Abstract
We hypothesized that treatment of very low birth weight premature infants with r-HuEPO would increase erythrocyte incorporation and gastrointestinal absorption of iron. Infants with birth weights ≤1.25 kg and gestational ages <31 wk were randomized to receive 6 wk of 500 U of r-HuEPO/kg/wk (epo group, n = 7) or placebo (placebo group, n = 7). All infants received daily enteral supplementation with 6 mg of elemental iron per kg. An enteral test dose of a stable iron isotope, 58Fe, was administered after the 1st (“early dosing”) and 4th (“late dosing”) wk of treatment. Mean (±SD) erythrocyte incorporation of the dose of 58Fe administered determined 2 wk after early dosing was significantly greater in the epo group compared with the placebo group (4.4%± 1.6 versus 2.0 ± 1.4%, p = 0.013). In contrast, after late 58Fe dosing, there was no difference between groups in incorporation (3.8 ± 1.6% versus 5.5 ± 2.7%). Within the epo group, percentage erythrocyte incorporation of58 Fe did not differ between early and late dosing, whereas in the placebo group it increased 3-fold (p < 0.01). Percentage absorption of 58Fe was not different between the epo and placebo groups after both early dosing (30 ± 22% versus 34 ± 8%) and late dosing (32 ± 9% versus 31 ± 6%). Absorption of nonlabeled elemental iron and 58Fe were significantly correlated with one another. The percentage of the absorbed 58Fe dose incorporated into Hb was not different between groups. We conclude that, although erythropoietin treatment stimulates erythrocyte iron incorporation in premature infants, it has no effect on iron absorption at the r-HuEPO dose studied.
Similar content being viewed by others
Main
Anemia occurring among very low birth weight premature infants during the first weeks and months of life is a prevalent and important clinical problem. Treatment of this condition with r-HuEPO has been suggested as a means of reducing the large number of erythrocyte transfusions these infants typically receive(1, 2). Although previous studies have demonstrated that r-HuEPO is capable of stimulating erythropoiesis in premature infants(3), two large multicenter clinical trials have found only modest reductions in the number of erythrocyte transfusions received by treated infants(4, 5).
Among the possible causes for the low clinical efficacy of r-HuEPO is the limited availability of iron(6–8). In epo-treated adults, the importance of adequate iron stores and iron availability is well recognized. Because the bulk of iron acquired in fetal life is laid down during the last trimester when growth is rapid, premature infants are born with disproportionately low body iron stores, thus increasing their dependence on an adequate supply of exogenous iron.
Although several studies have assessed enteral absorption and erythrocyte incorporation of iron in premature infants(9, 10), little is known about the effect of epo treatment on these parameters of iron metabolism. Thus the objective of the present study was to examine the effect of erythropoietin treatment on iron absorption and incorporation in premature infants. We hypothesized that epo treatment would increase both gastrointestinal absorption and erythrocyte incorporation of iron. This was assessed during our institution's participation in a multicenter placebo-controlled blinded trial of r-HuEPO(5). As per the multicenter protocol, all infants received daily supplements of 6 mg of elemental iron per kg. Iron absorption and erythrocyte incorporation were determined after enteral administration of a test dose of 58Fe, a stable isotope of iron. All infants were studied twice: once at the end of the 1st wk of epo treatment (“early dosing”) and again at the end of wk 4 (“late dosing”).
METHODS
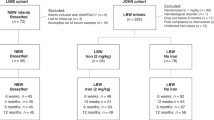
Study design. The study included 14 infants who comprised the University of Iowa cohort of the U.S. Collaborative Erythropoietin Multicenter Study(5). This 11-center study used a randomized double-blind, placebo-controlled experimental design with stratification by birth weight. Infants received r-HuEPO or placebo for 6 wk. The primary study outcome of the multicenter study was the number of erythrocyte transfusions, with various hematologic parameters serving as secondary outcomes. The study protocols (i.e. the collaborative and present iron studies) were approved by the University of Iowa Committee on Research Involving Human Subjects, and informed written permission was obtained from one or both parents.
Under the multicenter study protocol, seven Iowa infants were assigned to receive placebo (placebo group) and seven to receive r-HuEPO (epo group). On two separate occasions, i.e. after 1 wk of treatment and again after 4 wk of treatment, a stable, nonradioactive isotope of iron (58Fe) was administered enterally followed by collection of stools for 10 d and sampling of blood at 3 consecutive weekly intervals. We thereby tested our hypotheses that epo treatment leads to increased absorption of ingested iron and increased incorporation of iron into erythrocytes.
