Abstract
This study investigated developmental changes in the contractile system of the mesenteric small arteries of the rabbit. Arteries about 1 mm in length and 100-250 μm in internal diameter were dissected out from the mesenteric bed of the fetus (29 d of gestation), newborn (3-5 d old), and adult rabbit. Vascular contraction was induced by high KCl concentration, and contractile force was measured using a tension transducer. The sensitivity of vascular contraction to high KCl was similar in the three age groups. To determine the role of Ca influx across the sarcolemma in vascular contraction, the vasorelaxant effect of diltiazem was studied in the artery precontracted with high KCl concentration. The vasorelaxant effect of diltiazem in the fetus and newborn was less than in the adult. To estimate the size of the intracellular Ca pool, caffeine-induced and noradrenaline-induced contraction were measured in the Ca- and Na-free solution. In the fetus and newborn, both the caffeine-induced contraction and noradrenaline-induced contraction were greater than in the adult. The ultrastructural study showed that the endoplasmic reticulum was abundant in the fetus and newborn, and it was scarce in the adult. These data indicate that the dependency of vascular contraction on Ca influx across the sarcolemma increases and the intracellular Ca store decreases with development in the mesenteric resistance arteries.
Similar content being viewed by others
Main
We showed previously that contraction of the premature myocardium is dependent on Ca influx across the sarcolemma, rather than on Ca release from the sarcoplasmic reticulum(1). We also showed that, in the myocardium of the relatively early fetus of the rabbit, the sarcoplasmic reticulum was scarcely observed, and it developed with age(2). Developmental changes in the contractile system of vascular smooth muscle have not been examined extensively.
Kullama et al.(3) showed in the rat aorta that the vasorelaxant effect of diltiazem on contraction in the newborn was less than in the adult. In contrast, Karaki et al.(4) and Seguchi et al.(5), using the rabbit aorta, showed that the effect of verapamil and diltiazem on KCl- or norepinephrine-induced contraction in the newborn was similar to or greater than that in the adult. Seguchi et al.(5) also showed that caffeine-induced contraction of the aorta in the newborn was less than in the adult, suggesting that contraction of the aorta in the newborn depends more on Ca influx across the sarcolemma and less on the intracellular Ca pool than in the adult.
The contractile system of vascular smooth muscle cells in the small arteries may be different from that in the aorta. For example, Clauvin et al.(6) showed that norepinephrine-induced contraction in the absence of extracellular Ca decreased from proximal to distal arteries, suggesting that the amount of intracellular Ca pool is less in the more distal arteries. Small arteries are physiologically important because they regulate resistance of the circulation. The purpose of the present study was to determine developmental changes in contractile system of the small resistance arteries.
Stimulation of α-adrenoreceptor increases Ca influx across the sarcolemma and Ca release from intracellular Ca store sites. Membrane depolarization also opens the Ca channel and increases Ca influx across the sarcolemma(7, 8). The increased Ca influx may further induce Ca release from intracellular Ca store sites, and the increased[Ca]i results in vascular contraction. To determine the dependence of vascular contraction on the Ca influx across the sarcolemma, the effect of diltiazem on the force of contraction was measured. The size of the intracellular Ca pool was examined using caffeine and noradrenaline. These drugs release Ca from intracellular store sites(6, 9, 10).
METHODS
Experiments were performed using the rabbit mesenteric artery. The fetus at the 29th day of gestation (term 31 d) and 3-5-d-old newborn and 4-8-mo-old adult New Zealand White rabbits were used.
Preparation of vessels. After the doe was anesthetized with pentobarbital sodium (40 mg/kg), the fetuses were delivered by cesarean section and were used immediately. The animals were heparinized (15 U/100 g of body weight, i.v.) and anesthetized with pentobarbital sodium (40 mg/kg). The abdomen was opened, and a segment (2-5 cm) of the small intestine (the proximal part of jejunum) with attached mesentery was removed and placed in ice-cold HEPES-buffered solution. Under a dissecting microscope (model SMZ, Nikon, Tokyo), a segment of a second branch resistance artery, about 1 mm in length, was isolated as described by Mulvany and Halpern(11).
