Key Points
-
Chemotherapy-induced peripheral neuropathic pain (CIPNP) affects up to 80% of patients during chemotherapy; it is a severe adverse effect that can limit dose and choice of chemotherapy
-
Many substances already approved for treating neuropathic pain failed to ameliorate CIPNP in clinical trials, underlining the importance of assessing drug efficacy in CIPNP independently of other neuropathic pain states
-
CIPNP has distinctive mechanisms that depend on the causative cytostatic drug; this heterogeneity could explain why results from trials addressing classic neuropathic pain states do not translate to CIPNP
-
Clinical trial designers in academia and industry are encouraged to implement sensory profiling in patient stratification to tailor the analgesic treatment according to the individual underlying mechanisms of CIPNP
-
Mechanisms involved in CIPNP include disruption of axonal transport, altered ion channel and receptor activity, neuronal injury and inflammation, oxidative stress, and mitochondrial damage
-
Suggestions for mechanism-based therapy of CIPNP include duloxetine for oxaliplatin-induced CIPNP, and combination of neuroprotective and anti-inflammatory substances for CIPNP caused by paclitaxel or vincristine
Abstract
Chemotherapy-induced peripheral neuropathic pain (CIPNP)—a severe adverse effect observed in up to 80% of patients during treatment with antineoplastic drugs—limits the tolerable dose of cytostatics, and can lead to discontinuation of chemotherapy. Many drugs that are approved for the treatment of other neuropathic pain states have shown little or no analgesic effect on CIPNP in large randomized, placebo-controlled clinical trials. Here, we review the known mechanisms of CIPNP induced by the three most commonly used cytostatics: paclitaxel, oxaliplatin and vincristine. These substances have distinct neurotoxic and neuroinflammatory properties, but they also have overlapping contributions to pathogenesis of CIPNP that could potentially be targeted for prevention or treatment of CIPNP. We discuss the failure of previously tested antioxidants, neuroprotective agents, anticonvulsants and antidepressants as therapeutic or preventative strategies, and suggest individualized, mechanism-based therapeutic options for CIPNP associated with each of the three main drug groups. We point out the necessity to assess drug efficacy in CIPNP independently of other neuropathic pain states, and emphasize the need for delineation of subpopulations of patients with CIPNP for more-efficient treatment. Finally, we discuss novel therapeutic strategies and recent progress in treatment of CIPNP, and evaluate the potential benefits of these recent proceedings for future therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pachman, D. R., Barton, D. L., Watson, J. C. & Loprinzi, C. L. Chemotherapy-induced peripheral neuropathy: prevention and treatment. Clin. Pharmacol. Ther. 90, 377–387 (2011).
Loprinzi, C. L. et al. The paclitaxel acute pain syndrome: sensitization of nociceptors as the putative mechanism. Cancer J. 13, 399–403 (2007).
Grisold, W., Cavaletti, G. & Windebank, A. J. Peripheral neuropathies from chemotherapeutics and targeted agents: diagnosis, treatment, and prevention. Neuro Oncol. 14 (Suppl. 4), iv45–iv54 (2012).
Manji, H. Toxic neuropathy. Curr. Opin. Neurol. 24, 484–490 (2011).
Argyriou, A. A., Bruna, J., Marmiroli, P. & Cavaletti, G. Chemotherapy-induced peripheral neurotoxicity (CIPN): an update. Crit. Rev. Oncol. Hematol. 82, 51–77 (2012).
Park, S. B. et al. Chemotherapy-induced peripheral neurotoxicity: a critical analysis. CA Cancer J. Clin. 63, 419–437 (2013).
Park, S. B. et al. Mechanisms underlying chemotherapy-induced neurotoxicity and the potential for neuroprotective strategies. Curr. Med. Chem. 15, 3081–3094 (2008).
Materazzi, S. et al. TRPA1 and TRPV4 mediate paclitaxel-induced peripheral neuropathy in mice via a glutathione-sensitive mechanism. Pflugers Arch. 463, 561–569 (2012).
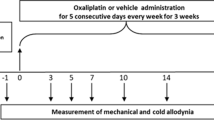
Nassini, R. et al. Oxaliplatin elicits mechanical and cold allodynia in rodents via TRPA1 receptor stimulation. Pain 152, 1621–1631 (2011).
