periorbital muscles to record eye movements (electrooculogram, five fetuses). A catheter was placed in the fetal trachea to measure intratracheal pressure. For the ECMO system, two catheters (Biomedicus, Eden Prairie, MN) were placed: one for drainage to the ECMO system (12-14 French) was advanced 10 cm into the right external jugular vein to the right atrium, and one for return of oxygenated blood to the fetus (8-10 French) was advanced 3 cm into the right carotid artery toward the aortic arch. These catheters were connected to 60-cm tubes of 10-mm diameter capped at the end and filled with heparinized saline(50 U/mL). These tubes permitted later connection to the ECMO system. All catheters, tubing, and electrode cables were exteriorized through a small incision in the flank of the ewe. Catheters were placed in the ewe's carotid artery and jugular vein for blood sampling or infusing antibiotics. The ECMO catheters were flushed twice/d with 5 mL of heparinized saline (50 U/mL), and both catheters were connected to a continuous infusion of 1 mL/h heparinized saline (50 U/mL). Antibiotics were given daily to the ewe (ampicillin, 1 g/d) and to the fetus (ampicillin, 150 mg/kg/d, and gentamicin, 5 mg/kg/d) until the end of experimentation.
ECMO. The ECMO system used was as previously described(14–16). In brief, it consisted of 0.65-cm inside diameter silastic tubing connected to a venous reservoir, a peristaltic pump, and a membrane lung (Scimed, 0.8 m2, MN). The circuit was enclosed in a thermostatically controlled box which maintained blood temperatures at 39.5°C. Blood was drained from the right atrium via the jugular vein, and returned to the aorta through the carotid catheter. The blood gases were set by altering the gases supplied to the membrane lung. The ECMO circuit was primed with 350 mL of freshly citrated adult sheep blood. The blood in the circuit was kept at 39.5°C, and blood gases and pH were held within the fetal physiologic range. The membrane lung was supplied with a gas mixture (approximately 0.4 L/min O2, 1.5 L/min N2, and 0.1 L/min CO2) at a total flow rate of 2.0 L/min. Heparin was infused to maintain activated coagulation time at 350-450 s. After connecting the ECMO circuit to the fetus, the pump flow was started at 50 mL/min and then increased slowly to approximately 150-200 mL/min within 15 min.
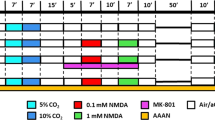
Experimental protocol. Recordings were obtained before connecting the animal to ECMO, during periods on ECMO, during hypercapnia periods, and during periods of hypercapnia accompanied with central cooling. Baseline recordings (Hewlett Packard; 7758 A recorder, paper speed of 1 cm/min) of ECoG activity, integrated diaphragmatic EMG and integrated nuchal EMG, electrooculogram, tracheal and blood pressure, heart rate, and core temperature were started on the 2nd d postsurgery before connection to the ECMO system. On the 3rd d postsurgery, when the fetal blood gases were within the normal range and the incidence of fetal breathing movements was normal(1), the fetuses were connected to the ECMO system maintaining fetal temperature, blood gases, and pH. Recordings taken within 1 h of starting ECMO perfusion were not used for analysis.
Fetal hypercapnia was obtained by increasing the CO2 concentration of the gas flow to the membrane lung. Hypercapnia was defined as a fetal Paco2 at least 1 kPa higher than baseline. The core temperature of the fetus was reduced by 1-3°C by decreasing the circuit blood temperature. This was done by turning off the heating element of the box containing the circuit and placing ice around the membrane lung and in contact with the circuit. It took 20-30 min to decrease fetal central temperature by 1°C at a pump flow of 200 mL/min. Whenever fetal Paco2 did not increase significantly from control, CO2 flow to the membrane lung was increased to obtain the desired Paco2 level. Experiments did not start until the desired conditions, i.e. Paco2 increased 1 kPa, central temperature decreased 1°C, had been reached.
The experimental protocol was divided into three periods during ECMO:1) control periods, 2) hypercapnia periods followed by return to normocapnia, and 3) hypercapnia periods associated with central cooling. There was a minimum control period on ECMO of 2 h. Hypercapnia and hypercapnia associated with central cooling experimental periods were at least 1 h long (except in one fetus in which the experiment was 30 min). Fetal blood gases were taken approximately every 15 min during a control or experimental period.
