Abstract
Objectives:
This study aimed to examine the association of adipocyte fatty acid-binding protein (FABP4) levels with left ventricular diastolic dysfunction (LVDD) in obese subjects with varying degrees of the metabolic syndrome (MetS).
Methods:
Fifty morbidly obese subjects with LVDD were selected at random and matched by age (±5 years) and sex with 50 morbidly obese with normal left ventricular (LV) function. In addition, 24 healthy lean subjects were included as controls.
Results:
Median FABP4 levels (interquartile range) in obese subjects with LVDD were significantly higher (42 ng ml−1 (32–53)) than in obese with normal LV function (24 ng ml−1 (36–43), P=0.036), and in normal weight controls (13 ng ml−1 (10–20), P<0.0001). Increasing FABP4 tertiles were significantly associated with parameters of LVDD, the number of LVDD components, physical performance and epicardial fat thickness. In multivariate regression analysis adjusting for age, sex and adiposity, FABP4 levels remained significantly associated with parameters of diastolic function. The association of FABP4 levels with LVDD was mainly observed in subjects with metabolic complications, but not in metabolically healthy obese.
Conclusions:
FABP4 levels are significantly associated with LVDD in obese subjects, when the MetS is present. Thus, FABP4 may be a link between obesity and cardiometabolic disorders.
Similar content being viewed by others
Introduction
Adipocyte fatty acid-binding protein (FABP4, also termed ‘A-FABP’) is a member of the cytosolic fatty acid-binding protein family and is highly expressed in adipose tissue by means of adipocytes and macrophages.1, 2 The biological function of FABP4 is the binding and trafficking of fatty acids from cell membranes to intracellular targets.3 Recent studies support a novel role of FABP4 independent of its function as a carrier protein.4 Several animal-based and clinical studies have demonstrated that FABP4 has an important role in obesity-related insulin resistance, inflammation and atherosclerosis, suggesting FABP4 as a potential link between obesity and cardiometabolic diseases.5, 6, 7, 8, 9 In experimental animal models, FABP4 deficiency protects against the development of diabetes and atherosclerosis in both genetic and dietary forms of obesity.5, 10 Furthermore, humans with a functional genetic variant of the FABP4 gene, resulting in reduced adipose tissue expression of FABP4, have a significantly reduced risk for type 2 diabetes and coronary artery disease.6
FABP4 has also been shown to directly suppress cardiomyocyte contraction in vitro,11 suggesting a pathogenetic role of FABP4 in heart dysfunction. In accordance with these in vitro data, serum concentrations of FABP4 are elevated in heart failure (HF) patients and are associated with the incidence and severity of HF.12, 13 Moreover, FABP4 serum levels are associated with the parameters of left ventricular remodeling and function in healthy obese women.14, 15, 16, 17
These data imply that FABP4 may have a causal role in the pathogenesis of HF, particularly in obese subjects with metabolic alterations.
Left ventricular diastolic dysfunction (LVDD) has been described as an early sign of obese and diabetic cardiomyopathy preceding the systolic damage. Indeed, LVDD is a well-recognized consequence of obesity that can progressively lead to HF, and is linked to increased mortality.14, 15, 16 Interestingly, our previous data have shown direct depressive effects from human adipocytes factors on both contraction and relaxation rates in isolated perfused rat hearts.18 These in vitro functional changes are similar to those observed in the obese subjects.
Although there is evidence about the association of FABP4 serum levels with the incidence and prevalence of HF, FABP4 levels have not been correlated to parameters of LVDD so far. Thus, in the present study, we hypothesized that serum FABP4 is a novel marker for LVDD in morbidly obese subjects with varying degrees of metabolic syndrome (MetS).
Subjects and methods
Study population
Subjects were participants of the ‘Obesity weight reduction and remodeling study’, a prospective longitudinal study evaluating excessive body fat for its pathogenic potential in terms of cardiometabolic diseases and assessing the effects of considerable weight reduction on the interactions in systems biology.
