Abstract
These studies determined the effects of fetal treatment with betamethasone alone, or in combination with thyroid hormone (thyroxine; T4), on postnatal renal and endocrine adaptations in preterm newborn lambs. Ovine fetuses (126 d of gestation; term = 150 d) received single, ultrasound-guided intramuscular injections of saline, 0.5 mg/kg betamethasone (Celestone Soluspan®, or 0.5 mg/kg betamethasone plus 60 μg/kg T4. After 48 h, lambs were delivered, treated with surfactant (Survanta®, 100 mg/kg), and ventilated for 3 h. Due to maintained urine flow in the betamethasone-treated animals and a significant decrease in the saline group, betamethasone versus saline urine flow values (0.11 ± 0.03versus 0.03 ± 0.004 mL·min-1·kg-1) were significantly elevated by the end of studies. GFR (1.5 ± 0.3 versus 0.8 ± 0.2 mL·min-1·kg-1) and mean blood pressure (61± 4 versus 42 ± 3 mm Hg) values also were higher in the betamethasone-treated animals. Although renal blood flow, renal plasma flow, and fractional sodium excretion rates did not differ, betamethasoneversus saline values for the filtration fraction (11.9 ± 1.5versus 7.4 ± 1.5%) and total sodium reabsorption (196± 38 versus 81 ± 16μEq·min-1·kg-1) were increased. Betamethasoneversus saline treatment also was associated with significant reductions in plasma angiotensin II (125 ± 23 versus 550± 140 pg/mL) and AVP (116 ± 19 versus 230 ± 77 pg/mL) levels. Overall, the effects of combined betamethasone + T4 treatment were similar to the effects of betamethasone alone. Conclusions: 1) fetal betamethasone injection 48 h before delivery stabilizes GFR and significantly alters endocrine function in preterm newborn lambs, and 2) the addition of T4 does not augment betamethasone-induced renal and endocrine responses.
Similar content being viewed by others
Main
The effectiveness of antenatal glucocorticoids alone or in combination with thyroid hormones to decrease the severity of chronic lung disease in premature human newborns is widely recognized(1, 2). However, information regarding effects on other organs, including the kidney, is limited(3, 4). Fetal renal function is characterized, in part by reduced sodium and water reabsorption relative to term newborns and adults(5, 6). Thus, changes in renal sodium and water reabsorption after the transition from fetal to neonatal life are essential to the newborn's ability to establish fluid and electrolyte homeostasis in the extrauterine environment. However, the ability of the preterm newborn kidney to shift from the fetal pattern of exaggerated natriuresis and diuresis(7, 8) to increased sodium reabsorption is often limited. The resulting hyponatremia and hypovolemia are increasingly recognized as important sources of perinatal morbidity in the premature newborn. Although renal adaptation in term newborns has been studied and fetal studies have provided insight into premature fetal renal function(5), studies of preterm newborn renal adaptive mechanisms are lacking. We have recently used the surfactant-treated, ventilated preterm lamb model to characterize postnatal renal adaptations in preterm and near term lambs(9). In the present studies we have expanded this model to include ultrasound-guided fetal glucocorticoid and thyroid hormone injections(10, 11) 48 h before delivery. This unique approach has allowed us for the first time to directly assess the efficacy of fetal injections of betamethasone alone or in combination with thyroid hormone on renal function in ventilated preterm newborn lambs.
METHODS
Animals. Twenty-three pregnant ewes carrying singleton fetuses of known gestation were obtained from the Nebeker Ranch (Palmdale, CA). Animal handling and study protocols were reviewed and approved by the Harbor-UCLA Animal Care and Use Review Committee. At 125 or 126 d of gestation (term = 150 d) ewes were restrained without anesthesia in a position suited to ultrasound-guided injections(11). The fetus was imaged with a real time ultrasound system (Acusonics Opus I, Lane Cove, Australia) with a 5 MHz sector transducer as described previously(10, 12). The fetal heart and chest were imaged, and the fetus was injected in either the neck or shoulder (using a 9-cm 20-gauge spinal needle) with a single dose of 0.15 M saline (n = 9), 0.5 mg/kg betamethasone (Celestone Soluspan®, Schering Pharmaceuticals, Kenilworth, NJ; n = 7) alone or 0.5 mg/kg betamethasone plus 60μg/kg T4 (Sigma Chemical Co., St. Louis, MO; n = 7). An estimated fetal body weight of 3 kg was used to calculate dosages; the injection volume was 2.5 mL or 0.15 M saline. The betamethasone and T4 doses were based on previously demonstrated improvements in 127- or 128-d premature ovine newborn pulmonary function(10, 12).
