Key Points
-
Chronic migraine is a clearly defined subtype of migraine affecting between 1–2% of the general population, yet it receives little attention
-
Chronic migraine usually develops from episodic migraine at a conversion rate of about 3% a year; the chronification is reversible
-
Risk factors for migraine chronification include overuse of acute migraine medication, ineffective acute treatment, obesity, depression, low educational status and stressful life events
-
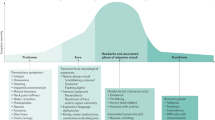
The pathophysiology of migraine chronification can be understood as a threshold problem: certain predisposing factors combined with frequent headache pain lower the threshold of migraine attacks, thereby increasing the risk of chronic migraine
-
Treatment options include pharmacological and nonpharmacological options and neuromodulation
-
Prevention of chronification is essential, and requires adequate treatment of individual migraine attacks, early initiation of preventive medication and avoiding analgesic overuse
Abstract
Chronic migraine has a great detrimental influence on a patient's life, with a severe impact on socioeconomic functioning and quality of life. Chronic migraine affects 1–2% of the general population, and about 8% of patients with migraine; it usually develops from episodic migraine at an annual conversion rate of about 3%. The chronification is reversible: about 26% of patients with chronic migraine go into remission within 2 years of chronification. The most important modifiable risk factors for chronic migraine include overuse of acute migraine medication, ineffective acute treatment, obesity, depression and stressful life events. Moreover, age, female sex and low educational status increase the risk of chronic migraine. The pathophysiology of migraine chronification can be understood as a threshold problem: certain predisposing factors, combined with frequent headache pain, lower the threshold of migraine attacks, thereby increasing the risk of chronic migraine. Treatment options include oral medications, nerve blockade with local anaesthetics or corticoids, and neuromodulation. Well-defined diagnostic criteria are crucial for the identification of chronic migraine. The International Headache Society classification of chronic migraine was recently updated, and now allows co-diagnosis of chronic migraine and medication overuse headache. This Review provides an up-to-date overview of the classification of chronic migraine, basic mechanisms and risk factors of migraine chronification, and the currently established treatment options.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
D'Amico, D. et al. Quality of life and disability in primary chronic daily headaches. Neurol. Sci. 24 (Suppl. 2), S97–S100 (2003).
Buse, D. C. et al. Chronic migraine prevalence, disability, and sociodemographic factors: results from the American Migraine Prevalence and Prevention Study. Headache 52, 1456–1470 (2012).
Bigal, M. E., Serrano, D., Reed, M. & Lipton, R. B. Chronic migraine in the population: burden, diagnosis, and satisfaction with treatment. Neurology 71, 559–566 (2008).
Katsarava, Z. et al. Primary headache disorders in the Republic of Georgia Prevalence and risk factors. Neurology 73, 1796–1803 (2009).
Blumenfeld, A. M. et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS). Cephalalgia 31, 301–315 (2011).
Wiendels, N. J. et al. Chronic frequent headache in the general population: comorbidity and quality of life. Cephalalgia 26, 1443–1450 (2006).
Berra, E. et al. Cost of Chronic and Episodic Migraine. A pilot study from tertiary headache centre northern Italy. J. Headache Pain 16, 532 (2015).
Munakata, J. et al. Economic burden of transformed migraine: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache 49, 498–508 (2009).
iHeadache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33, 629–808 (2013).
Headache Classification Committee et al. New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 26, 742–746 (2006).
Straube, A. et al. Prevalence of chronic migraine and medication overuse headache in Germany — the German DMKG headache study. Cephalalgia 30, 207–213 (2010).
Scher, A. I., Stewart, W. F., Liberman, J. & Lipton, R. B. Prevalence of frequent headache in a population sample. Headache 38, 497–506 (1998).
Yoon, M.-S. et al. Prevalence of primary headaches in Germany: results of the German Headache Consortium Study. J. Headache Pain 13, 215–223 (2012).
Silberstein, S. D., Lipton, R. B. & Sliwinski, M. Classification of daily and near-daily headaches: field trial of revised IHS criteria. Neurology 47, 871–875 (1996).