Subjects and feedings. Eligibility and transfusion criteria were identical to those of the multicenter study(5). Eligibility required birth weight ≤1250 g, gestational age <31 wk, postnatal age between 7 and 42 d, hematocrit <40%, phlebotomy losses<7.5 mL during the preceding week, stable respiratory status (fractional concentration of inspired O2 ≤ 0.3 and O2 saturation ≥ 85% by pulse oximetry), mean airway pressure of ≤8 cm H2O if on assisted ventilation, and caloric intake ≥60 kcal/kg/d for ≥2 d with ≥50% of calories received enterally. Infants were not eligible if they had received erythrocyte transfusions within 5 d, if they had experienced severe disease or had a congenital malformation of a major organ, seizures, anemia due to factors other than phlebotomy losses and prematurity, intracranial hemorrhage≥ grade III, or infection. Uniform criteria for erythrocyte transfusion based on hematocrit and clinical condition were applied(5).
With the exception of iron and vitamin supplementation, management of fluids and nutrition was not specified by study protocol but was under the direction of the medical team. All infants received parenteral nutrition before study entry, and five of the 14 study infants were still receiving parenteral nutrition at the time of study entry. During the study 10 infants were fed formula (Similac Special Care, Ross Products Division, Abbott Laboratories, Columbus, OH) with iron concentration of 3-4 mg/L. Of the four infants who were fed human milk, three also received formula, whereas the fourth received only human milk fortified with Enfamil Human Milk Fortifier(Mead Johnson Nutritionals, Evansville, IN). Feedings were administered by continuous intragastric infusion, by bolus gavage, or by nipple. As per multicenter study protocol, all infants, regardless of feeding, received supplemental iron in a dose of 6 mg/kg daily as ferrous sulfate (Fer-in-Sol, Mead Johnson Nutritionals) in three divided doses given between feedings. Ascorbic acid (Ce-vi-Sol, Mead Johnson Nutritionals) was added to the iron in a dose of 5 mg/mg of iron (molar ratio of 1.6:1). An additional daily multivitamin preparation was given to all infants in a dose of 1.8 mL/d in three divided doses at times other than those when the iron was given. (The daily supplement (1.8 mL) contained 1,500 IU of vitamin A, 400 IU of vitamin D2, 60 mg of vitamin C, 0.5 mg of thiamine, 1.5 μg of vitamin B12, 0.6 mg of riboflavin, 8 mg of niacin, 0.4 mg of pyrodoxine, 60μg of folate, and 15 IU of vitamin E.) The nursing records were used to calculate daily enteral and i.v. intakes of calories, protein and iron.
Procedures. Beginning at study entry, r-HuEPO (R. W. Johnson Pharmaceutical Research Institute, Raritan, N.J.) was administered s.c. in a dose of 500 U/kg/wk (100 U/kg/d, five times a week) for 6 wk. Placebo(vehicle) was administered in identical fashion.
Administration of 58 Fe test doses. On d 8 of the study(“early dosing”), and again on d 29 (“late dosing”), each infant received three doses of 58Fe together with the scheduled iron supplements. These test doses were administered after a 1-h pause in continuous feedings or 2 h after bolus feeding.
Enriched 58Fe (93.24 weight% 58Fe, U.S. Services, Inc., Summit, NJ) was converted to ferrous sulfate as described by Janghorbani et al.(11) and stored in nitrogen-purged vials maintained at room temperature. On the day of dosing, an amount of the58 Fe solution which provided approximately 0.15 mg/kg 58Fe was drawn into each of three tuberculin syringes and precisely weighed. Ascorbic acid (10 mg/kg) was weighed, solubilized in a small volume of water, and aspirated into each of the three syringes containing the 58Fe. Into separate syringes, a solution of natural abundance ferrous sulfate was weighed(1.85 mg/kg). The contents of both syringes were administered separately through the infant's gavage tube, which was flushed with 5 mL of a 10% glucose solution. Thus, dosing provided a total of 0.45 mg/kg of 58Fe together with 5.55 mg/kg of natural abundance iron and 30 mg/kg of ascorbic acid.
Stools were collected for 10 d after dosing with the use of disposable diapers (Huggies, Kimberly-Clark, Neenah, WI). Fecal markers were not used. Blood was obtained by heelstick for isotopic analysis before the first test dose and at weekly intervals thereafter. The last sample was drawn 1 wk after completion of r-HuEPO treatment.
Determination of iron intake. Total daily elemental iron intake(Fed) was calculated as the sum of supplemental iron, taken as the prescribed amount of iron (6 mg/kg/d), plus iron received in formula. The latter was determined from the recorded volume of intake and the manufacturer's stated iron concentration of formula. The iron concentration of breast milk was not determined, and the small amount of iron received from breast milk was disregarded for the four infants who received breast milk. Total daily elemental iron intake was calculated for the same 10-d period during which stool collections were performed.
Laboratory methods. Hb concentration was determined on whole blood in a Technicon H-1 Autoanalyzer (Miles, Inc., Tarrytown, NY), whereas reticulocyte counting was done by flow cytometry after staining with thiazol orange on a FACS-can flow cytometer (Becton Dickinson, Mountain View, CA).