Delivery protocol. Forty-eight hours after injection (127 or 128 d of gestation) ewes were sedated with an intramuscular injection of ketamine hydrochloride (15-20 mg/kg) and given combined spinal-epidural anesthesia (10 mL of 2% lidocaine: 0.5% bupivacaine 1:1). After a midline maternal abdominal incision and hysterotomy, the fetal head and neck were delivered and an intramuscular injection of a mixture of ketamine/acepromazine(10 mg/kg/0.1 mg/kg) administered. The anterior neck was infiltrated with 2% lidocaine, followed by tracheotomy and insertion of a 4.5-mm endotracheal tube. The tube was firmly tied in place, and airway liquid was aspirated. The umbilical cord was clamped and cut, and blood was collected from the placental umbilical vein for pH, blood gas and hormone determinations, and for newborn transfusion.
Lambs were delivered, weighed, dried, and treated with surfactant(Survanta®, Ross Laboratories, Columbus, OH; 100 mg/kg) via direct intratracheal instillation before the first breath(13). Lambs were mechanically ventilated with 100% oxygen using pressure-cycled infant ventilators. Initial ventilator settings included: positive-end expiratory pressure of 0.3 kPa, a rate of 40 breaths/min, and an inspiratory time of 0.7 s. Peak inspiratory pressure was initially set at 3.4 kPa and adjusted to achieve Pco2 values of 4.0-5.3 kPa. Peak inspiratory pressure was limited to 3.9 kPa to avoid pneumothorax.
After initiation of ventilation (1-2 min after birth), a 5 French polyethylene catheter was placed in the descending aorta distal to the kidneys via the umbilical artery for blood sampling and blood pressure monitoring. After catheter placement, lambs received an infusion of filtered (Hemonate, Gesco International, San Antonio, TX) placental blood (10 mL/kg). A single dose of [3H]inulin (10 μCi) was injected via the umbilical artery catheter, and plasma inulin clearance was used to compare GFR among the groups. After local lidocaine infiltration of the skin, a bladder catheter(inside diameter, 1.3 mm; outside diameter, 2.3 mm, with multiple entry ports) was placed by suprapubic cystotomy to permit timed urine collections. A 3.5 French polyethylene catheter was passed into the left ventricle via the right carotid artery for left ventricular pressure monitoring and to provide a route for microsphere injections. Placement of catheters was completed within 10 min after delivery. Maintenance fluids (5% dextrose in water) were administered at equal rates into the umbilical artery and left ventricular catheters for a total volume of 0.075 mL·min-1·kg-1. Blood pressure and heart rates were monitored continuously. Body temperature was monitored by rectal thermometer and maintained at 39.0 ± 0.5 °C by use of a radiant warmer, heating pad, and heat lamps.
Fetal arterial blood samples (0.3 mL) for measurements of pH and blood gasses were collected on average every 30 min, and/or 5 min after ventilator adjustments to monitor ventilatory status. Blood samples (6 mL) were collected from the placental umbilical vein after delivery of the lamb, and via the umbilical artery catheter at 20, 60, 120, and 180 min after delivery for measurements of hematocrit, plasma osmolality, electrolytes,[3H]inulin, AVP, AII, and ANF levels. Blood samples were replaced vol:vol with washed and filtered maternal red blood cells. Evaluation of postnatal adaptation continued for 3 h after birth.
Fetal urine samples for flow rate, osmolality, and electrolyte concentration measurements were collected at 10-min intervals during the first 40 min. Subsequent urine collections were at 1-h and at 40-min intervals thereafter. Estimates of GFR were calculated only for the last two 40-min urine collection periods to ensure that calculations were based on stable plasma inulin levels. Fetal mean arterial and left ventricular tracings were monitored continuously with a Beckman R-611 physiologic recorder (Beckman Instruments, Fullerton, CA) and Statham P23DB pressure transducers (Gould, Oxnard, CA). In addition to the continuous paper record, acquired data were continuously streamed (25 Hz per channel) to an AT microcomputer by use of Codas acquisition software (DATAQ Instruments, Inc., Akron, OH). Mean blood pressure and heart rate values were derived by post hoc analysis of the acquired data.
