Abstract
Background:
To determine the effect of urologist and radiologist learning curves and changes in MRI-TRUS fusion platform during 9 years of NCI’s experience with multiparametric magnetic resonance imaging (mpMRI)/TRUS fusion biopsy.
Methods:
A prospectively maintained database of patients undergoing mpMRI followed by fusion biopsy (Fbx) and systematic biopsy (Sbx) from 2007 to 2016 was reviewed. The patients were stratified based on the timing of first biopsy. Cohort 1 (7/2007−12/2010) accounted for learning curve. Cohort 2 (1/2011–5/2013) and cohort 3 (5/2013–4/2016) included patients biopsied prior to and after debut of a new software platform, respectively. Clinically significant (CS) disease was defined as Gleason 7 (3+4) or higher. McNemar’s test compared cancer detection rates (CDRs) of Sbx and Fbx between time periods.
Results:
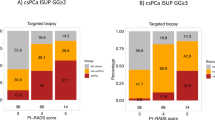
1528 patients were included in the study with 230, 537 and 761 patients included in three respective cohorts. Median age (interquartile range) was 61.0 (±9.0), 62.0 (±7.3), and 64.0 (±11.0) years in three cohorts, respectively (P<0.001). Fbx and Sbx had comparable CS CDR in cohort 1 (24.8 vs 22.2%, P=0.377). Fbx detected significantly more CS disease compared to Sbx in the following two periods (cohort 2: 31.5 vs 25.0%, P=0.001; cohort 3: 36.4 vs 30.3%, P<0.001) and detected significantly less low risk disease in the same period (cohort 2: 14.5 vs 19.6%, P<0.001; cohort 3: 12.6 vs 16.7%, P<0.001). Even after multivariate adjustment with age, PSA, race, clinical stage and MRI suspicion score, Fbx CS cancer detection increased in successive cohorts (cohort 2: OR 2.23, P=0.043; cohort 3: OR 2.92, P=0.007).
Conclusions:
In the past 9 years, there has been significant improvement in the accuracy of Fbx. Our results show that after an early learning period, Fbx detected higher rates of CS cancer and lower rates of clinically insignificant cancer than Sbx. Software advances allowed for even greater detection of CS disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lecornet E, Ahmed HU, Hu Y, Moore CM, Nevoux P, Barratt D et al. The accuracy of different biopsy strategies for the detection of clinically important prostate cancer: a computer simulation. J Urol 2012; 188: 974–980.
Kvale R, Moller B, Wahlqvist R, Fossa SD, Berner A, Busch C et al. Concordance between Gleason scores of needle biopsies and radical prostatectomy specimens: a population-based study. BJU Int 2009; 103: 1647–1654.
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015; 313: 390–397.
Moore CM, Robertson NL, Arsanious N, Middleton T, Villers A, Klotz L et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol 2013; 63: 125–140.
Kuru TH, Roethke MC, Seidenader J, Simpfendorfer T, Boxler S, Alammar K et al. Critical evaluation of magnetic resonance imaging targeted, transrectal ultrasound guided transperineal fusion biopsy for detection of prostate cancer. J Urol 2013; 190: 1380–1386.
Bjurlin MA, Mendhiratta N, Wysock JS, Taneja SS . Multiparametric MRI and targeted prostate biopsy: improvements in cancer detection, localization, and risk assessment. Central Eur J Urol 2016; 69: 9–18.
Harris RD, Schned AR, Heaney JA . Staging of prostate cancer with endorectal MR imaging: lessons from a learning curve. Radiographics 1995; 15: 813–829 discussion 829–832.
Rosenkrantz AB, Ayoola A, Hoffman D, Khasgiwala A, Prabhu V, Smereka P et al. The learning curve in prostate MRI interpretation: self-directed learning versus continual reader feedback. AJR Am J Roentgenol 2017; 208: W92–w100.
Rosenkrantz AB, Pujara AC, Taneja SS . Use of a quality improvement initiative to achieve consistent reporting of level of suspicion for tumor on multiparametric prostate MRI. AJR Am J Roentgenol 2016; 206: 1040–1044.
Emberton M . Has magnetic resonance-guided biopsy of the prostate become the standard of care? Eur Urol 2013; 64: 720–721.
Greer MD, Choyke PL, Turkbey B . PI-RADSv2: How we do it. J Magn Reson Imaging 2017; 46: 11–23.
Yerram NK, Volkin D, Turkbey B, Nix J, Hoang AN, Vourganti S et al. Low suspicion lesions on multiparametric magnetic resonance imaging predict for the absence of high-risk prostate cancer. BJU Int 2012; 110: E783–E788.
Barentsz JO, Richenberg J, Clements R, Choyke P, Verma S, Villeirs G et al. ESUR prostate MR guidelines 2012. Eur Radiol 2012; 22: 746–757.
Naing NN . Easy way to learn standardization: direct and indirect methods. Malays J Med Sci 2000; 7: 10–15.
Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT . Assessment of the learning curve in health technologies. A systematic review. Int J Technol Assess Health Care 2000; 16: 1095–1108.
Subramonian K, Muir G . The 'learning curve' in surgery: what is it, how do we measure it and can we influence it? BJU Int 2004; 93: 1173–1174.
Gold RH, Bassett LW, Widoff BE . Highlights from the history of mammography. Radiographics 1990; 10: 1111–1131.
Miglioretti DL, Gard CC, Carney PA, Onega TL, Buist DS, Sickles EA et al. When radiologists perform best: the learning curve in screening mammogram interpretation. Radiology 2009; 253: 632–640.
