Key Points
-
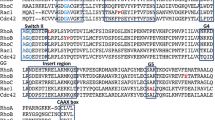
The Rho GTPase family of enzymes is a diverse group of proteins that have critical roles in a number of cellular processes, including cell migration, cell polarity, cell adhesion, cell cycle progression, and regulation of the cytoskeleton. At present, transforming protein RhoA, Ras-related C3 botulinum toxin substrate 1 (Rac1), and cell division control protein 42 homologue (CDC42) are the best characterized
-
The processes that involve Rho GTPases are integral to the development, progression, and spread of malignancy, including urothelial carcinoma
-
The activity of these GTPases is regulated by a number of regulatory proteins, including guanine nucleotide exchange factors (GEFs), GTPase-activating proteins (GAPs), and, in certain classes of GTPases, guanine nucleotide exchange inhibitors (GDIs)
-
The growing understanding of Rho GTPase pathway regulation has resulted in identification of many potential drug targets in several cancers, including urothelial carcinoma. The most promising drug targets are those that inhibit Rho-associated protein kinase (ROCK), a downstream effector of RhoA
-
Most studies of the relationships between the Rho GTPase pathway and malignancy are being performed in preclinical models; the cell culture studies show promise, suggesting that activity levels of proteins are linked with disease characteristics and that inhibition of these proteins can have favourable effects on the disease phenotype
-
In vitro studies are promising, but this field is nascent and it remains to be seen whether manipulation of the Rho GTPase pathway can be a clinically useful anticancer tool. Rho GTPases are highly conserved proteins with considerable homology and complex regulatory processes, meaning considerable potential for off-target effects exists
Abstract
Urothelial carcinoma remains a clinical challenge: non-muscle-invasive disease has a high rate of recurrence and risk of progression, and outcomes for patients with advanced disease are poor, owing to a lack of effective systemic therapies. The Rho GTPase family of enzymes was first identified >30 years ago and contains >20 members, which are divided into eight subfamilies: Cdc42, Rac, Rho, RhoUV, RhoBTB, RhoDF, RhoH, and Rnd. Rho GTPases are molecular on–off switches, which are increasingly being understood to have a critical role in a number of cellular processes, including cell migration, cell polarity, cell adhesion, cell cycle progression, and regulation of the cytoskeleton. This switch is an evolutionarily conserved system in which GTPases alternate between GDP-bound (inactive) and GTP-bound (active) forms. The activities of these Rho GTPases are many, context-dependent, and regulated by a number of proteins that are being progressively elucidated. Aberrations of the Rho GTPase signalling pathways have been implicated in various malignancies, including urothelial carcinoma, and understanding of the role of Rho GTPases in these diseases is increasing. This signalling pathway has the potential for therapeutic targeting in urothelial carcinoma. Research in this area is nascent, and much work is necessary before current laboratory-based research can be translated into the clinic.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2016. CA Cancer J. Clinicians 66, 7–30 (2016).
Sievert, K. D. et al. Economic aspects of bladder cancer: what are the benefits and costs? World J. Urol. 27, 295–300 (2009).
Burger, M. et al. Epidemiology and risk factors of urothelial bladder cancer. Eur. Urol. 63, 234–241 (2013).
Czerniak, B., Dinney, C. & McConkey, D. Origins of bladder cancer. Annu. Rev. Pathol. 11, 149–174 (2016).
Pasin, E., Josephson, D. Y., Mitra, A. P., Cote, R. J. & Stein, J. P. Superficial bladder cancer: an update on etiology, molecular development, classification, and natural history. Rev. Urol. 10, 31–43 (2008).
Woldu, S. L., Bagrodia, A. & Lotan, Y. Guideline of guidelines: non-muscle-invasive bladder cancer. BJU Int. 119, 371–380 (2017).
O'Donnell, M. A. Advances in the management of superficial bladder cancer. Semin. Oncol. 34, 85–97 (2007).
Kurth, K. H. et al. Factors affecting recurrence and progression in superficial bladder tumours. Eur. J. Cancer 31a, 1840–1846 (1995).
Heney, N. M. Natural history of superficial bladder cancer. Prognostic features and long-term disease course. Urol. Clin. North Am. 19, 429–433 (1992).
Youssef, R. F. & Lotan, Y. Predictors of outcome of non-muscle-invasive and muscle-invasive bladder cancer. TheScientificWorldJournal 11, 369–381 (2011).
