Key Points
-
Diagnosis of Parkinson disease (PD) requires motor symptoms, but it is now clear that the typical motor signs are preceded by preclinical and prodromal phases of the disease
-
The utility of a marker of prodromal PD depends on the strength of evidence that it is a relevant marker, its specificity, its lead time, and the practicalities of assessment
-
Identification of reliable markers requires prospective studies; studies in high-risk populations are susceptible to selection bias and limited generalizability
-
The strongest marker of prodromal PD is rapid eye movement (REM) sleep behaviour disorder; other markers supported by strong evidence include subtle motor dysfunction, olfactory loss, autonomic dysfunction and affective disorders
-
Markers of prodromal PD have been combined to predict the probability of prodromal PD, most notably in the International Parkinson Disease Movement Disorders Society task force diagnostic guidelines
Abstract
Efforts to develop neuroprotective therapy for Parkinson disease (PD) are focusing on the early stages of disease, which offer the best opportunity to intervene. Early PD can be divided into preclinical, prodromal and clinical stages; in this Review, we focus on the prodromal stage and markers that can be used to identify prodromal PD. We consider the necessary properties of a marker, before providing an overview of the proven and potential markers of prodromal PD, including clinical nonmotor markers, clinical motor markers, neuroimaging markers and tissue biomarkers. Markers for which the ability to predict conversion to PD is supported by the strongest evidence include olfactory loss, REM sleep behaviour disorder and constipation. Markers with the highest diagnostic strength include REM sleep behaviour disorder, dopaminergic imaging and subtle motor parkinsonism. The lead time — the period between the appearance of a marker and conversion to PD — is highly variable between markers, ranging from 5 years for impaired motor performance to >20 years for autonomic symptoms. The cost of screening for these markers also varies dramatically: some require just questionnaires, whereas others require sophisticated scanning techniques. Finally, we summarize how prodromal and risk markers can be combined to estimate the probability that an individual has prodromal PD, with a focus on the International Parkinson Disease and Movement Disorders Society (MDS) Prodromal Parkinson Criteria.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stern, M. B., Lang, A. & Poewe, W. Toward a redefinition of Parkinson's disease. Mov. Disord. 27, 54–60 (2012).
Berg, D. et al. Changing the research criteria for the diagnosis of Parkinson's disease: obstacles and opportunities. Lancet Neurol. 12, 514–524 (2013).
Fearnley, J. M. & Lees, A. J. Ageing and Parkinson's disease: substantia nigra regional selectivity. Brain 114, 2283–2301 (1991).
Fuente-Fernandez, R. et al. Age-specific progression of nigrostriatal dysfunction in Parkinson's disease. Ann. Neurol. 69, 803–810 (2011).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol. Aging 24, 197–211 (2003).
Braak, H. & Del, T. K. Invited article: nervous system pathology in sporadic Parkinson disease. Neurology 70, 1916–1925 (2008).
Beach, T. G. et al. Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropathol. 117, 613–634 (2009).
Parkkinen, L., Pirttila, T. & Alafuzoff, I. Applicability of current staging/categorization of α-synuclein pathology and their clinical relevance. Acta Neuropathol. 115, 399–407 (2008).
Sulzer, D. & Surmeier, D. J. Neuronal vulnerability, pathogenesis, and Parkinson's disease. Mov. Disord. 28, 715–724 (2013).
Adler, C. H. & Beach, T. G. Neuropathological basis of nonmotor manifestations of Parkinson's disease. Mov. Disord. (2016).
London, B. et al. Predictors of prognosis in patients with olfactory disturbance. Ann. Neurol. 63, 159–166 (2008).
Kang, S. H. et al. REM sleep behavior disorder in the Korean elderly population: prevalence and clinical characteristics. Sleep 36, 1147–1152 (2013).
Berg, D. et al. MDS research criteria for prodromal Parkinson's disease. Mov. Disord. 30, 1600–1611 (2015).
Ross, W. et al. Association of olfactory dysfunction with risk of future Parkinson's disease. Ann. Neurol. 63, 167–173 (2008).
Berg, D. et al. The PRIPS study: screening battery for subjects at risk for Parkinson's disease. Eur. J. Neurol. 20, 102–108 (2013).