Volkin D, Turkbey B, Hoang AN, Rais-Bahrami S, Yerram N, Walton-Diaz A et al. Multiparametric magnetic resonance imaging (MRI) and subsequent MRI/ultrasonography fusion-guided biopsy increase the detection of anteriorly located prostate cancers. BJU Int 2014; 114: E43–E49.
Kongnyuy M, Sidana A, George AK, Muthigi A, Iyer A, Fascelli M et al. The significance of anterior prostate lesions on multiparametric magnetic resonance imaging in African-American men. Urol Oncol 2016; 34: e215–e221.
Gaziev G, Wadhwa K, Barrett T, Koo BC, Gallagher FA, Serrao E et al. Defining the learning curve for multiparametric magnetic resonance imaging (MRI) of the prostate using MRI-transrectal ultrasonography (TRUS) fusion-guided transperineal prostate biopsies as a validation tool. BJU Int 2016; 117: 80–86.
Buus S, Rylander S, Hokland S, Sondergaard CS, Pedersen EM, Tanderup K et al. Learning curve of MRI-based planning for high-dose-rate brachytherapy for prostate cancer. Brachytherapy 2016; 15: 426–434.
Ou YC, Yang CK, Chang KS, Wang J, Hung SW, Tung MC et al. The surgical learning curve for robotic-assisted laparoscopic radical prostatectomy: experience of a single surgeon with 500 cases in Taiwan, China. Asian J Androl 2014; 16: 728–734.
Atug F, Castle EP, Srivastav SK, Burgess SV, Thomas R, Davis R . Positive surgical margins in robotic-assisted radical prostatectomy: impact of learning curve on oncologic outcomes. Eur Urol 2006; 49: 866–871 discussion 871-862.
Ahlering TE, Eichel L, Edwards RA, Lee DI, Skarecky DW . Robotic radical prostatectomy: a technique to reduce pT2 positive margins. Urology 2004; 64: 1224–1228.
Zorn KC, Wille MA, Thong AE, Katz MH, Shikanov SA, Razmaria A et al. Continued improvement of perioperative, pathological and continence outcomes during 700 robot-assisted radical prostatectomies. Can J Urol 2009; 16: 4742–4749.
Patel VR, Palmer KJ, Coughlin G, Samavedi S . Robot-assisted laparoscopic radical prostatectomy: perioperative outcomes of 1500 cases. J Endourol 2008; 22: 2299–2305.
Vickers AJ, Bianco FJ, Serio AM, Eastham JA, Schrag D, Klein EA et al. The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst 2007; 99: 1171–1177.
Latchamsetty KC, Borden LS Jr, Porter CR, Lacrampe M, Vaughan M, Lin E et al. Experience improves staging accuracy of endorectal magnetic resonance imaging in prostate cancer: what is the learning curve? Can J Urol 2007; 14: 3429–3434.
Akin O, Riedl CC, Ishill NM, Moskowitz CS, Zhang J, Hricak H . Interactive dedicated training curriculum improves accuracy in the interpretation of MR imaging of prostate cancer. Eur Radiol 2010; 20: 995–1002.
Fleshner K, Carlsson SV, Roobol MJ . The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol 2017; 14: 26–37.
McGinley KF, McMahon GC, Brown GA . Impact of the US Preventive Services Task Force Grade D Recommendation: Assessment of Evaluations for elevated prostate-specific antigen and prostate biopsies in a large urology group practice following statement revision. Rev Urol 2015; 17: 171–177.
Banerji JS, Wolff EM, Massman JD 3rd, Odem-Davis K, Porter CR, Corman JM . Prostate needle biopsy outcomes in the era of the U.S. Preventive Services Task Force Recommendation against prostate specific antigen based screening. J Urol 2016; 195: 66–73.
Olsson C, Anderson A, Kapoor D . MP39-04 initial prostate cancer detection before and after United States Preventive Services Task Force Recommendation on prostate cancer screening. J Urol 195: e542.
Rosenberg M, Crawford D, Newmark J, Steiner M . MP39-01 use of PSA screening guidelines among primary care physicians. J Urol 195: e541.
Acknowledgements
This research was supported by the Intramural Research Program of the National Institutes of Health (NIH), National Cancer Institute, Center for Cancer Research, and the Center for Interventional Oncology. NIH and Philips Healthcare have a cooperative research and development agreement. NIH and Philips share intellectual property in the field. This research was also made possible through the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH by the Doris Duke Charitable Foundation (Grant #2014194), the American Association for Dental Research, the Colgate-Palmolive Company, Genentech, and other private donors. For a complete list, visit the foundation website at http://www.fnih.org.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Calio, B., Sidana, A., Sugano, D. et al. Changes in prostate cancer detection rate of MRI-TRUS fusion vs systematic biopsy over time: evidence of a learning curve. Prostate Cancer Prostatic Dis 20, 436–441 (2017). https://doi.org/10.1038/pcan.2017.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2017.34
This article is cited by
-
The learning curve for robotic-assisted transperineal MRI/US fusion-guided prostate biopsy
Scientific Reports (2024)
-
A prospective study on inter-operator variability in semi-robotic software-based MRI/TRUS-fusion targeted prostate biopsies
World Journal of Urology (2022)
-
Role of multiparametric prostate MRI in the management of prostate cancer
World Journal of Urology (2021)
-
Techniques and Outcomes of MRI-TRUS Fusion Prostate Biopsy
Current Urology Reports (2021)
-
Review article: MRI-targeted biopsies for prostate cancer diagnosis and management
World Journal of Urology (2021)