Abstract
A major revision of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines was published in December 2011, which takes account of the fact that chronic obstructive pulmonary disease (COPD) is a multi-system disease with effects on the patient beyond the effects of airflow limitation alone. The guidelines present a novel way of assessing the patient with COPD, linked to the major goals of stable COPD management of reducing symptoms (measured by the modified Medical Research Council Dyspnoea Score and/or COPD Assessment Tool) and reducing future risk (measured by the severity of airflow limitation and/or exacerbation history in the previous 12 months). Four patient groups are identified on the basis of their symptom/risk profile and a pharmacotherapy strategy is described using this profile. Emphasis is still placed on three pivotal features of non-pharmacological management: (1) reduction of exposure to risk factors (principally tobacco smoke); (2) promotion of exercise; and (3) immunisation against influenza and pneumococcal disease. In addition, there is a new chapter on the importance of assessing and treating co-morbid disease. The guidelines are a welcome advance in the management of COPD, but need further development to guide the more holistic approach to the management of patients with COPD in primary care.
Similar content being viewed by others
Introduction
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) produced its first consensus report on the global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (COPD) in 2001.1 Since then the GOLD guidelines have been adopted worldwide, influencing national guidelines and the design of international clinical trials in COPD. The report has been updated annually from 2006, but a major revision was published in December 20112 containing changes related to diagnosis, assessment, management of stable disease, and management of co-morbidities.
This article discusses these changes and the implications for primary care.
Diagnosis and assessment
Diagnosis
The key points are:
“A clinical diagnosis of COPD should be considered in any patient who has dyspnoea, chronic cough or sputum production and/or a history of exposure to risk factors for the disease”.
“Spirometry is required to make the diagnosis in this clinical context; the presence of a post-bronchodilator FEV1/FVC <0.70 confirms the presence of airflow limitation and thus of COPD”.
This confirms the importance of post-bronchodilator spirometry in making a diagnosis of COPD. There has been considerable debate about whether the fixed ratio of <0.7 or the lower limit of normal (LLN) of forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) should be used to define airflow limitation.3 The GOLD 2011 guidelines have advocated using the fixed ratio, citing lack of suitable reference equations and longitudinal studies validating use of the LLN. This is in line with the National Institute for Health and Clinical Excellence (NICE) UK COPD guidelines (2010)4 and the American College of Physicians (ACP), American College of Chest Physicians (ACCP), American Thoracic Society (ATS) and European Respiratory Society (ERS) guidelines (2011).5 However, it is acknowledged that the fixed ratio tends to over-diagnose airflow limitation in the elderly and under-diagnoses airflow limitation in patients aged <45 years. When screening or case-finding patients with undiagnosed COPD using spirometry, it is therefore important that the patient has the characteristic symptoms of COPD and not merely apparent airflow limitation.
Assessment
The aims of assessment are:
-
To determine the impact of the disease upon the patient's life.
-
To determine the risk of future events (exacerbations, mortality).
-
To guide therapy.
Traditionally, GOLD guidelines have equated severity of disease with the severity of airflow limitation (GOLD 1=mild, GOLD 2=moderate, GOLD 3=severe, GOLD 4=very severe).1,2 However there is only a weak correlation between FEV1, symptom severity, and patient health status,6 whilst there is an increasing appreciation of the role of co-morbidities such as cardiovascular disease, depression and muscle wasting7 on COPD control. The severity of airflow limitation is a positive predictor of mortality and hospitalisations, but a history of frequent exacerbations (≥2 exacerbations in the previous year) is itself a strong predictor of future risk.8
In light of these changes in thinking about COPD as being more than a disease of airflow limitation, the 2011 GOLD guidelines propose a new system of assessment linked to management which incorporates measurement of:
-
1
Symptoms and/or health status using the modified British Medical Research Council Dyspnoea Scale (mMRC) (see Table 1) and the eight-question COPD Assessment Tool (CAT).9 An mMRC score of ≥2 or a CAT score of ≥10 is indicative of high impact of symptoms.
