Abstract
Background:
We investigated the impact of skeletal-related events (SREs) on health-related quality of life (HRQoL) in patients with metastatic castration-resistant prostate cancer (mCRPC) in phase III trials of enzalutamide versus placebo.
Methods:
Patients with mCRPC experiencing at least one SRE during AFFIRM and PREVAIL were assessed for trajectory-adjusted mean change in HRQoL by first SRE using Functional Assessment of Cancer Therapy-Prostate (FACT-P; AFFIRM, three domains, and PREVAIL, nine domains) and EQ-5D (PREVAIL) instruments.
Results:
First SREs caused HRQoL deterioration in both trials. Spinal cord compression had the largest impact, with clinically meaningful reductions in seven of nine FACT-P domains in PREVAIL and all three in AFFIRM (mean (95% confidence interval (CI)) change in FACT-P total score –16.95 (–26.47, –7.44) and –9.69 (–16.10, –3.27), respectively). In PREVAIL, first SREs caused clinically meaningful declines in EQ-5D utility index, irrespective of category; spinal cord compression had the largest impact (mean (95% CI) change –0.24 (–0.39, –0.08)). In AFFIRM, FACT-P and FACT-General total scores showed clinically meaningful declines after radiation/surgery to bone.
Conclusions:
SREs were associated with clinically meaningful functional declines in the daily lives of patients with mCRPC. Spinal cord compression had the largest impact on HRQoL.
Similar content being viewed by others
Introduction
In metastatic castration-resistant prostate cancer (mCRPC), bone is the most frequent site of metastases.1 Skeletal metastases occur in 90% of CRPC patients and can result in significant morbidity,2 primarily through skeletal-related events (SREs).3 SREs include pathologic fracture, spinal cord compression, palliative radiation or surgery to bone and change in antineoplastic therapy secondary to bone pain.4, 5, 6 Additionally, SREs may cause reduced mobility, loss of independence and decreased health-related quality of life (HRQoL),7 and have been associated with increased mortality in bone mCRPC.8
In mCRPC patients with bone metastases, a key goal is to decrease the morbidity associated with SREs, preserving or improving HRQoL and functional independence.9 Delaying SREs is an important treatment goal and the subject of research in patients with mCRPC who initially do not have major cancer-related symptoms in the chemotherapy-naïve setting.10 Furthermore, delaying SRE onset is recognized by the US Food and Drug Administration as a clinically important indicator of preservation of functionality and HRQoL.11 It is also important to understand how SREs relate to patient-reported outcomes, as assessing HRQoL in CRPC assumes increasing importance in new treatment evaluation.12
Two recent phase III trials assessed the efficacy of the androgen receptor signaling inhibitor enzalutamide in mCRPC patients who were chemotherapy-naïve (PREVAIL) or had previously received chemotherapy (AFFIRM).5, 6 In addition to significant improvements in overall and progression-free survival, enzalutamide was associated with HRQoL benefits versus placebo and delayed first SRE occurrence.9, 13, 14 Indeed, enzalutamide was associated with a 28% reduction in risk in the time to first SRE versus placebo in PREVAIL (hazard ratio 0.72; 95% confidence interval (CI): 0.61, 0.84; P<0.001)5 and a 31% reduction in AFFIRM (hazard ratio 0.69; 95% CI: 0.57, 0.84; P<0.001).6
In our analysis, we characterize the clinical relevance of SREs in terms of their association with mCRPC patients’ trajectories of HRQoL and health-state preferences by assessing patient-reported outcome data from both PREVAIL and AFFIRM.
Materials and methods
Data from PREVAIL and AFFIRM were analyzed separately.
Study designs
SREs and HRQoL were assessed in the phase III, randomized, double-blind, placebo-controlled PREVAIL and AFFIRM trials comparing oral enzalutamide 160 mg per day versus placebo in patients with asymptomatic or mildly symptomatic chemotherapy-naïve mCRPC, despite androgen-deprivation therapy (PREVAIL) or mCRPC previously treated with one or two chemotherapy regimens (AFFIRM).
The designs (including choice of sample size, inclusion/exclusion criteria and randomization/blinding methods), patient populations and overall results of these trials have been described in detail elsewhere.5, 6
Both trials were approved by the independent review board at each study site and conducted according to the principles of the Declaration of Helsinki and Good Clinical Practice Guidelines. Patients provided written informed consent before study participation.