Abida, W., Bajorin, D. F. & Rosenberg, J. E. First-line treatment and prognostic factors of metastatic bladder cancer for platinum-eligible patients. Hematol. Oncol. Clin. North Am. 29, 319–328 (2015).
Saxman, S. B. et al. Long-term follow-up of a phase III intergroup study of cisplatin alone or in combination with methotrexate, vinblastine, and doxorubicin in patients with metastatic urothelial carcinoma: a cooperative group study. J. Clin. Oncol. 15, 2564–2569 (1997).
von der Maase, H. et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J. Clin. Oncol. 18, 3068–3077 (2000).
Bellmunt, J. et al. Long-term survival results of a randomized phase III trial of vinflunine plus best supportive care versus best supportive care alone in advanced urothelial carcinoma patients after failure of platinum-based chemotherapy. Ann. Oncol. 24, 1466–1472 (2013).
Rosenberg, J. E. et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387, 1909–1920 (2016).
Sharma, P. et al. Nivolumab monotherapy in recurrent metastatic urothelial carcinoma (CheckMate 032): a multicentre, open-label, two-stage, multi-arm, phase 1/2 trial. Lancet Oncol. 17, 1590–1598 (2016).
The Cancer Genome Atlas Research Network. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature 507, 315–322 (2014).
Shariat, S. F. et al. Survivin as a prognostic marker for urothelial carcinoma of the bladder: a multicenter external validation study. Clin. Cancer Res. 15, 7012–7019 (2009).
Shariat, S. F. et al. p53 predictive value for pT1-2 N0 disease at radical cystectomy. J. Urol. 182, 907–913 (2009).
Shariat, S. F. et al. Prospective evaluation of a preoperative biomarker panel for prediction of upstaging at radical cystectomy. BJU Int. 113, 70–76 (2014).
Smith, S. C. et al. A 20-gene model for molecular nodal staging of bladder cancer: development and prospective assessment. Lancet Oncol. 12, 137–143 (2011).
Smith, S. C., Baras, A. S., Lee, J. K. & Theodorescu, D. The COXEN principle: translating signatures of in vitro chemosensitivity into tools for clinical outcome prediction and drug discovery in cancer. Cancer Res. 70, 1753–1758 (2010).
Jones, R. T., Felsenstein, K. M. & Theodorescu, D. Pharmacogenomics: Biomarker-directed therapy for bladder cancer. Urol. Clin. North Am. 43, 77–86 (2016).
Jordan, E. J. & Iyer, G. Targeted therapy in advanced bladder cancer: what have we learned? Urol. Clin. North Am. 42, 253–262 (2015).
Kim, J. W., Tomita, Y., Trepel, J. & Apolo, A. B. Emerging immunotherapies for bladder cancer. Curr. Opin. Oncol. 27, 191–200 (2015).
Yang, X. et al. Diphtheria toxin-epidermal growth factor fusion protein DAB389EGF for the treatment of bladder cancer. Clin. Cancer Res. 19, 148–157 (2013).
Vetter, I. R. & Wittinghofer, A. The guanine nucleotide-binding switch in three dimensions. Science 294, 1299–1304 (2001).
Wennerberg, K., Rossman, K. L. & Der, C. J. The Ras superfamily at a glance. J. Cell Sci. 118, 843–846 (2005).
Li, G. & Qian, H. Kinetic timing: a novel mechanism that improves the accuracy of GTPase timers in endosome fusion and other biological processes. Traffic 3, 249–255 (2002).
Coleman, D. E. et al. Structures of active conformations of Gi alpha 1 and the mechanism of GTP hydrolysis. Science 265, 1405–1412 (1994).
Prive, G. G. et al. X-Ray crystal structures of transforming p21 ras mutants suggest a transition-state stabilization mechanism for GTP hydrolysis. Proc. Natl Acad. Sci. USA 89, 3649–3653 (1992).
Hoffman, G. R., Nassar, N. & Cerione, R. A. Structure of the Rho family GTP-binding protein Cdc42 in complex with the multifunctional regulator RhoGDI. Cell 100, 345–356 (2000).
Johnson, J. L., Erickson, J. W. & Cerione, R. A. New insights into how the Rho guanine nucleotide dissociation inhibitor regulates the interaction of Cdc42 with membranes. J. Biol. Chem. 284, 23860–23871 (2009).