Table 1 Modified Medical Research Council Dyspnoea Scale*. From the Global Strategy for Diagnosis, Management, and Prevention of COPD, revised 2011.2 Used with permission from the Global Initiative for Chronic Obstructive Lung Disease (GOLD), www.goldcopd.org -
2
Future risk determined by exacerbation history and degree of airflow limitation using the GOLD classification. GOLD 3 or 4 (severe/very severe) or a history of ≥2 exacerbations in the previous year confers ‘high risk’. If both these indices are used to assess risk, the highest risk score is used.
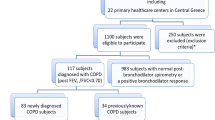
These measurements are used to divide patients into four groups (Figure 1):
-
Group A: low risk, less symptoms — typically GOLD 1 or 2 and/or 0–1 exacerbations per year, mMRC score <2 or CAT score <10.
-
Group B: low risk, more symptoms — typically GOLD 1 or 2 and/or 0–1 exacerbations per year, mMRC score ≥2 or CAT score ≥10.
-
Group C: high risk, less symptoms — typically GOLD 3 or 4 and/or ≥2 exacerbations per year, mMRC score 0–1 or CAT score <10.
-
Group D: high risk, more symptoms — typically GOLD 3 or 4 and/or ≥2 exacerbations per year, mMRC score ≥2 or CAT score ≥10.
Association between symptoms, spirometric classification and future risk of exacerbations. From the Global Strategy for Diagnosis, Management, and Prevention of COPD, revised 2011.2 Adapted and used with permission from the Global Initiative for Chronic Obstructive Lung Disease (GOLD), www.goldcopd.org
In addition, the guidelines state that an assessment of co-morbidities should be made and treated (see later), plus additional investigations such as pulse oximetry (in stable patients with FEV1 <35% predicted and/or signs of cor pulmonale/respiratory failure), radiological imaging, and more specialist tests such as lung volume testing and diffusion capacity in selected patients.
Management
The 2011 GOLD guidelines have condensed the goals of stable COPD management into two major aims: (1) reduction of symptoms and (2) reduction of future risk. This is shown in Figure 2. However, the use of ‘reduction of symptoms’ alone as an overarching aim tends to undervalue the role of co-morbidities and the impact of the disease on the daily life of the patient. It is therefore proposed that the goals of COPD management in primary care should be to: (1) improve current control, defined as improvement in symptoms, daily activities, co-morbidities (medical and psychosocial), and health status; and (2) reduce future risk, defined as reduction in mortality, exacerbations (including hospitalisations), reduced treatment side-effects, and reduced disease progression. This is shown in Figure 3. Pharmacological therapy
GOLD 2011 goals of treatment for stable COPD. From the Global Strategy for Diagnosis, Management, and Prevention of COPD, revised 2011.2 Used with permission from the Global Initiative for Chronic Obstructive Lung Disease (GOLD), www.goldcopd.org
Pharmacological therapy
In line with the new proposed system of assessment, pharmacological management of stable COPD is based on the four patient groups identified by this assessment (Table 2). The details of this algorithm are beyond the scope of this paper. The pharmacotherapy for COPD is discussed in more detail by Jones and Østrem in a previous issue of this journal,10 but several points are noteworthy:
-
(1) Although the algorithm is intuitively correct, the evidence base for the recommendations is not strong, especially in the lower risk groups where the evidence tends to come from subgroup/post hoc analysis of large randomised controlled trials such as TORCH11 and UPLIFT.12 In addition, the entry criteria for these studies tend to be based on severity of airflow limitation (± a certain exacerbation or symptom level). There is a need to devise clinical trials of COPD therapy based on the new patient group criteria in order to base firmer treatment recommendations.
-
(2) The guidelines no longer recommend use of inhaled corticosteroids (ICS) unless they are in combination with a long-acting inhaled β2-agonist (LABA). They recommend that LABA/ICS combinations should initially be used in patients with more severe airflow limitation (FEV1 <50% predicted) and/or a history of frequent exacerbations. This compares with the NICE recommendations (FEV1 <50% predicted with symptoms/ exacerbations) and the ACP/ACCP/ATS/ERS recommendations (FEV1 <60% predicted with symptoms).5
-
(3) The phosphodiesterase-4 inhibitor roflumilast may be useful to reduce exacerbations for patients with FEV1 <50% predicted, chronic bronchitis, and frequent exacerbations.
