Abstract
Background:
Admission to hospital with chronic obstructive pulmonary disease (COPD) is associated with deprivation and season. However, it is not known whether deprivation and seasonality act synergistically to influence the risk of hospital admission with COPD.
Aims:
To investigate whether the relationship between season/temperature and admission to hospital with COPD differs with deprivation.
Methods:
All COPD admissions (ICD10 codes J40-J44 and J47) were obtained for the decade 2001–2010 for all Scottish residents by month of admission and 2009 Scottish Index of Multiple Deprivation (SIMD) quintile. Confidence intervals for rates and absolute differences in rates were calculated and the proportion of risk during winter attributable to main effects and interactions were estimated. Monthly rates of admission by average daily minimum temperatures were plotted for each quintile of SIMD.
Results:
Absolute differences in admission rates between winter and summer increased with greater deprivation. In the most deprived quintile, in winter 19.4% (95% CI 17.3% to 21.4%) of admissions were attributable to season/deprivation interaction, 61.2% (95% CI 59.5% to 63.0%) to deprivation alone, and 5.2% (95% CI 4.3% to 6.0%) to winter alone. Lower average daily minimum temperatures over a month were associated with higher admission rates, with stronger associations evident in the more deprived quintiles.
Conclusions:
Winter and socioeconomic deprivation-related factors appear to act synergistically, increasing the rate of COPD admissions to hospital more among deprived people than among affluent people in winter than in the summer months. Similar associations were observed for admission rates and temperatures. Interventions effective at reducing winter admissions for COPD may have potential for greater benefit if delivered to more deprived groups.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of mortality and morbidity with approximately 2.7 million deaths and more than 26 million disability-adjusted life years lost globally in 2000.1 Hospital admissions account for the majority of healthcare-associated costs for COPD.2
Admission to hospital with COPD is associated with seasonal variation3 as well as deprivation,4 while low socioeconomic status5 and low temperature6 are both associated with an increased risk of COPD exacerbation. Previous studies have identified that an increased risk of mortality in winter differs by socioeconomic status.7 However, it is not known whether deprivation and seasonality act synergistically to influence the risk of hospital admission with COPD.
Detecting interactions requires a larger number of events than is needed for studies examining main effects. We used national data over a 10-year period to investigate whether the relationship between season or temperature and admission to hospital with COPD differed by an area-based measure of socioeconomic status, the Scottish Index of Multiple Deprivation (SIMD).8
Methods
All COPD admissions (identified using International Classification of Diseases 10th revision codes J40-J44 and J47) were identified for the decade 2001–2010 for all Scottish residents by month of admission and 2009 SIMD quintile from national hospital records held by Information Services Division (ISD), NHS National Services Scotland. SIMD quintiles are calculated on a three-yearly basis for each super output area in Scotland. The SIMD score is obtained from a weighted sum of seven domains (employment, income, crime, housing, health, education, and access). Details of the individual components of each domain and the method of weighting and combining these are available at the Scottish Government website (http://www.scotland.gov.uk/Topics/Statistics/SIMD/BackgroundMethodology).
Person-years for each quintile by age and sex were calculated as one-fifth of the sum of each mid-year population estimate for Scotland. Monthly averages of daily minimum temperatures in Scotland for the same period were obtained from the Meteorological Office (www.metoffice.gov.uk/climate/uk/datasets).
Confidence intervals (CIs) for COPD admission rates and absolute differences in the rate for each season were calculated assuming Poisson and binomial distributions, respectively. Interaction ‘effects’ reported directly from most regression models other than linear regression (such as Poisson, logistic, Cox) reflect interaction on a multiplicative scale and have limited interpretability. Instead, using the method proposed by Rothman,9 we estimated the proportion of risk attributable to winter, to deprivation, and to the interaction between these main effects (the Attributable Proportion, AP) on the additive scale, which is relevant both for biological inferences and health service planning. CIs and p values for the relative excess risk of interaction (RERI) were obtained using a parametric bootstrap method similar to that described by Osman et al.,10 although we used a Poisson rather than a binomial distribution and did not apply a continuity correction given the large number of events. In sensitivity analyses we repeated the estimation for RERI and the AP using the method described by Hosmer and Lemeshow, implemented with the R package EpiR.11,12
Monthly rates of admission by average daily minimum temperatures were calculated and plotted for each quintile of SIMD, and point estimates and 95% CIs were obtained using negative binomial regression. We calculated RERI using parametric bootstrap methods in a similar manner as for season, treating SIMD quintile as a continuous variable as RERI is interpretable when both exposure variables are continuous.13 Statistical analyses were performed in R 2.13.1 (Vienna, Austria).