Hodge, R. G. & Ridley, A. J. Regulating Rho GTPases and their regulators. Nat. Rev. Mol. Cell Biol. 17, 496–510 (2016).
Isomura, M., Kikuchi, A., Ohga, N. & Takai, Y. Regulation of binding of rhoB p20 to membranes by its specific regulatory protein, GDP dissociation inhibitor. Oncogene 6, 119–124 (1991).
Cherfils, J. & Zeghouf, M. Regulation of small GTPases by GEFs, GAPs, and GDIs. Physiol. Rev. 93, 269–309 (2013).
Boulter, E. et al. Regulation of Rho GTPase crosstalk, degradation and activity by RhoGDI1. Nat. Cell Biol. 12, 477–483 (2010).
Tnimov, Z. et al. Quantitative analysis of prenylated RhoA interaction with its chaperone, RhoGDI. J. Biol. Chem. 287, 26549–26562 (2012).
Trabalzini, L. & Retta, S. F. Ras Signaling: Methods and Protocols. (Humana Press, 2014).
Madaule, P. & Axel, R. A novel ras-related gene family. Cell 41, 31–40 (1985).
Didsbury, J., Weber, R. F., Bokoch, G. M., Evans, T. & Snyderman, R. rac, a novel ras-related family of proteins that are botulinum toxin substrates. J. Biol. Chem. 264, 16378–16382 (1989).
Boureux, A., Vignal, E., Faure, S. & Fort, P. Evolution of the Rho family of ras-like GTPases in eukaryotes. Mol. Biol. Evol. 24, 203–216 (2007).
Hall, A. Rho family GTPases. Biochem. Soc. Trans. 40, 1378–1382 (2012).
Wang, H. R. et al. Regulation of cell polarity and protrusion formation by targeting RhoA for degradation. Science 302, 1775–1779 (2003).
Heasman, S. J. & Ridley, A. J. Mammalian Rho GTPases: new insights into their functions from in vivo studies. Nat. Rev. Mol. Cell Biol. 9, 690–701 (2008).
Ridley, A. J. Rho GTPases and actin dynamics in membrane protrusions and vesicle trafficking. Trends Cell Biol. 16, 522–529 (2006).
Etienne-Manneville, S. & Hall, A. Rho GTPases in cell biology. Nature 420, 629–635 (2002).
Fernandez-Medarde, A. & Santos, E. Ras in cancer and developmental diseases. Genes Cancer 2, 344–358 (2011).
Price, L. S. & Collard, J. G. Regulation of the cytoskeleton by Rho-family GTPases: implications for tumour cell invasion. Semin. Cancer Biol. 11, 167–173 (2001).
Forbes, S. A. et al. COSMIC: exploring the world's knowledge of somatic mutations in human cancer. Nucleic Acids Res. 43, D805–D811 (2015).
Smithers, C. C. & Overduin, M. Structural mechanisms and drug discovery prospects of Rho GTPases. Cells 5, 26 (2016).
Sakata-Yanagimoto, M. et al. Somatic RHOA mutation in angioimmunoblastic T cell lymphoma. Nat. Genet. 46, 171–175 (2014).
Yoo, H. Y. et al. A recurrent inactivating mutation in RHOA GTPase in angioimmunoblastic T cell lymphoma. Nat. Genet. 46, 371–375 (2014).
Porter, A. P., Papaioannou, A. & Malliri, A. Deregulation of Rho GTPases in cancer. Small GTPases 7, 123–138 (2016).
Khosravi-Far, R., Solski, P. A., Clark, G. J., Kinch, M. S. & Der, C. J. Activation of Rac1, RhoA, and mitogen-activated protein kinases is required for Ras transformation. Mol. Cell. Biol. 15, 6443–6453 (1995).
Karlsson, R., Pedersen, E. D., Wang, Z. & Brakebusch, C. Rho GTPase function in tumorigenesis. Biochim. Biophys. Acta 1796, 91–98 (2009).
Ridley, A. J. Rho proteins and cancer. Breast Cancer Res. Treat. 84, 13–19 (2004).
Fritz, G., Just, I. & Kaina, B. Rho GTPases are over-expressed in human tumors. Int. J. Cancer 81, 682–687 (1999).
Lawson, C. D. et al. Rho GTPase transcriptome analysis reveals oncogenic roles for Rho GTPase-activating proteins in basal-like breast cancers. Cancer Res. 76, 3826–3837 (2016).