Non-pharmacological therapy
The importance of identification of and reducing exposure to risk factors is emphasised. Smoking cessation is a key intervention, but reducing indoor and outdoor pollution is a major public health priority worldwide. Exercise promotion is recommended for all patents and pulmonary rehabilitation for patients with an mMRC score of 2 or 3 (MRC score of 3 or 4), but raises doubts about its efficacy in patients with mMRC score 4 (MRC score 5, housebound).
Co-morbidities
There is a new chapter in the guidelines reflecting the importance and treatment of co-morbidities in improving current control and reducing future risk.
The chapter highlights the co-morbidities of cardiovascular disease, anxiety and depression, osteoporosis, and lung cancer. The guidelines state: “In general the presence of co-morbidities should not alter COPD treatment and co-morbidities should be treated as if the patient did not have disease.” For example, someone with heart failure should still be treated with β-blockers in spite of having COPD and, similarly, the presence of heart failure should not alter disease-specific treatment for COPD. However, this advice may have to be tempered by individual circumstances (e.g. the choice of an antidepressant will be influenced by whether a patient with COPD is on an antimuscarinic agent).
Another major challenge for primary care is how patients with several long-term conditions (in this case with COPD as the ‘reference disease’) can be most efficiently managed in combination with the different specialist services.
Discussion
The fundamental change in the assessment of the patient with COPD is to be welcomed. The classification of disease severity by airflow limitation alone served little practical use in managing the individual patient, especially as airflow limitation has poor correlation with the impact of the disease upon the patient. The incorporation of primary care-friendly symptom/health status questionnaires (mMRC/CAT) into the assessment process is also a positive advance, as is the link of the assessment system to a pharmacotherapy strategy. However, the new guidelines have some omissions and raise some problems and challenges for primary care.
A major omission in the guidelines is guidance regarding the assessment and management of palliative care needs. In addition, whilst the co-morbidities of anxiety and depression are dealt with, the important co-morbidity of social need, for example — an important factor after hospital admission for acute COPD14 — is not.
Some of the challenges for primary care in implementing these guidelines are:
-
1
The pivotal role of spirometry in the diagnosis of COPD provides a major challenge to primary care in developed countries where the quality of spirometry is variable3 and in developing countries where there is limited access to relatively expensive diagnostic equipment.
-
2
One of the key elements of the new guidelines is the importance of recording exacerbation history. There has been little consensus on how to record this in practice. In many clinical studies the definition of a severe exacerbation has been an episode requiring oral steroids/antibiotics or hospitalisation.11–13 This is relatively easy to record during a routine COPD check-up, but the GOLD 2011 definition of an exacerbation as ‘an acute event characterised by a worsening of the patient's respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication’ may be more difficult to record accurately.
-
3
One of the important reasons for assessing disease severity is to enable primary care physicians to stratify routine COPD care in practice according to disease severity (e.g routinely to assess high-risk patients more frequently). The multidimensional primary care-friendly DOSE assessment tool15 can be used to assess future risk and its use in practice to case-manage high-risk patients may improve outcomes.16 The less primary care-friendly multidimensional BODE index17 is also a good prognostic indicator. The proposed GOLD 2011 assessment method has the potential to identify high-risk patients, which raises the question as to how these multidimensional assessment tools will fit in with the new system.
-
4
While the 2011 GOLD guidelines undoubtedly are a positive move to a more multidimensional approach to assessment and management of the patient with a clear pharmacotherapy, there is a need to develop a more primary care-focussed holistic assessment and treatment algorithm better suited to primary care, similar to that promoted by the UK NICE 2010 guidelines and by the Primary Care Respiratory Society UK (Figure 4).18
Conclusions
The 2011 GOLD guidelines offer a new system of assessment and treatment of patients with COPD according to current control (symptoms/health status) and future risk (exacerbation history and/or airflow limitation severity) and by taking co-morbidities into account. The system offers a novel way of selecting patients for inclusion in therapeutic clinical trials in stable COPD, but a stronger evidence base may be required to convince national guideline committees to follow the pharmacotherapy recommendations (especially in patients with milder disease). Further development is needed to make the guidelines suitable for implementation in primary care.