Results
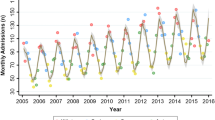
Admission rates were considerably higher in the more deprived quintiles than in the least deprived quintiles for all seasons of the year (Table 1).
Absolute differences in admission rates between winter and summer increased with increasing deprivation. The 95% CIs for these effect measures did not overlap, providing evidence of effect measure heterogeneity on an additive scale. Furthermore, the relative risk for interaction was 1.36 (95% CI 1.21 to 1.51, p<0.001), indicating that there was evidence of interaction on an additive scale.
Assuming that the rates of admission were reasonable approximates for risks and that there is no confounding, 19.4% (95% CI 17.3% to 21.4%) of the increased risk (attributable proportion) of admissions among the most deprived quintile in winter were estimated to be attributable to the interaction between winter and deprivation, 61.2% (95% CI 59.5% to 63.0%) to deprivation alone, and 5.2% (95% CI 4.3% to 6.0%) to winter alone. Identical confidence intervals (to two decimal places) were obtained for the RERI and AP using the method of Hosmer and Lemeshow.11
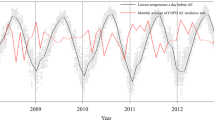
There were similar associations with COPD admissions for temperature by deprivation. Lower daily minimum temperatures (averaged over a month) were associated with higher admission rates, with the strongest associations evident in the more deprived quintiles (Figure 1). Across the full range of temperatures, admission rates were consistently higher for more deprived quintiles. There was no year-to-year variability evident (data not shown). The RERI was 0.83 (95% CI 0.71 to 0.95, p<0.001) which can be interpreted as follows:13 for every 5°C decrease in average daily minimum temperature and change from the least deprived to most deprived quintile, the monthly relative risk of admission is 0.83 higher than if there had been no interaction.
Discussion
Main findings
Winter and socioeconomic deprivation appear to act synergistically, being associated with the rate of COPD admissions to hospital in winter (compared with summer) to a greater extent among more deprived people than among less deprived people. Similar associations by deprivation were observed between COPD admission rates and minimum temperatures. Similar previous associations have been reported for an interaction between socioeconomic status, winter and all-cause mortality, but we are not aware of a previous study demonstrating this effect for admission to hospital with COPD.
Interpretation of findings in relation to previously published work
The differences between deprivation quintiles were large, with five times as many excess winter admissions in the most deprived groups compared with the least deprived groups. The specific mechanism underlying the increased association between winter and admission to hospital with COPD in people from more deprived areas is unknown. Maintaining the warmth guideline of 21°C in living areas for at least 9 hrs/day is associated with better health status among people with COPD,14 and maintaining homes at this temperature may be more difficult for people living in more deprived areas. Much of the current research into the role of temperature/deprivation and morbidity/mortality has focused on housing quality and ability to heat the home. Findings have included associations between poor housing quality and respiratory illness,15 and also the fact that fuel poverty is related to poor health.16
Smoking is associated with area-based measures of deprivation,17,18 and smoking is both a major determinant of indoor air pollution and is associated with symptom burden in people with COPD.19 Indoor air quality is likely be worse in more deprived areas than in less deprived areas, and this difference may have a larger effect in winter when people appear to spend more time indoors and in motor vehicles.20
Alternatively, since airflow limitation (which defines COPD) is associated with deprivation,21 there may be a larger pool of people with underlying COPD among whom susceptibility to admission is unmasked by winter-related factors. Cohort studies in prevalent COPD populations are needed to identify whether seasonal differences in rates of admission differ by deprivation among people with established COPD as well as in the general population.