Analysis of results. Fetal blood gases were averaged to derive values for each hour. Both integrated EMG activity of the diaphragm and the negative tracheal pressure deflections represented respiratory output. Fetal breathing was defined when activity of the diaphragm and/or repeated negative deflections of tracheal pressure were present for at least 1 min (>6 breaths/min). Fetal ECoG was analyzed visually into LV ECoG and HV ECoG activity. The incidence per hour and length of periods of LV ECoG activity were analyzed, as were the incidence of fetal breathing movements per hour, the incidence of fetal breathing movements during LV ECoG, and the frequency and amplitude of fetal breathing movements. Frequency of fetal breathing movements per minute was analyzed by counting all breaths after replaying the tape onto the chart recorder at a higher paper speed. The amplitude was analyzed by measuring the area under the curve of the integrated EMG activity of the diaphragm and dividing it by the duration of the period (Quantimed 570, Leica). The area under the integrated nuchal EMG activity was determined in the same way. The amplitude of breathing movements and the amount of nuchal muscle activity were expressed as a percentage of the mean breath amplitude and the mean nuchal muscle activity, respectively, measured during control periods on ECMO for each fetus. Mean arterial blood pressure and heart rate were analyzed every 10 min and averaged over the experimental periods. Fetal blood gases and pH were analyzed from fetal arterial blood samples with a Radiometer ABL3 (values converted to 39.5°C during control, during cooling periods fetal blood gases were corrected to fetal central temperature).
All data are given as mean ± SEM. n in statistical analysis was the number of fetuses, repeated trials on individual fetuses being averaged before statistical analysis. The Friedman and Wilcoxon signed rank tests were used for statistical comparison of data between hypercapnia and control periods and between hypercapnia associated with cooling and hypercapnia periods.
RESULTS
Experiments were performed on seven fetal lambs, at gestational age 131-134 d. Baseline recordings before connection to the ECMO system were obtained at least 48 h (range 55-70 h) after surgery for a duration of at least 11 h. Fetal blood gases and pH before connection to the ECMO system were: pH 7.36± 0.01, Paco2 5.84 ± 0.14 kPa, Pao2 3.15 ± 0.23 kPa. Mean arterial blood pressure was 67.7 ± 3 mm Hg, and heart rate was 163.8 ± 8 beats/min. Nuchal EMG was always associated with HV ECoG. Rapid eye movements (n = 5) were always associated with LV ECoG and fetal breathing movements. During the baseline, LV ECoG occurred 52.5± 2.0% of the time. Fetal breathing movements were present 36.3± 3.0% of the total time and 69.4 ± 5.4% of the time during LV ECoG.
Control periods on ECMO (n = 7, experiments = 17). On the 3rd d postsurgery the fetuses were connected to the ECMO system. Physiologic variables are reported in Table 1. Nuchal EMG activity was associated with HV ECoG; rapid eye movements were associated with LV ECoG and fetal breathing movements.
Hypercapnia periods on ECMO (n = 7, experiments = 15). Nuchal EMG activity was associated with HV ECoG, and the area of nuchal muscle activity was not different from control on ECMO. Compared with control periods on ECMO there was a significant increase in amplitude, frequency, and incidence of fetal breathing movements during LV ECoG (Table 1). However, breathing movements remained periodic, associated with rapid eye movements and LV ECoG (Fig. 1).
Intrauterine recording of a fetus at 132-d gestation, connected to the ECMO system, of approximately 1 h during hypercapnia. Tracings are, from the top, electrocortical activity, integrated nuchal EMG, integrated diaphragm EMG (two traces), blood pressure, and heart rate. Blood gas and pH samples were taken at the indicated times, CO2 flow was increased at the time indicated. Note that fetal breathing movements were present only during LV ECoG, even during hypercapnia, and were associated with rapid eye movements. Nuchal muscle activity was present during HV ECoG.
Hypercapnia accompanied by central cooling on ECMO (n = 7, experiments = 7). In five out of seven experiments, fetal Paco2 did not increase significantly after 20-30 min while fetal central temperature was decreased by 1°C. In these experiments fetal hypercapnia was produced by increasing CO2 flow to the membrane lung. In the remaining two experiments, fetal Paco2 increased to a hypercapnic level without increasing CO2 flow to the membrane lung.
In the experiments where hypercapnia was combined with central cooling, central temperature decreased by a mean of 2.1°C, and fetal Paco2 increased to 7.90 ± 0.13 kPa. Nuchal muscle activity was present during both ECoG states, with increased amplitude during HV ECoG (Fig. 2). The amount of nuchal muscle activity was significantly increased compared with hypercapnia on ECMO(Table 1). Rapid eye movements were present during LV ECoG. In three out of seven fetal lambs, breathing activity remained associated with LV ECoG. In the other four fetal lambs breathing activity was present continuously during both HV ECoG and LV ECoG (Fig. 2). However, the frequency of fetal breathing movements decreased significantly compared with those found in hypercapnia alone(Table 1). There was no change in the amplitude of breathing movements, and they were still modulated by electrocortical activity, resulting in a lower frequency during HV ECoG than during LV ECoG. This was present for the time that hypercapnia and central cooling were allowed (1 h).