Mazieres, J. et al. Loss of RhoB expression in human lung cancer progression. Clin. Cancer Res. 10, 2742–2750 (2004).
Sato, N. et al. RhoB is frequently downregulated in non-small-cell lung cancer and resides in the 2p24 homozygous deletion region of a lung cancer cell line. Int. J. Cancer 120, 543–551 (2007).
Orgaz, J. L., Herraiz, C. & Sanz-Moreno, V. Rho GTPases modulate malignant transformation of tumor cells. Small GTPases 5, e29019 (2014).
Arias-Romero, L. E. & Chernoff, J. Targeting Cdc42 in cancer. Expert Opin. Ther. Targets 17, 1263–1273 (2013).
Cook, D. R., Rossman, K. L. & Der, C. J. Rho guanine nucleotide exchange factors: regulators of Rho GTPase activity in development and disease. Oncogene 33, 4021–4035 (2014).
Cerami, E. et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404 (2012).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6, pl1 (2013).
Golovanov, A. P. et al. Structure-activity relationships in flexible protein domains: regulation of rho GTPases by RhoGDI and D4 GDI. J. Mol. Biol. 305, 121–135 (2001).
Scheffzek, K., Stephan, I., Jensen, O. N., Illenberger, D. & Gierschik, P. The Rac-RhoGDI complex and the structural basis for the regulation of Rho proteins by RhoGDI. Nat. Struct. Biol. 7, 122–126 (2000).
DerMardirossian, C. & Bokoch, G. M. GDIs: central regulatory molecules in Rho GTPase activation. Trends Cell Biol. 15, 356–363 (2005).
Griner, E. M. et al. RhoC is an unexpected target of RhoGDI2 in prevention of lung colonization of bladder cancer. Mol. Cancer Res. 13, 483–492 (2015).
Said, N., Sanchez-Carbayo, M., Smith, S. C. & Theodorescu, D. RhoGDI2 suppresses lung metastasis in mice by reducing tumor versican expression and macrophage infiltration. J. Clin. Invest. 122, 1503–1518 (2012).
Quail, D. F. & Joyce, J. A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 19, 1423–1437 (2013).
Gildea, J. J. et al. RhoGDI2 is an invasion and metastasis suppressor gene in human cancer. Cancer Res. 62, 6418–6423 (2002).
Harding, M. A. & Theodorescu, D. RhoGDI2: a new metastasis suppressor gene: discovery and clinical translation. Urol. Oncol. 25, 401–406 (2007).
Theodorescu, D. et al. Reduced expression of metastasis suppressor RhoGDI2 is associated with decreased survival for patients with bladder cancer. Clin. Cancer Res. 10, 3800–3806 (2004).
Ahmed, M. et al. An osteopontin/CD44 axis in RhoGDI2-mediated metastasis suppression. Cancer Cell 30, 432–443 (2016).
Ahmed, M. et al. Osteopontin: a potentially important therapeutic target in cancer. Expert Opin. Ther. Targets 15, 1113–1126 (2011).
Weber, G. F., Ashkar, S. & Cantor, H. Interaction between CD44 and osteopontin as a potential basis for metastasis formation. Proc. Assoc. Am. Physicians 109, 1–9 (1997).
Bourguignon, L. Y., Zhu, H., Shao, L. & Chen, Y. W. CD44 interaction with tiam1 promotes Rac1 signaling and hyaluronic acid-mediated breast tumor cell migration. J. Biol. Chem. 275, 1829–1838 (2000).
Terawaki, S. et al. The PHCCEx domain of Tiam1/2 is a novel protein- and membrane-binding module. EMBO J. 29, 236–250 (2010).
Nobes, C. D. & Hall, A. Rho, Rac, and Cdc42 GTPases regulate the assembly of multimolecular focal complexes associated with actin stress fibers, lamellipodia, and filopodia. Cell 81, 53–62 (1995).
Michiels, F., Habets, G. G. M., Stam, J. C., van der Kammen, R. A. & Collard, J. G. A role for Rac in Tiaml-induced membrane ruffling and invasion. Nature 375, 338–340 (1995).
Sottnik, J. L. & Theodorescu, D. CD44: a metastasis driver and therapeutic target. Oncoscience 3, 320–321 (2016).
Maisel, D. et al. Targeting tumor cells with anti-CD44 antibody triggers macrophage-mediated immune modulatory effects in a cancer xenograft model. PloS ONE 11, e0159716 (2016).
