Abstract
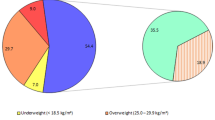
In view of their known high incidence of noninsulin dependent diabetes(NIDDM), we sought to determine whether Native American (Plains Indian) children and adolescents show evidence of risk factors for both NIDDM and cardiovascular disease. Children and adolescents between the ages of 4 and 19 y were recruited, and field days were organized for data collection, which included height, weight [to compute body mass index (BMI)], waist and hip circumference, family histories, quantum of Native American ancestry, and blood sampling for fasting lipids, apolipoproteins, insulin, and glucose. BMI increased with age in boys and girls and tended to be higher than in Caucasian children. The difference was significant in 5-9-y-old (p < 0.05) and 10-14-y-old (p < 0.05) boys and 10-14-y-old girls(p < 0.001). Ten- to 14-y-old girls in the highest quartile for BMI had higher triglyceride levels (p < 0.05) and lower HDL cholesterol (p < 0.001) when compared with those in the lower quartiles. In contrast, 15-19 y olds in the highest quartile for BMI had higher cholesterol, LDL cholesterol, and apolipoprotein B (p < 0.001). The mean fasting insulin levels were not related to BMI. The data suggest that, within this Plains Indian population, obesity associated with elevated lipid levels tends to begin at an early age in Native American children. Insulin levels do not appear to be related to BMI, a putative index of adiposity, in this population of children known to be prone to NIDDM in adult life.
Similar content being viewed by others
Main
Diabetes appears to have been rare among Native Americans before 1930(1). However, since then disease prevalence has increased(1, 2) with associated high mortality(3). In Oklahoma, a state represented by over 30 tribes, diabetes is a leading cause of death(4). Furthermore, recent evidence suggests that the onset age for NIDDM in Native Americans is decreasing(5), possibly because of the relationship between obesity and NIDDM(6) and the increase in the numbers of obese children(5). Evidence that obesity in childhood may lead to the development of diabetes and its cardiovascular complications(7) led us to suppose that early detection of predisposing factors might be particularly relevant in our Plains Indian population with a view to eventual reversal of risk.
The study was designed to explore the interrelationships between weight, BMI, lipids, apolipoproteins, insulin, and glucose in Native American children. We were particularly interested in the relationship of these factors to family history of diabetes and atherosclerosis, and degree of Native American ancestry or quantum. Also, owing to known associations of NIDDM and obesity with derangements in lipoprotein transport(7, 8), we elected to examine whether apoA-I, apoB, apoC-III, and Lp(a) could be additional markers of inherited risk. ApoA-I and apoB, the apolipoproteins associated, respectively, with HDL and LDL, have been good descriminators for atherosclerosis in adults(9, 10) and the apoA-I:apoB ratio has been shown to reflect parental myocardial infarction in children(11) implying a genetic influence on the levels. ApoC-III, a correlate of plasma triglyceride(12), has been found to be a useful predictor of atherosclerosis regression when assayed in the heparin-precipitated and supernatant fractions after the addition of heparin-manganese for the determination of HDL cholesterol(13). Also the finding that this apolipoprotein is transferred to HDL-cholesterol during lipolysis of VLDL(14) has supported use of the ratio of apoC-III in the heparin supernate to precipitate (apoC-III ratio) as an index of VLDL catabolism(15).
Lp(a), on the other hand, is classed as a lipoprotein which contains a unique protein, closely resembling plasminogen(16). Because high levels of Lp(a) predispose to atherosclerosis(17) and are genetically determined by molecular size polymorphism(18, 19), studies in Native Americans are of particular interest. A relationship of Lp(a) to diabetes had been previously suggested by the finding that decreased insulin secretion was related to high levels of Lp(a)(20, 21). We therefore added Lp(a) to a collection of candidate risk factors which we proposed to test for a relationship to a family history of either NIDDM or atherosclerosis.
METHODS
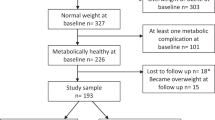
Research design. Parents of 103 Plains Indian children residing in rural and metropolitan Oklahoma were approached about the possible participation of their children in this study. With the assistance of American Indian lay workers of the Anadarko Catholic Church and the staff of the Oklahoma City Indian Clinic, parents and their children were recruited to form the study group.
After approval by the University of Oklahoma and the Indian Health Services Institutional Review Boards, respective tribal approval was granted, and informed consent was obtained at the research sites. An important part of the initial stage was the team's efforts to clearly indicate to the parents of potential participants the importance of this study and to inform them that a report on the findings of the study would be provided to them by mail, prepared without the use of overly technical or professional jargon. In addition, a brief summary of the protocol was presented to each participant and the parent(s) at the time of blood sample collection.