Procedures
In both studies, SRE was defined as radiotherapy or surgery to bone for prostate cancer, pathological bone fracture, spinal cord compression or change of antineoplastic therapy to treat prostate cancer-related bone pain. Change in analgesic medication for bone pain or initiation of bisphosphonates or denosumab were not considered to be SREs. However, we analyzed only the first three SRE categories: radiotherapy or surgery to bone for prostate cancer, pathological bone fracture and spinal cord compression. In PREVAIL, patients were assessed for SREs every 4 weeks to week 49 and every 12 weeks thereafter. This assessment was included to evaluate the time before occurrence of important clinical manifestations of disease progression. In AFFIRM, patients were followed for SREs every 12 weeks from week 13 until lost to follow-up, withdrawal of consent or death.
HRQoL was assessed using Functional Assessment of Cancer Therapy-Prostate (FACT-P) version 415, 16, 17 (both trials) and EQ-5D18 (PREVAIL only) instruments (see Methods in the Supplementary Information). Higher scores represent better health states.
In PREVAIL, nine FACT-P domains were assessed: FACT-P total score, FACT-General (FACT-G) score, FACT-Trial Outcome Index (TOI), FACT Advanced Prostate Symptom Index, physical wellbeing, functional wellbeing, emotional wellbeing, social/family wellbeing and prostate cancer subscale. Patients completed FACT-P at baseline, weeks 5 and 13, and then every 12 weeks until study drug discontinuation. EQ-5D data were collected at baseline and week 13, and then every 12 weeks until treatment discontinuation.
In AFFIRM, three FACT-P domains were assessed: FACT-P total score, FACT-G and prostate cancer subscale. Data were prospectively collected at baseline, weeks 13, 17, 21 and 25, and every 12 weeks thereafter until study drug discontinuation.
In both studies, HRQoL instruments were administered before patients were interviewed by their physicians or received study medication. ‘Post-SRE assessment’ was the first assessment made <100 days after an SRE occurred. Patients without an assessment during that interval were considered to have missing post-SRE assessments.
Statistical analyses
All analyses were performed on intention-to-treat populations (all patients randomized). The analysis was performed on the combined (enzalutamide and placebo) treatment arms; where the number of patients allowed, the impact of SREs on HRQoL was stratified by treatment. Only patients experiencing at least one SRE (AFFIRM, n=421; PREVAIL, n=587) were included in the analysis. Additionally, we included only patients with baseline and one or more post-SRE HRQoL outcome values. SREs were categorized as: (1) radiation or surgery to bone, (2) pathologic bone fractures and (3) spinal cord compression. For patients with multiple SREs, only the first SRE event category was used. If a patient experienced more than one type of SRE as the first SRE, he was included in the analysis of each SRE category. A separate analysis was performed for each SRE category.
To determine the immediate impact of an SRE (any category) on HRQoL outcomes, we included all outcome assessments up to the date of the SRE of interest and first post-SRE assessment. We used linear mixed-effect models with intercept as random effects to model each patient’s longitudinal trajectory of HRQoL outcome before the first SRE.19 How far the post-SRE value of HRQoL outcome deviated from the trajectory (predicted value) was estimated by calculating the trajectory-adjusted mean change (TAMC; mean deviation of the post-SRE value from the expected value) after the patient’s first SRE (see the Supplementary Information for further details of these analyses).
Standardized effect size was calculated by dividing TAMC by overall standard deviation at baseline. Following Cohen’s benchmarks,20, 21 effect sizes of 0.2, 0.5 and 0.8 were characterized as small, medium and large, respectively. TAMC results were interpreted using previously established minimal clinically important differences (MCIDs). The MCID was the smallest difference in a patient-reported outcome score interpreted as clinically important or meaningful to the patient; these have been defined for FACT-P (and its subscales), FACT-G and EQ-5D (Table 1). In our analyses, the lower end of the range indicated a clinically meaningful change. TAMCs were considered statistically significant if the 95% CI excluded zero.
Data were analyzed using SAS version 9.3 (SAS Institute, Cary, NC, USA). Adjustments for multiple comparisons were not made because these were exploratory analyses.