Plasma erythropoietin was measured in triplicate in a double antibody RIA(12) using a modification of the original method of Garcia et al.(13). Plasma indicators of iron status were measured in duplicate. Iron was determined electrochemically with a Ferrochem II analyzer (ESA, Inc., Bedford, MA). Ferritin was determined using the Rianen Assay System Ferritin [125I] Radioimmunoassay Kit(Catalog no. NEA-078, DuPont, Billerica, MA). Transferrin was determined by an antigen-antibody turbidimetric method using rabbit anti-human transferrin antiserum (Boehringer Mannheim, Indianapolis, IN)(14). Transferrin saturation was derived from the plasma concentrations of iron and transferrin, assuming two transferrin high affinity iron binding sites.
Isotopic analysis (58Fe/57Fe ratio) was performed by inductively coupled plasma mass spectrometry using slightly different methods and different instrumentation for blood and feces. Whole blood lysates were used to determine the mass isotope ratio of 58Fe to 57Fe as described by Janghorbani et al.(11). Feces were dry-ashed together with the diapers in which they were collected, ashes were reconstituted in 14% nitric acid, and total (elemental) iron was determined by atomic absorption spectrophotometry(15). The abundance isotope ratio (IR58/57) was determined as described by Fomon et al.(16).
Calculations. The percentage of the 58Fe dose(58Fed) incorporated into erythrocytes was calculated as described by Fomon et al.(17), except that blood volume was assumed to be 80 mL/kg of body weight(18). The amount of 58Fe label excreted in feces(58Fef) was calculated according to the method of Ziegler et al.(19) for stable isotopes of zinc as:Equation where Fef is total fecal iron, 0.02119 is the natural isotopic abundance (atom%) of 57Fe, 0.9323 is the abundance of 58Fe in the enriched preparation, IRf is the determined isotope ratio of the fecal pool, IR0 is the isotope ratio of feces before dosing (natural abundance in the case of early dosing, and ratio determined 10 d after early dosing in the case of late dosing), 0.0656 is the abundance of 57Fe in the enriched preparation, and 14.212 is the 58/57 isotope ratio of the enriched preparation. Percentage absorption of58 Fe (58Fe%a) was calculated as:Equation


Percentage absorption of iron was also determined as elemental iron absorption and calculated as the difference between total iron intake(Fed) and fecal total iron excretion (Fef):Equation

Data analysis. Statistical analyses were performed using Statview 4.5 and SuperANOVA v1.11 (Abacus Concepts, Inc., Berkeley, CA). Mean values for continuous variables were compared using paired or unpaired parametric, or nonparametric procedures as indicated. Where multiple testing was performed between groups, the Bonferroni post hoc procedure was performed to avoid inflating the degrees of freedom. For repeated measures analysis of variance, missing data were handled by substituting the mean interval value for the group. Differences in categorical variables between groups were examined by χ2. The association between variables was examined using simple linear regression. For data not distributed normally, natural logarithm transformed data were used. Statistical comparisons of58 Fe erythrocyte incorporation were based on values obtained 2 wk after administration of the 58Fe test dose. Two-tailed comparisons were used exclusively. An α error level ≤0.05 was considered significant.
RESULTS
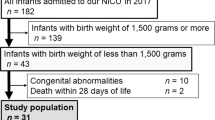
Clinical characteristics of infants in the epo and placebo groups were similar, except for gestational age at birth and postconceptional age at study entry, which by chance were 1.6 and 2.0 wk lower in the epo group (p< 0.05) (Table 1). This was explained by a tendency for more small for gestational age and multiple birth infants in the placebo group. Mean weight gain during the 6-wk study period was 903 g in the epo group and 1040 g in the placebo group (p = NS). At the conclusion of the study, mean weight was 1863 ± 290 g in the epo group and 2040± 160 g in the placebo group (p = NS). Phlebotomy losses and volume and number of erythrocyte transfusions before study entry were comparable in the two groups.
All 14 study infants remained clinically stable throughout the study. No major infections occurred, and steroids were not used. Two epo group infants received diuretics, one for bronchopulmonary dysplasia and the other for a patent ductus arteriosus. Epo and placebo infants had similar numbers of episodes of feeding intolerance and did not differ with respect to age at initiation of nipple feedings and age at start of ad libitum feedings. All seven infants in the epo group and three in the placebo group completed the study as planned. In three of the four placebo infants who were discharged home before completing 6 wk of treatment, 10-d stool collections and 2-wk post-58Fe blood samples were obtained before discharge. One placebo infant discharged on study d 30 did not receive the late 58Fe dose.