Tension measurement. The mesenteric artery preparation was placed in a tissue bath that was mounted on the stage of an inverted microscope (model TMD, Nikon) and kept at 37°C. Two tungsten wires (25μm in diameter, Thermionic Products Co., North Plainfield, NJ) were threaded into the lumen, and the preparation was placed in a myograph (Living Systems, Burlington, VT)(11, 12). The tungsten wires were secured by stainless screws to specially designed holders. One holder was connected to a micromanipulator and the other was connected to a force transducer (Kulite Semiconductor, Leonia, NJ). Isometric tension was monitored using the force transducer and a recorder (San-ei Sokki, Tokyo, Japan). When once set up, the preparation was superfused with an oxygenated solution at 5 mL/min.
The optimal resting tension in vitro would be the one which is equivalent to the transmural pressure in vivo. In the present study, however, resting tension lower than the optimal tension was used as described previously(11, 12). The optimal resting tension was calculated using the LaPlace's equation(13). It was assumed that mean pressure of the mesenteric small artery in vivo is 16 mm Hg for the fetus, 32 mm Hg for the newborn, and 80 mm Hg for the adult. These values were calculated based on the assumption that the pressure in resistance arteries with internal diameters of 100-300 μm is 80-90% of the arterial mean pressure and the arterial mean pressure is 20 mm Hg in the fetus, 40 mm Hg in the 3-d-old newborn, and 90 mm Hg in the adult rabbit(14–16). It is uncertain whether the same ratio of intraluminal pressure to mean arterial pressure can be applied in the three age groups. However, Raj and Chen(17) showed a 32-44% pressure drop from the main pulmonary artery to 80-μm arteries in the newborn lamb. Davis et al.(18) showed about 45% pressure drop from mean arterial pressure to the 80-μm artery in the cheek pouch of the adult hamster. These data suggest that the pressure drop along the small arteries may be similar in the premature and mature animals.
Axial vessel length and distance between the wires were measured while the vessels were stretched gradually. The vessel circumference and wall tension were calculated, and exponential curves of vessel circumference versus tension were constructed. The slopes of the curves were similar in the three age groups. The artery was stretched until the resting wall tension reached the level corresponding to the transmural mean pressure in vivo. The vessel circumference at this point was expressed as Lop. Then the vessel circumference was adjusted so that the operating circumference was 80% of Lop(L80%). The resting tension in the fetus at this point was 0.12 ± 0.03 mN/mm, 0.23 ± 0.04 mN/mm in the newborn, and 0.35± 0.03 mN/mm in the adult. In a preliminary study, KCl concentration in the solution increased from 5 to 120 mM at various vessel circumferences. At L80%, developed tension was near maximal (about 80% of the maximum) and the resting tension was relatively low (about 12% of the developed tension) in the three age groups.
Experimental protocol. All mesenteric artery rings were initially stabilized for 30 min in Krebs-Henseleit solutions at 37°C. The control Krebs-Henseleit solution contained (in mM): NaCl, 118; KCl, 5; CaCl2, 1.5; glucose, 6; MgCl2, 1; NaHCO3, 24; NaH2PO4, 0.436. The solution was equilibrated with 95% O2, 5% CO2, yielding a final pH of 7.38-7.42, Pco2 of 35-42 mm Hg, and Po2 of 660-690 mm Hg. In experiments to study the effect of high KCl, the KCl concentration was increased from 5 to 50, 80, and 120 mM. In K-rich solutions, the NaCl was replaced, mol by mol, by KCl. Finally, to obtain maximal contraction, the Ca concentration was increased from 1.5 to 10 mM. In a preliminary study, an increase in Ca concentration from 10 to 20 mM in 120 mM KCl solution did not further enhance vascular contraction in all age groups.
To determine the dependence of vascular contraction on the Ca influx across the sarcolemma, the effect of diltiazem on the force of contraction was measured. Diltiazem (Sigma Chemical Co.) was added to the Krebs-Henseleit solution containing 50 mM KCl at 10-7 to 10-5 M. Initially the vascular contraction was induced by 50 mM KCl, and after the mechanical function reached a new steady state, the vessel was superfused with solutions containing 10-7 to 10-5 M diltiazem (Sigma Chemical Co.) in addition to 50 mM KCl.