Scher, A. I., Stewart, W. F., Ricci, J. A. & Lipton, R. B. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain 106, 81–89 (2003).
Mathew, N. T., Reuveni, U. & Perez, F. Transformed or evolutive migraine. Headache 27, 102–106 (1987).
Buse, D. C., Manack, A., Serrano, D., Turkel, C. & Lipton, R. B. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J. Neurol. Neurosurg. Psychiatry 81, 428–432 (2010).
Manack, A., Buse, D. C., Serrano, D., Turkel, C. C. & Lipton, R. B. Rates, predictors, and consequences of remission from chronic migraine to episodic migraine. Neurology 76, 711–718 (2011).
Mathew, N. T., Kurman, R. & Perez, F. Drug induced refractory headache — clinical features and management. Headache 30, 634–638 (1990).
Kudrow, L. Paradoxical effects of frequent analgesic use. Adv. Neurol. 33, 335–341 (1982).
Katsarava, Z. et al. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology 62, 788–790 (2004).
Bahra, A., Walsh, M., Menon, S. & Goadsby, P. J. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache 43, 179–190 (2003).
Paemeleire, K., Bahra, A., Evers, S., Matharu, M. S. & Goadsby, P. J. Medication-overuse headache in patients with cluster headache. Neurology 67, 109–113 (2006).
Williams, L., O'Connell, K. & Tubridy, N. Headaches in a rheumatology clinic: when one pain leads to another. Eur. J. Neurol. 15, 274–277 (2008).
Zwart, J.-A., Dyb, G., Hagen, K., Svebak, S. & Holmen, J. Analgesic use: a predictor of chronic pain and medication overuse headache: the Head-HUNT Study. Neurology 61, 160–164 (2003).
Bigal, M. E. et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache 48, 1157–1168 (2008).
Lipton, R. B. et al. Ineffective acute treatment of episodic migraine is associated with new-onset chronic migraine. Neurology 84, 688–695 (2015).
Bigal, M. E., Liberman, J. N. & Lipton, R. B. Obesity and migraine: a population study. Neurology 66, 545–550 (2006).
Bigal, M. E. & Lipton, R. B. Obesity is a risk factor for transformed migraine but not chronic tension-type headache. Neurology 67, 252–257 (2006).
Ashina, S. et al. Depression and risk of transformation of episodic to chronic migraine. J. Headache Pain 13, 615–624 (2012).
Fava, A. et al. Chronic migraine in women is associated with insulin resistance: a cross-sectional study. Eur. J. Neurol. 21, 267–272 (2014).
Peterlin, B. L., Rosso, A. L., Rapoport, A. M. & Scher, A. I. Obesity and migraine: the effect of age, gender and adipose tissue distribution. Headache 50, 52–62 (2010).
He, Z. et al. Metabolic syndrome in female migraine patients is associated with medication overuse headache: a clinic-based study in China. Eur. J. Neurol. 22, 1228–1234 (2015).
Kitamura, E., Kanazawa, N. & Hamada, J. Hyperleptinemia increases the susceptibility of the cortex to generate cortical spreading depression. Cephalalgia 35, 327–334 (2015).
De Simone, R. et al. Intracranial pressure in unresponsive chronic migraine. J. Neurol. 261, 1365–1373 (2014).
Mathew, N. T., Ravishankar, K. & Sanin, L. C. Coexistence of migraine and idiopathic intracranial hypertension without papilledema. Neurology 46, 1226–1230 (1996).
Vieira, D. S. S. et al. Idiopathic intracranial hypertension with and without papilloedema in a consecutive series of patients with chronic migraine. Cephalalgia 28, 609–613 (2008).
De Simone, R. & Ranieri, A. The role of intracranial hypertension in the chronification of migraine. Neurol. Sci. 36 (Suppl. 1), 23–28 (2015).
Stuginski-Barbosa, J., Macedo, H. R., Bigal, M. E. & Speciali, J. G. Signs of temporomandibular disorders in migraine patients: a prospective, controlled study. Clin. J. Pain 26, 418–421 (2010).
Corchs, F. et al. Sensitivity to aversive stimulation, posttraumatic symptoms and migraines: what do they have in common? Med. Hypotheses 77, 534–535 (2011).