Results
SRE data for combined treatment arms
PREVAIL
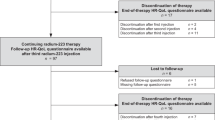
In PREVAIL, 1717 patients were randomized to enzalutamide (n=872) or placebo (n=845). Overall, 587 patients (34.2%) experienced at least one SRE; 426 patients (24.8%) experienced one SRE, 109 (6.4%) experienced two SREs and 52 (3.0%) experienced three or more SREs. Radiation or surgery to bone was the most common first SRE (in 410 patients (23.9%); that is, 70% of patients who had at least one SRE) (Figure 1).
Table 2 shows baseline demographic and disease characteristics of patients experiencing at least one SRE during AFFIRM and PREVAIL. Baseline pain (Brief Pain Inventory question 3, worst pain in previous 24 h) was 0–1 (asymptomatic) in ≈59% of patients and 2–3 (mildly symptomatic) in 39%. Approximately one-quarter of patients who experienced SREs had received bisphosphonate treatment at baseline (Supplementary Table S1). Table 1 shows baseline HRQoL scores of patients included in the analysis.
In PREVAIL, first SREs caused declines in EQ-5D utility index (TAMC) that were statistically significant (95% CI excludes zero) and clinically meaningful (exceeded lower limit of MCID range; Table 1), irrespective of SRE category (Table 3). Spinal cord compression had the largest impact on utility index (mean (95% CI)) decrease –0.24 (–0.39, –0.08)).
Spinal cord compression had the broadest impact on FACT-P, significantly diminishing HRQoL in seven of nine domains (not social/family wellbeing or emotional wellbeing) to a clinically meaningful extent, inducing a mean (95% CI) decrease in FACT-P total score of –16.95 (–26.47, –7.44) points. Radiation or surgery to bone was associated with statistically significant declines in physical wellbeing, functional wellbeing and FACT-TOI and an increase in social/family wellbeing, although none were clinically meaningful. Pathologic bone fractures showed no statistically significant changes in any FACT-P outcome.
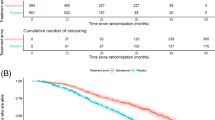
Effect size was small to medium for radiation or surgery to bone and pathologic fractures, ranging from –0.24 to –0.52 (Figure 2a). In all outcome categories, spinal cord compression had the greatest effect size and was the only SRE with effect sizes that could be characterized as large.
Impact of SREs on HRQoL outcomes scores by SRE category in (a) PREVAIL and (b) AFFIRM. EWB, emotional wellbeing; FACT-G, Functional Assessment of Cancer Therapy-General; FACT-P, Functional Assessment of Cancer Therapy-Prostate; FAPSI, Functional Assessment of Cancer Therapy Advanced Prostate Symptom Index; FWB, functional wellbeing; HRQoL, health-related quality of life; PCS, prostate cancer subscale; PWB, physical wellbeing; SRE, skeletal-related event; SWB, social wellbeing; TOI, Trial Outcome Index.
AFFIRM
In AFFIRM, 1199 patients were randomized to enzalutamide (n=800) or placebo (n=399). Overall, 421 patients (35.1%) experienced at least one SRE; 408 (34.0%) experienced one SRE, 12 (1.0%) experienced two SREs and only one patient (0.1%) experienced three or more SREs.
Distribution by first SRE type is shown in Figure 1. Radiation or surgery to bone was the most common SRE (in 291 patients (24.3%); that is, 69.1% of patients who had more than one SRE), and pathologic bone fracture the least common (in 47 patients (3.9%)).
Baseline pain (Brief Pain Inventory question 3, worst pain in previous 24 h) was 2–3 (mildly symptomatic) in approximately 39% of patients and >3 (severely symptomatic) in 37% (Table 2). Approximately half of patients who experienced SREs had received bisphosphonate treatment at baseline (Supplementary Table S1). Table 1 shows baseline HRQoL scores.
In AFFIRM, there were clinically meaningful and statistically significant declines in FACT-P and FACT-G total scores after any SRE, radiation or surgery to bone or spinal cord compression. For FACT-P prostate cancer subscale score, statistically significant declines were observed for any SRE, radiation or surgery to bone and spinal cord compression, but this was clinically meaningful only for spinal cord compression (Table 4). Pathologic bone fractures were associated with declines in all three HRQoL measures, but none were statistically significant.