The size of the intracellular Ca pool was examined using caffeine and noradrenaline. These drugs release Ca from intracellular store sites(6, 9, 10). We considered that the effect on contraction was proportional to the size of the intracellular Ca pool. The degree of caffeine-induced or noradrenaline-induced contraction was normalized by the degree of KCl-induced contraction. To eliminate the Ca efflux via Na-Ca exchange and Ca influx via Ca channel, the effect of caffeine or noradrenaline was examined in the absence of extracellular Na and Ca. Initially, the vessel was superfused with a control HEPES solution. The HEPES solution contained (in mM): NaCl, 142; KCl, 5; CaCl2, 1.5; glucose, 6; MgCl2, 1; HEPES, 5; pH 7.4, with 1 M NaOH. The HEPES solution was equilibrated with 100% O2. The vessel was then superfused with a HEPES solution which did not contain Ca and Na. The Ca- and Na-free solution contained in mM:N-methylglucamine, 142; KCl, 4; K2-EGTA, 1; glucose, 6; MgCl2, 1; HEPES, 5; pH 7.4, with 1 M HCl. Ten minutes after superfusion with the Ca- and Na-free solution, the vessel was superfused with the Ca- and Na-free solution containing 20 mM caffeine or noradrenaline. After the developed tension reached its peak value, the vessel was superfused again with a control HEPES solution. After the mechanical function returned to control, vascular contraction was induced by a solution containing 120 mM K and 10 mM Ca. Because α-adrenoreceptor density may be different in the three age groups, noradrenaline-induced contraction in the Ca- and Na-free solution was also normalized by the degree of noradrenaline-induced contraction measured in the presence of Ca and Na in the solution. The effect of noradrenaline(10-5 M) was initially studied in a control HEPES solution and then the effect of noradrenaline was studied in the Ca- and Na-free solution. A stock solution of noradrenaline (10-3 M) (Nakarai Chemical, Tokyo) containing 10-3 M ascorbic acid was made just before use and diluted to a final concentration of 10-5 M in a HEPES solution.
In some experiments, the effect of caffeine was examined in a vessel from which the endothelium was removed. The endothelium was removed using the method of Li and Bukoski(19). The absence of a relaxation response to acetylcholine (1 μM) of vessels precontracted with 50 mM KCl was taken as evidence that the endothelium was removed.
Developed tension was calculated as total tension - resting tension. Developed tension observed during diltiazem, caffeine, or noradrenaline superfusion was expressed as percent of the control developed tension induced by KCl.
Skinned smooth muscle fibers. Because intracellular Ca concentration ([Ca]i was not measured directly and contractile tension was used as an indicator of [Ca]i in the present study, sensitivity of myofibrils to Ca was measured in three age groups. Skinned smooth muscle fibers of the mesenteric artery were prepared using the method of Saida et al.(20). The vessel was mounted in a wire myograph with a volume capacity of 1 mL, and the contractile force was monitored using a force transducer. The tissue bath was initially filled with a control HEPES solution. The solution was then changed to the relaxing solution (30 mM TES, 10 mM EGTA, 3.3 mM Na2-ATP, 5 mM MgCl2, 130 mM KCl, pH 7.1, with 1 M KOH) containing 100 μg/mL saponin and 10 μM Ca ionophore A23187. The incubation was carried out for 20 min at 25°C. Saponin was used for chemical skinning of the smooth muscle cells, and A23187 was used to inactivate the function of the sarcoplasmic reticulum. After the incubation, the skinned smooth muscle was washed once with the relaxing solution that did not contain saponin and A23187. Contraction of the skinned smooth muscle was induced by changing the solution to the relaxing solution containing various amounts of CaCl2. The pCa (-log [Ca]) of the solution was changed from 8 to 4.5. The pH was adjusted with 1 M KOH to 7.1. The amounts of CaCl2 to be added were calculated using programs described by Fabiato and Fabiato(21), and the apparent stability constants of EGTA and ATP used for calculation of pCa were as described previously(1). Developed tension at various pCa was normalized by the maximal developed tension obtained in each preparation.