Peterlin, B. L., Tietjen, G., Meng, S., Lidicker, J. & Bigal, M. Post-traumatic stress disorder in episodic and chronic migraine. Headache 48, 517–522 (2008).
Luconi, R. et al. Prognostic significance of personality profiles in patients with chronic migraine. Headache 47, 1118–1124 (2007).
Stankewitz, A., Aderjan, D., Eippert, F. & May, A. Trigeminal nociceptive transmission in migraineurs predicts migraine attacks. J. Neurosci. 31, 1937–1943 (2011).
Judit, A., Sándor, P. S. & Schoenen, J. Habituation of visual and intensity dependence of auditory evoked cortical potentials tends to normalize just before and during the migraine attack. Cephalalgia 20, 714–719 (2000).
Stankewitz, A. & May, A. Cortical excitability and migraine. Cephalalgia 27, 1454–1456 (2007).
Weiller, C. et al. Brain stem activation in spontaneous human migraine attacks. Nat. Med. 1, 658–660 (1995).
Maniyar, F. H., Sprenger, T., Monteith, T., Schankin, C. & Goadsby, P. J. Brain activations in the premonitory phase of nitroglycerin-triggered migraine attacks. Brain J. Neurol. 137, 232–241 (2014).
Cosentino, G. et al. Cyclical changes of cortical excitability and metaplasticity in migraine: evidence from a repetitive transcranial magnetic stimulation study. Pain 155, 1070–1078 (2014).
Schulte, L. H., Jürgens, T. P. & May, A. Photo-, osmo- and phonophobia in the premonitory phase of migraine: mistaking symptoms for triggers? J. Headache Pain 16, 14 (2015).
Dahlem, M. A. et al. Understanding migraine using dynamic network biomarkers. Cephalalgia 35, 627–630 (2015).
Lipton, R. B. et al. Cutaneous allodynia in the migraine population. Ann. Neurol. 63, 148–158 (2008).
Louter, M. A. et al. Cutaneous allodynia as a predictor of migraine chronification. Brain J. Neurol. 136, 3489–3496 (2013).
Bigal, M. E. et al. Prevalence and characteristics of allodynia in headache sufferers: a population study. Neurology 70, 1525–1533 (2008).
Bigal, M. E. & Lipton, R. B. Clinical course in migraine: conceptualizing migraine transformation. Neurology 71, 848–855 (2008).
Welch, K. M., Nagesh, V., Aurora, S. K. & Gelman, N. Periaqueductal gray matter dysfunction in migraine: cause or the burden of illness? Headache 41, 629–637 (2001).
Gentile, G. et al. Lack of association between oxidative stress-related gene polymorphisms and chronic migraine in an Italian population. Expert Rev. Neurother. 15, 215–225 (2015).
Schulte, L. H., Sprenger, C. & May, A. Physiological brainstem mechanisms of trigeminal nociception: an fMRI study at 3T. NeuroImage 124, 518–525 (2015).
Youssef, A. M., Macefield, V. G. & Henderson, L. A. Pain inhibits pain; human brainstem mechanisms. NeuroImage 124 (Pt A), 54–62 (2016).
Stankewitz, A., Voit, H. L., Bingel, U., Peschke, C. & May, A. A new trigemino-nociceptive stimulation model for event-related fMRI. Cephalalgia 30, 475–485 (2010).
Denuelle, M., Fabre, N., Payoux, P., Chollet, F. & Geraud, G. Hypothalamic activation in spontaneous migraine attacks. Headache 47, 1418–1426 (2007).
Cernuda-Morollón, E. et al. Increased VIP levels in peripheral blood outside migraine attacks as a potential biomarker of cranial parasympathetic activation in chronic migraine. Cephalalgia 35, 310–316 (2015).
Cernuda-Morollón, E. et al. Interictal increase of CGRP levels in peripheral blood as a biomarker for chronic migraine. Neurology 81, 1191–1196 (2013).
Burstein, R. et al. Thalamic sensitization transforms localized pain into widespread allodynia. Ann. Neurol. 68, 81–91 (2010).