Abbott, R. D. et al. Frequency of bowel movements and the future risk of Parkinson's disease. Neurology 57, 456–462 (2001).
Berg, D., Marek, K., Ross, G. W. & Poewe, W. Defining at-risk populations for Parkinson's disease: lessons from ongoing studies. Mov. Disord. 27, 656–665 (2012).
Jennings, D. et al. Imaging prodromal Parkinson disease: the Parkinson Associated Risk Syndrome Study. Neurology 83, 1739–1746 (2014).
Pringsheim, T., Jette, N., Frolkis, A. & Steeves, T. D. The prevalence of Parkinson's disease: a systematic review and meta-analysis. Mov. Disord. 29, 1583–1590 (2014).
Siderowf, A. et al. Impaired olfaction and other prodromal features in the Parkinson At-Risk Syndrome Study. Mov. Disord. 27, 406–412 (2012).
Ponsen, M. M. et al. Idiopathic hyposmia as a preclinical sign of Parkinson's disease. Ann. Neurol. 56, 173–181 (2004).
Postuma, R. B., Gagnon, J. F., Bertrand, J. A., Genier Marchand, D. & Montplaisir, J. Y. Parkinson risk in idiopathic REM sleep behavior disorder: preparing for neuroprotective trials. Neurology 84, 1104–1113 (2015).
Sohrabi, H. R. et al. Olfactory discrimination predicts cognitive decline among community-dwelling older adults. Transl Psychiatry 2, e118 (2012).
Postuma, R. B. et al. Risk factors for neurodegeneration in idiopathic rapid eye movement sleep behavior disorder: a multicenter study. Ann. Neurol. 77, 830–839 (2015).
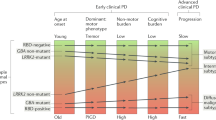
Fereshtehnejad, S. M. et al. New clinical subtypes of Parkinson disease and their longitudinal progression: a prospective cohort comparison with other phenotypes. JAMA Neurol. 72, 863–873 (2015).
Nomura, T., Inoue, Y., Kagimura, T. & Nakashima, K. Clinical significance of REM sleep behavior disorder in Parkinson's disease. Sleep Med. 14, 131–135 (2013).
Anang, J. B. et al. Predictors of dementia in Parkinson disease: a prospective cohort study. Neurology 83, 1253–1260 (2014).
Kang, S. H., Lee, H. M., Seo, W. K., Kim, J. H. & Koh, S. B. The combined effect of REM sleep behavior disorder and hyposmia on cognition and motor phenotype in Parkinson's disease. J. Neurol. Sci. 368, 374–378 (2016).
Schenck, C. H. et al. Rapid eye movement sleep behavior disorder: devising controlled active treatment studies for symptomatic and neuroprotective therapy—a consensus statement from the International Rapid Eye Movement Sleep Behavior Disorder Study Group. Sleep Med. 14, 795–806 (2013).
Chiu, H. F. et al. Sleep-related injury in the elderly —an epidemiological study in Hong Kong. Sleep 23, 513–517 (2000).
Ohayon, M. M., Caulet, M. & Priest, R. G. Violent behavior during sleep. J. Clin. Psychiatry 58, 369–376 (1997).
Schenck, C. H., Boeve, B. F. & Mahowald, M. W. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 14, 744–748 (2013).
Iranzo, A. et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLoS ONE 9, e89741 (2014).
Wing, Y. K. et al. Prospective outcome of rapid eye movement sleep behaviour disorder: psychiatric disorders as a potential early marker of Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 83, 470–472 (2012).
Arnulf, I. et al. Sleepiness in idiopathic REM sleep behavior disorder and Parkinson disease. Sleep 38, 1529–1535 (2015).
Boot, B. P. et al. Probable rapid eye movement sleep behavior disorder increases risk for mild cognitive impairment and Parkinson disease: a population-based study. Ann. Neurol. 71, 49–56 (2012).
Boeve, B. F. et al. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep Med. 14, 754–762 (2013).
Sixel-Doring, F., Trautmann, E., Mollenhauer, B. & Trenkwalder, C. Associated factors for REM sleep behavior disorder in Parkinson disease. Neurology 77, 1048–1054 (2011).