Subjects included 103 American Indian children (48 female and 55 male) between the ages of 4 and 19 y. The children represented 12 different Indian tribes, such as the Apache, Comanche, Cheyenne, Kiowa, Ponca, and Wichita. Over half (n = 52) of the study group were members of the Kiowa Tribe. Blood quantum levels, the proportion of Indian blood of each study group member, ranged from 12.5% to 100%. The mean blood quantum level was 68.2%.
The data collected for this study included height and weight for the calculation of BMI [weight (kg) ÷ height (m2)], waist and hip circumference, family history of cigarette smoking, obesity, diabetes, cardiovascular disease (myocardial infarction, peripheral vascular disease, and hypertension), Indian blood quantum, serum cholesterol, triglyceride, HDL cholesterol, derived LDL cholesterol, apoA-I, apoB, apoC-III, and fasting serum glucose and insulin.
Serum samples were analyzed by the Laboratory of Lipid and Lipoprotein Studies at the Oklahoma Medical Research Foundation for lipid and apolipoprotein levels using Lipid Research Clinics methodology for total cholesterol, triglyceride, and HDL cholesterol(22), followed by calculation of the LDL cholesterol using the Friedewald formula(23). Apolipoproteins were assayed by electroimmunoassay(24–26) using antibodies prepared on site. The apoC-III ratio was determined from the direct measurement of apoC-III in the supernate and precipitate after heparin-manganese precipitation(27) and computing the respective ratio. Insulin was measured with RIA using a double antibody system(28). Glucose was measured by glucose oxidase using a Beckman autoanalyzer.
Study group data were then compared with similar data from Caucasian children collected during the Lipid Research Clinics survey in 1984(29).
Statistical methods. BMI was grouped in 5-y age brackets from age 5 to 20 y and compared with predominantly Caucasian children studied by the Lipid Research Clinics using t testing. Lipid values were grouped in the same age brackets and separated by quartiles for BMI so as to compare lipid values in the highest BMI quartile with those in the lower quartiles by t testing. The lipid values were also compared with Caucasian children from Oklahoma. Fasting insulin values were log-transformed and compared with all other parameters. Pearson correlation coefficients were used to test the associations between continuous variables. Univariate analysis was used to assess distribution of the variables. Log transformation was conducted if skewness was observed. Spearman correlation coefficients were used for correlating nonparametric variables such as quantum of Indian blood and Lp(a) with the continuous variables.
Insulin, glucose, insulin resistance, triglyceride, BMI, VLDL cholesterol, and apoC-III ratio values were logtransformed due to skewness. The Pearson correlation coefficient was used to test for associations between the continuous variables and glucose, insulin, insulin:glucose ratio, BMI, and lipid values.
RESULTS
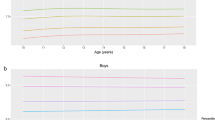
The mean BMI increased with age when examined in 5-y brackets from age 5 to 20 y in male subjects (Table 1). The mean BMI tended to be higher in the Native American children than in the Lipid Research Clinic children who were predominantly Caucasian. The difference was significant in the 5-9-y-old and 10-14-y-old boys (p < 0.05) and 10-14-y-old girls (p < 0.001) (Table 1). Ten to 14 y olds tended to have a higher triglyceride (p < 0.05) and a lower HDL cholesterol (p < 0.001) when in the highest quartiles for BMI compared with the other three (Fig. 1,Table 2). In contrast, the 15-19 y olds tended to have a higher triclyceride, LDL cholesterol, and apoB (p < 0.001) when in the highest quartile for BMI (Fig. 2,Table 2).
The mean log-transformed fasting insulin levels for Native American children (derived from Table 3) correlated with glucose(r = 0.35, p < 0.001) and with the insulin:glucose ratio (r = 0.95, p < 0.0001), but did not correlate with BMI when adjusting for age using published BMI norms and percentiles for age(30).
There were no significant associations with Lp(a) using nonparametric testing.
CONCLUSIONS
The tendency for Native American children to have a higher BMI earlier than children in the much larger Lipid Research Clinics population suggests that obesity in the Oklahoma Plains Indian population begins at an early age. A similar observation in American Indians and Alaskan Natives(5) supports the hypothesis that prevailing cultural influences on genetic predisposition to obesity are operative in childhood. North American Indian tribes are thought to have undergone a secular change in body composition in the earlier part of this century judging from photographs which showed them to be lean(1). It follows that cultural changes known to have been in effect during this same period may have contributed to both the increased prevalence of obesity in both children(5) and adults(1). Because NIDDM in Native American tribes increased substantially during this period(1, 6), obesity can be implicated as a major predisposing factor(2, 3). However, it should be pointed out that increased weight may in part be attributed to gains in lean body mass, meaning that BMI may not be an ideal index of adiposity for all growing children and adolescents.