Andreou, A. P. & Goadsby, P. J. Topiramate in the treatment of migraine: a kainate (glutamate) receptor antagonist within the trigeminothalamic pathway. Cephalalgia 31, 1343–1358 (2011).
Andreou, A. P., Shields, K. G. & Goadsby, P. J. GABA and valproate modulate trigeminovascular nociceptive transmission in the thalamus. Neurobiol. Dis. 37, 314–323 (2010).
Summ, O., Charbit, A. R., Andreou, A. P. & Goadsby, P. J. Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain 133, 2540–2548 (2010).
De Felice, M. et al. Triptan-induced latent sensitization: a possible basis for medication overuse headache. Ann. Neurol. 67, 325–337 (2010).
Green, A. L. et al. Increased susceptibility to cortical spreading depression in an animal model of medication-overuse headache. Cephalalgia 34, 594–604 (2014).
Becerra, L. et al. Triptans disrupt brain networks and promote stress-induced CSD-like responses in cortical and subcortical areas. J. Neurophysiol. 115, 208–217 (2016).
de Tommaso, M. et al. Central sensitisation phenomena in primary headaches: overview of a preventive therapeutic approach. CNS Neurol. Disord. Drug Targets 7, 524–535 (2008).
Evers, S., Jensen, R. & European Federation of Neurological Societies. Treatment of medication overuse headache — guideline of the EFNS headache panel. Eur. J. Neurol. 18, 1115–1121 (2011).
Rossi, P., Jensen, R., Nappi, G., Allena, M. & COMOESTAS Consortium. A narrative review on the management of medication overuse headache: the steep road from experience to evidence. J. Headache Pain 10, 407–417 (2009).
Diener, H.-C. et al. Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia 27, 814–823 (2007).
Aurora, S. K. et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia 30, 793–803 (2010).
Diener, H. C. et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia 30, 804–814 (2010).
Dodick, D. W. et al. OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache 50, 921–936 (2010).
Chiang, C.-C., Schwedt, T. J., Wang, S.-J. & Dodick, D. W. Treatment of medication-overuse headache: a systematic review. Cephalalgia 36, 371–386 (2016).
Holroyd, K. A., Penzien, D. B. & Cordingley, G. E. Propranolol in the management of recurrent migraine: a meta-analytic review. Headache 31, 333–340 (1991).
Linde, K. & Rossnagel, K. Propranolol for migraine prophylaxis. Cochrane Database Syst. Rev. 2, CD003225 (2004).
Silberstein, S. D. & Goadsby, P. J. Migraine: preventive treatment. Cephalalgia 22, 491–512 (2002).
Brandes, J. L. et al. Topiramate for migraine prevention: a randomized controlled trial. JAMA 291, 965–973 (2004).
Chronicle, E. & Mulleners, W. Anticonvulsant drugs for migraine prophylaxis. Cochrane Database Syst. Rev. 3, CD003226 (2004).
Diener, H.-C. et al. Topiramate in migraine prophylaxis — results from a placebo-controlled trial with propranolol as an active control. J. Neurol. 251, 943–950 (2004).
Silberstein, S. D., Neto, W., Schmitt, J., Jacobs, D. & MIGR-001 Study Group. Topiramate in migraine prevention: results of a large controlled trial. Arch. Neurol. 61, 490–495 (2004).
Freitag, F. G. et al. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology 58, 1652–1659 (2002).
Klapper, J. Divalproex sodium in migraine prophylaxis: a dose-controlled study. Cephalalgia 17, 103–108 (1997).
Mathew, N. T. et al. Migraine prophylaxis with divalproex. Arch. Neurol. 52, 281–286 (1995).
Silvestrini, M. et al. Topiramate in the treatment of chronic migraine. Cephalalgia 23, 820–824 (2003).
Silberstein, S. D. et al. Efficacy and safety of topiramate for the treatment of chronic migraine: a randomized, double-blind, placebo-controlled trial. Headache 47, 170–180 (2007).
Silberstein, S. et al. Topiramate treatment of chronic migraine: a randomized, placebo-controlled trial of quality of life and other efficacy measures. Headache 49, 1153–1162 (2009).