We examined the statistical interaction on an additive scale throughout this analysis. Where interaction is used in the statistical sense, interaction in additive models implies no interaction in multiplicative models and vice versa. Hence, statistical interaction is a function of the particular form of model chosen and is therefore of no intrinsic significance. Coefficients obtained from interaction terms (parameters) of most regression models (e.g. Poisson, logistic, Cox) correspond to interaction on a multiplicative scale, which has limited direct interpretability. As argued by Rothman, if biological interaction is present, the risk in any population with dual exposures should be more (or less) than the sum of the attributable risk for each single exposure plus the risk in those who are unexposed; as such it is defined in terms of interaction on an additive scale.9 Notwithstanding discussions around what constitutes biological interaction, from the health service planning and public health perspective, interaction on the additive scale is of most relevance as this translates directly to important clinical and health service-related measures such as absolute risk reduction and numbers needed to treat.
Strengths and limitations of this study
This study uses the robust data collected by ISD, NHS National Services Scotland. By including all COPD admissions in this way, we believe this work reflects the target population (Scottish residents) and minimises the risk of any bias.
This work is limited by the use of average temperatures across the country and therefore does not take account of significant regional variation or the effects of maximum/minimum temperatures.
An additional limitation of our study is that we analysed aggregated data and were therefore unable to take into account the fact that some of the admissions pertain to the same patients, thus the CIs may be too narrow. However, given the magnitude of the interaction, we think that this would have been unlikely to make a substantial difference to the conclusions. Indeed, the p value for the RERI was <1×10−4.
Implications for future research, policy and practice
Excess winter admissions to hospital with COPD are higher among people from deprived areas. Public health interventions aimed at reducing winter admissions with COPD should focus on more deprived groups.
Conclusions
Our findings imply that population-wide interventions aimed at reducing winter admissions with COPD (such as winter fuel benefits or subsidised home insulation) may have potential for greater benefit if delivered to more deprived groups. Indeed, our estimates suggest that eliminating the effects of winter among 100,000 persons for one year would lead to a reduction of an additional 320 COPD admissions if targeted at the most deprived quintile rather than the least deprived quintile.
References
Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J 2006;27(2):397–412. http://dx.doi.org/10.1183/09031936.06.00025805
Britton M . The burden of COPD in the UK: results from the confronting COPD survey. Respir Med 2003;97(Suppl 3):S71–9. http://dx.doi.org/10.1016/S0954-6111(03)80027-6
Bryden C, Bird W, Halpin D, Levy M, eds. Seasonality in COPD emergency admissions to hospital and predictability using surveillance for influenza-like-illness. BTS Winter Meeting, 2006.
Calderon-Larranaga A, Carney L, Soljak M, et al. Association of population and primary healthcare factors with hospital admission rates for chronic obstructive pulmonary disease in England: national cross-sectional study. Thorax 2010;66(3):191–6. http://dx.doi.org/10.1136/thx.2010.147058
Eisner MD, Blanc PD, Omachi TA, et al. Socioeconomic status, race and COPD health outcomes. J Epidemiol Community Health 2011;65(1):26–34. http://dx.doi.org/10.1136/jech.2009.089722
Donaldson GC, Seemungal T, Jeffries DJ, Wedzicha JA . Effect of temperature on lung function and symptoms in chronic obstructive pulmonary disease. Eur Respir J 1999;13(4):844–9. http://dx.doi.org/10.1034/j.1399-3003.1999.13d25.x
Healy JD . Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health 2003;57(10):784–9. http://dx.doi.org/10.1136/jech.57.10.784
Scottish Government SAsH. Evaluation of statistical techniques in the Scottish Index of Multiple Deprivation. 2005. Available from: http://www.scotland.gov.uk/Publications/2005/10/1893201/32023.
Rothman KJ . The estimation of synergy or antagonism. Am J Epidemiol 1976;103(5):506–11.