Postuma, R. B. et al. A single-question screen for rapid eye movement sleep behavior disorder: a multicenter validation study. Mov. Disord. 27, 913–916 (2012).
Frauscher, B. et al. Validation of the Innsbruck REM sleep behavior disorder inventory. Mov. Disord. 27, 1673–1678 (2012).
Postuma, R. B. et al. Screening for prodromal Parkinson's disease in the general community: a sleep-based approach. Sleep Med. 21, 101–105 (2016).
Fahn, S., Elton, R. & members of the UPDRS Development Committee in Recent Developments in Parkinson's Disease (eds Fahn, S., Marsden, C. D., Calne, D. & Goldstein, M.) 153–163 (MacMillan HealthCare Information, 1987).
Postuma, R. B., Lang, A. E., Gagnon, J. F., Pelletier, A. & Montplaisir, J. Y. How does parkinsonism start? Prodromal parkinsonism motor changes in idiopathic REM sleep behaviour disorder. Brain 135, 1860–1870 (2012).
Hasmann, S. E. et al. Instrumented functional reach test differentiates individuals at high risk for Parkinson's disease from controls. Front. Aging Neurosci. 6, 286 (2014).
Keezer, M. R., Wolfson, C. & Postuma, R. B. Age, gender, comorbidity, and the MDS-UPDRS: results from a population-based study. Neuroepidemiology 46, 222–227 (2016).
Haehner, A. et al. Olfactory loss may be a first sign of idiopathic Parkinson's disease. Mov. Disord. 22, 839–842 (2007).
Ross, G. W. et al. Association of olfactory dysfunction with risk for future Parkinson's disease. Ann. Neurol. 63, 167–173 (2008).
Ponsen, M. M., Stoffers, D., Twisk, J. W., Wolters, E. C. & Berendse, H. W. Hyposmia and executive dysfunction as predictors of future Parkinson's disease: a prospective study. Mov. Disord. 24, 1060–1065 (2009).
Postuma, R. B., Gagnon, J. F., Vendette, M., Desjardins, C. & Montplaisir, J. Olfaction and color vision identify impending neurodegeneration in REM behavior disorder. Ann. Neurol. 69, 811–818 (2011).
Mahlknecht, P. et al. Olfactory dysfunction predicts early transition to a Lewy body disease in idiopathic RBD. Neurology 84, 654–658 (2015).
Jennings, D., Stern, M., Siderowf, A. & Marek, K. Longitudinal imaging and phenoconversion in the PARS prodromal cohort [abstract]. Neurodegener. Dis. 15 (Suppl. 1), 242 (2015).
Berg, D. et al. Time to redefine PD? Introductory statement of the MDS Task Force on the definition of Parkinson's disease. Mov. Disord. 29, 454–462 (2014).
McShane, R. H. et al. Anosmia in dementia is associated with Lewy bodies rather than Alzheimer's pathology. J. Neurol. Neurosurg. Psychiatry 70, 739–743 (2001).
Postuma, R. B. et al. Identifying prodromal Parkinson's disease: pre-motor disorders in Parkinson's disease. Mov. Disord. 27, 617–626 (2012).
Hummel, T., Sekinger, B., Wolf, S. R., Pauli, E. & Kobal, G. 'Sniffin' Sticks': olfactory performance assessed by the combined testing of odour identification, odor discrimination and olfactory threshold. Chem. Senses 22, 39–52 (1997).
Doty, R. L., Shaman, P. & Dann, M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol. Behav. 32, 489–502 (1984).
Savica, R. et al. Medical records documentation of constipation preceding Parkinson disease: a case-control study. Neurology 73, 1752–1758 (2009).
Gao, X., Chen, H., Schwarzschild, M. A. & Ascherio, A. A prospective study of bowel movement frequency and risk of Parkinson's disease. Am. J. Epidemiol. 174, 546–551 (2011).
Lin, C. H., Lin, J. W., Liu, Y. C., Chang, C. H. & Wu, R. M. Risk of Parkinson's disease following severe constipation: a nationwide population-based cohort study. Parkinsonism Relat. Disord. 20, 1371–1375 (2014).
Plouvier, A. O. et al. Prodromal symptoms and early detection of Parkinson's disease in general practice: a nested case-control study. Fam. Pract. 31, 373–378 (2014).