Obese patients intending to participate in a weight reduction program were offered enrollment in our research study before the start of the program. Patients were eligible for enrollment if they were 18–65 years old, with a body mass index (BMI) >30 kg m−2 and a constant body weight in the last 3 months, and if they signed the declaration of consent. Exclusion criteria were described elsewhere.19, 20 Healthy normal weight control subjects (BMI 20–24.9 kg m−2) of similar age and gender distribution were also included. They were recruited by flyers and advertisements. MetS was defined according to the NCEP ATPIII criteria: abdominal obesity (waist circumference ⩾102 cm for men, ⩾88 cm for women), raised triglycerides (⩾150 mg dl−1), reduced HDL cholesterol (<40 mg dl−1 for men, ⩽50 mg dl−1 for women), elevated blood pressure (⩾130/⩾85 mm Hg) and impaired fasting glucose (⩾110 mg dl−1).21 The study was approved by the local Ethics Committee.
For the present study, 50 morbidly obese subjects with LVDD were selected at random and matched by age (±5 years) and sex with 50 morbidly obese subjects with normal left ventricular (LV) function. From the latter, four subjects were excluded due to incomplete data. In addition, 24 healthy normal weight control subjects served as controls.
Echocardiography
Echocardiography was performed using a standard ultrasound system (Philips iE33, Philips Medical Systems, Hamburg, Germany). LV ejection fraction (EF) was measured on the basis of the modified biplane Simpson’s method. The following parameters were measured according to previous ASE guidelines:22 parasternal long-axis diameter and apical four-chamber area. Measurements were done just before mitral valve opening. LV mass index was calculated by the Devereux formula indexed to the body surface area. Conventional transmitral flow was measured with pw-Doppler. Early (E), late atrial (A) transmitral peak flow velocities, their ratio (E/A) and deceleration time (DT) of the early transmitral flow velocity were measured and three consecutive beats were averaged. Pulsed-wave tissue Doppler imaging was performed at the junction of the lateral mitral annulus and three consecutive beats were averaged. Early diastolic velocities (e′ lateral) were recorded. Ratios of E/e′ lateral were calculated. Moreover, we determined the isovolumetric relaxation time, the difference between measured duration of reversed pulmonary vein atrial systole flow (Ard) and duration of mitral A wave flow (Ad), as well as the ratio of pulmonary vein systolic (S) and diastolic (D) flow velocities by pw-Doppler measurements.23
We measured the agreement between E/e′ measurements of two expert cardiologists in obese study participants by the use of the concordance correlation coefficient (CCC). The CCC combines a measure for precision and a measure for accuracy to evaluate reproducibility and inter-rater reliability.24 The CCC for 20 duplicate E/e′ measurements of the two expert sonographers was 0.976±0.014 (P<0.0001).
Definition of diastolic dysfunction
Diastolic dysfunction was defined as fulfilment of the following criteria: (1) a preserved systolic LV function (EF>50%) and (2) presence of at least two of the following criteria consistent with abnormal LV relaxation, filling, diastolic distensibility or diastolic stiffness:23 E/e′ lat.>8, E/A<0.8 and DT>200 ms−1 or E/A>2 and DT<160 ms−1, e′ lat.<10 cm s−1, e′/a′<0.9, S<D in pulmonary venous flow, Ard-Ad>0 ms−1, LV mass>149 g m−2 (in men), >122 g m−2 (in women) or an enlarged left atrial (LA) size (LA area (4 CH planimetry)) >20 cm2 or LA diameter (PLAX) >48 mm). In contrast, subjects with a normal lateral e′ ⩾10 cm s−1 together with a normal LA size were classified as having normal LV function according to ASE 2009 consensus criteria.22
Anthropometric and metabolic evaluation
Body composition was determined by bioelectrical impedance analysis using Nutriguard-Impedance analysis apparatus (Data Input GmbH, Darmstadt, Germany). Body weight, height, waist and hip circumference, and blood pressure were measured in a standardized manner.
Serum samples were collected after a 12 h overnight fast and immediately stored at −70 °C. The samples had not been thawed before the present measurements. FABP4 concentrations were determined by enzyme immunometric assay (EIA, Cayman Chemical, Ann Arbor, MI, USA) with an intra-assay coefficient of variation of 3.9% and an inter-assay coefficient of variation of 5.1%. The GDF-15 concentrations were determined by enzyme-linked immunosorbent assay (Quantikine, R&D Systems Europe, Wiesbaden, Germany). The NT-proBNP levels were determined by a standard chemiluminescence immunoassay (Roche Diagnostics, Mannheim, Germany). Fasting glucose, insulin, blood lipids and high-sensitivity C-reactive protein were determined by standard methods in the certified clinical chemistry laboratory of the University Hospital. Insulin resistance was estimated by homeostasis model assessment index (HOMA-IR) by the formula: (fasting insulin (μU ml−1) × fasting glucose (mmol l−1)/22.5).