Initially low pretreatment plasma epo concentrations in the epo group rose sharply once treatment with r-HuEPO was started, whereas in the placebo group endogenous plasma epo levels rose to a lesser extent, but significantly, toward the end of the study period (F5,30 = 7.12, p< 0.0002) (Fig. 1a). The Hb concentration in the epo group exhibited little variation throughout the study period, whereas in the placebo group Hb levels initially declined, but then rose (Fig. 1b). Differences in Hb concentration were statistically significant between the two groups at study wk 3 and 4. Reticulocyte counts were similar in both groups (Fig. 1c). After cessation of r-HuEPO treatment, there was a precipitous drop in reticulocyte count in the epo group, whereas in the placebo group the relatively high level of erythropoiesis was sustained. When compared with all 80 placebo infants in the multicenter study, the seven placebo infants in the present study evidenced somewhat higher Hb concentrations and reticulocyte counts during the late weeks of the study. Phlebotomy losses during the study period were a third less in all infants in the Iowa subset compared with the entire multicenter population. Blood loss among the former was greater in the epo group than in the placebo group (27 ± 9 mL versus 17± 4 mL, p = 0.03), whereas the mean number of transfusions was similar: epo = 0.9 (range: 0-2) versus placebo = 0.4 (range: 0-1).
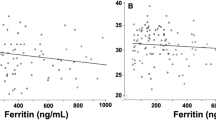
Although plasma iron concentration itself did not differ significantly between groups, nor change with time (Fig. 2), other indicators of iron status changed in both groups during the study. In the epo group, plasma transferrin concentration increased over baseline (p< 0.001), whereas percent transferrin saturation decreased (p< 0.03). In the placebo group similar, only more pronounced, changes occurred. Plasma ferritin levels fell significantly to equivalent degrees in both groups (p < 0.001).
(a) Plasma iron concentration, (b) plasma transferrin concentration, (c) percent plasma transferrin iron saturation, and (d) plasma ferritin concentration. The shaded cross-hatched areas indicate the 6-wk treatment period during which study infants received either placebo or r-HuEPO. “Early” and“late” refer to the 58Fe test meals. Data are shown as mean± SEM.
Energy and protein intakes tended to be lower in epo than in placebo infants, but differences were not statistically significant during any study week (Fig. 3,a and b). Epo group infants tended to be somewhat lighter than placebo infants (Fig. 3c).
Erythrocyte incorporation of 58Fe 2 wk after early dosing was significantly greater in the epo group compared with the placebo group (4.36± 1.65% versus 1.99 ± 1.39%, p < 0.01)(Fig. 4 and Table 2). Although mean percentage58 Fe incorporation increased progressively in both groups at successive weekly time points (Fig. 4), inspection of data from individual infants revealed that, although all seven placebo infants demonstrated continuously increasing values, three of the epo infants manifested declining 58Fe values after the first weekly measurement.
Erythrocyte 58Fe incorporation after“early” and “late” enteral test doses of 58Fe. Data are shown as the weekly mean ± SEM percentage of 58Fe incorporated into Hb after the two doses. The shaded cross-hatched area indicates the 6-wk treatment period during which study infants received either placebo or r-HuEPO. Data after late 58Fe dosing have been re-zeroed using the 58Fe erythrocyte incorporation values from wk 4. The asterisk(*) indicates where significant weekly differences were observed between the two groups (p < 0:01).
Erythrocyte 58Fe incorporation 2 wk after late dosing was not significantly different between the epo and placebo groups (3.84 ± 1.64% versus 5.52 ± 2.68%) (Fig. 4 and Table 2). Compared with early dosing, a tendency toward lower58 Fe incorporation was observed in the epo group, whereas incorporation was increased significantly (p < 0.01) in the placebo group. In the placebo group as a whole, consecutive weekly incorporation values increased, as did values in each of the seven infants. In the epo group, on the other hand, mean values for 58Fe incorporation declined after the 1st wk, as did values in all seven of the infants.
Thirteen complete 10-d stool collections were obtained: seven in placebo and six in epo-treated infants. Percentage 58Fe absorption was not different between the epo and placebo groups after either early or late58 Fe dosing (Table 2). Percentage elemental iron absorption was similar to percentage 58Fe absorption, and, like the latter, values did not differ between groups, nor between early and late dosing. Values for percent 58Fe absorption and percent elemental iron absorption in the combined groups were significantly related (r = 0.74, p = 0.004, n = 13).
Percentage 58Fe erythrocyte incorporation and absorption were examined separately for associations with clinical data and laboratory measurements obtained during the week of 58Fe dosing. Among epo infants, the only significant relationships identified were inverse associations of 58Fe incorporation with plasma iron concentration(p < 0.05) and with transferrin saturation (p < 0.01). In contrast, among placebo infants percent 58Fe incorporation was significantly directly associated with reticulocyte count (p< 0.05), plasma epo (p < 0.01), plasma transferrin(p < 0.001), postnatal age (p < 0.05), postconceptional age (p < 0.01), daily energy intake (p< 0.001), and the time from the last erythrocyte transfusion (p< 0.05). In this group, significant inverse associations were observed for58 Fe incorporation with Hb concentration (p < 0.05) and with plasma transferrin saturation (p < 0.01) in the placebo group. Percentage 58Fe incorporation was not correlated with percentage iron absorption in either group. Additionally, in both groups 58Fe erythrocyte incorporation, 58Fe absorption, and elemental iron absorption were not significantly associated with any of the remaining laboratory or clinical variables, including phlebotomy loss.