Riento, K. & Ridley, A. J. Rocks: multifunctional kinases in cell behaviour. Nat. Rev. Mol. Cell Biol. 4, 446–456 (2003).
del Peso, L. et al. Rho proteins induce metastatic properties in vivo. Oncogene 15, 3047–3057 (1997).
Kamai, T. et al. Significant association of Rho/ROCK pathway with invasion and metastasis of bladder cancer. Clin. Cancer Res. 9, 2632–2641 (2003).
Kamai, T. et al. RhoA is associated with invasion and lymph node metastasis in upper urinary tract cancer. BJU Int. 91, 234–238 (2003).
Kamai, T. et al. Increased Rac1 activity and Pak1 overexpression are associated with lymphovascular invasion and lymph node metastasis of upper urinary tract cancer. BMC Cancer 10, 164 (2010).
Kumar, R., Gururaj, A. E. & Barnes, C. J. p21-activated kinases in cancer. Nat. Rev. Cancer 6, 459–471 (2006).
Balasenthil, S. et al. p21-activated kinase-1 signaling mediates cyclin D1 expression in mammary epithelial and cancer cells. J. Biol. Chem. 279, 1422–1428 (2004).
Ito, M. et al. P21-activated kinase 1: a new molecular marker for intravesical recurrence after transurethral resection of bladder cancer. J. Urol. 178, 1073–1079 (2007).
Redelman-Sidi, G., Iyer, G., Solit, D. B. & Glickman, M. S. Oncogenic activation of Pak1-dependent pathway of macropinocytosis determines BCG entry into bladder cancer cells. Cancer Res. 73, 1156–1167 (2013).
Gulhati, P. et al. mTORC1 and mTORC2 regulate EMT, motility and metastasis of colorectal cancer via RhoA and Rac1 signaling pathways. Cancer Res. 71, 3246–3256 (2011).
Jacinto, E. et al. Mammalian TOR complex 2 controls the actin cytoskeleton and is rapamycin insensitive. Nat. Cell Biol. 6, 1122–1128 (2004).
Gupta, S. et al. Mammalian target of rapamycin complex 2 (mTORC2) is a critical determinant of bladder cancer invasion. PloS ONE 8, e81081 (2013).
Zou, Z., Chen, J., Yang, J. & Bai, X. Targeted inhibition of Rictor/mTORC2 in cancer treatment: a new era after rapamycin. Curr. Cancer Drug Targets 16, 288–304 (2016).
Gerullis, H. et al. A phase II trial of temsirolimus in second-line metastatic urothelial cancer. Med. Oncol. 29, 2870–2876 (2012).
Milowsky, M. I. et al. Phase II study of everolimus in metastatic urothelial cancer. BJU Int. 112, 462–470 (2013).
Seront, E. et al. Phase II study of everolimus in patients with locally advanced or metastatic transitional cell carcinoma of the urothelial tract: clinical activity, molecular response, and biomarkers. Ann. Oncol. 23, 2663–2670 (2012).
Hau, A. M., Nakasaki, M., Nakashima, K., Krish, G. & Hansel, D. E. Differential mTOR pathway profiles in bladder cancer cell line subtypes to predict sensitivity to mTOR inhibition. Urol. Oncol. 35, 593–599 (2017).
Wei, L., Surma, M., Shi, S., Lambert-Cheatham, N. & Shi, J. Novel insights into the roles of Rho kinase in cancer. Arch. Immunol. Ther. Exp. 64, 259–278 (2016).
Uehata, M. et al. Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature 389, 990–994 (1997).
Deng, L. et al. Rho-kinase inhibitor, fasudil, suppresses glioblastoma cell line progression in vitro and in vivo. Cancer Biol. Ther. 9, 875–884 (2010).
Xia, Y. et al. Rho kinase inhibitor fasudil suppresses the vasculogenic mimicry of B16 mouse melanoma cells both in vitro and in vivo. Mol. Cancer Ther. 14, 1582–1590 (2015).
Hinsenkamp, I. et al. Inhibition of Rho-associated kinase 1/2 attenuates tumor growth in murine gastric cancer. Neoplasia 18, 500–511 (2016).
Asano, T. et al. Mechanism of action of a novel antivasospasm drug, HA1077. J. Pharmacol. Exp. Ther. 241, 1033–1040 (1987).
Asano, T. et al. Vasodilator actions of HA1077 in vitro and in vivo putatively mediated by the inhibition of protein kinase. Br. J. Pharmacol. 98, 1091–1100 (1989).