The mean insulin levels in Pima Indian children were found to be increased relative to a control Caucasian population(31), a finding which may predict risk for NIDDM(32), but in this cross-sectional study, fasting insulin failed to correlate with BMI when adjusted for age. We were unable to compare insulin levels with previously published studies owing to known variation in insulin assay methodology and lack of reliable standards. However, it is likely that cross-cultural comparison would show differences in fasting insulin(31), and insulin level could be a predictor of NIDDM in Native American children, because ongoing studies on adults in the same population have estimated the prevalence of NIDDM in adults aged 45-74 y to be 38% in men and 42% in women(33, 34).
We also investigated whether early and excessive weight gain in adolescence is associated with adverse lipid and apolipoprotein distribution among lipoproteins. Our finding, that adolescents in the highest quartile for BMI, aged 10-15 y, had a higher triglyceride level but a lower HDL cholesterol level, suggests that the early phases of adolescent weight gain are associated with defective triglyceride disposal(15). These findings indicate that these adolescents become at increased risk for atherosclerosis when they become obese, a phenomenon which is known to occur in adults(35–37). Specifically, the lipoprotein distribution appears to change with age from one characterized by predominant hypertriglyceridemia in the younger obese adolescents to a hypercholesterolemic pattern in the older obese adolescents. The obese younger adolescents were relatively hypertriglyceridemic with a lower HDL cholesterol, but the older obese adolescents aged 15-20 y had a higher LDL cholesterol and apoB values compared with their nonobese counterparts. This observation is comparable to the finding of a correlation of obesity with LDL cholesterol in older adolescents and young adults of Caucasian origin residing in Bogalusa, in contrast to neighboring black children(38). However, the total sample size was smaller in this pilot study, and after stratification reduced statistical power could have been insufficient to demonstrate significance. It should also be pointed out that the significant differences occurred within the desirable ranges for age and therefore should not be considered abnormal but suggesting a trend for relatively increased lipid levels in these Native American adolescents.
Our question, whether a family history of diabetes or heart attacks was associated with biochemical markers of lipoprotein transport, was unanswered because there were no associations with either a family history of diabetes or cardiovascular disease. Previous associations of Lp(a) with insulin secretion(20, 21) have been observed, suggesting that Lp(a) may have a relationship to β cell failure, a recognized sequel to insulin resistance(39); however, larger studies may be required to support or disprove these earlier findings. Many studies have shown Lp(a) to be significantly associated with risk for atherosclerosis(17, 19, 40), whereas some studies have had negative conclusions(41, 42). Our failure to relate Lp(a) to a family history of heart attacks may have been due to a relatively low rate of cardiovascular disease as reported in some American Indian tribes(1) or the impression among Native American tribes that diabetes is always the primary illness despite the presence of underlying primary defects in lipoprotein transport which may have resulted in heart attacks.
Because adverse health outcomes associated with both obesity and early development of atherosclerosis are potentially reversible at an early age(43, 44), the results of our study provide a rationale for investigation of serial change in lipid profiles in longitudinal studies which take into account the influence of age-dependent and culture-specific life style trends. Because the onset and progression of obesity precedes and may predict NIDDM and is associated with the development of high risk lipoprotein profiles, intervention strategy should be aimed at early assessment followed by attempts to modify life style-related factors such as diet and exercise. Subsequent decreases in body fat and plasma lipid levels may then result in improved long-term cardiovascular health.