Spinal cord compression had the largest impact on FACT-P total score (mean (95% CI) decrease –9.69 (–16.10, –3.27); Table 4). Pathologic bone fractures and radiation or surgery to bone determined mean (95% CI) changes in FACT-P total score of –7.62 (–16.80, 1.56; not significant) and –6.69 (–10.26, –3.12) points, respectively. Effect sizes on HRQoL outcomes were small or medium in all cases, ranging from –0.17 to –0.49. In all three HRQoL outcome categories, spinal cord compression showed the largest effect size (Figure 2b).
SRE data stratified by treatment arm
For any SRE and radiation or surgery to bone categories, TAMCs in HRQoL outcomes in PREVAIL and AFFIRM were stratified by treatment arm (Supplementary Tables S2 and S3).
For enzalutamide-treated patients in PREVAIL, there were clinically meaningful and statistically significant declines in four FACT-P domains (functional wellbeing, prostate cancer subscale, FACT-P total score and FACT-TOI) after any SRE. In contrast, there were no statistically significant declines in FACT-P outcomes after any SRE for patients receiving placebo, except for physical wellbeing, and none were clinically meaningful. There were also substantive declines in EQ-5D utility index in both enzalutamide and placebo groups after any SRE.
For radiation or surgery to bone, enzalutamide-treated patients had statistically significant declines in FACT-P physical wellbeing, functional wellbeing and FACT-TOI domains and an increase in social/family wellbeing. None of these were clinically meaningful. With placebo, there were statistically significant declines in physical wellbeing and FACT-TOI and a significant increase in social/family wellbeing, but none were clinically meaningful.
In AFFIRM, in both the any SRE and radiation or surgery to bone categories, enzalutamide was associated with a statistically significant and clinically meaningful decline in FACT-P total, prostate cancer subscale and FACT-G total scores. There were no significant changes with placebo.
Discussion
Our findings show an association between SREs and significant functional decline in patients’ daily lives, and HRQoL in general, in patients with mCRPC. In PREVAIL and AFFIRM, similar proportions (just over one-third) of patients developed SREs, most commonly radiation or surgery to bone (≈70%).
Associations between SREs and HRQoL outcomes in both trials was greatest for spinal cord compression, with statistically and clinically meaningful reductions in most FACT-P domains assessed. Spinal cord compression also induced the largest reductions in FACT-P total score in both trials and had the largest impact on EQ-5D utility index in PREVAIL. Furthermore, spinal cord compression had the largest effect size on all FACT-P domains in both studies. Although expected, this helps calibrate, to some extent, our measurement of the effects of the other SREs. The impact of spinal cord compression on HRQoL measures was also larger in chemotherapy-naïve mCRPC patients in PREVAIL than in those previously treated with docetaxel in AFFIRM. The greater impact of spinal cord compression (versus other SREs) on HRQoL reflects its debilitating symptoms, which range from minor sensory, motor and autonomic changes to severe pain and complete paralysis.25 Thus, more than 90% of such patients have pain26 with other common signs, including radiculopathy, weakness, sensory changes (e.g., paresthesia, loss of sensation), incontinence and autonomic dysfunction (e.g., urinary hesitancy, retention).27 Moreover, metastatic spinal cord compression is an acute condition requiring emergency care to prevent loss of neurological function and reverse established deficits.28
The more pronounced effect of spinal cord compression on HRQoL likely reflects not only its magnitude of effect on HRQoL but also the timing of HRQoL measurement. As HRQoL data is only measured every 12 weeks, SREs may occur up to 3 months beforehand. Thus, for example, patients undergoing radiotherapy for pain may experience some resolution of symptoms and some level of recovery and relief before their next HRQoL assessment. Also, for example, in the case of a moderate fracture, many of its effects also may have resolved when HRQoL is next measured. In contrast, spinal cord compression has a longer duration of impact and sequelae are often still present when patients undergo HRQoL assessment.