Dodick, D. W. et al. The impact of topiramate on health-related quality of life indicators in chronic migraine. Headache 47, 1398–1408 (2007).
Limmroth, V., Biondi, D., Pfeil, J. & Schwalen, S. Topiramate in patients with episodic migraine: reducing the risk for chronic forms of headache. Headache 47, 13–21 (2007).
Mei, D. et al. Topiramate and triptans revert chronic migraine with medication overuse to episodic migraine. Clin. Neuropharmacol. 29, 269–275 (2006).
Lipton, R. B. et al. Topiramate intervention to prevent transformation of episodic migraine: the topiramate INTREPID study. Cephalalgia 31, 18–30 (2011).
Pascual, J., Rivas, M. T. & Leira, R. Testing the combination beta-blocker plus topiramate in refractory migraine. Acta Neurol. Scand. 115, 81–83 (2007).
Silberstein, S. D. et al. Randomized, placebo-controlled trial of propranolol added to topiramate in chronic migraine. Neurology 78, 976–984 (2012).
Stovner, L. J. et al. A comparative study of candesartan versus propranolol for migraine prophylaxis: a randomised, triple-blind, placebo-controlled, double cross-over study. Cephalalgia 34, 523–532 (2013).
Magalhães, E., Menezes, C., Cardeal, M. & Melo, A. Botulinum toxin type A versus amitriptyline for the treatment of chronic daily migraine. Clin. Neurol. Neurosurg. 112, 463–466 (2010).
Yurekli, V. A. et al. The effect of sodium valproate on chronic daily headache and its subgroups. J. Headache Pain 9, 37–41 (2008).
Spira, P. J. & Beran, R. G. & Australian Gabapentin Chronic Daily Headache Group. Gabapentin in the prophylaxis of chronic daily headache: a randomized, placebo-controlled study. Neurology 61, 1753–1759 (2003).
Saper, J. R., Lake, A. E., Cantrell, D. T., Winner, P. K. & White, J. R. Chronic daily headache prophylaxis with tizanidine: a double-blind, placebo-controlled, multicenter outcome study. Headache 42, 470–482 (2002).
Bigal, M., Rapoport, A., Sheftell, F., Tepper, D. & Tepper, S. Memantine in the preventive treatment of refractory migraine. Headache 48, 1337–1342 (2008).
Calandre, E. P., Garcia-Leiva, J. M., Rico-Villademoros, F., Vilchez, J. S. & Rodriguez-Lopez, C. M. Pregabalin in the treatment of chronic migraine: an open-label study. Clin. Neuropharmacol. 33, 35–39 (2010).
Engel, E. R., Kudrow, D. & Rapoport, A. M. A prospective, open-label study of milnacipran in the prevention of headache in patients with episodic or chronic migraine. Neurol. Sci. 35, 429–435 (2014).
Edvardsson, B. Atenolol in the prophylaxis of chronic migraine: a 3-month open-label study. SpringerPlus 2, 479 (2013).
Pascual-Gómez, J. et al. Zonisamide in the preventive treatment of refractory migraine. Rev. Neurol. 50, 129–132 (in Spanish) (2010).
Volpe, F. M. An 8-week, open-label trial of duloxetine for comorbid major depressive disorder and chronic headache. J. Clin. Psychiatry 69, 1449–1454 (2008).
Ayata, C., Jin, H., Kudo, C., Dalkara, T. & Moskowitz, M. A. Suppression of cortical spreading depression in migraine prophylaxis. Ann. Neurol. 59, 652–661 (2006).
Bigal, M. E. et al. Safety, tolerability, and efficacy of TEV-48125 for preventive treatment of chronic migraine: a multicentre, randomised, double-blind, placebo-controlled, phase 2b study. Lancet Neurol. 14, 1091–1100 (2015).
Aurora, S. K. et al. OnabotulinumtoxinA for treatment of chronic migraine: pooled analyses of the 56-week PREEMPT clinical program. Headache 51, 1358–1373 (2011).
Lia, C., Tosi, P., Giardini, G., Caligiana, L. & Bottacchi, E. Onabotulinumtoxin A for prophylaxis in chronic migraine: preliminary data from Headache Regional Centre of Aosta Valley. Neurol. Sci. 35 (Suppl. 1), 175–176 (2014).