Schrag, A., Horsfall, L., Walters, K., Noyce, A. & Petersen, I. Prediagnostic presentations of Parkinson's disease in primary care: a case-control study. Lancet Neurol. 14, 57–64 (2015).
Noyce, A. J. et al. Meta-analysis of early nonmotor features and risk factors for Parkinson disease. Ann. Neurol. 72, 893–901 (2012).
Postuma, R. B., Gagnon, J. F., Pelletier, A. & Montplaisir, J. Prodromal autonomic symptoms and signs in Parkinson's disease and dementia with Lewy bodies. Mov. Disord. 28, 597–604 (2013).
Gray, M. T., Munoz, D. G., Gray, D. A., Schlossmacher, M. G. & Woulfe, J. M. Alpha-synuclein in the appendiceal mucosa of neurologically intact subjects. Mov. Disord. 29, 991–998 (2014).
Luk, K. C. et al. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science 338, 949–953 (2012).
Svensson, E. et al. Vagotomy and subsequent risk of Parkinson's disease. Ann. Neurol. 78, 522–529 (2015).
Gibbons, C. H. & Freeman, R. Clinical implications of delayed orthostatic hypotension: a 10-year follow-up study. Neurology 85, 1362–1367 (2015).
Velseboer, D. C., de Haan, R. J., Wieling, W., Goldstein, D. S. & de Bie, R. M. Prevalence of orthostatic hypotension in Parkinson's disease: a systematic review and meta-analysis. Parkinsonism Relat. Disord. 17, 724–729 (2011).
Gao, X. et al. Erectile function and risk of Parkinson's disease. Am. J. Epidemiol. 166, 1446–1450 (2007).
Abbott, R. D. et al. Excessive daytime sleepiness and subsequent development of Parkinson disease. Neurology 65, 1442–1446 (2005).
Gao, J. et al. Daytime napping, nighttime sleeping, and Parkinson disease. Am. J. Epidemiol. 173, 1032–1038 (2011).
Simuni, T. et al. Correlates of excessive daytime sleepiness in de novo Parkinson's disease: a case control study. Mov. Disord. 30, 1371–1381 (2015).
Arnulf, I. Excessive daytime sleepiness in parkinsonism. Sleep Med. Rev. 9, 185–200 (2005).
Merino-Andreu, M., Arnulf, I., Konofal, E., Derenne, J. P. & Agid, Y. Unawareness of naps in Parkinson's disease and in disorders with excessive daytime sleepiness. Neurology 60, 1553–1554 (2003).
Leentjens, A. F., Van den, A. M., Metsemakers, J. F., Lousberg, R. & Verhey, F. R. Higher incidence of depression preceding the onset of Parkinson's disease: a register study. Mov. Disord. 18, 414–418 (2003).
Leentjens, A. F., Driessen, G., Weber, W., Drukker, M. & van Os, J. Mental health care use in Parkinson's disease: a record linkage study. Neuroepidemiology 30, 71–75 (2008).
Fang, F. et al. Depression and the subsequent risk of Parkinson's disease in the NIH-AARP Diet and Health Study. Mov. Disord. 25, 1157–1162 (2010).
Gustafsson, H., Nordstrom, A. & Nordstrom, P. Depression and subsequent risk of Parkinson disease: a nationwide cohort study. Neurology 84, 2422–2429 (2015).
Weisskopf, M. G., Chen, H., Schwarzschild, M. A., Kawachi, I. & Ascherio, A. Prospective study of phobic anxiety and risk of Parkinson's disease. Mov. Disord. 18, 646–651 (2003).
Alonso, A., Rodriguez, L. A., Logroscino, G. & Hernan, M. A. Use of antidepressants and the risk of Parkinson's disease: a prospective study. J. Neurol. Neurosurg. Psychiatry 80, 671–674 (2009).
Seeley, W. W., Crawford, R. K., Zhou, J., Miller, B. L. & Greicius, M. D. Neurodegenerative diseases target large-scale human brain networks. Neuron 62, 42–52 (2009).
Bower, J. H. et al. Anxious personality predicts an increased risk of Parkinson's disease. Mov. Disord. 25, 2105–2113 (2010).
Ishihara, L. & Brayne, C. What is the evidence for a premorbid parkinsonian personality: a systematic review. Mov. Disord. 21, 1066–1072 (2006).