Abe, H. et al. The Rho-kinase inhibitor HA-1077 suppresses proliferation/migration and induces apoptosis of urothelial cancer cells. BMC Cancer 14, 412 (2014).
Chang, H. R. et al. The suppressive effect of Rho kinase inhibitor, Y-27632, on oncogenic Ras/RhoA induced invasion/migration of human bladder cancer TSGH cells. Chem. Biol. Interact. 183, 172–180 (2010).
Huang, H. P. et al. Y27632 attenuates the aristolochic acid-promoted invasion and migration of human urothelial cancer TSGH cells in vitro and inhibits the growth of xenografts in vivo. Nephrol. Dialysis Transplant. 27, 565–575 (2012).
Rath, N. & Olson, M. F. Rho-associated kinases in tumorigenesis: re-considering ROCK inhibition for cancer therapy. EMBO Rep. 13, 900–908 (2012).
Tsai, C. C. et al. 7-Chloro-6-piperidin-1-yl-quinoline-5,8-dione (PT-262), a novel ROCK inhibitor blocks cytoskeleton function and cell migration. Biochem. Pharmacol. 81, 856–865 (2011).
Vigil, D. et al. ROCK1 and ROCK2 are required for non-small cell lung cancer anchorage-independent growth and invasion. Cancer Res. 72, 5338–5347 (2012).
Patel, R. A. et al. RKI-1447 is a potent inhibitor of the Rho-associated ROCK kinases with anti-invasive and antitumor activities in breast cancer. Cancer Res. 72, 5025–5034 (2012).
Patel, R. A., Liu, Y., Wang, B., Li, R. & Sebti, S. M. Identification of novel ROCK inhibitors with anti-migratory and anti-invasive activities. Oncogene 33, 550–555 (2014).
Kale, V. P. et al. A novel selective multikinase inhibitor of ROCK and MRCK effectively blocks cancer cell migration and invasion. Cancer Lett. 354, 299–310 (2014).
US National Library of Medicine. ClinicalTrials.gov http://clinicaltrials.gov/ct/show/NCT01585701 (2017).
Lu, Q. Y. et al. Green tea extract modulates actin remodeling via Rho activity in an in vitro multistep carcinogenic model. Clin. Cancer Res. 11, 1675–1683 (2005).
Abiatari, I. et al. Consensus transcriptome signature of perineural invasion in pancreatic carcinoma. Mol. Cancer Ther. 8, 1494–1504 (2009).
Riechelmann, H. et al. Phase I trial with the CD44v6-targeting immunoconjugate bivatuzumab mertansine in head and neck squamous cell carcinoma. Oral Oncol. 44, 823–829 (2008).
Alchemia Limited Alchemia announces phase III trial results for HA-Irinotecan in metastatic colorectal cancer Marketwired.com (2014).
Wennerberg, K. & Der, C. J. Rho-family GTPases: it's not only Rac and Rho (and I like it). J. Cell Sci. 117, 1301–1312 (2004).
Knowles, A. M. & Hurst, C. D. Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity. Nat. Rev. Cancer 15, 25–41 (2015).
Sanli, O. et al. Bladder Cancer. Nat. Rev. Dis. Primers 3, 17022 (2017).
Author information
Authors and Affiliations
Contributions
S.L.W., R.C.H., and L.-M.K. researched data for the article; S.L.W., R.C.H., O.S., and V.M. made substantial contributions to discussions of content; S.L.W. and R.C.H. wrote the article; and S.L.W., L.-M.K., O.S., and V.M. reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Woldu, S., Hutchinson, R., Krabbe, LM. et al. The Rho GTPase signalling pathway in urothelial carcinoma. Nat Rev Urol 15, 83–91 (2018). https://doi.org/10.1038/nrurol.2017.184
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2017.184
This article is cited by
-
RTKN2 knockdown alleviates the malignancy of breast cancer cells by regulating the Wnt/β-catenin pathway
Scientific Reports (2023)
-
KDM6A-ARHGDIB axis blocks metastasis of bladder cancer by inhibiting Rac1
Molecular Cancer (2021)
-
A novel HDGF-ALCAM axis promotes the metastasis of Ewing sarcoma via regulating the GTPases signaling pathway
Oncogene (2021)
-
Rho GTPases in cancer radiotherapy and metastasis
Cancer and Metastasis Reviews (2020)