Radiation or surgery to bone was associated with statistically significant and clinically meaningful declines in FACT-P and FACT-G total scores in AFFIRM; however, in PREVAIL, none of the changes in FACT-P outcomes were clinically meaningful, although several showed statistically significant changes. These results are consistent with a previous study in advanced prostate cancer, where radiation to bone was associated with statistically significant declines in four of five FACT-G domains and a statistically significant reduction in EQ-5D utility index and EQ visual analog scale scores.29 However, although radiotherapy has the potential for beneficial effects such as alleviating bone pain, it can be associated with pervasive negative effects on HRQoL such as adverse events and the negative psychological effect of a patient realizing that the cancer is sufficiently severe to require radiotherapy and repeated hospital visits for treatment.29
Pathologic bone fractures were not associated with statistically significant changes in any FACT-P outcomes in either study, although in PREVAIL they were associated with significant declines in EQ-5D utility index. In AFFIRM, although changes in FACT-P/FACT-G outcomes associated with pathologic bone fractures were not statistically significant, they were clinically significant; the lack of statistical significance perhaps reflects the small sample size. This contrasts with the study by Weinfurt et al.29 where pathologic fractures were associated with significant declines in two of five FACT-G domains and in EQ visual analog scale and EQ-5D utility index in patients with metastatic prostate cancer (some of whom were receiving antineoplastic therapy). Pathologic fractures can seriously affect HRQoL of cancer patients30 and have been correlated with reduced survival in malignant bone disease.31 It may be that, in the context of the effect sizes associated with this variable, the small sample size caused the 95% CIs to include zero in this subgroup and precluded detection of statistical significance. Furthermore, pathologic fractures vary considerably in severity; it may be that the fractures in our analysis were not particularly severe.
We also looked for between-treatment differences in the effect of SREs on HRQoL. For some variables, such as pathologic fracture and spinal cord compression, low patient numbers precluded reliable analysis by treatment group. Thus, we confined our analysis to outcomes with sufficient patient numbers (any SRE and radiation or surgery to bone). In general, changes were largely concordant between treatments. Over both trials, enzalutamide was associated with clinically meaningful and statistically significant declines in several FACT-P domains after any SRE. For radiation or surgery to bone, there were clinically meaningful declines in FACT-P domains with enzalutamide in AFFIRM but not PREVAIL. In contrast, there were no clinically meaningful declines in FACT-P domains with placebo in either trial after any SRE or after radiation or surgery to bone. Note that the small sample size of the placebo arm in both trials likely caused the 95% CIs to include zero.
Bisphosphonates were used by approximately 25 and 52% of patients with at least one SRE in PREVAIL and AFFIRM, respectively. However, it has been reported previously that the benefit of enzalutamide on reducing the risk of first SRE versus placebo occurred regardless of bisphosphonate (or bisphosphonate or denosumab in PREVAIL) use.10, 13
Recent analyses from both AFFIRM and PREVAIL showed that median time to first SRE was significantly longer with enzalutamide than placebo (P⩽0.0001), and time to HRQoL deterioration was also delayed.10, 13 In mCRPC, delaying or preventing SREs is an important treatment goal10, 32, 33 and reflects preservation of HRQoL and functionality.11 Our analysis provides quantitative data linking the most commonly observed adverse consequence of advanced metastatic prostate cancer—complications from skeletal involvement—with quantitative HRQoL measures.
Some limitations of our analyses should be considered. A higher proportion of enzalutamide patients were available for HRQoL assessment in both trials because of disease progression occurring earlier with placebo, at which time HRQoL data collection ceased. Absence of HRQoL data after disease progression is a recognized drawback of trials using HRQoL as a secondary end point. Additionally, our SRE categories did not include ‘change of antineoplastic therapy to treat prostate cancer-related bone pain’; however, few patients had SREs in this additional category (AFFIRM, 3–4%; PREVAIL, 6–9%) (Astellas data on file, 2014).13 Finally, the study design may have led us to underestimate changes in HRQoL outcomes caused by SREs. The recall period of FACT-P is 7 days, but we collected HRQoL data every 12 weeks; therefore, a patient experiencing a moderate fracture may not have had an HRQoL assessment until 2–3 months after the event, by which time many of the fracture’s effects may have resolved.