Intrauterine recording of a fetus at 132-d gestation connected to the ECMO system of approximately 1 h during hypercapnia associated with central cooling. Tracings are, from the top, electrocortical activity, integrated nuchal EMG, integrated diaphragm EMG (two traces), blood pressure, and heart rate. Blood gas and pH samples were taken at the time indicated. Note that fetal breathing movements continued during HV ECoG. Nuchal muscle activity was present continuously. Both were still modulated by electrocortical activity.
COMMENT
The incidence, frequency, and amplitude of fetal breathing movements during LV ECoG increased significantly during hypercapnia, as expected(5). There was no change in incidence or length of periods of LV ECoG either during hypercapnia or during hypercapnia accompanied by central cooling. During hypercapnia with central cooling, there was an increase in nuchal muscle activity, blood pressure, and heart rate, and a decrease in rate of fetal breathing movements. Furthermore, breathing activity became continuous in four out of seven fetal lambs. These results show that the association of hypercapnia with central cooling can override the inhibition of fetal breathing movements normally present during HV ECoG, resulting in continuous breathing activity.
As previously discussed, the use of ECMO could introduce new variables which might change fetal behavior(14–16). However, during ECMO there was a normal incidence of LV ECoG and fetal breathing movements, and rapid eye movements were associated with LV ECoG and nuchal muscle activity with HV ECoG: all this constitutes normal fetal behavior. It is therefore unlikely that the use of extracorporeal circulation by itself influenced our observations. The great advantage of the technique is the possibility of controlling fetal temperature and blood gases directly, independently of the ewe or the placenta.
In utero, after maturation of electrocortical activity fetal breathing movements and rapid eye movements are normally present only during LV ECoG, and nuchal EMG activity is present during HV ECoG and absent during LV ECoG(1, 17, 18). Hypercapnia is known to stimulate fetal breathing movements(5–9, 17, 19, 20), thus our finding that fetal hypercapnia produced with ECMO resulted in an increase in frequency and amplitude and incidence of fetal breathing movements during LV ECoG is in agreement with earlier studies. During these hypercapnia periods there was no change in fetal behavior, as seen from the absence of a change in the incidence or length of periods of LV ECoG, eye movements remaining associated with LV ECoG and nuchal EMG with HV ECoG. However, at variance with a previous report(5) we found that the incidence of LV ECoG during fetal hypercapnia did not increase. In this study hypercapnia was induced by maternal hypercapnia, it may be that the increase in incidence of LV ECoG was due to the release of substances from the placenta or the ewe(21).
During both hypercapnia alone and that accompanied by central cooling we found an increase in the amplitude of fetal breathing, but during the latter there was a decrease in the frequency of breathing movements. This lack of an association between the fall in frequency and an increase in amplitude suggests that the effect on frequency is not due to a stimulation of pulmonary stretch receptors(22). We favor the view that, during cooling periods, the decrease in frequency is related to decreased metabolic demand(23). Fetal breathing movements were not only influenced by temperature but still clearly modulated by electrocortical activity, because the frequency of breathing movements was lower during HV ECoG than during LV ECoG. This reflects the difference in the control of fetal breathing movements during LV ECoG and HV ECoG. Similarly, it is reported that postnatally breathing movements are more influenced by metabolic influences during HV ECoG and by behavioral influences during LV ECoG(24).
Hypercapnia alone was not sufficient to initiate respiratory activity during HV ECoG, as reported earlier(7, 19, 20, 25). The mechanism for this inhibition of fetal breathing movements during HV ECoG is not understood, but clearly it is not due simply to the absence of chemical drive to breathe. There is evidence that additional peripheral input, e.g. electrical stimulation of the sciatic nerve(26) or decreasing cutaneous fetal temperature(13), can produce continuous fetal breathing. In four out of seven fetuses, breathing activity became continuous when hypercapnia was accompanied by central cooling. This suggests that additional afferent input produced by central cooling might change the balance of central inhibitory and excitatory processes, causing an increase in the sensitivity to CO2. We cannot explain why breathing did not become continuous in all experiments, because there was no difference in the degree of decrease of central temperature, in the amount of nuchal muscle activity, or in the level of fetal Paco2. All this suggests that breathing activity in utero is under delicate control, perhaps dependent on subtle changes in CO2 sensitivity. Furthermore, it could be speculated that the presence of continuous breathing at birth is due to changes in CO2 sensitivity produced by increased afferent input at that time.