Khalil, M., Zafar, H. W., Quarshie, V. & Ahmed, F. Prospective analysis of the use of OnabotulinumtoxinA (BOTOX) in the treatment of chronic migraine; real-life data in 254 patients from Hull, U. K. J. Headache Pain 15, 54 (2014).
Grazzi, L. & Usai, S. Onabotulinum toxin A (Botox) for chronic migraine treatment: an Italian experience. Neurol. Sci. 36 (Suppl. 1), 33–35 (2015).
Jackson, J. L., Kuriyama, A. & Hayashino, Y. Botulinum toxin A for prophylactic treatment of migraine and tension headaches in adults: a meta-analysis. JAMA 307, 1736–1745 (2012).
Cady, R. K., Schreiber, C. P., Porter, J. A. H., Blumenfeld, A. M. & Farmer, K. U. A multi-center double-blind pilot comparison of onabotulinumtoxinA and topiramate for the prophylactic treatment of chronic migraine. Headache 51, 21–32 (2011).
Silberstein, S. D. et al. OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J. Neurol. Sci. 331, 48–56 (2013).
Grazzi, L. & Usai, S. Botulinum toxin A: a new option for treatment of chronic migraine with medication overuse. Neurol. Sci. 35 (Suppl. 1), 37–39 (2014).
Boudreau, G. P., Grosberg, B. M., McAllister, P. J., Lipton, R. B. & Buse, D. C. Prophylactic onabotulinumtoxinA in patients with chronic migraine and comorbid depression: an open-label, multicenter, pilot study of efficacy, safety and effect on headache-related disability, depression, and anxiety. Int. J. Gen. Med. 9, 79–86 (2015).
Maasumi, K., Thompson, N. R., Kriegler, J. S. & Tepper, S. J. Effect of onabotulinumtoxinA injection on depression in chronic migraine. Headache 55, 1218–1224 (2015).
Sandrini, G. et al. Botulinum toxin type-A in the prophylactic treatment of medication-overuse headache: a multicenter, double-blind, randomized, placebo-controlled, parallel group study. J. Headache Pain 12, 427–433 (2011).
Blumenfeld, A. M., Aurora, S. K., Laranjo, K. & Papapetropoulos, S. Unmet clinical needs in chronic migraine: rationale for study and design of COMPEL, an open-label, multicenter study of the long-term efficacy, safety, and tolerability of onabotulinumtoxinA for headache prophylaxis in adults with chronic migraine. BMC Neurol. 15, 100 (2015).
Burstein, R., Zhang, X., Levy, D., Aoki, K. R. & Brin, M. F. Selective inhibition of meningeal nociceptors by botulinum neurotoxin type A: therapeutic implications for migraine and other pains. Cephalalgia 34, 853–869 (2014).
Lackovic´, Z., Filipovic´, B., Matak, I. & Helyes, Z. Botulinum toxin type A activity in cranial dura: implications for treatment of migraine and other headaches. Br. J. Pharmacol. 173, 279–291 (2016).
Cernuda-Morollón, E. et al. OnabotulinumtoxinA decreases interictal CGRP plasma levels in patients with chronic migraine. Pain 156, 820–824 (2015).
Cady, R. et al. An exploratory study of salivary calcitonin gene-related peptide levels relative to acute interventions and preventative treatment with onabotulinumtoxinA in chronic migraine. Headache 54, 269–277 (2014).
Hollanda, L., Monteiro, L. & Melo, A. Botulinum toxin type a for cephalic cutaneous allodynia in chronic migraine: a randomized, double-blinded, placebo-controlled trial. Neurol. Int. 6, 5133 (2014).
Edvinsson, J., Warfvinge, K. & Edvinsson, L. Modulation of inflammatory mediators in the trigeminal ganglion by botulinum neurotoxin type A: an organ culture study. J. Headache Pain 16, 555 (2015).
Sun-Edelstein, C. & Rapoport, A. M. Update on the pharmacological treatment of chronic migraine. Curr. Pain Headache Rep. 20, 6 (2016).