6 min-walk test
Patients were instructed to walk from end to end in an enclosed corridor, covering as much ground as they could during 6 min. The distance walked was read using an electronic meter counter, and the maximum heart rate was immediately measured.
Statistical analysis
Categorical variables were compared using the Fisher’s exact test. Continuous variables were compared using one-way analysis of variance for normally distributed variables (if significant, the Student’s t-test for the comparison of two groups or the Tukey–Kramer post hoc test for multiple pairwise comparisons were used). For non-normally distributed variables we used the Kruskal–Wallis test, and the Dwass–Steel post hoc test was used to make all possible pairwise comparisons, accounting for multiple testing. Association between echocardiographic parameters and tertiles of FABP4 levels were analyzed with one-way analysis of variance. Statistical significance was considered at the 0.05 level. All analyses were conducted using JMP Version 9 (SAS Institute Inc., Cary, NC, USA) and STATA 8 (Statacorp., College Station, TX, USA).
Results
The clinical characteristics of obese subjects with LVDD and with normal LV function and lean controls are displayed in (Table 1). Subjects with LVDD were significantly more obese and had a higher systolic blood pressure than obese subjects with normal LV function. Nevertheless, metabolic parameters such as fasting glucose, insulin and HOMA-IR levels, as well as blood lipids, inflammatory markers and adipokines were comparable in obese subjects with and without LVDD.
The corresponding echocardiographic characteristics are shown in (Table 2). By definition, obese subjects with LVDD presented with higher features of LV hypertrophy such as septal thickness, relative wall thickness, LV mass and left atrial size, as well as higher E/e′, Ard-Ad values and isovolumetric relaxation time than obese subjects without LVDD. Moreover, lower e′ and e′/a′ were found in the group of LVDD obese. In contrast, there was no difference with respect to EF and end-systolic/end-diastolic LV diameters. Obese subjects with LVDD showed a decreased physical performance in comparison with obese subjects with normal LV function, as observed by a shortened 6-min walk distance.
With respect to HF markers, GDF-15 and FABP4 levels were significantly higher in the obese with LVDD than without LVDD (Table 2).
In Figure 1 the performance of FABP4 serum levels is demonstrated for a variety of echocardiographic parameters of diastolic function. FABP4 levels have been categorized into tertiles of parameter distributions. There was a significant correlation between increasing tertiles of FABP4 with epicardial fat thickness, decreasing e′, increasing E/e′ filling index, LA size, the number of LVDD criteria, as well as decreasing 6-min walking distance. Similar findings could be observed for LV mass (P for trend <0.0001), E/A ratio (measured by pw Doppler, P for trend 0.033), e′/a′ ratio (measured by tissue Doppler, P for trend 0.009), isovolumetric relaxation time (P for trend 0.043) and GDF-15 plasma levels (P for trend 0.002).
Association of increasing tertiles of FABP4 serum levels with epicardial fat thickness, parameters of LVDD and physical performance (6-min walking distance). The figures illustrate both the means diamonds (dotted; the upper and lower edges span the 95% confidence interval) and the box and whisper plots (representing the median, 25, 75, 10, and 90% quantiles) of each parameter.
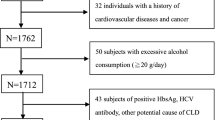
FABP4 serum levels increased by the number of MetS components (from 29.9±4.2 in obese subjects with no additional MetS component to 51±4.0 ng ml−1 in subjects with more than three MetS components, P<0.0001). In Figure 2 FABP4 serum levels are depicted in obese subjects with or without LVDD stratification according to the existence of the MetS. FABP4 levels were comparable in metabolically healthy obese subjects with and without LVDD. However, when the MetS was present, FABP4 levels were significantly higher in the obese with LVDD than in the MetS obese with normal LV function.