Previous attempts to induce continuous breathing in utero by decreasing central temperature using a cooling coil passed through the oropharynx were unsuccessful(13). One possible explanation for this could be the stimulation of upper airway receptors by the low temperature of the coil which may have inhibited breathing activity or because the fetuses remained normocapnic. Further indication that continuous fetal breathing is dependent on the level of Paco2 is provided by our previous finding(27) that breathing stimulated by cooling and hypercapnia becomes intermittent again when the Paco2 is decreased to normocapnic or hypocapnic levels. In the present study the association of central cooling with hypercapnia was essential for producing continuous breathing, because hypercapnia alone did not result in continuous breathing. Further evidence for the influence of temperature on CO2 sensitivity is provided by experiments on newborn animals that show a decreased respiratory response to CO2 in a warmer environment(28) (Malcolm and Henderson-Smart, personal communication).
It is of interest that central hypothermia did not change the fetal ECoG pattern. Nuchal muscle activity was increased but still modulated by LV ECoG. Finally, there was a significant increase in blood pressure and heart rate during hypercapnia combined with central cooling, probably due to an increase of catecholamine levels(29, 30).
In summary, fetal hypercapnia produced directly by ECMO results in a significant increase in amplitude, frequency, and incidence of fetal breathing movements during LV ECoG but no increase in incidence of LV ECoG. Central cooling combined with hypercapnia could override the inhibition during HV ECoG, resulting in continuous breathing. We speculate that cooling increased afferent input to the brainstem, changing the CO2 sensitivity and overriding the inhibition during HV ECoG. Further studies are being conducted to characterize this mechanism further, as it may be essential for the initiation of continuous breathing at birth.
Abbreviations
- ECMO:
-
extracorporeal membrane oxygenation
- HV ECoG:
-
high voltage electrocortical activity
- LV ECoG:
-
low voltage electrocortical activity
- Paco2:
-
partial pressure of arterial CO2
- Pao2:
-
partial pressure of arterial O2
- EMG:
-
electromyography
References
Dawes GS, Fox HE, Leduc BM, Liggins GC, Richards RT 1972 Respiratory movements and rapid eye movement sleep in the foetal lamb. J Physiol 220: 119–143.
Dawes GS, Gardner WN, Johnston BM, Walker DW 1983 Breathing in fetal lambs: the effect of brain stem section. J Physiol 335: 535–553.
Blanco CE, Martin CB, Hanson MA, McCooke HB 1987 Determinants of the onset of continuous air breathing at birth. Eur J Obstet Gynecol Reprod Biol 26: 175–182.
Berger PJ, Horne RSC, Soust M, Walker AM, Maloney JE 1990 Breathing at birth and the associated blood gas and pH in the lamb. Respir Physiol 82: 251–266.
Boddy K, Dawes GS, Fisher R, Pinter S, Robinson JS 1974 Foetal respiratory movements, electrocortical and cardiovascular responses to hypoxaemia and hypercapnia in sheep. J Physiol 243: 599–618.
Chapman RLK, Dawes GS, Rurak DW, Wilds PL 1980 Breathing movements in fetal lambs and the effect of hypercapnia. J Physiol 302: 19–29.
Ritchie JWK, Lakhani K 1980 Fetal breathing movements in response to maternal inhalation of 5% carbon dioxide. Am J Obstet Gynecol 136: 386–388.
Bowes G, Wilkinson MH, Dowling M, Ritchie BC, Brodecky V, Maloney JE 1981 Hypercapnic stimulation of respiratory activity in unanesthetized fetal sheep in utero. J Appl Physiol 50: 701–708.
Dawes GS, Gardner WN, Johnston BM, Walker DW 1982 Effects of hypercapnia on tracheal pressure, diaphragm and intercostal electromyograms in unanesthetized fetal lambs. J Physiol 326: 461–474.
Connors G, Hunse C, Carmichael L, Natale R, Richardson B 1988 The role of carbon dioxide in the generation of human fetal breathing movements. Am J Obstet Gynecol 158: 322–327.
Connors G, Hunse C, Carmichael L, Natale R, Richardson B 1989 Control of fetal breathing in the human fetus between 24 and 34 weeks' gestation. Am J Obstet Gynecol 160: 932–938.
Johnston BM, Gluckman PD 1989 Lateral pontine lesions effect central chemosensitivity in unanesthetized fetal lambs. J Appl Physiol 67: 1113–1118.
Gluckman PD, Gunn TR, Johnston BM 1983 The effect of cooling on breathing and shivering in unanesthetized fetal lambs in utero. J Physiol 343: 495–506.