Nestoriuc, Y. & Martin, A. Efficacy of biofeedback for migraine: a meta-analysis. Pain 128, 111–127 (2007).
Busch, V. & Gaul, C. Exercise in migraine therapy — is there any evidence for efficacy? A critical review. Headache 48, 890–899 (2008).
Irby, M. B. et al. Aerobic exercise for reducing migraine burden: mechanisms, markers, and models of change processes. Headache 56, 357–369 (2016).
Harris, P., Loveman, E., Clegg, A., Easton, S. & Berry, N. Systematic review of cognitive behavioural therapy for the management of headaches and migraines in adults. Br. J. Pain 9, 213–224 (2015).
Smitherman, T. A., Wells, R. E. & Ford, S. G. Emerging behavioral treatments for migraine. Curr. Pain Headache Rep. 19, 13 (2015).
Luedtke, K., Allers, A., Schulte, L. H. & May, A. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia 36, 474–492 (2016).
Magis, D. & Schoenen, J. Advances and challenges in neurostimulation for headaches. Lancet Neurol. 11, 708–719 (2012).
Saracco, M. G., Valfrè, W., Cavallini, M. & Aguggia, M. Greater occipital nerve block in chronic migraine. Neurol. Sci. 31 (Suppl. 1), S179–S180 (2010).
Serra, G. & Marchioretto, F. Occipital nerve stimulation for chronic migraine: a randomized trial. Pain Physician 15, 245–253 (2012).
Silberstein, S. D. et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia 32, 1165–1179 (2012).
Schwedt, T. J., Dodick, D. W., Hentz, J., Trentman, T. L. & Zimmerman, R. S. Occipital nerve stimulation for chronic headache — long-term safety and efficacy. Cephalalgia 27, 153–157 (2007).
Palmisani, S. et al. A six year retrospective review of occipital nerve stimulation practice — controversies and challenges of an emerging technique for treating refractory headache syndromes. J. Headache Pain 14, 67 (2013).
Dodick, D. W. et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: long-term results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia 35, 344–358 (2015).
Schoenen, J. et al. Migraine prevention with a supraorbital transcutaneous stimulator A randomized controlled trial. Neurology 80, 697–704 (2013).
Hann, S. & Sharan, A. Dual occipital and supraorbital nerve stimulation for chronic migraine: a single-center experience, review of literature, and surgical considerations. Neurosurg. Focus 35, E9 (2013).
Reed, K. L., Black, S. B., Banta, C. J. & Will, K. R. Combined occipital and supraorbital neurostimulation for the treatment of chronic migraine headaches: initial experience. Cephalalgia 30, 260–271 (2010).
Straube, A., Ellrich, J., Eren, O., Blum, B. & Ruscheweyh, R. Treatment of chronic migraine with transcutaneous stimulation of the auricular branch of the vagal nerve (auricular t-VNS): a randomized, monocentric clinical trial. J. Headache Pain 16, 543 (2015).
Kinfe, T. M. et al. Cervical non-invasive vagus nerve stimulation (nVNS) for preventive and acute treatment of episodic and chronic migraine and migraine-associated sleep disturbance: a prospective observational cohort study. J. Headache Pain 16, 101 (2015).
Cecchini, A. P. et al. Vagus nerve stimulation in drug-resistant daily chronic migraine with depression: preliminary data. Neurol. Sci. 30, S101–S104 (2009).
Mauskop, A. Vagus nerve stimulation relieves chronic refractory migraine and cluster headaches. Cephalalgia 25, 82–86 (2005).
Hord, E. D., Evans, M. S., Mueed, S., Adamolekun, B. & Naritoku, D. K. The effect of vagus nerve stimulation on migraines. J. Pain 4, 530–534 (2003).
Barbanti, P. et al. Non-invasive vagus nerve stimulation for acute treatment of high-frequency and chronic migraine: an open-label study. J. Headache Pain 16, 61 (2015).
Lipton, R. B. et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 9, 373–380 (2010).
Bhola, R. et al. Single-pulse transcranial magnetic stimulation (sTMS) for the acute treatment of migraine: evaluation of outcome data for the UK post market pilot program. J. Headache Pain 16, 535 (2015).