DISCUSSION
r-HuEPO is being used to prevent and treat anemia in premature infants(3). The present study was undertaken to determine the effect of epo treatment on erythrocyte incorporation and gastrointestinal absorption of iron by premature infants. In several recent r-HuEPO treatment trials in premature infants, insufficient availability of iron was felt to have an adverse impact on the effectiveness of epo(6–8). The importance of the availability of iron therefore led us to conduct the present study. We formulated the study hypothesis that epo would stimulate both incorporation and absorption of iron, as has been observed by Skikne and Cook(20) in adult subjects. Based on results obtained with early dosing 1 wk after the start of epo treatment, we found that epo treatment stimulates erythrocyte incorporation of iron. We also found that there was no effect of epo on iron absorption. We are aware of but one previous study concerning the effect of epo treatment on iron metabolism in premature infants. In that study, presented in abstract form(21), a nonsignificant trend toward higher percentage 58Fe incorporation and lower absorption was observed among infants treated with the same epo dosing regimen used here.
Absorption of iron. In interpreting results of iron absorption studies, it is important to consider the precise circumstances under which the tests were performed. Iron is generally better absorbed when given on an empty stomach than when ingested with food. A number of food components either enhance (e.g. ascorbic acid) or inhibit (e.g. calcium, casein) the absorption of iron. Percent iron absorption is inversely related to the amount of iron ingested. Subjects in poor iron nutritional status absorb a greater percentage of iron than subjects in good iron status. In the present study 58Fe was administered between feedings, with ascorbic acid and together with a substantial amount of iron. Moreover, our study infants received generous amounts of supplemental iron (6 mg/kg/d) throughout the entire study. Judging from serum ferritin concentrations, these infants were in good iron nutritional status. Under these circumstances, absorption of58 Fe after early dosing averaged 33.6% in the placebo group, and 30.3% in the epo group (p = NS). The elemental balance technique produced similar results, and similarly failed to show an effect of epo. After late58 Fe dosing, results were similar to early dosing and also failed to show an effect of epo. In a study of preterm infants using the radioisotope,59 Fe, given together with iron-fortified formula (Fe concentration 25μg/mL), Gorten et al.(22) found that absorption of 59Fe was 31.5 ± 19.2% and that absorption was not influenced by whether iron-fortified or unfortified formula was fed before and after the test. Dauncey et al.(23), using the elemental balance technique, found that iron absorption from iron-fortified breast milk averaged 34% in preterm infants, regardless of the level of iron fortification. Similar to the present study, the study of Ehrenkranz et al.(9) used a test dose of 58Fe given with ascorbic acid between feedings but, unlike the present study, the test dose did not include additional iron. Mean absorption of iron was 41.6 ± 17.6%.
The results of the present and the earlier studies suggest that percent absorption of iron by premature infants is considerably greater than by adults in good iron nutritional status. For example, Larsen and Milman(24) observed mean iron absorption of 8.5% in normal adult subjects given a small dose (9.9 mg) of iron with ascorbic acid and without food. Furthermore, percent iron absorption by premature infants is remarkably constant despite the use of different methods and despite differences in test conditions anticipated to exert an influence. Thus, iron absorption was similar whether the isotope was given with feedings(22) or between feedings(9)(present study), and was similar whether the isotope was given with additional iron(22) (present study) or without additional iron(9). These findings, and the lack of effect of epo treatment on iron absorption observed by us despite a slight, but significant, 2-wk difference in postconceptional age, lend support to the speculation advanced by Dauncey et al.(23) that iron absorption by premature infants is unregulated by the level of iron intake.
Erythrocyte incorporation of iron. In the present study, erythrocyte incorporation by placebo-treated infants 2 wk after dosing averaged 1.99 ± 1.39% of the dose. Among the previous studies of erythrocyte incorporation in premature infants, only that by Zlotkin et al.(10) used conditions similar to those in the present study. 58Fe was given between feedings with 1.5 mg/kg iron to infants averaging 25 d of age. In the study of Zlotkin et al.(10), erythrocyte incorporation 2 wk after dosing averaged 4.4 ± 2.7%. On the other hand, Ehrenkranz et al.(9) gave 58Fe with ascorbic acid between feedings, but with no additional iron. Mean erythrocyte incorporation of 58Fe in the nine infants receiving low iron formula during the study was 12.5 ± 10.2%. Gorten et al.(22) gave radioiron(59Fe) with ascorbic acid but together with formula with an iron content of 25 μg/mL. The majority of the 14 preterm infants had Hb concentrations less than 100 g/L and reticulocyte counts greater than 5%; mean age at study was 29 d. Mean erythrocyte incorporation of 59Fe was 15.3± 12.4%. Oettinger et al.(25) gave59 Fe in formula without added iron to 10 premature infants 1-7 d of age. Incorporation averaged 2.8% (range: 0.29-6.8%).