Multivariate-adjusted regression analysis of the relationship of different diastolic function parameters with FABP4 serum levels are shown in (Table 3). When accounting for age, sex and visceral obesity (waist-to-hip ratio) there was a significant relationship of FABP4 levels with almost all parameters of diastolic function, with the exception of NT-proBNP levels. The highest beta weights were observed for the association of FABP4 levels with LA size and E/e′ filling index. However, additional adjustment for the existence of the MetS, defined according to NCEP ATPIII, reduced the beta estimates and weakened the association with LVDD parameters.
Discussion
The results of the present study indicate that obesity with LVDD is connected with higher FABP4 levels, particularly when MetS is present.
FABP4 is a small lipid-binding protein, highly expressed in adipose tissue and also expressed in macrophages. It is one of the most abundant cytoplasmic proteins in mature adipocytes with a main function of intracellular binding and trafficking of lipid ligands. However, significant amounts of this protein are found in the circulation and the levels of circulating FABP4 are directly associated with, and even predict the development of the MetS.1, 25 Although its biological role is not fully understood, its function has been correlated to insulin resistance, lipid metabolism, inflammation and atherosclerosis.26 Moreover, increased FABP4 levels have been associated with increased frequencies of cardiovascular events such as acute coronary syndromes, coronary artery disease mortality and congestive HF.17, 27 Indeed, serum FABP4 levels are increasing progressively with the New York Heart Association (NYHA) functional class, and are positively correlated with NT-proBNP, echocardiographic parameters of LV geometry and systolic dysfunction in HF patients.12, 13, 17, 28
Owing to the increasing prevalence of risk factors such as obesity and the MetS, the prevalence of HF is increasing. LVDD is a common pathophysiological mechanism underlying this disorder, with preclinical LVDD believed to be a precursor of HF with preserved EF.29, 30 In fact, LVDD is a common finding in the general population and even asymptomatic LVDD is a powerful and independent risk for increased mortality.31
Our results indicate that FABP4 levels are also related to parameters of LVDD in the morbidly obese. However, the association between LVDD and FABP4 levels was weakened when adjusting for the existence of the MetS. These findings bring to question whether FABP4 is involved in causative links between adiposity, the MetS and related cardiovascular complications, such as LVDD, and ultimately HF.
Although there is ample evidence that FABP4 serum levels correlate with metabolic and inflammatory risk factors and independently predict the presence of the MetS,32, 33 the relation of FABP4 with LVDD might be found only as an indirect association, as the MetS comprises LVDD risk factors such as hypertension and disturbed glucose metabolism. This may be supported by the fact that in our study FABP4 levels were almost identical in obese with and without LVDD, when the MetS was not present.
In contrast, experimental evidence suggests that FABP4 released from human adipocytes potentially links obesity with the development of myocardial contractile dysfunction. Specifically, it has been recently demonstrated that mature human adipocytes release FABP4 in the extracellular medium that strongly suppress the contraction of cardiomyocytes by attenuating intracellular Ca2+ levels, suggesting a direct role in the pathogenesis of myocardial dysfunction.11
Taking into consideration the accumulated evidence for FABP4 as a potential biomarker in systolic and diastolic HF, the crucial question is whether this biomarker is really able to substantially influence current clinical decision making or change the management of HF patients, and whether it has better diagnostic or prognostic accuracy (that is, higher clinical sensitivity) than current prediction tools. In this regard, it needs to be demonstrated that increasing values of FABP4 are translated to higher mortality risk in patients with HF, particularly in the obese. Therefore, prospective outcome studies should be performed to elucidate whether FABP4 also has prognostic impact on morbidity and mortality in the obese.
Although we observed an increase of FABP4 levels in relation to different degrees of LVDD, our results cannot be interpolated to obese subjects with congestive HF. Thus, it would be interesting to see the effect of therapeutical HF management on FABP4 levels in these patients, that is, the effects of loop diuretics in congestive HF. Moreover, the prospective study of serial measurements of FABP4 and its role in relation to considerable weight reduction on diastolic function would reveal interesting future aims of the present study cohort and may help validate FABP4 as a suitable biomarker.