Renal blood flow was measured 30 min before the end of studies using radiolabeled microspheres(14). A measured number of counts/min of either 57Co- or 85Sr-labeled microspheres (15.5± 0.1-μm diameter; DuPont NEN, Boston, MA) were mixed with 5 mL of maternal blood just before injection over 15 s into the left ventricle. During the left ventricular injection, a reference sample was withdrawn with a Harvard pump (Harvard Apparatus Co., South Natick, MA) from the aortic catheter (5 mL/min for 2 min) into a preweighed, heparinized syringe. The blood volume withdrawn was determined gravimetrically, and microsphere content was assessed in an LKB Compugamma counter. At the end of the experiments, the lambs were killed with an overdose of pentobarbital and exsanguinated, and the kidneys were removed. The kidneys were decapsulated and weighed, and the57 Co and 85Sr microsphere levels were determined.
Analytical techniques. Blood pH, Po2, and Pco2 values were determined on a NOVA Stat Profile Plus 3 blood analyzer (NOVA Biomedical, Waltham, MA). Plasma and urine osmolalities were measured by freezing-point depression (Advanced Digimatic Osmometer; model MO, Advanced Instruments, Needham Heights, MA). Blood and urine electrolyte (sodium, potassium, and chloride) concentrations were determined on a NOVA electrolyte analyzer (NOVA Biomedical, Waltham, MA). Plasma and urine[3H]inulin-specific activities were assessed by counting aliquots (0.1 mL) in Hydrofluor (National Diagnostics, Somerville, NJ) in a Beckman LS-335 liquid scintillation counter.
Blood samples were divided immediately into chilled test tubes for determinations of AVP (lithium heparin; 40 μg/mL blood) and ANF/AII(aprotinin, 0.4 trypsin-inhibiting unit/mL blood; and K2EDTA, 3 mg/mL). Tubes were vortexed and centrifuged immediately at 4 °C. Plasma samples were separated and frozen (-20 °C) for extraction within 1-2 wk. Plasma AVP extraction and RIA were performed as previously described(15, 16). Sensitivity of the AVP assay is 0.8 pg of AVP/tube, with intraassay and interassay coefficients of variation of 6 and 9%, respectively. Plasma extraction for ANF and AII determinations was performed as previously described(17) for ANF, with recoveries of added peptide of 85 ± 5 and 93 ± 1%, respectively. Plasma ANF determinations were conducted by RIA, with an assay sensitivity of 2 pg/tube and intraassay and interassay coefficients of variation of 11 and 13%, respectively(17). Plasma AII levels were determined from the ANF plasma extracts by use of RIA kits obtained from Peninsula Laboratories (Belmont, CA). Intraassay and interassay coefficients of variation for AII average 6 and 9%, respectively, with an overall assay sensitivity of 2 pg/tube.
Data analysis. All values are expressed as the mean ± SEM. Differences over time and differences among saline-, betamethasone-, and betamethasone + T4-treated groups were assessed by repeated measures two-way analysis of variance with time as the within-subjects factor and treatment as the among-subjects factor. Multiple comparison tests included either the Student-Newman Keuls or Dunnett's test, as appropriate. Statistical significance for all analyses was accepted at p < 0.05.
RESULTS
Mean body weights and umbilical cord blood pH, blood gas and hematocrit, and plasma osmolality and electrolyte values were similar among the saline-, betamethasone-, and betamethasone + T4-treated animals(Tables 1 and 2). Mean Pco2 values were maintained ± 5.3 kPa in all groups throughout experiments. Arterial Po2 values in both betamethasone-treated groups were significantly increased relative to the saline animals. Plasma sodium and chloride concentrations were similar among the study groups. Umbilical cord plasma potassium concentrations also were similar among the study groups(Table 2), and plasma potassium concentration did not change in the saline-treated lambs. However, by 180 min betamethasone- and betamethasone + T4-treated animals' plasma potassium concentrations were significantly reduced relative to their umbilical cord blood values and the 3-h saline values (Table 2). Mean blood pressure values 20 min after delivery were similar in saline-, betamethasone-, and betamethasone + T4-treated lambs (47 ± 2, 54 ± 6, and 56± 2 mm Hg, respectively). By 3 h after birth, betamethasone-treated animals exhibited significant elevations in mean blood pressure and heart rate values relative to saline-treated animals (Table 1). In contrast, in betamethasone + T4-treated animals, mean blood pressure and heart rate values, although elevated, were not statistically different from those of saline-treated animals. More detailed analyses of the pulmonary and cardiovascular data are available in other reports(18, 19). The focus of this report is the renal and endocrine results.