Koo, B. B. Restless leg syndrome across the globe: epidemiology of the restless legs syndrome/Willis–Ekbom disease. Sleep Med. Clin. 10, 189–205 (2015).
Wong, J. C., Li, Y., Schwarzschild, M. A., Ascherio, A. & Gao, X. Restless legs syndrome: an early clinical feature of Parkinson disease in men. Sleep 37, 369–372 (2014).
Buttner, T. et al. Distorted color discrimination in 'de novo' parkinsonian patients. Neurology 45, 386–387 (1995).
Bertrand, J. A. et al. Color discrimination deficits in Parkinson's disease are related to cognitive impairment and white-matter alterations. Mov. Disord. 27, 1781–1788 (2012).
Lawson, R. A. et al. Cognitive decline and quality of life in incident Parkinson's disease: the role of attention. Parkinsonism Relat. Disord. 27, 47–53 (2016).
Aarsland, D. Cognitive impairment in Parkinson's disease and dementia with Lewy bodies. Parkinsonism Relat. Disord. 22 (Suppl. 1), S144–S148 (2016).
Weintraub, D. et al. Cognitive performance and neuropsychiatric symptoms in early, untreated Parkinson's disease. Mov. Disord. 30, 919–927 (2015).
Postuma, R. B. et al. MDS clinical diagnostic criteria for Parkinson's disease. Mov. Disord. 30, 1591–1600 (2015).
Chahine, L. M. et al. Cognition in individuals at risk for Parkinson's: Parkinson associated risk syndrome (PARS) study findings. Mov. Disord. 31, 86–94 (2016).
Darweesh, S. et al. Trajectories of prediagnostic motor and non-motor functioning in Parkinson disease [abstract]. Neurology 86, s5.005 (2016).
Iranzo, A. et al. Decreased striatal dopamine transporters uptake and substantia nigra hyperechogenicity as risk markers of synucleinopathy in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective study. Lancet Neurol. 9, 1070–1077 (2010).
Eisensehr, I. et al. Reduced striatal dopamine transporters in idiopathic rapid eye movement sleep behaviour disorder. comparison with Parkinson's disease and controls. Brain 123, 1155–1160 (2000).
Morrish, P. K., Rakshi, J. S., Bailey, D. L., Sawle, G. V. & Brooks, D. J. Measuring the rate of progression and estimating the preclinical period of Parkinson's disease with [18F]dopa PET. J. Neurol. Neurosurg. Psychiatry 64, 314–319 (1998).
Nurmi, E. et al. Rate of progression in Parkinson's disease: a 6-[18]fluoro-L-dopa PET study. Mov. Disord. 16, 608–615 (2001).
Gaenslen, A. et al. The specificity and sensitivity of transcranial ultrasound in the differential diagnosis of Parkinson's disease: a prospective blinded study. Lancet Neurol. 7, 417–424 (2008).
Iova, A. et al. Postnatal decrease in substantia nigra echogenicity. Implications for the pathogenesis of Parkinson's disease. J. Neurol. 251, 1451–1454 (2004).
Iranzo, A. et al. Five-year follow-up of substantia nigra echogenicity in idiopathic REM sleep behavior disorder. Mov. Disord. 29, 1774–1780 (2014).
Schroeder, U. et al. Substantia nigra hyperechogenicity in healthy controls: a [18Fluoro] Dopa-PET follow-up study. J. Neurol. 260, 1907–1911 (2013).
Ellmore, T. M. et al. Altered nigrostriatal and nigrocortical functional connectivity in rapid eye movement sleep behavior disorder. Sleep 36, 1885–1892 (2013).
Scherfler, C. et al. White and gray matter abnormalities in idiopathic rapid eye movement sleep behavior disorder: a diffusion-tensor imaging and voxel-based morphometry study. Ann. Neurol. 69, 400–407 (2011).
Rolinski, M. et al. Basal ganglia dysfunction in idiopathic REM sleep behaviour disorder parallels that in early Parkinson's disease. Brain 139, 2224–2234 (2016).
Miyamoto, T. et al. Reduced cardiac 123I-MIBG scintigraphy in idiopathic REM sleep behavior disorder. Neurology 67, 2236–2238 (2006).