Ultrastructure. Small pieces of the mesenteric arteries were placed in ice-cold 3% glutardehyde fixative buffered with 0.1 M phosphate buffer (pH 7.4) for 60 min. After three washings with 0.1 M phosphate buffer, specimens were placed in OsO4 (1%) buffered with 0.1 M phosphate buffer. After osmication, the vessels were dehydrated in ethanol and embedded in a Poly Bed 812 resin. Thin sections for electron microscopy were cut with a glass knife on an ultramicrotome (LKB Ultrotome V) and stained with uranyl acetate and lead citrate. These sections were examined using a Nihondenshi electron microscope (JEM1200EX) at a magnification of 30,000. Morphometric analysis was performed in three animals of a different litter for each age group. A total of 15 micrographs for each age group were taken, and the relative area occupied by the myofibrils in the cell (excluding the extracellular space) was measured using an electrical digitizer. Because the present method did not measure the cellular volume, the present measurement should be considered as a semiquantification.
Statistical analysis. Results were expressed as mean ± SE. For comparison between three groups, one-way analysis of variance with Wilcoxon's rank sum test was used. The probability was considered to be significant if the p value was less than 0.05(22).
RESULTS
The external and internal diameters of the mesenteric artery in the three age groups under resting conditions are shown in Table 1.
High K concentrations cause membrane depolarization and vascular contraction. Initially, the effect of KCl on vascular contraction was studied. Maximal developed tension obtained in the 120 mM KCl and 10 mM Ca solution was 1.03 ± 0.18 mN/mm in the fetus, 1.79 ± 0.15 mN/mm in the newborn, and 2.89 ± 0.25 mN/mm in the adult (n = 11). Although absolute values of contractile force induced by high KCl concentration increased with age, sensitivity to high KCl concentration was similar in the three age groups (Fig. 1). To obtain a mild degree of vascular contraction, a KCl concentration of 50 mM was chosen arbitrarily and used to induce vascular contraction and to examine the effect of diltiazem.
Effect of high KCl concentrations on contraction in the small mesenteric arteries. The values are mean ± SEM of six experiments. Maximal contraction was observed at 125 mM KCl and 10 mM Ca in all age groups. The relative degree of contraction at various K concentrations was similar in the three age groups.
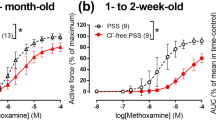
Membrane depolarization activates slow Ca channels and induces Ca release from the intracellular Ca store sites. To estimate the role of Ca channels in the vascular contraction, the effect of the Ca antagonist was examined. Diltiazem, 10-7 M, caused a small increase in developed tension in the fetus (to 116 ± 5%), but not in the newborn. This concentration of diltiazem significantly decreased developed tension in the adult (Fig. 2). Diltiazem higher than 10-7 M caused vasorelaxation in all age groups, and the vasorelaxant effect in the fetus and newborn was significantly less than in the adult (Fig. 2). In additional experiments, the degree of KCl-induced contraction was examined in the presence of diltiazem. Initially the vessel was superfused with a solution containing 10-6 or 10-5 M diltiazem, and then the vascular contraction was induced by 50 mM KCl. The degree of inhibition of KCl-induced contraction by diltiazem was identical to the data shown in Figure 2.
Effect of diltiazem on KCl-induced contraction in the small mesenteric arteries. The values are mean ± SEM of six experiments. Vascular contraction was induced by 50 mM KCl, and then the effect of diltiazem was examined. *Significantly different from the newborn and fetal values. **Significantly different from the fetal value. The effect of diltiazem on KCl-induced contraction in the fetus and newborn was significantly less than in the adult.
The size of the intracellular Ca pool was estimated using caffeine (Fig. 3) and noradrenaline (Fig. 4). The caffeine-induced contraction in the Ca- and Na-free solution in the newborn and fetus was similar (35 ± 5 and 27 ± 5% of the KCl-induced contraction, respectively), and it was significantly greater than in the adult (10 ± 1%). The effect of caffeine on vascular contraction was studied in the vessels from which the endothelium was removed. In the absence of the endothelium, the caffeine-induced contraction was identical to that in the vessels with endothelium in the three age groups. The degree of noradrenaline-induced contraction in the Ca- and Na-free solution in the fetus and newborn was similar, and it was significantly greater than in the adult (Fig. 4,Table 2).