It is evident that there are large differences between studies in determined rates of iron incorporation. Based on conditions known to affect iron absorption in older subjects, these differences are not readily explained by the conditions under which the isotopic labels were given. Because absorption of iron in reported studies is relatively constant, it is likely that postabsorptive factors control erythrocyte iron incorporation. It appears that epo, both exogenous and endogenous, could be one of several factors controlling iron incorporation. Despite their 2-wk younger postconceptional age, the epo group demonstrated 2-3-fold greater iron incorporation after early dosing than did their more mature placebo group counterparts. This suggests that small developmental differences do not limit the ability of premature infants to respond to r-HuEPO.
Erythrocyte incorporation of an administered iron isotope has been used widely as a surrogate of iron absorption(26). In adult subjects, 80% or more of absorbed iron is used for Hb synthesis within 2-3 wk. For example, Larsen and Milman(24) found that adult subjects incorporated 92.9% of absorbed iron into erythrocytes within 2 wk. In contrast, after early dosing, placebo infants in the present study absorbed 34% of the 58Fe dose administered, but incorporated a scant 1.99% of the dose. In the study of Gorten et al.(22), absorption averaged 31.5% and incorporation 15.3%. Similarly, in the study of Ehrenkranz et al.(9), absorption averaged 41.6% and incorporation only 12.0%. Thus, unlike in adults, erythrocyte iron incorporation in premature infants does not appear to be a valid surrogate of iron absorption.
Based on the present findings, it is thus apparent that premature infants differ from adult humans not only in the larger proportion of ingested iron that they absorb, but also in the much smaller proportion of absorbed iron that they promptly use for Hb synthesis. The relatively large amount of iron not used promptly is probably entering storage sites. Garby et al.(27) reported that, after i.v. injection of 59Fe in term newborn infants, there was erythrocyte incorporation of 20-30% of injected iron within 2-3 wk, followed by a slower rate of appearance of label in the circulation that continued for the duration of the study. Eventually, after about 4 mo as much as 85% of the injected label appeared in circulating erythrocytes. It is therefore possible that enterally absorbed label could continue to appear in the circulation of premature infants for prolonged periods. In fact, in the present study, after late dosing in the placebo group incorporation of 58Fe continued to increase for 3 wk after dosing without showing a tendency to plateau.
Interpretation of our data on erythrocyte iron incorporation obtained after late dosing presents serious difficulties. This is due in part to the strong endogenous erythropoietic response displayed by the placebo group. Also, the fact that by chance the placebo group included four growth-retarded infants compared with two in the epo group may be relevant in this regard. However, even more confounding was the peculiar and unprecedented course which the58 Fe erythrocyte incorporation took in the epo group. After the initial appearance of label in the circulation, there followed a decrease over the two subsequent weeks. There appear to be only two explanations possible for a disappearance of label from the circulation. One is that erythrocytes were taken out of circulation. The possibility that erythrocytes formed under intense epo treatment may senesce prematurely and have a shortened life span has been suggested in previous reports(28, 29). The other possible explanation is an underestimation of percent 58Fe incorporation secondary to an underestimation of true erythrocyte mass. Our method of calculation assumes that all erythrocytes are in the circulation and that blood volume is 80 mL/kg. The presence of sequestered erythrocytes outside the circulation or of an expanded blood volume are compatible with our data. Whichever is the correct explanation, our observations suggest that treatment with high doses of epo may have hitherto unrecognized effects on erythrocyte life span or on erythrocyte mass.
Although clinical and laboratory factors associated with 58Fe incorporation in the placebo group were diverse, the significant associations of erythrocyte 58Fe incorporation with energy intake, reticulocyte count, time interval from the previous erythrocyte transfusion, and transferrin saturation may be important. Energy intake, and in particular protein intake, and rapid growth have been directly associated with plasma epo levels and erythropoietic activity in several studies in neonatal animals(30–33). The inverse association of58 Fe erythrocyte incorporation with time from the last erythrocyte transfusion was probably the result of increased Hb levels depressing erythropoietin production(34). Conversely, the negative association of 58Fe incorporation and transferrin saturation in both placebo and epo group infants is likely to be due to increased endogenous or exogenous erythropoietin-mediated erythropoiesis.
What are the implications of the present iron metabolism findings for deciding whether to treat premature low birth weight infants with r-HuEPO? Although the early 58Fe erythrocyte incorporation, Hb, and reticulocyte data are consistent with other infant studies in demonstrating r-HuEPO's capability to stimulate erythropoiesis, similar data after late dosing among placebo group infants document that non-r-HuEPO-treated infants are fully capable of rapid increases in Hb values to those equivalent to their epo-treated counterparts. This seeming paradox is more apparent than real as the Hb concentration of placebo infants at the time of late dosing was significantly lower. Importantly, the placebo group consisted of well nourished, rapidly growing premature infants provided with generous supplements of enteral iron, free of clinical signs of anemia, and experiencing only limited phlebotomy loss. Under these circumstances, as is the case for many 4-6-wk-old premature infants, administration of r-HuEPO, or red blood cell transfusions, is of questionable value when compared with allowing natural processes to take over and stimulate erythropoiesis. The important issue of what benefit r-HuEPO may have for the group of younger, less mature and sicker infants who receive a majority of their red blood cell transfusions in the first month of life cannot be inferred from the present data(35), but will require further study.