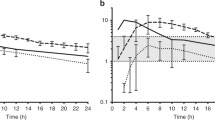
Initially, urine flow rates were significantly higher in the saline-treated animals relative to those receiving betamethasone alone. Although urine flow rates in the betamethasone + T4-treated animals tended to exceed those of both the saline-treated and betamethasone-treated lambs during the 1st h, the differences were not statistically significant. Urine flow rates were similar in all three groups by 60 min and remained stable through 180 min in the betamethasone- and betamethasone + T4-treated lambs. Thereafter, urine flow declined markedly in the saline group relative to the 40-min saline value and was significantly below the betamethasone- and betamethasone + T4-treated values by the end of observation. During the first 30 min after delivery, sodium excretion rates in the betamethasone-treated lambs were significantly below those of the saline-treated animals (Fig. 1). Consistent with the urine flow pattern, sodium excretion values tended to be higher in the betamethasone + T4-treated group during the initial hour, but were not statistically different from the saline- or betamethasone-treated lambs. Due to a gradual and significant decrease in sodium excretion in the saline-treated animals, sodium excretion was significantly higher in the betamethasone- and betamethasone + T4-treated animals by 180 min (Fig. 1).
Mean ± SEM urine flow and sodium excretion values during the 180 min after cesarean delivery in ventilated preterm lambs delivered 48 h after receiving a single ultrasound-guided intramuscular injection of saline, 0.5 mg/kg betamethasone (BETA), or betamethasone + 60 μg/kg T4 (BETA + T4).* Differs from saline, p < 0.05; **differs from the 40-min value of the same group, p < 0.05.
The apparent volumes of distribution for [3H]inulin were similar in all three groups throughout the study (Fig. 2). Plasma inulin-specific activities were stable by 60 min and did not change through 180 min. Thus, GFR values were calculated for the last two 40-min urine collection periods (100-140 and 140-180 min). Because these values did not differ within groups, the data were combined to yield a single GFR value reflecting the last 80 min of study. As evident from Figure 3, GFR values were 2-fold higher in the betamethasone- and betamethasone + T4-treated animals relative to the saline group. Fractional sodium excretion and total sodium reabsorption values also were calculated for the last two urine collection periods and expressed as a single value representing the final 80 min of observation. Although fractional sodium excretion values tended to be lower in the betamethasone- and betamethasone + T4-treated animals, there were no differences among the groups (Fig. 3). Despite the similar fractional sodium excretion rates, the total amount of sodium reabsorbed during the last 40 min of study was 2-fold higher in the betamethasone- and betamethasone + T4-treated groups relative to the saline-treated animals (Fig. 3).
Mean ± SEM plasma [3H]inulin-specific activities in ventilated preterm lambs after a single 10 μCi/kg intraarterial injection. Lambs were delivered 48 h after receiving a single ultrasound-guided intramuscular injection of saline, 0.5 mg/kg betamethasone(BETA), or betamethasone + 60 μg/kg T4 (BETA +T4).
Mean ± SEM values for GFR, fractional sodium excretion, and total sodium reabsorption in ventilated preterm lambs 180 min after cesarean delivery. Lambs were delivered 48 h after receiving a single ultrasound-guided intramuscular injection of saline, 0.5 mg/kg betamethasone(BETA), or betamethasone + 60 μg/kg T4 (BETA +T4). *Differs from saline, p < 0.05.
Values for urine osmolality, osmolar clearance, free water clearance, and potassium and chloride excretions at 180 min are summarized inTable 3. Urine osmolalities and osmolar clearances per 100 mL of GFR were not different among the treatment groups. There were no differences in free water clearance values or urinary excretions of potassium or chloride among the study groups.
Total renal blood flow and renal plasma flow rate values did not differ among the three groups (Table 1). The filtration fraction was significantly higher in betamethasone-treated animals and tended to increase in the betamethasone + T4-treated animals relative to the saline-treated group (Table 1).
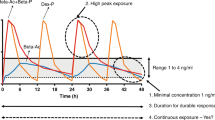
Plasma AII, AVP, and ANF values are summarized inFigure 4 andTable 2. Umbilical cord plasma values for AII and ANF were similar in the betamethasone, betamethasone + T4, and saline groups. Plasma AVP levels at delivery were significantly lower in the betamethasone-treated lambs relative to the two other groups. However, plasma AVP levels increased in all three groups and were not different by 20 min. Although plasma AVP values increased and remained elevated relative to reported fetal values(17), betamethasone- and betamethasone + T4-treated lamb plasma AVP levels were significantly below the saline-treated values at 180 min. Plasma AII levels decreased relative to the umbilical cord values and remained stable after 60 min in the betamethasone- and betamethasone + T4-treated groups. In contrast, plasma AII levels in the saline-treated animals increased after 60 min. By the end of observation plasma AII levels were more than 5-fold higher in the saline-treated lambs relative to either group receiving betamethasone. Although plasma AII levels in the betamethasone + T4-treated lambs also were lower than in the saline group, the values remained approximately 2-fold above those of the animals receiving betamethasone alone. There were no significant differences in plasma ANF levels among the groups, and plasma ANF levels did not change in any group during the study (Table 2).