Antal, A., Kriener, N., Lang, N., Boros, K. & Paulus, W. Cathodal transcranial direct current stimulation of the visual cortex in the prophylactic treatment of migraine. Cephalalgia 31, 820–828 (2011).
Dilli, E. et al. Occipital nerve block for the short-term preventive treatment of migraine: a randomized, double-blinded, placebo-controlled study. Cephalalgia 35, 959–968 (2015).
Inan, L. E. et al. Greater occipital nerve blockade for the treatment of chronic migraine: a randomized, multicenter, double-blind, and placebo-controlled study. Acta Neurol. Scand. 132, 270–277 (2015).
Popeney, C. A. & Aló, K. M. Peripheral neurostimulation for the treatment of chronic, disabling transformed migraine. Headache 43, 369–375 (2003).
Saper, J. R. et al. Occipital nerve stimulation for the treatment of intractable chronic migraine headache: ONSTIM feasibility study. Cephalalgia 31, 271–285 (2011).
Lipton, R. B. et al. PRISM study: occipital nerve stimulation for treatment-refractory migraine [abstract]. Cephalalgia 29 (Suppl. 1), 30 (2009).
Chen, Y.-F. et al. Occipital nerve stimulation for chronic migraine — a systematic review and meta-analysis. PLoS ONE 10, e0116786 (2015).
Chen, S.-P. et al. Vagus nerve stimulation inhibits cortical spreading depression. Pain 157, 797–805 (2016).
Brighina, F. et al. rTMS of the prefrontal cortex in the treatment of chronic migraine: a pilot study. J. Neurol. Sci. 227, 67–71 (2004).
Teepker, M. et al. Low-frequency rTMS of the vertex in the prophylactic treatment of migraine. Cephalalgia 30, 137–144 (2010).
Acknowledgements
The authors of this article were supported by the 7th Framework EU-project EuroHeadPain (#602633) and by the German Research Foundation, SFB936/A5 (to A.M).
Author information
Authors and Affiliations
Contributions
Both authors researched the data for the article, provided substantial contributions to discussions of its content, wrote the article and undertook review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
FURTHER INFORMATION
Glossary
- Cutaneous allodynia
-
In cutaneous allodynia, central sensitization to pain causes normally non-noxious tactile stimuli to skin (such as showering, shaving, brushing the hair or wearing tight clothing) to be experienced as painful.
- Descending pain-modulating network
-
A top-down pain modulation system in which brain areas includingthe frontal lobe, hypothalamus and amygdala project on periaqueductal grey, which controls the transmission of nociceptive information in the spinal cord.
- Biofeedback
-
Monitoring of bodily function and responses with biofeedback, such as electromyogram, can help relieve muscle tension and thereby alleviate headache.
- Manual therapy
-
In patients with headache, manual therapy, also known as manipulative therapy — including massage therapy, physiotherapy and spinal manipulative therapy — aims to alleviate headache by relieving muscle tension and increasing mobility of the cervical spine.
- Electrical stimulation
-
Therapeutic options using electrical current, voltage or induction of currents by magnetic fields to influence nerve or muscular functioning.
Rights and permissions
About this article
Cite this article
May, A., Schulte, L. Chronic migraine: risk factors, mechanisms and treatment. Nat Rev Neurol 12, 455–464 (2016). https://doi.org/10.1038/nrneurol.2016.93
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.93
This article is cited by
-
CGRP-targeted medication in chronic migraine - systematic review
The Journal of Headache and Pain (2024)
-
The prevalence of headache in the adult population of Morocco: a cross-sectional population-based study
The Journal of Headache and Pain (2024)
-
Theory of mind in chronic migraine with medication overuse assessed with the MASC
Scientific Reports (2024)
-
Geschlechtsspezifische Ergebnisse des Dresdner Kinder- und Jugendkopfschmerzprogrammes DreKiP
Der Schmerz (2024)
-
Utility of Repetitive Transcranial Magnetic Stimulation for Chronic Daily Headache Prophylaxis: A Systematic Review and Meta-Analysis
Current Pain and Headache Reports (2024)