The present report provides new data regarding erythrocyte incorporation and absorption of iron in iron-supplemented premature infants treated with erythropoietin. Although erythrocyte iron incorporation was significantly accelerated in the early weeks of epo treatment, placebo-treated infants demonstrated remarkable catch-up once their Hb nadir was reached, triggering a surge of erythropoiesis. Associations of erythrocyte iron incorporation with nutritional intake, transferrin saturation, and previous erythrocyte transfusions in placebo infants suggest that postabsorptive factors are important determinants of iron incorporation. Iron absorption was unregulated as daily dosing with generous supplements of iron resulted in 30-34% iron absorption in both placebo and epo-treated infants. Routine administration of epo does not offer a distinct advantage when administered to well nourished premature infants experiencing only modest phlebotomy losses and free of clinical signs of anemia while growing appropriately.
Abbreviations
- epo:
-
erythropoietin
- r-HuEPO:
-
recombinant human erythropoietin
- IR:
-
abundance isotope ratio
References
Christensen RD 1989 Hematopoiesis in the fetus and neonate. Pediatr Res 26: 531–535
Stockman JA 1988 Erythropoietin: off again, on again. J Pediatr 112: 906–908
Strauss RG 1995 Erythropoietin in the pathogenesis and treatment of neonatal anemia. Transfusion 35: 68–73
Maier RF, Obladen M, Sciagalla P, Linderkamp O, Duc G, Hieronimi G, Halliday HL, Versmold HT, Moriette G, Jorch G, Verellen G, Semmekrot BA, Grauel EL, Holland BM, Wardrop CAJ 1994 The effect of epoetinβ (recombinant human erythropoietin) on the need for transfusion in very-low-birth-weight infants. N Engl J Med 330: 1173–1178
Shannon KM, Keith JF, Mentzer WC, Erenkrantz RA, Brown MS, Widness JA, Gleason CA, Bifano EM, Millard DD, Davis CB, Stevenson DK, Alverson DC, Simmons CF, Brim M, Abels RI, Phibbs RH 1995 Recombinant human erythropoietin stimulates erythropoiesis and reduces erythrocyte transfusions in very low birth weight preterm infants. Pediatrics 85: 1–8
Shannon K 1993 Recombinant erythropoietin in anemia of prematurity: five years later. Pediatrics 92: 614–617
Strauss RG 1994 Erythropoietin and neonatal anemia. N Engl J Med 330: 1227–1228
Wilimas JA, Crist WM 1995 Erythropoietin-not yet a standard treatment for anemia of prematurity. Pediatrics 95: 9–10
Ehrenkranz RA, Gettner PA, Nelli CM, Sherwonit EA, Williams JW, Pearson HA, Ting BTG, Janghorbani M 1992 Iron absorption and incorporation in red blood cells by very low birth weight infants: studies with the stable isotope 58Fe. J Pediatr Gastroenterol Nutr 15: 270–278
Zlotkin SH, Lay D, Kjarsgaard J, Longley T 1995 Iron absorption in very low birthweight premature infants using two isotopes of iron (57Fe and 58Fe). J Pediatr Gastroenterol Nutr 21: 190–199
Janghorbani M, Ting BTG, Fomon SJ 1986 Erythrocyte incorporation of ingested stable isotope of iron (58Fe). Am J Hematol 21: 277–288
Georgieff MK, Landon MB, Mills MM, Hedlund BE, Faassen AE, Schmidt RL, Ophoven JJ, Widness JA 1990 Abnormal iron distribution in infants of diabetic mothers: spectrum and maternal antecedents. J Pediatr 117: 455–461
Garcia JF, Ebbe SN, Hollander L, Cutting HO, Miller ME, Cronkite EP 1982 Radioimmunoassay of erythropoietin: circulating levels in normal and polycythemic human beings. J Lab Clin Med 99: 624–635
Borum PR, Bennett SG 1985 A simple and inexpensive method for plasma transferrin determination. Nutr Res 5: 937–940
Haschke F, Ziegler EE, Edwards BB, Fomon SJ 1986 Effect of iron fortification of infant formula on trace mineral absorption. J Pediatr Gastroenterol Nutr 5: 768–773
Fomon SJ, Ziegler EE, Nelson SE, Serfass RE, Frantz JA 1995 Erythrocyte incorporation of iron by 56-day-old infants fed a58 Fe-labeled supplement. Pediatr Res 38: 373–378
Fomon SJ, Ziegler EE, Rogers RR, Nelson SE, Edwards BB, Guy DG, Erve JC, Janghorbani M 1989 Iron absorption from infant foods. Pediatr Res 26: 250–254
Hudson IRB, Cooke A, Holland B, Houston A, Jones JG, Turner T, Wardrop CAJ 1990 Red cell volume and cardiac output in anaemic preterm infants. Arch Dis Child 65: 672–675