Mean ± SEM plasma AII and AVP levels in cesarean-delivered, ventilated preterm lambs during the 180 min after delivery. Lambs were delivered 48 h after receiving a single ultrasound-guided intramuscular injection of saline, 0.5 mg/kg betamethasone (BETA), or betamethasone + 60 μg/kg T4 (BETA +T4). *Differs from saline, p < 0.05;+ differs from the respective umbilical cord value, p < 0.05; **differs from saline and the respective umbilical cord value,p < 0.05.
DISCUSSION
The successful transition from fetal to neonatal life involves an array of adaptive responses. Despite current sophisticated means for ventilatory and temperature support, limitations in the ability of the preterm infant to conserve sodium and water may restrict overall adaptive potential(7, 8). Demonstrated beneficial effects of glucocorticoids on pulmonary function(10, 13, 20) and limited data suggesting thyroid hormones may enhance betamethasone-induced pulmonary effects(1, 12) led us to investigate the effects of betamethasone alone and the combined effects of betamethasone + T4 on preterm newborn renal function. In addition to pronounced pulmonary(10, 12, 13, 18) and cardiovascular(19) effects, the current experiments demonstrate significant postnatal renal and endocrine changes in preterm newborn lambs delivered 48 h after a single fetal intramuscular injection of betamethasone. However, the addition of T4 did not appear to augment the effects of betamethasone alone.
The betamethasone-induced increases in GFR and urine flow observed(Figs. 1 and2) are consistent with the betamethasone-induced increases in blood pressure and GFR reported by Stonestreet et al.(4) in near term fetal and newborn lambs and with previously reported fetal responses to acute cortisol infusion(21). Although acute cortisol infusion has been reported to increase fetal renal blood flow(14), in the present studies total renal blood flow and renal plasma flow values did not differ among the three groups. Instead, the betamethasone-induced increases in GFR resulted primarily from an almost 2-fold increase in the filtration fraction. Although the higher blood pressure noted in the betamethasone-treated animals could have contributed to the increase in filtration fraction, no significant relationship between blood pressure and GFR could be demonstrated in any group. Instead, consistent with previous studies(4), we speculate the increase in filtration fraction reflects direct changes in renal vascular resistance. A direct betamethasone-induced renal vascular effect to increase GFR is important to consider because increases in filtration fraction, and not renal blood flow, are thought to explain the marked perinatal increase in GFR observed in term newborn lambs(22, 23).
Initial urine flow rates were significantly higher in saline relative to betamethasone-treated animals (Fig. 1). However, urine flow significantly decreased in the saline-treated lambs, whereas urine flow was maintained in the betamethasone- and betamethasone + T4-treated lambs. The resulting significantly higher urine flow and sodium excretion rates in the betamethasone-treated lambs relative to saline are consistent with the higher GFR values observed in those animals receiving betamethasone. Acute cortisol infusion also increases GFR and evokes natriuresis in early gestation (112 d) fetal lambs(21). However, later in gestation, the fetal natriuretic response to cortisol is reduced(24). Because negative free water clearance and similar urine osmolalities were observed in all three study groups in the present experiments, AVP-mediated water reabsorption also was apparently maximal in all three groups. Thus, despite significant differences in GFR and urine flow rates by the end of 3 h, betamethasone treatment was accompanied by appropriate increases in sodium and water reabsorption and maintained glomerulotubular balance.
Osmolar clearance values were significantly higher in the betamethasone-treated animals. However, osmolar clearance per unit GFR was not different among the study groups (Table 3). Thus, the ability of betamethasone-treated lambs to maintain similar negative free water clearances, urine osmolalities (Table 2), and fractional sodium excretion rates (Fig. 2) despite increases in filtration fraction and GFR would require an increase in renal sodium reabsorption. In agreement, total sodium reabsorption actually increased in the betamethasone-treated animals (Fig. 3). The increase in sodium reabsorption could simply reflect changes in sodium reabsorption in an attempt to maintain glomerulotubular balance in response to the increase in GFR and filtered sodium load. However, the limited ability of the preterm fetal (newborn) proximal tubule to increase sodium reabsorption(24), the larger fraction of the sodium load delivered distally(6) and the overall limited ability to initiate appropriate renal autoregulatory responses before 115 d of gestation(17) suggest renal sodium handling changed in response to prenatal betamethasone exposure. Previously reported effects of fetal glucocorticoid exposure to increase neonatal renal tubular function(3) and tubular Na,KATPase activity(25, 26), and the trend for lower fractional sodium excretion values and increases in total renal sodium reabsorption in the betamethasone-treated animals (Fig. 2) all support this possibility. Thus, in addition to renal vascular effects, as already discussed, single-dose ovine fetal betamethasone treatment increases preterm newborn renal sodium reabsorption.