Several limitations should be mentioned. First, the relatively small sample size of our study poses a certain limitation; thus, our results should be verified by more comprehensive studies. Second, the present study is limited by its utilization of echocardiographic techniques for the diagnosis of diastolic abnormalities. In fact, most of the noninvasive parameters for assessment of LV diastolic function by Doppler echocardiography are heart rate-, preload- and afterload-dependent, and may vary over time in a given patient. Moreover, because we studied very obese subjects, echocardiographic measurements might be error-prone or imprecise. However, reliability analysis performed with interobserver agreement statistics shows that concordance correlation for Doppler measurements is reasonably good, thus allowing the use of these measures in epidemiological studies.
In conclusion, we showed for the first time that FABP4 serum levels are positively associated with LVDD in morbidly obese subjects with MetS.
References
Maeda K . Role of adiponectin and adipocyte fatty acid binding protein in the metabolic syndrome. Diabetes Res Clin Pract 2007; 77: S17–S22.
Kralisch S, Fasshauer M . Adipocyte fatty acid binding protein: a novel adipokine involved in the pathogenesis of metabolic and vascular disease? Diabetologia 2013; 56: 10–21.
Furuhashi M, Hotamisligil GS . Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov 2008; 7: 489–503.
Queipo-Ortuno MI, Escote X, Ceperuelo-Mallafre V, Garrido-Sanchez L, Miranda M, Clemente-Postigo M et al. FABP4 dynamics in obesity: discrepancies in adipose tissue and liver expression regarding circulating plasma levels. PLoS One 2012; 7: e48605.
Hotamisligil GS, Johnson RS, Distel RJ, Ellis R, Papaioannou VE, Spiegelman BM . Uncoupling of obesity from insulin resistance through a targeted mutation in aP2, the adipocyte fatty acid binding protein. Science 1996; 274: 1377–1379.
Tuncman G, Erbay E, Hom X, De Vivo I, Campos H, Rimm EB et al. A genetic variant at the fatty acid-binding protein aP2 locus reduces the risk for hypertriglyceridemia, type 2 diabetes, and cardiovascular disease. Proc Natl Acad Sci USA 2006; 103: 6970–6975.
Stejskal D, Karpisek M . Adipocyte fatty acid binding protein in a Caucasian population: a new marker of metabolic syndrome? Eur J Clin Invest 2006; 36: 621–625.
Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH et al. Circulating adipocyte-fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulation 2007; 115: 1537–1543.
Cabre A, Lazaro I, Girona J, Manzanares JM, Marimon F, Plana N et al. Plasma fatty acid binding protein 4 is associated with atherogenic dyslipidemia in diabetes. J Lipid Res 2008; 49: 1746–1751.
Uysal KT, Scheja L, Wiesbrock SM, Bonner-Weir S, Hotamisligil GS . Improved glucose and lipid metabolism in genetically obese mice lacking aP2. Endocrinology 2000; 141: 3388–3396.
Lamounier-Zepter V, Look C, Alvarez J, Christ T, Ravens U, Schunck WH et al. Adipocyte fatty acid-binding protein suppresses cardiomyocyte contraction: a new link between obesity and heart disease. Circ Res 2009; 105: 326–334.
Djousse L, Bartz TM, Ix JH, Kochar J, Kizer JR, Gottdiener JS et al. Fatty acid-binding protein 4 and incident heart failure: the cardiovascular health study. Eur J Heart Fail 2013; 15: 394–399.
Liu M, Zhou M, Bao Y, Xu Z, Li H, Zhang H et al. Circulating adipocyte fatty acid-binding protein levels are independently associated with heart failure. Clin Sci (Lond) 2013; 124: 115–122.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM . Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006; 355: 251–259.
Zile MR, Baicu CF, Gaasch WH . Diastolic heart failure—abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med 2004; 350: 1953–1959.
Aljaroudi W, Alraies MC, Halley C, Rodriguez L, Grimm RA, Thomas JD et al. Impact of progression of diastolic dysfunction on mortality in patients with normal ejection fraction. Circulation 2012; 125: 782–788.
Engeli S, Utz W, Haufe S, Lamounier-Zepter V, Pofahl M, Traber J et al. Fatty acid binding protein 4 predicts left ventricular mass and longitudinal function in overweight and obese women. Heart 2013; 99: 944–948.
Look C, Morano I, Ehrhart-Bornstein M, Bornstein SR, Lamounier-Zepter V . BMS309403 directly suppresses cardiac contractile function. Naunyn Schmiedebergs Arch Pharmacol 2011; 384: 255–263.