Effect of caffeine on contraction of the small mesenteric arteries. The vessels were superfused with a Ca- and Na-free solution and then 20 mM caffeine was applied to block Ca influx and Na-Ca exchange. Maximal contraction was then induced using a solution containing 120 mM K and 10 mM Ca. Caffeine caused a significant contraction in the newborn and fetus. In contrast, the caffeine-induced contraction in the adult was minimal.
Effect of noradrenaline on contraction of the small mesenteric arteries. Noradrenaline (10-5 M)-induced contraction was initially examined in the control solution. The vessels were then superfused with a Ca- and Na-free solution to block Ca influx and Na-Ca exchange. Noradrenaline (10-5 M) was applied in the Ca- and Na-free solution. Finally, maximal contraction was induced using a solution containing 120 mM K and 10 mM Ca. Noradrenaline-induced contraction in the fetus and newborn was greater than in the adult.
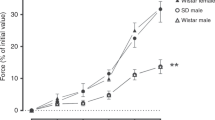
The tension-[Ca]i relationship was determined in the skinned smooth muscle fibers to estimate sensitivity of myofibrils to Ca in the three age groups. At pCa 6.0, the relative degree of activation in the adult was greater than in the newborn and fetus (Fig. 5). The half-maximal activation (Kd) was observed at [Ca] of 0.81 ± 0.20 μM (Kd) in the adult (n = 6), and the Kd value was significantly less than in the newborn (1.40 ± 0.17 μM, n = 6) and fetus (1.44 ± 0.21 μM, n = 6).
Relative value of developed tension measured in the skinned smooth muscle fibers of the mesenteric artery. The values are mean± SEM of six experiments. pCa = -log [Ca]. The half-maximal activation (Kd) was observed at [Ca] of 0.81 ± 0.20μM (Kd) in the adult, and the value was significantly less than in the newborn (1.40 ± 0.17 μM) and fetus (1.44 ± 0.21μM). *Significantly different from the newborn and fetal values.
The ultrastructural study showed that the endoplasmic reticulum was abundant in the fetus and newborn, but it was scarce in the adult (Fig. 6). Morphometric analysis was performed to estimate the amount of myofibrils. The fraction of myofibrils in the vascular smooth muscle cells in the fetus (25 ± 3%) and newborn (47 ± 12%) was less than in the adult (77 ± 7%). The value in the fetus was significantly less than in the newborn.
Electron micrographs of smooth muscle cells in the mesenteric small artery. MF, myofibrils; ER, endoplasmic reticulum. Calibration bars are 1 μm. In the fetus (A) and newborn (B), the endoplasmic reticulum is well developed. In the adult (C), the endoplasmic reticulum is poorly developed, but myofibrils are abundant.
DISCUSSION
Previous studies have shown that the contractile force of large arteries increases with development(3, 23), but its mechanism has not been studied. In the present study, in accordance with the data in the large vessels, maximal contractile force obtained in the high K and Ca solution increased with age, and the values in the newborn and fetus were 62 and 36% of the adult value, respectively. Because the amount of myofibrils increased with age in the ultrastructural study (Fig. 6), the increase in contractile force is most likely due to the developmental changes in the amount of myofibrils. The amounts of myofibrils in the newborn and fetus were 61 and 32% of the adult value, respectively. Therefore, it is likely that the contractile force developed by a unit volume of myofibrils is similar in the three age groups.
Kullama et al.(3) showed in the rat aorta that the vasorelaxant effect of diltiazem on contraction in the newborn was less than in the adult. In contrast, Karaki et al.(4), using the rabbit aorta, showed that the effect of verapamil on KCl- or norepinephrine-induced contraction in the newborn was similar to or greater than that in the adult. These authors attributed the age-related difference in the effect of Ca antagonists to the qualitative changes in Ca channels.
Membrane depolarization increases Ca influx across the sarcolemma and induces Ca release from intracellular store sites. The present study showed that the sensitivity to a high K concentration in the fetus, newborn, and adult was similar (Fig. 1). This suggests that membrane depolarization causes a similar degree of activation of the contractile system in the three age groups. The present study showed that the vasorelaxant effect of diltiazem in the fetus and newborn was less than in the adult (Fig. 2). The result may suggest that the Ca channels in the immature small artery are less sensitive to blockade by diltiazem than in the mature small artery and that Ca channels may change qualitatively with development. Furthermore, because the vasorelaxant effect in the fetus and newborn was less than in the adult even at a high concentration of diltiazem(10-5 M), the dependency of contraction on Ca influx through the Ca channels may be less in the premature small artery than in the mature small artery. To confirm these hypotheses, a direct measurement of slow Ca current should be performed.