Abbreviations
- NIDDM:
-
noninsulin-dependent diabetes mellitus
- BMI:
-
body mass index
- ApoA-I, apoB, and apoC-II:
-
apolipoproteins A-I, B, and C-II
- Lp(a):
-
lipoprotein (a)
References
West KM 1974 Diabetes in American Indians and other populations of the new world. Diabetes 23: 841–855
Knowler WC, Pettitt DJ, Savage PJ, Bennett PH 1981 Diabetes incidence in Pima Indians: contributions of obesity and parental diabetes. Am J Epidemiol 113: 144–156
Pettitt DJ, Lisse JR, Knowler WC, Bennett PH 1982 Mortality as a function of obesity and diabetes. Am J Epidemiol 115: 359–366
U.S. Congress, Office of Technology Assessment, Indian Health Care 1986 OTA-H-290. U.S. Government Printing Office, Washington, DC
Broussard BA, Johnson A, Hines JH, Story M, Fichtner R, Hauck F, Bachman-Carter K, Hayes J, Frohlich K, Gray N, Valway S, Gohdes D 1991 Prevalence of obesity in American Indians and Alaska Natives. Am J Clin Nutr 53: 1535S–1542S
Knowler WC, Pettitt DJ, Saad MF, Charles MA, Nelson RG, Howard BV, Bogardus C, Bennett PH 1991 Obesity in the Pima Indians: its magnitude and relationship with diabetes. Am J Clin Nutr 53: 1543S–1551S
Garrison RJ, Wilson PW, Castelli WP, Feinlieb M, Kannel WB, McNamara PM 1980 Obesity and lipoprotein cholesterol in the Framingham offspring study. Metabolism 29: 1053–1060
Haffner SM, Stern MP, Hazuda HP, Mitchell BD, Patterson JK, Ferrani E 1989 Parental history of diabetes is associated with increased cardiovascular risk factors. Arteriosclerosis 9: 928–933
Avogaro P, Bon GB, Cazzolato G, Quincy GB 1979 Are apolipoproteins better descriminators than lipids for atherosclerosis?. Lancet 1: 901–903
Riesen WF, Mordasini R, Salzmann C, Theler A, Gurtner HP 1980 Apoproteins and lipids as descriminators of severity of coronary heart disease. Atherosclerosis 37: 157–162
Freedman DS, Srinivasan SR, Shear CL, Franklin FA, Webber LS, Berenson GS 1986 The relation of apolipoproteins A-I and B in children to parental myocardial infarction. N Engl J Med 315: 721–726
Schonfeld G, George PK, Miller J, Reilly P, Witztum J 1979 Aolipoprotein C-II and C-III levels in hyperlipoproteinemia. Metabolism 28: 1001–1009
Blankenhorn DH, Nessim SA, Johnson RL, Sanmarco ME, Azen SP, Cashen-Hemphill L 1987 Beneficial effects of combined colestipol-niacin therapy on coronary atherosclerosis and coronary venous bypass grafts. JAMA 257: 3233–3240
Chajek T, Eisenberg S 1978 Very low density lipoprotein metabolism of phospholipids, cholesterol, and apolipoprotein C in the isolated perfused rat heart. J Clin Invest 61: 1654–1665
Alaupovic P 1981 David Rubenstein Memorial Lecture: the biochemical and clinical significance of the interrelationship between very low density and high density lipoproteins. Can J Biochem 59: 565–579
Eaton DL, Fless GM, Kohr WJ, McClean JW, Xu QT, Miller CG, Lawn RM, Scanu AM 1987 Partial amino acid sequence of apolipoprotein (a) shows that it is homologous to plasminogen. Proc Natl Acad Sci USA 84: 3224–3228
Dahlen G, Berg K, Gillnas T 1975 Lp(a) lipoprotein/pre-β-lipoprotein in Swedish middle-aged males and in patients with coronary heart disease. Clin Genet 7: 334–341
Scanu AM 1990 Lipoprotein (a): a genetically determined cardiovascular pathogen in search of a function. J Lab Clin Med 116: 142–146
Scanu AM, Fless GM 1990 Lipoprotein (a): heterogeneity and biological relevance. J Clin Invest 85: 1709–1715
Dahlen G, Berg K 1976 Pre-β-lipoprotein and Lp(a) antigen in relation to triglyceride levels and insulin release following an oral glucose load in middle-aged males. Acta Med Scand 199: 413–419
Dahlen G, Berg K 1979 Confirmation of an influence of the inherited Lp(a) variation on serum insulin and glucose levels. Clin Genet 16: 418–427
Lipid Research Clinics Program Manual of Laboratory Operations, Lipid and Lipoprotein Analysis 1974 DHEW Publication No. NIH 75-628, Vol I. U.S. Government Printing Office, Washington, DC
Friedewald WT, Levy RI, Fredrickson DS 1972 Estimation of the concentration of low density lipoprotein cholesterol in plasma, without the use of preparative ultracentrifugation. Clin Chem 18: 499–502
Curry MD, Alaupovic P, Suenram CA 1976 Determination of apolipoprotein A and its constitutive A-I and A-II polypeptides by separate electroimmunoassays. Clin Chem 22: 315–322