Kuipers IM, Maertzdorf WJ, de Jong DS, Hanson MA, Blanco CE 1994 The effect of mild hypocapnia on breathing and behavior in unanesthetized normoxic fetal lambs. J Appl Physiol 76: 1476–1480.
Kuipers IM, Maertzdorf WJ, de Jong DS, Hanson MA, Blanco CE 1994 The effect of maternal hypoxemia on behavior in unanesthetized normoxic or mildly hyperoxic fetal lambs. J Appl Physiol 76: 2535–2540.
Kuipers IM, Maertzdorf WJ, de Jong DS, Hanson MA, Blanco CE 1992 Fetal breathing is not initiated after cord occlusion in the unanesthetized fetal lamb in utero. J Dev Physiol 17: 233–240.
Clewlow F, Dawes GS, Johnston BM, Walker DW 1983 Changes in breathing, electrocortical and muscle activity in unanaesthetized fetal lambs with age. J Physiol 341: 463–476.
Ioffe S, Jansen AH, Chernick V 1987 Maturation of spontaneous fetal diaphragmatic activity and fetal response to hypercapnia and hypoxemia. J Appl Physiol 62: 609–622.
Jansen AH, Ioffe S, Russell BJ, Chernick V 1982 Influence of sleep state on the response to hypercapnia in fetal lambs. Respir Physiol 48: 125–142.
Rigatto H, Lee D, Davi M, Moore M, Rigatto E, Cates D 1988 Effect of increased arterial CO2 on fetal breathing and behavior in sheep. J Appl Physiol 64: 982–987.
Faucher DJ, Laptook AR, Porter JC, Rosenfeld CR 1991 Effects of acute hypercapnia on maternal and fetal vasopressin and catecholamine release. Pediatr Res 30: 368–374.
Blanco CE, Martin CB, Hanson MA, McCooke HB 1987 Breathing activity in fetal sheep during mechanical ventilation of the lungs in utero. Eur J Obstet Gynecol Reprod Biol 26: 175–182.
Osborne S, Milsom WK 1993 Ventilation is coupled to metabolic demands during progressive hypothermia in rodents. Respir Physiol 92: 305–318.
Phillipson EA, Bowes G 1986 Control of breathing during sleep. In: Fishman AP, Cherniack NS, Widdicombe JG (eds) Handbook of Physiology, Section 3: The Respiratory System, Vol. II, Part 2. American Physiological Society, Bethesda, MD, pp 649–689.
Walker AM, Oakes GK, Ehrenkranz R, McLaughlin M, Chez RA 1976 Effects of hypercapnia on uterine and umbilical circulations in conscious pregnant sheep. J Appl Physiol 41: 727–733.
Moss IR, Scarpelli EM 1979 Generation and regulation of breathing in utero: fetal CO2 response test. J Appl Physiol 47: 527–531.
Kuipers IM, Maertzdorf WJ, de Jong DS, Hanson MA, Blanco CE 1994 The effect of central cooling in unanesthetized fetal lambs: the role of CO2 . Pediatr Res 35:A408.
Wanatabe T, Kumar P, Hanson MA 1993 Effects of warm environmental temperature on the gain of the respiratory chemoreflex in the kitten. J Physiol 459: 336P
Sidi D, Kuipers JRG, Heymann MA, Rudolph AM 1983 Effects of ambient temperature on oxygen consumption and the circulation in newborn lambs at rest and during hypoxemia. Pediatr Res 17: 254–258.
Gunn TR, Johnston BM, Iwamoto HS, Fraser M, Nicholls MG, Gluckman PD 1985 Haemodynamic and catecholamine responses to hypothermia in the fetal sheep in utero. J Dev Physiol 7: 241–249.
Acknowledgements
The authors thank Jan Geilen, Ton van den Bogaard, May Bost, Joyce Suyk, Frans Slangen, and Peter Franssen for the technical assistance and for the animal care.
Author information
Authors and Affiliations
Additional information
Supported by a grant (900-519-105) from the Netherlands Organization for Scientific Research (NWO). M.A.H. is supported by the Wellcome Trust.
Cardiothoracic Surgery, and Extra Corporeal Circulation, London, United Kingdom
Rights and permissions
About this article
Cite this article
Kuipers, I., Maertzdorf, W., De Jong, D. et al. The Effect of Hypercapnia and Hypercapnia Associated with Central Cooling on Breathing in Unanesthetized Fetal Lambs. Pediatr Res 41, 90–95 (1997). https://doi.org/10.1203/00006450-199701000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199701000-00014