If the [Ca]i required for vascular contraction in the mature artery is higher than in the premature artery, a similar degree of reduction of [Ca]i may result in the greater relaxation in the adult. The result obtained using skinned fibers, however, suggests that the Ca concentration required by the myofibrils in the mature artery is lower than that in the premature artery (Fig. 5). Therefore, it is unlikely that the greater sensitivity of the mature artery to diltiazem is explained by the difference in the sensitivity of myofibrils to Ca.
The size of the intracellular Ca pool was estimated using caffeine and noradrenaline. The data suggested that the size of the intracellular Ca pool was greater in the premature vessels than in the adult (Figs. 3 and 4). The ultrastructural study also showed a greater amount of the endoplasmic reticulum in the premature vessels than in the mature vessels. Because the endoplasmic reticulum is an important organelle regulating intracellular Ca(24), the ultrastructural study seems to be in agreement with the results using caffeine and noradrenaline. It must be noted, however, that the present study did not show directly whether the intracellular Ca pool detected by the present method is physiologically important or not.
Seguchi et al.(5) showed in the rabbit aorta that the effect of diltiazem in the newborn was greater than in the adult. They also showed that caffeine-induced contraction of the aorta in the newborn was less than in the adult. These data suggested that contraction of the aorta in the newborn depended more on Ca influx across the sarcolemma and less on the intracellular Ca pool than what is found for the adult. It is interesting that developmental changes in the source of contractile Ca in the small arteries is different from that in the aorta. It has been shown that norepinephrine-induced contraction in the absence of extracellular Ca decreased from proximal to distal arteries, suggesting that the amount of intracellular Ca pool is less in the more distal arteries in the mature animal(6). How these developmental changes are regulated remains to be studied.
One may argue that contraction of small arteries is regulated mainly by catecholamines in vivo, and the clinical implication of the data using high K concentrations is not clear. In the present study, noradrenaline was not used to examine the effect of diltiazem mainly because norepinephrine caused a transient contraction, but the contractile force returned toward the control level continuously, and it was difficult to obtain a steady state contraction.
If the contraction of the resistance artery is controlled by a membrane potential(10, 25), then it is likely that there is no age-related difference in the degree of activation of the contractile system under control conditions (Fig. 1), no matter how the source of contractile Ca changes with development. Even if that is the case, the present study suggests that the effect of Ca antagonists on the resistance artery in the premature animals may be different from that in the mature animals. In agreement with this hypothesis, Gibson et al.(26) showed that verapamil decreased systemic resistance in the adult dog, but not in the puppy.
In summary, the present data indicate that, in the mesenteric resistance arteries, the dependency of vascular contraction on Ca influx across the sarcolemma increases, and the intracellular Ca store decreases with development.
Abbreviations
- HEPES:
-
N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid
- TES:
-
N-tris(hydroxymethyl)methyl-2-aminoethanesulfonic acid
References
Nakanishi T, Jarmakani JM 1984 Developmental changes in myocardial mechanical function and subcellular organelles. Am J Physiol 246:H615–H625.
Nakanishi T, Okuda H, Kamata K, Abe K, Sekiguchi M, Takao A 1987 Development of myocardial contractile system in the fetal rabbit. Pediatr Res 22: 201–207.
Kullama LK, Balaraman V, Claybaugh JR, Ichimura WM, Pichoff BE, Nakamura KT 1991 Differential ontogeny of in vitro vascular responses to three categories of calcium channel antagonists in rats. Pediatr Res 29: 278–281.
Karaki H, Nakagawa H, Urakawa N 1985 Age-related changes in the sensitivity to verapamil and sodium nitroprusside of vascular smooth muscle of rabbit aorta. Br J Pharmacol 85: 223–228.
Seguchi M, Nakazawa M, Nakanishi T, Kinugawa Y, Takao A 1990 Developmental change of vascular smooth muscle contraction in the rabbit thoracic aorta. Circulation 82: III–491
Cauvin C, Saida K, van Breemen C 1984 Extracellular Ca dependence and diltiazem inhibition of contraction in rabbit conduit arteries and mesenteric resistance vessels. Blood Vessels 21: 23–31.