Curry MD, Gustafson A, Alaupovic P 1978 Electroimmunoassay, radioimmunoassy and radial immunodiffusion assay evaluated for quantification of human apolipoprotein. B Clin Chem 24: 280–286
Curry MD, McConathy WJ, Fesmire JD, Alaupovic P 1980 Quantitative determination of apolipoprotein C-III by electroimmunoassay. Biochim Biophys Acta 617: 503–513
Burstein M, Scholnick HR, Morfin R 1970 Rapid method for the isolation of lipoproteins from human serum by precipitation with polyanions. J Lipid Res 11: 583–595
Morgan CR, Lazarow AL 1963 Immunoassay of insulin: two antibody system: plasma insulin levels of normal, subdiabetic and diabetic rats. Diabetes 12: 115–126
Christensen B, Glueck C, Kwiterovitch P, Degroot I, Chase G, Heiss G, Mowery R, Tamir I, Rifkind B 1980 Plasma cholesterol and triglyceride distributions in 13, 665 children and adolescents: the prevalence study of the Lipid Research Clinics program. Pediatr Res 14: 194–202
Hammer LD, Kraemmer HC, Wilson DM, Ritter PL, Dornbusch SM 1991 Standardized percentile curves of body mass index for children and adolescents. Am J Dis Child 145: 259–263
Pettitt DJ, Moll PP, Knowler WC, Mott DM, Nelson RG, Saad MF, Bennett PH, Kottke BA 1993 Insulinemia in children at low and high risk of NIDDM. Diabetes Care 16: 608–615
Zimmett PZ, Collins VR, Dowse GK, Knight LT 1992 Hyperinsulinemia in youth is a predictor of type II (non-insulin-dependent) diabetes mellitus. Diabetologia 35: 534–541
Howard BV, Welty TK, Fabsitz RR, Cowan LD, Oopik AJ, Le NA, Yey J, Savage PJ, Lee ET 1992 Risk factors for coronary heart disease in diabetic and nondiabetic Native Americans. Diabetes 41( suppl 2): 4–11
Lee ET, Anderson PS, Bryan J, Bahr C, Coniglione T, Cleves M 1985 Diabetes, parental diabetes, and obesity in Oklahoman Indians. Diabetes Care 8: 107–113
Hubert HB, Feinlieb M, McNamara PM, Castelli WP 1983 Obesity as an independent risk factor for cardiovascular disease: a 26 year followup of participants in the Framingham Heart Study. Circulation 67: 968–977
Aristimuno GG, Foster TA, Voors AW, Srinivasan SR 1984 Influence of persistent obesity in children on cardiovascular risk factors: the Bogalusa Heart Study. Circulation 69: 895–904
Smoak SC, Burke GL, Webber LS, Srinivasan SR, Berenson GS 1987 Relation of obesity to clustering of cardiovascular disease risk factors in children and young adults: the Bogalusa Heart Study. Am J Epidemiol 125: 364–372
Wattigney WA, Harsha DW, Srinivasan SR, Webber LS, Berenson GS 1991 Increasing impact of obesity on serum lipids and lipoproteins in young adults. Arch Intern Med 151: 2017–2022
Weir GC 1982 Non-insulin dependent diabetes mellitus: interplay between B-cell inadequacy and insulin resistance. Am J Med 73: 461–464
Dahlen GH, Guyton GR, Attar M, Farmer JA, Kautz JA, Gotto AM Jr 1986 Association of levels of lipoprotein Lp(a), plasma lipids, and other lipoproteins with coronary artery disease documented by angiography. Circulation 74: 758
Jauhiainen M, Koskinen P, Ehnholm C, Frick MH, Mantarri M, Manninen V, Huttunen JK 1991 Lipoprotein (a) and coronary heart disease risk: a nested case-control study of the Helsinki Heart Study participants. Atherosclerosis 89: 59–67
Durrington PN, Ishola M, Hunt L 1988 Apolipoproteins(a), A-I, and B and parental history in men with early onset ischaemic heart disease. Lancet 2: 1070
Butcher AH, Frank GC, Harsha DW, Serpas DC, Little SD, Nicklas TA, Hunter SM, Berenson GS 1988 Heart Smart: a school health program meeting the 1990 objectives for the nation. Health Educ Q 15: 17–34
Walter HJ, Hofman A, Vaughn RD, Wynder EL 1988 Modification of risk factors for coronary heart disease. Five-year results of a school-based intervention trial. Modification of risk factors for coronary heart disease. N Engl J Med 318: 1093–1100
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Blackett, P., Taylor, T., Russell, D. et al. Lipoprotein Changes in Relation to Body Mass Index in Native American Adolescents. Pediatr Res 40, 77–81 (1996). https://doi.org/10.1203/00006450-199607000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199607000-00014