Nie L, Chu H, Li F, Cole SR . Relative excess risk due to interaction. Epidemiology 2010;21(4):552–6. http://dx.doi.org/10.1097/EDE.0b013e3181e09b0b
Hosmer DW, Lemeshow S . Confidence interval estimation of interaction. Epidemiology 1992;3(5):452–6. http://dx.doi.org/10.1097/00001648-199209000-00012
Stevenson M, Nunes T, Sanchez J, et al. epiR: An R package for the analysis of epidemiological data. 0.9-45 ed 2012. http://CRAN.R-project.org/package=epiR
Knol MJ, van der Tweel I, Grobbee DE, Numans ME, Geerlings MI . Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int J Epidemiol 2007;36(5):1111–18. http://dx.doi.org/10.1093/ije/dym157
Osman LM, Ayres JG, Garden C, Reglitz K, Lyon J, Douglas JG . Home warmth and health status of COPD patients. Eur J Public Health 2008;18(4):399–405. http://dx.doi.org/10.1093/eurpub/ckn015
Blane D, Mitchell R, Bartley M . The ‘inverse housing law’ and respiratory health. J Epidemiol Community Health 2000;54(10):745–9. http://dx.doi.org/10.1136/jech.54.10.745
de Vries R, Blane D . Fuel poverty and the health of older people: the role of local climate. J Public Health 2012 Nov 23 [Epub ahead of print].
Shohaimi S, Luben R, Wareham N, et al. Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk Cohort of the European Investigation into Cancer (EPIC-Norfolk). J Epidemiol Community Health 2003;57(4):270–6. http://dx.doi.org/10.1136/jech.57.4.270
Kleinschmidt I, Hills M, Elliott P . Smoking behaviour can be predicted by neighbourhood deprivation measures. J Epidemiol Community Health 1995;49(Suppl 2):S72–7. http://dx.doi.org/10.1136/jech.49.Suppl_2.S72
Osman LM, Douglas JG, Garden C, et al. Indoor air quality in homes of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2007;176(5):465–72. http://dx.doi.org/10.1164/rccm.200605-589OC
McCurdy T, Graham SE . Using human activity data in exposure models: analysis of discriminating factors. J Expos Sci Environ Epidemiol 2003;13(4):294–317. http://dx.doi.org/10.1038/sj.jea.7500281
Mannino DM, Buist AS . Global burden of COPD: risk factors, prevalence, and future trends. Lancet 2007;370(9589):765–73. http://dx.doi.org/10.1016/S0140-6736(07)61380-4
Acknowledgements
Handling editor David Bellamy
Statistical review Gopal Netuveli
Funding No funding was received for the writing of this paper.
Author information
Authors and Affiliations
Contributions
DAM made substantial contributions to conception and design, acquisition of data and analysis and interpretation of data, and drafted the article. JRM made substantial contributions to conception and design and analysis and interpretation of data. CMF made substantial contributions to acquisition of data and analysis and interpretation of data. WM made substantial contributions to conception and design. SHW made substantial contributions to conception and design and analysis and interpretation of data. All authors revised the article critically for important intellectual content and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest in relation to the article.
Rights and permissions
About this article
Cite this article
McAllister, D., Morling, J., Fischbacher, C. et al. Socioeconomic deprivation increases the effect of winter on admissions to hospital with COPD: retrospective analysis of 10 years of national hospitalisation data. Prim Care Respir J 22, 296–299 (2013). https://doi.org/10.4104/pcrj.2013.00066
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2013.00066
This article is cited by
-
Findings from a pilot randomised trial of a social network self-management intervention in COPD
BMC Pulmonary Medicine (2020)
-
A non-randomised controlled pilot study of clinical pharmacist collaborative intervention for community dwelling patients with COPD
npj Primary Care Respiratory Medicine (2018)
-
Which patients with advanced respiratory disease die in hospital? A 14-year population-based study of trends and associated factors
BMC Medicine (2017)
-
A retrospective study of the impact of a telephone alert service (Healthy Outlook) on hospital admissions for patients with chronic obstructive pulmonary disease
npj Primary Care Respiratory Medicine (2014)