Karaki H, Weiss GB 1988 Calcium release in smooth muscle. Life Sci 42: 111–122.
Nelson MT 1993 Ca-activated potassium channels and ATP-sensitive potassium channels as modulators of vascular tone. Trends Cardiovasc Med 3: 54–60.
Kanaide H, Kobayashi S, Nishimura J, Hasegawa M, Shogakiuchi Y, Matsumoto T, Nakamura M 1988 Quin2 microfluorometry and effects of verapamil and diltiazem on calcium release from rat aorta smooth muscle cells in primary culture. Circ Res 63: 16–26.
Cauvin C, Lukeman S, Cameron J, Hwang O, van Breemen C 1985 Differences in norepinephrine activation and diltiazem inhibition of calcium channels in isolated rabbit aorta and mesenteric resistance vessels. Circ Res 56: 822–828.
Mulvany MJ, Halpern W 1977 Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41: 19–26.
Wang Y, Coceani F 1992 Isolated pulmonary resistance vessels from fetal lambs. Circ Res 71: 320–330.
Halpern W, Kelley M 1991 In vitro methodology for resistance arteries. Blood Vessels 28: 245–251.
Dawes GS, Handler JJ, Mott JC 1957 Some cardiovascular responses in foetal, newborn, and adult rabbits. J Physiol 139: 123–136.
Downing SE 1960 Baroreceptor reflexes in newborn rabbits. J Physiol 150: 201–213.
Mulvany MJ, Aalkjaer C 1990 Structure and function of small arteries. Physiol Rev 70: 921–961.
Raj IU, Chen P 1986 Microvascular pressures measured by micropuncture in isolated perfused lamb lungs. J Appl Physiol 61: 2194–2201.
Davis MJ, Ferrer PN, Gore RW 1986 Vascular anatomy and hydrostatic pressure profile in the hamster cheek pouch. Am J Physiol 250:H291–H303.
Li J, Bukoski RD 1993 Endothelium-dependent relaxation of hypertensive resistance arteries is not impaired under all conditions. Circ Res 72: 290–296.
Saida K, Nonomura Y 1978 Characteristics of Ca and Mg-induced tension development in chemically skinned smooth muscle fibers. J Gen Physiol 72: 1–14.
Fabiato A, Fabiato F 1979 Calculator for computing the composition of the solutions containing multiple metals and ligands used for experiments in skinned muscle cells. J Physiol (Paris) 75: 463–505.
Snedecor GW, Cochran WG ( 1970 Statistical Methods. Iowa State University Press, Ames
Hayashi S, Toda N 1978 Age-related changes in the response of rabbit isolated aortae to vasoactive agents. Br J Pharmacol 64: 229–237.
Devine CE, Somlyo AV, Somlyo AP 1972 Sarcoplasmic reticulum and excitation-contraction coupling in mammalian smooth muscles. J Cell Biol 52: 690–718.
Mulvany MJ, Aalkjaer C, Petersen TT 1984 Intracellular sodium, membrane potential, and contractility of rat mesenteric small arteries. Circ Res 54: 740–749.
Gibson R, Driscoll D, Gillette P, Hartley C, Entman ML 1981 The comparative electrophysiologic and hemodynamic effects of verapamil in puppies and adult dogs. Dev Pharmacol Ther 2: 104–116.
Acknowledgements
The authors thank Dr. Kooichi Saida at the Pharmacology Institute, Bayer Yakuhin for his useful advice, and Hiroaki Nagao for technical assistance in the ultrastructural study.
Author information
Authors and Affiliations
Additional information
Supported by a Research Grant 5670702 and 7670907 from the Japanese Ministry of Education, Science, and Culture and by a grant-in-aid from the Japan Research Promotion Society for Cardiovascular Diseases.
Rights and permissions
About this article
Cite this article
Nakanishi, T., Gu, H., Abe, K. et al. Developmental Changes in the Contractile System of the Mesenteric Small Artery of Rabbit. Pediatr Res 41, 65–71 (1997). https://doi.org/10.1203/00006450-199701000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199701000-00010