Baessler A, Strack C, Rousseva E, Wagner F, Bruxmeier J, Schmiedel M et al. Growth-differentiation factor-15 improves reclassification for the diagnosis of heart failure with normal ejection fraction in morbid obesity. Eur J Heart Fail 2012; 14: 1240–1248.
Strack C, Baessler A, Wagner F, Bruxmeier J, Yaroslavskii O, Rousseva E et al. Mannose-binding lectin in obesity with different degrees of metabolic syndrome abnormalities: association with atherogenic and metabolic traits. J Atheroscler Thromb 2012; 19: 539–551.
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C . Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433–438.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 2009; 10: 165–193.
Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 2007; 28: 2539–2550.
Lin LI . A concordance correlation coefficient to evaluate reproducibility. Biometrics 1989; 45: 255–268.
Xu A, Wang Y, Xu JY, Stejskal D, Tam S, Zhang J et al. Adipocyte fatty acid-binding protein is a plasma biomarker closely associated with obesity and metabolic syndrome. Clin Chem 2006; 52: 405–413.
Makowski L, Hotamisligil GS . The role of fatty acid binding proteins in metabolic syndrome and atherosclerosis. Curr Opin Lipidol 2005; 16: 543–548.
Bao Y, Lu Z, Zhou M, Li H, Wang Y, Gao M et al. Serum levels of adipocyte fatty acid-binding protein are associated with the severity of coronary artery disease in Chinese women. PLoS One 2011; 6: e19115.
Cabre A, Valdovinos P, Lazaro I, Bonet G, Bardaji A, Masana L . Parallel evolution of circulating FABP4 and NT-proBNP in heart failure patients. Cardiovasc Diabetol 2013; 12: 72.
Maeder MT, Kaye DM . Heart failure with normal left ventricular ejection fraction. J Am Coll Cardiol 2009; 53: 905–918.
Kitzman DW . Diastolic heart failure in the elderly. Heart Fail Rev 2002; 7: 17–27.
Mogelvang R, Sogaard P, Pedersen SA, Olsen NT, Marott JL, Schnohr P et al. Cardiac dysfunction assessed by echocardiographic tissue Doppler imaging is an independent predictor of mortality in the general population. Circulation 2009; 119: 2679–2685.
Terra X, Quintero Y, Auguet T, Porras JA, Hernandez M, Sabench F et al. FABP 4 is associated with inflammatory markers and metabolic syndrome in morbidly obese women. Eur J Endocrinol 2011; 164: 539–547.
Karakas SE, Almario RU, Kim K . Serum fatty acid binding protein 4, free fatty acids, and metabolic risk markers. Metabolism 2009; 58: 1002–1007.
Acknowledgements
We thank Kathleen Eisenhofer for kindly proofreading this paper. This study was supported by the German Competence Network of Obesity funded by the Federal Ministry of Education and Research (collaborative project ‘Central and peripheral mechanisms of obesity’, 01GI1122G to VLZ, 01GI1128 to MB and 01GI1320 to AB), by internal funds from the University of Regensburg and the EU Framework 7 project ‘LipidomicNet’.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Baessler, A., Lamounier-Zepter, V., Fenk, S. et al. Adipocyte fatty acid-binding protein levels are associated with left ventricular diastolic dysfunction in morbidly obese subjects. Nutr & Diabetes 4, e106 (2014). https://doi.org/10.1038/nutd.2014.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nutd.2014.3
Keywords
This article is cited by
-
Elevated S-adenosylhomocysteine induces adipocyte dysfunction to promote alcohol-associated liver steatosis
Scientific Reports (2021)
-
The adipokine fatty-acid binding protein 4 and cardiac remodeling
Cardiovascular Diabetology (2020)
-
Association between adipocyte fatty acid-binding protein with left ventricular remodelling and diastolic function in type 2 diabetes: a prospective echocardiography study
Cardiovascular Diabetology (2020)
-
Landscape of heart proteome changes in a diet-induced obesity model
Scientific Reports (2019)
-
Plasma fatty acid-binding protein 4 (FABP4) as a novel biomarker to predict gestational diabetes mellitus
Acta Diabetologica (2016)