Holtbernd, F. et al. Abnormal metabolic network activity in REM sleep behavior disorder. Neurology 82, 620–627 (2014).
Dang-Vu, T. T. et al. Hippocampal perfusion predicts impending neurodegeneration in REM sleep behavior disorder. Neurology 79, 2302–2306 (2012).
Alonso, A., Huang, X., Mosley, T. H., Heiss, G. & Chen, H. Heart rate variability and the risk of Parkinson disease: The Atherosclerosis Risk in Communities study. Ann. Neurol. 77, 877–883 (2015).
Jain, S. et al. Cardiovascular physiology in premotor Parkinson's disease: a neuroepidemiologic study. Mov. Disord. 27, 988–995 (2012).
Postuma, R. B., Lanfranchi, P. A., Blais, H., Gagnon, J. F. & Montplaisir, J. Y. Cardiac autonomic dysfunction in idiopathic REM sleep behavior disorder. Mov. Disord. 25, 2304–2310 (2010).
Postuma, R. B. et al. Cardiac autonomic denervation in Parkinson's disease is linked to REM sleep behavior disorder. Mov. Disord. 26, 1529–1533 (2011).
Stokholm, M. G., Danielsen, E. H., Hamilton-Dutoit, S. J. & Borghammer, P. Pathological α-synuclein in gastrointestinal tissues from prodromal parkinson's disease patients. Ann. Neurol. 79, 940–949 (2016).
Vilas, D. et al. Assessment of α-synuclein in submandibular glands of patients with idiopathic rapid-eye-movement sleep behaviour disorder: a case-control study. Lancet Neurol. 15, 708–718 (2016).
Adler, C. H. et al. Peripheral synucleinopathy in early Parkinson's disease: submandibular gland needle biopsy findings. Mov. Disord. 31, 250–256 (2016).
Noyce, A. J. et al. PREDICT-PD: identifying risk of Parkinson's disease in the community: methods and baseline results. J. Neurol. Neurosurg. Psychiatry 85, 31–37 (2014).
Darweesh, S. K. et al. Predicting Parkinson disease in the community using a nonmotor risk score. Eur. J. Epidemiol. 31, 679–684 (2016).
Nalls, M. A. et al. Diagnosis of Parkinson's disease on the basis of clinical and genetic classification: a population-based modelling study. Lancet Neurol. 14, 1002–1009 (2015).
Mahlknecht, P. et al. Prodromal Parkinson's disease as defined per MDS research criteria in the general elderly community. Mov. Disord. 31, 1405–1408 (2016).
Acknowledgements
R.B.P. has received grants from the Fonds de la Recherche en Sante Quebec, the Canadian Institute of Health Research, the Parkinson Society of Canada, the Weston-Garfield Foundation, the Michael J. Fox foundation, and the Webster Foundation. D.B. has received research grants from the European Union, the German Parkinson's Disease Association, the Michael J. Fox Foundation and Parkinson Fonds Deutschland.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
R.B.P. has received funding for consultancy from Biotie, Biogen and Roche, and speaker fees from Novartis Canada and Teva Neurosciences. D.B. has received funds for consultancy and/or speaking from Lundbeck, Novartis, Teva and UCB, and research grants from Janssen Pharmaceuticals, Teva and UCB.
Rights and permissions
About this article
Cite this article
Postuma, R., Berg, D. Advances in markers of prodromal Parkinson disease. Nat Rev Neurol 12, 622–634 (2016). https://doi.org/10.1038/nrneurol.2016.152
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.152
This article is cited by
-
Neurocognitive correlates of semantic memory navigation in Parkinson’s disease
npj Parkinson's Disease (2024)
-
Sexual dysfunction in a sample of Egyptian patients with Parkinson’s disease
Neurological Sciences (2024)
-
Theta oscillations and minor hallucinations in Parkinson’s disease reveal decrease in frontal lobe functions and later cognitive decline
Nature Mental Health (2023)
-
Relationship Between Short-chain Fatty Acids and Parkinson’s Disease: A Review from Pathology to Clinic
Neuroscience Bulletin (2023)
-
Correlation of olfactory function factors with cardiac sympathetic denervation in Parkinson’s disease
Journal of Neurology (2023)