Acute cortisol infusion also has been shown to decrease fetal intravascular volume(27), consistent with the slightly higher mean hematocrit values observed in the betamethasone-treated animals. However, despite the suggested differences in hematocrit and the increases in GFR and urine flow, the apparent volume of distribution of [3H]inulin and the plasma sodium and chloride concentrations were not different among the study groups. In contrast, the saline-infused animals were characterized by significantly elevated plasma potassium levels (6.2 ± 1 mEq/L), and a lower urinary potassium excretion rate relative to the betamethasone-treated animals (Tables 2 and 3). Interestingly, a similar pattern of reduced GFR and hyperkalemia is often observed in very low birth weight preterm human infants(28) and may reflect limitations in the preterm newborn's ability to maintain adequate GFR in the immediate postnatal period.
Perinatal increases in circulating AII and AVP levels are consistent with their respective effects to increase renal sodium and water reabsorption, and both peptides are potent vasoconstrictor agents. Although the immediate postnatal period was characterized by increases in fetal plasma AII and AVP levels, postnatal plasma AII and AVP levels in the betamethasone- and betamethasone +T4-treated groups were significantly lower than in the saline-treated animals (Fig. 4). Thus, the higher mean blood pressure and GFR values in the betamethasone-treated animals were not due to elevated circulating AII or AVP levels. Chronic fetal cortisol infusion suppresses basal plasma renin activity(29), renal renin gene expression(30), hepatic angiotensinogen levels(30, 31), and probably plasma AII levels in fetal sheep(27, 29, 30), but augments the renin response to hemorrhage(32). Thus, the high plasma AII levels at delivery followed by reduced levels as the betamethasone-treated groups adapted would be consistent with the reported effects of fetal cortisol treatment. Alternatively, the attenuated plasma AII levels observed in the betamethasone- and betamethasone + T4-treated animals may simply reflect changes in feedback inhibition due to the higher mean blood pressures in these animals. In addition, glucocorticoid-induced increases in vascular smooth muscle cell AII type I receptor expression may have augmented AII effectiveness(33). In contrast to the effect on plasma AII levels, fetal cortisol infusion has no effect on ovine fetal basal plasma AVP levels, or the AVP responses to hypotension, hemorrhage, or hypoxemia(34, 35). Interestingly, acute cortisol infusion has been reported to augment fetal AVP responses to hypertonicity(36). Collectively, the lower plasma AII levels observed in the betamethasone-treated animals are consistent with steroid-induced inhibition of ovine fetal renal renin release and gene expression(27, 29, 30), angiotensinogen gene expression(30, 31), and perhaps an increase in vascular AII receptors(33), although renal AII receptor expression is suppressed(30, 37). In contrast, improved cardiovascular status(20) rather than glucocorticoid-induced suppression of AVP secretion may explain the lower AVP levels observed in the betamethasone-treated animals.
In summary, we have used a ventilated lamb model to investigate postnatal renal adaptation in the premature newborn. This model has been extensively used for studies of pulmonary adaptation, and the present studies provide the first animal data on the effects of prenatal hormone treatment on premature newborn renal function. Although these initial studies were of relatively short duration (3 h), renal adaptive responses were significantly altered by a single fetal betamethasone injection 48 h before delivery. The increases in blood pressure, GFR, and sodium reabsorption are consistent with the changes expected in term newborns during this same period(22, 23). Alternatively, increases in GFR, urine flow, and sodium excretion, if maintained, could impair regulation of sodium homeostasis in the preterm newborn. Further studies extending over the first 24-48 h after delivery will be necessary to assess the overall impact of prenatal betamethasone exposure on preterm newborn renal adaptation.
Abbreviations
- AII:
-
angiotensin II
- ANF:
-
atrial natriuretic factor
- T4:
-
thyroxine
References
Ballard PL 1986 Hormones and lung maturation. Monogr Endocrinol 28: 197–235.