In conclusion, our analyses show an association between SREs and clinically meaningful functional declines in the daily lives of patients with mCRPC. As expected, spinal cord compression had the largest impact on HRQoL. Moreover, the impact was larger in chemotherapy-naïve mCRPC patients. Treatments that reduce or delay emergence of SREs may slow HRQoL decline in mCRPC. In AFFIRM and PREVAIL, both time to first SRE and time to HRQoL deterioration were delayed with enzalutamide versus placebo.
References
Butoescu V, Tombal B . Practical guide to bone health in the spectrum of advanced prostate cancer. Can J Urol 2014; 21 (Suppl 1): 84–92.
Hotte SJ, Saad F . Current management of castrate-resistant prostate cancer. Curr Oncol 2010; 17 (Suppl 2): S72–S79.
Brown JE, Sim S . Evolving role of bone biomarkers in castration-resistant prostate cancer. Neoplasia 2010; 12: 685–696.
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L et alZoledronic Acid Prostate Cancer Study Group. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst 2004; 96: 879–882.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS et alPREVAIL Investigators.. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 2014; 371: 424–433.
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K et al, AFFIRM investigators. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 2012; 367: 1187–1197.
Ayala-Ramirez M, Palmer JL, Hofmann MC, de la Cruz M, Moon BS, Waguespack SG et al. Bone metastases and skeletal-related events in patients with malignant pheochromocytoma and sympathetic paraganglioma. J Clin Endocrinol Metab 2013; 98: 1492–1497.
Howard LE, De Hoedt AM, Aronson WJ, Kane CJ, Amling CL, Cooperberg MR et al. Do skeletal-related events predict overall survival in men with metastatic castration-resistant prostate cancer? Prostate Cancer Prostatic Dis 2016; 19: 380–384.
Cathomas R, Bajory Z, Bouzid M, El Ghoneimy A, Gillessen S, Goncalves F et al. Management of bone metastases in patients with castration-resistant prostate cancer. Urol Int 2014; 92: 377–386.
Loriot Y, Miller K, Sternberg CN, Fizazi K, De Bono JS, Chowdhury S et al. Effect of enzalutamide on health-related quality of life, pain, and skeletal-related events in asymptomatic and minimally symptomatic, chemotherapy-naive patients with metastatic castration-resistant prostate cancer (PREVAIL): results from a randomised, phase 3 trial. Lancet Oncol 2015; 16: 509–521.
Autio KA, Scher HI, Morris MJ . Therapeutic strategies for bone metastases and their clinical sequelae in prostate cancer. Curr Treat Options Oncol 2012; 13: 174–188.
Moul JW, Dawson N . Quality of life associated with treatment of castration-resistant prostate cancer: a review of the literature. Cancer Invest 2012; 30: 1–12.
Fizazi K, Scher HI, Miller K, Basch E, Sternberg CN, Cella D et al. Effect of enzalutamide on time to first skeletal-related event, pain, and quality of life in men with castration-resistant prostate cancer: results from the randomised, phase 3 AFFIRM trial. Lancet Oncol 2014; 15: 1147–1156.
Cella D, Ivanescu C, Holmstrom S, Bui CN, Spalding J, Fizazi K . Impact of enzalutamide on quality of life in men with metastatic castration-resistant prostate cancer after chemotherapy: additional analyses from the AFFIRM randomized clinical trial. Ann Oncol 2015; 26: 179–185.
Esper P, Mo F, Chodak G, Sinner M, Cella D, Pienta KJ . Measuring quality of life in men with prostate cancer using the Functional Assessment of Cancer Therapy-Prostate instrument. Urology 1997; 50: 920–928.
Cella D, Nichol MB, Eton D, Nelson JB, Mulani P . Estimating clinically meaningful changes for the Functional Assessment of Cancer Therapy-Prostate: results from a clinical trial of patients with metastatic hormone-refractory prostate cancer. Value Health 2009; 12: 124–129.
Victorson DE, Beaumont JL, Rosenbloom SK, Shevrin D, Cella D . Efficient assessment of the most important symptoms in advanced prostate cancer: the NCCN/FACT-P symptom index. Psychooncology 2011; 20: 977–983.
Rabin R, de Charro F . EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001; 33: 337–343.
Verbeke G, Molenberghs G . Linear Mixed Models for Longitudinal Data. Springer: New York, NY, USA, 2000.
Cohen J . Statistical Power Analysis for the Behavioural Sciences, 2nd edn. Lawrence Erlbaum: New York, NY, USA, 1988.
Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D . Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics 1999; 15: 141–155.
Cella D, Hahn EA, Dineen K . Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res 2002; 11: 207–221.
Yost KJ, Eton DT . Combining distribution- and anchor-based approaches to determine minimally important differences: the FACIT experience. Eval Health Prof 2005; 28: 172–191.
Pickard AS, Neary MP, Cella D . Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual Life Outcomes 2007; 5: 70.
Flounders JA, Ott BB . Oncology emergency modules: spinal cord compression. Oncol Nurs Forum 2003; 30: E17–E23.
Cancer Research UK What Spinal Cord Compression Is. Available at: http://www.cancerresearchuk.org/about-cancer/coping-with-cancer/coping-physically/spinal/what-spinal-cord-compression-is (last accessed August 2016).
Abrahm JL, Banffy MB, Harris MB . Spinal cord compression in patients with advanced metastatic cancer: ‘all I care about is walking and living my life’. JAMA 2008; 299: 937–946.
Sutcliffe P, Connock M, Shyangdan D, Court R, Kandala NB, Clarke A . A systematic review of evidence on malignant spinal metastases: natural history and technologies for identifying patients at high risk of vertebral fracture and spinal cord compression. Health Technol Assess 2013; 17: 1–274.
Weinfurt KP, Li Y, Castel LD, Saad F, Timbie JW, Glendenning GA et al. The significance of skeletal-related events for the health-related quality of life of patients with metastatic prostate cancer. Ann Oncol 2005; 16: 579–584.
Piccioli A, Rossi B, Scaramuzzo L, Spinelli MS, Yang Z, Maccauro G . Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014; 45: 412–417.
Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R . Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer 2007; 110: 1860–1867.
Sieber P . Emerging therapeutic for the treatment of skeletal-related events associated with metastatic castrate-resistant prostate cancer. Rev Urol 2014; 16: 10–20.
Merseburger AS, Haas GP, von Klot CA . An update on enzalutamide in the treatment of prostate cancer. Ther Adv Urol 2015; 7: 9–21.
Acknowledgements
This study was funded by Astellas Pharma and Medivation, the codevelopers of enzalutamide; Medivation was acquired by Pfizer in September 2016. Medical writing assistance was provided by Thomas Lavelle of Bioscript Science and editorial assistance was provided by Shannon Davis of Ashfield Healthcare Communications, both funded by the study sponsors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
FS received grants for research, honoraria (speaker and consultant) and serves on the advisory boards of Astellas, Medivation and Janssen. DP and SH and are employees of Astellas Pharma. SA is an employee of Medivation. TMB received grants for research funding from Astellas Pharma, Janssen Research and Development and Medivation, personal (consultancy) fees from Astellas Pharma and Janssen Japan and payment from Research to Practice for participation in a Certified Nursing Education program, which was supported, in part, by Medivation and Astellas Pharma. BT received grants, personal fees and nonfinancial support from Astellas and personal fees from Medivation. YL received personal fees from Astellas (advisory board, speaker, honoraria and travel) and from Medivation (advisory board, speaker). CI is an employee of Quintiles, which received funding from Astellas to conduct the analyses reported here.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Saad, F., Ivanescu, C., Phung, D. et al. Skeletal-related events significantly impact health-related quality of life in metastatic castration-resistant prostate cancer: data from PREVAIL and AFFIRM trials. Prostate Cancer Prostatic Dis 20, 110–116 (2017). https://doi.org/10.1038/pcan.2016.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.62
This article is cited by
-
Validation of Algorithms to Identify Bone Metastases Using Administrative Claims Data in a Japanese Hospital
Drugs - Real World Outcomes (2023)
-
Integrated analysis of pain, health-related quality of life, and analgesic use in patients with metastatic castration-resistant prostate cancer treated with Radium-223
Prostate Cancer and Prostatic Diseases (2022)
-
Bone Health in Men with Prostate Cancer: Review Article
Current Osteoporosis Reports (2019)
-
Decreased sensory nerve excitation and bone pain associated with mouse Lewis lung cancer in TRPV1-deficient mice
Journal of Bone and Mineral Metabolism (2018)
-
Enzalutamide: A Review in Castration-Resistant Prostate Cancer
Drugs (2018)