References
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management and prevention of chronic pulmonary disease, 2001. http://www.goldcopd.org/Guidelines/guidelines-resources.html.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management and prevention of chronic pulmonary disease, 2011. http://www.goldcopd.org/Guidelines/guidelines-resources.html.
Levy ML, Quanjer PH, Booker R, Cooper BG, Holmes S, Small IR . Diagnostic spirometry in primary care. Proposed standards for general practice compliant with American Thoracic Society and European Respiratory Society recommendations. Prim Care Respir J 2009;18(3):130–47. http://dx.doi.org/10.4104/pcrj.2009.00054
National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. London: National Clinical Guideline Centre, 2010. http://guidance.nice.org.uk/CG101 (accessed March 2012).
Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease: A Clinical Practice Guideline Update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med 2011;155:179–91.
Jones PW . Health status and the spiral of decline. COPD 2009;6:59–63. http://dx.doi.org/10.1080/15412550802587943
Holguin F, Folch E, Redd SC, Mannino DM . Co-morbidity and mortality in COPD related hospitalisations in the United States 1979 to 2001. Chest 2005;128:2005–11. http://dx.doi.org/10.1378/chest.128.4.2005
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363:1128–38. http://dx.doi.org/10.1056/NEJMoa0909883
The COPD Assessment Tool (CAT). www.catestonline.org (accessed March 2012)
Jones R, Østrem A . Optimising pharmacological maintenance treatment for COPD in primary care. Prim Care Respir J 2011;20(1):33–45. http://dx.doi.org/10.4104/pcrj.2010.00069
Calverley PW, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356(8):775–89. http://dx.doi.org/10.1056/NEJMoa063070
Tashkin DP, Celli B, Senn S, et al.; UPLIFT Study Investigators. A 4 year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008;359(15):1543–54. http://dx.doi.org/10.1056/NEJMoa0805800
Wedzicha JA, Calverley PM, Seemungal TA . The prevention of chronic obstructive disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med 2008;177(10):19–26.
Gruffydd-Jones K, Langley Johnson C, Dyer C, Badlan K, Ward S . What are the needs of patients following discharge from hospital after an acute exacerbation of chronic obstructive pulmonary disease (COPD)? Prim Care Respir J 2007;16(6):363–8. http://dx.doi.org/10.3132/pcrj.2007.00075
Jones RC, Donaldson GC, Chavannes NH, et al. Derivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE index. Am J Respir Crit Care Med 2009;180:1189–95. http://dx.doi.org/10.1164/rccm.200902-0271OC
Gruffydd-Jones K, Richman J, Jones RC, Wang X . A pilot study of case management of high risk COPD patients in a general practice. Family Pract 2010;5:494–8. http://dx.doi.org/10.1093/fampra/cmq045
Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnoea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004;350:1005–12. http://dx.doi.org/10.1056/NEJMoa021322
Primary Care Respiratory Society. Diagnosis and management of COPD in primary care. http://www.pcrs-uk.org/resources/copd_resources.php (accessed March 2012).
Acknowledgements
Funding None.
Handling editor Hilary Pinnock
Author information
Authors and Affiliations
Contributions
The manuscript is the sole work of the author.
Corresponding author
Ethics declarations
Competing interests
KGJ was a member of the NICE 2010 COPD Guidelines Committee and has spoken for and acted as a consultant for the following companies: Almirall, GlaxoSmithKline, AstraZeneca, Chiesi, Novartis, Mundi Pharma/Napp, Merck Sharpe & Dohme, Sandoz.
Rights and permissions
About this article
Cite this article
Gruffydd-Jones, K. GOLD guidelines 2011: what are the implications for primary care?. Prim Care Respir J 21, 437–441 (2012). https://doi.org/10.4104/pcrj.2012.00058
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2012.00058
This article is cited by
-
Four patients with a history of acute exacerbations of COPD: implementing the CHEST/Canadian Thoracic Society guidelines for preventing exacerbations
npj Primary Care Respiratory Medicine (2015)
-
DAMPs activating innate and adaptive immune responses in COPD
Mucosal Immunology (2014)