Crowley P, Chalmers I, Keirse M 1990 The effects of corticosteroid administration before preterm delivery: an overview of the evidence from controlled trials. Br J Obstet Gynaecol 97: 11–25.
Slotkin TA, Seidler RJ, Kavlock JAG 1992 Fetal dexamethasone exposure accelerates development of renal function: relationship to dose, cell differentiation and growth inhibition. J Dev Physiol 17: 55–61.
Stonestreet BS, Hansen NB, Laptook AR, Oh W 1983 Glucocorticoid accelerates renal functional maturation in fetal lambs. Early Hum Dev 8: 331–341.
Lumbers ER, Hill KJ, Bennett VJ 1987 Proximal and distal tubular activity in chronically catheterized fetal sheep compared with the adult. Can J Physiol Pharmacol 66: 697–702.
Robillard JE, Matson JR, Sessions C, Smith FG 1979 Developmental aspects of renal tubular reabsorption of water in the lamb fetus. Pediatr Res 13: 1172–1176.
Aperia A, Broberger O, Herin P, Thodenius K, Zetterstrom R 1983 Postnatal control of water and electrolyte homeostasis in pre-term and full-term infants. Acta Paediatr Scand Suppl 305: 61–65.
Castarino AT, Gruskay L, Corcoran RA, Polin RA, Baumgart S 1992 Sodium restriction versus daily maintenance replacement in very low birth weight premature neonates: a randomized, blind therapeutic trial. J Pediatr 120: 99–106.
Berry LM, Ikegami M, Woods E, Ervin MG 1995 Postnatal renal adaptation in preterm and term lambs. Reprod Fertil Dev 7: 491–498.
Jobe AH, Polk D, Ikegami M, Newnham J, Sly P, Kohen R, Kelly R 1993 Lung responses to ultrasound-guided fetal treatments with corticosteroids in preterm lambs. J Appl Physiol 75: 2099–2105.
Newnham JP, Kelly RW, Boyne P, Reid SE 1993 Ultrasound for research with fetal sheep. In: Neilson JP, Chambers SE (eds) Obstetric Ultrasound. Oxford University Press, New York, pp 203–222.
Polk DH, Ikegami M, Jobe AJ, Newham J, Sly P, Rolland K, Kelly R 1995 Postnatal lung function in preterm lambs: effects of a single exposure to betamethasone and thyroid hormones. Am J Obstet Gynecol 172: 872–881.
Ikegami M, Polk D, Tabor B, Lewis J, Yamada T, Jobe A 1991 Corticosteroid and thyrotropin-releasing hormone effects on preterm sheep lung function. J Appl Physiol 70: 2268–2278.
Heymann MA, Payne BD, Hoffman JIE, Rudolph AM 1977 Blood flow measurements with radionuclide-labeled particles. Prog Cardiovasc Dis 20: 55–79.
Ervin MG, Leake RD, Ross MG, Fisher DA 1985 Arginine vasotocin in ovine maternal and fetal blood, fetal urine and amniotic fluid. J Clin Invest 75: 1696–1701.
Weitzman RE, Reviczky A, Oddie TH, Fisher DA 1980 Effect of osmolality on arginine vasopressin and renin release after hemorrhage. Am J Physiol 238:E62–E68.
Ervin MG, Terry KA, Calvario G, Castro R, Ross MG, Leake RD, Fisher DA 1993 Vascular effects alter preterm fetal renal responses to vasopressin. Am J Physiol 266:R722–R729.
Chen CM, Ikegami M, Polk D, Jobe AH 1995 Fetal corticosteroid and T4 treatment effects on lung function of surfactant-treated preterm lambs. Am J Respir Crit Care Med 151: 21–26.
Padbury JF, Polk DH, Ervin MG, Berry LM, Ikegami M, Jobe AH 1995 Postnatal cardiovascular and metabolic responses to a single intramuscular dose of betamethasone in fetal sheep born prematurely by cesarean section. Pediatr Res 38: 709–715.
Stein HM, Oyama K, Martinez A, Chappell BA, Buhl E, Blount L, Padbury JF 1993 Effects of corticosteroids in preterm sheep on adaptation and sympathoadrenal mechanisms at birth. Am J Physiol 264:E763–E769.
Wintour EM, Coghlan JP, Townstoless M 1985 Cortisol is natriuretic in the immature ovine fetus. J Endocrinol 106:R13–R15.
Nakamura KT, Matherne GP, McWeeny OJ, Smith BA, Robillard JE 1987 Renal hemodynamics and functional changes during the transition from fetal to newborn life in sheep. Pediatr Res 21: 229–234.