Ziegler EE, Serfass RE, Nelson SE, Figueroa-Colón R, Edwards BB, Houk RS, Thompson JJ 1989 Effect of low zinc intake on absorption and excretion of zinc by infants studied with70 Zn as extrinsic tag. J Nutr 119: 1647–1653
Skikne BS, Cook JD 1992 Effect of enhanced erythropoiesis on iron absorption. J Lab Clin Med 120: 746–751
Ehrenkranz RA, Nelli CM, Sherwonit EA, Janghorbani M 1994 Recombinant human erythropoietin (r-HuEPO) stimulates incorporation of absorbed iron (Fe) into RBCs in VLBW infants. Pediatr Res 35: 311A( abstr)
Gorten MK, Hepner R, Workman JB 1963 Iron metabolism in premature infants. I. Absorption and utilization of iron as measured by isotopic studies. J Pediatr 63: 1063–1071
Dauncey MJ, Davies CG, Shaw JCL, Urman J 1978 The effect of iron supplements and blood transfusion on iron absorption by low birthweight infants fed pasteurized human breast milk. Pediatr Res 12: 899–904
Larsen L, Milman N 1975 Normal iron absorption determined by means of whole body counting and red cell incorporation of 59Fe. Acta Med Scand 198: 271–274
Oettinger L, Mills WB, Hahn PF 1954 Iron absorption in premature and full-term infants. J Pediatr 45: 302–306
Cook JD, Dassenko SA, Lynch SR 1991 Assessment of the role of nonheme-iron availabilty in iron balance. Am J Clin Nutr 54: 717–722
Garby L, Sjölin S, Vuille J-C 1964 Studies on erythrokinetics in infancy. IV. The long-term behaviour of radioiron in circulating foetal and adult haemoglobin, and its faecal excretion. Acta Paediatr Scand 53: 33–41
Baxter LM, Vreman HJ, Ball B, Stevenson DK 1995 Recombinant-human erythropoietin (r-HuEPO) increases total bilirubin production in premature infants. Clin Pediatr 34: 226–229
Stohlman F 1961 Humoral regulation of erythropoiesis VII. Shortened survival of erythrocytes produced by erythropoiesis or severe anemia. Proc Soc Exp Biol Med 107: 884–887
Meberg A, Hågå P, Johansen M 1980 Plasma erythropoietin levels in mice during the growth period. Br J Haematol 45: 569–574
Okano M, Ohnota H, Saski R 1992 Protein deficiency impairs erythropoiesis in rats by reducing serum erythropoietin concentration and the population size of erythroid precursor cells. J Nutr 122: 1376–1383
Brown MS, Shapiro H 1996 Effect of protein intake on erythropoiesis during erythropoietin treatment of anemia of prematurity. J Pediatr 128: 512–517
Bozzini CE, Alippi RM, Barcelo AC, Caro J 1989 Correlation between erythropoietic activity and body growth rate in hypertransfused polycythemic growing rats as the result of an erythropoietin-dependent operating mechanism. Exp Hematol 17: 77–80
Lachance C, Chessex P, Fouron JC, Widness JA, Bard H 1994 Myocardial, erythropoietic and metabolic adaptations to anemia of prematurity. J Pediatr 125: 278–282
Widness JA, Seward VJ, Kromer IJ, Burmeister LF, Bell EF, Strauss RG 1996 Changing patterns of red blood cell transfusion in very low birth weight infants. J Pediatr 129: 680–687
Acknowledgements
The authors thank Mark A. Hart for secretarial assistance, Ronald R. Rogers and Robert L. Schmidt for technical assistance, Terrie L. James for nursing care, Steve Nelson for management of the58 Fe data, and Morteza Janghorbani of the BioChemAnalysis Corporation in Chicago, IL for 58Fe determinations on erythrocytes.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Grant CRC RR00059, the Iowa Children's Miracle Network Telethon, the R. W. Johnson Pharmaceutical Research Institute, and The Gerber Companies Foundation.
Rights and permissions
About this article
Cite this article
Widness, J., Lombard, K., Ziegler, E. et al. Erythrocyte Incorporation and Absorption of 58Fe in Premature Infants Treated with Erythropoietin. Pediatr Res 41, 416–423 (1997). https://doi.org/10.1203/00006450-199703000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199703000-00019
This article is cited by
-
Roxadustat and Oral Iron Absorption in Chinese Patients with Anemia of Chronic Kidney Disease: A Randomized, Open-Label, Phase 4 Study (ALTAI)
Advances in Therapy (2024)
-
Iron absorption and oxidant stress during erythropoietin therapy in very low birth weight premature infants: a cohort study
BMC Pediatrics (2005)