Smith FG, Lumbers ER 1988 Changes in renal function following delivery of the lamb by cesarean section. J Dev Physiol 10: 145–148.
Hill KJ, Lumbers ER, Elbourne I 1988 The actions of cortisol on fetal renal function. J Dev Physiol 10: 85–96.
Aperia A, Larsson L 1984 Induced development of proximal tubular Na, K-ATPase, basolateral cell membranes and fluid reabsorption. Acta Paediatr Suppl 121: 133–141.
Igarashi Y, Aperia A, Larsson L, Zetterstrom R 1983 Effect of betamethasone on Na-K-ATPase activity and basal and lateral cell membranes in proximal tubular cells during early development. Am J Physiol 245:F232–F237.
Wood CE, Cheung CY, Brace RA 1987 Fetal heart rate, arterial pressure, and blood volume responses to cortisol infusion. Am J Physiol 253:R904–R909.
Shaffer SG, Kilbride HW, Hayen LK, Meade VM, Warady BA 1992 Hyperkalemia in very low birth weight infants. J Pediatr 121: 275–279.
Wood CE, Keil LC, Rudolph AM 1984 Physiological inhibition of ovine fetal plasma renin activity by cortisol. Endocrinology 115: 1792–1796.
Segar JL, Bedell K, Page WV, Mazursky JE, Nuyt AM, Robillard JE 1995 Effect of cortisol on gene expression of the renin-angiotensin system in fetal sheep. Pediatr Res 37: 741–746.
Olson AL, Robillard JE, Kisker CT, Smith BC, Perlman S 1991 Negative regulation of angiotensinogen gene expression by glucocorticoids in fetal sheep liver. Pediatr Res 30: 256–260.
Carbone GMR, Sheikh AU, Zehnder T, Rose JC 1995 Effect of chronic infusion of cortisol on renin gene expression and renin response to hemorrhage in fetal lambs. Pediatr Res 37: 316–320.
Sato A, Suzuki H, Murakami M, Nakazoto Y, Iwaita Y, Saruta T 1994 Glucocorticoid increases angiotensin II type 1 receptor and its gene expression. Hypertension 23: 25–30.
Akagi K, Berdusco ETM, Challis JRG 1990 Cortisol inhibits ACTH but not the AVP response to hypoxaemia in fetal lambs at days 123-128 of gestation. J Dev Physiol 14: 319–324.
Dix PM, Rose JC, Morris M, Hargrave BY, Meis BS, Meis PJ 1984 Cortisol infusion blocks andrenocorticotropic hormone but not vasopressin responses to hypotension in fetal lambs. Am J Obstet Gynecol 148: 317–321.
Van Den Anker JN, Wim CJ, Hop R, de Groot R, Van Der Heijden BJ, Broerse HM, Lindemans J, Sauer PJJ 1994 Effects of prenatal exposure to betamethasone and indomethacin on the glomerular filtration rate in the preterm infant. Pediatr Res 36: 578–581.
Robillard JE, Schutte BC, Page WV, Fedderson JA, Porter CO, Segar JL 1994 Ontogenic changes and regulation of renal angiotensin II type 1 receptor gene expression during fetal and newborn life. Pediatr Res 36: 755–762.
Acknowledgements
The authors gratefully acknowledge the contributions of Leslie Blount, Glenda Calvario, James Humme, James Surdilla, and Dr. Chung-Ming Chin to the completion of these studies, and the support provided by Rose Jaramillo in preparing the manuscript.
Author information
Authors and Affiliations
Additional information
Supported in part by Baxter Healthcare Corporation, Renal Division Extramural Grant Program, Grant HD-29713 from the National Institutes of Health, and an Established Investigatorship Award (to M.G.E.) from the American Heart Association.
Rights and permissions
About this article
Cite this article
Ervin, M., Berry, L., Ikegami, M. et al. Single Dose Fetal Betamethasone Administration Stabilizes Postnatal Glomerular Filtration Rate and Alters Endocrine Function in Premature Lambs. Pediatr Res 40, 645–651 (1996). https://doi.org/10.1203/00006450-199611000-00001
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199611000-00001
This article is cited by
-
A Reduction in Antenatal Steroid Dose Was Associated with Reduced Cardiac Dysfunction in a Sheep Model of Pregnancy
Reproductive Sciences (2023)
-
Effect of perinatal glucocorticoids on vascular health and disease
Pediatric Research (2017)
-
Evidence for Developmental Hypopituitarism in Ill Preterm Infants
Journal of Perinatology (2004)