Nieto, F. R. et al. Tetrodotoxin inhibits the development and expression of neuropathic pain induced by paclitaxel in mice. Pain 137, 520–531 (2008).
Xiao, W., Boroujerdi, A., Bennett, G. J. & Luo, Z. D. Chemotherapy-evoked painful peripheral neuropathy: analgesic effects of gabapentin and effects on expression of the alpha-2-delta type-1 calcium channel subunit. Neuroscience 144, 714–720 (2007).
Musatov, A. & Robinson, N. C. Susceptibility of mitochondrial electron-transport complexes to oxidative damage. Focus on cytochrome c oxidase. Free Radic. Res. 46, 1313–1326 (2012).
Peters, C. M., Jimenez-Andrade, J. M., Kuskowski, M. A., Ghilardi, J. R. & Mantyh, P. W. An evolving cellular pathology occurs in dorsal root ganglia, peripheral nerve and spinal cord following intravenous administration of paclitaxel in the rat. Brain Res. 1168, 46–59 (2007).
Ji, X. T. et al. Spinal astrocytic activation contributes to mechanical allodynia in a rat chemotherapy-induced neuropathic pain model. PLoS ONE 8, e60733 (2013).
Ji, R. R., Berta, T. & Nedergaard, M. Glia and pain: is chronic pain a gliopathy? Pain 154 (Suppl. 1), S10–S28 (2013).
Hershman, D. L. et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. 32, 1941–1967 (2014).
Rao, R. D. et al. Efficacy of gabapentin in the management of chemotherapy-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled, crossover trial (N00C3). Cancer 110, 2110–2118 (2007).
Kautio, A. L. et al. Amitriptyline in the prevention of chemotherapy-induced neuropathic symptoms. Anticancer Res. 29, 2601–2606 (2009).
Wani, M. C., Taylor, H. L., Wall, M. E., Coggon, P. & McPhail, A. T. Plant antitumor agents. VI. The isolation and structure of taxol, a novel antileukemic and antitumor agent from Taxus brevifolia. J. Am. Chem. Soc. 93, 2325–2327 (1971).
Shoudai, K., Peters, J. H., McDougall, S. J., Fawley, J. A. & Andresen, M. C. Thermally active TRPV1 tonically drives central spontaneous glutamate release. J. Neurosci. 30, 14470–14475 (2010).
Loprinzi, C. L. et al. Natural history of paclitaxel-associated acute pain syndrome: prospective cohort study NCCTG N08C1. J. Clin. Oncol. 29, 1472–1478 (2011).
Kavallaris, M. Microtubules and resistance to tubulin-binding agents. Nat. Rev. Cancer 10, 194–204 (2010).
Amos, L. A. & Lowe, J. How Taxol® stabilises microtubule structure. Chem. Biol. 6, R65–R69 (1999).
Shemesh, O. A. & Spira, M. E. Paclitaxel induces axonal microtubules polar reconfiguration and impaired organelle transport: implications for the pathogenesis of paclitaxel-induced polyneuropathy. Acta Neuropathol. 119, 235–248 (2010).
LaPointe, N. E. et al. Effects of eribulin, vincristine, paclitaxel and ixabepilone on fast axonal transport and kinesin-1 driven microtubule gliding: implications for chemotherapy-induced peripheral neuropathy. Neurotoxicology 37, 231–239 (2013).
Siau, C., Xiao, W. & Bennett, G. J. Paclitaxel- and vincristine-evoked painful peripheral neuropathies: loss of epidermal innervation and activation of Langerhans cells. Exp. Neurol. 201, 507–514 (2006).
Liu, C. C. et al. Prevention of paclitaxel-induced allodynia by minocycline: effect on loss of peripheral nerve fibers and infiltration of macrophages in rats. Mol. Pain 6, 76 (2010).
Jin, H. W., Flatters, S. J., Xiao, W. H., Mulhern, H. L. & Bennett, G. J. Prevention of paclitaxel-evoked painful peripheral neuropathy by acetyl-L-carnitine: effects on axonal mitochondria, sensory nerve fiber terminal arbors, and cutaneous Langerhans cells. Exp. Neurol. 210, 229–237 (2008).
Flatters, S. J. & Bennett, G. J. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain 122, 245–257 (2006).
Zheng, H., Xiao, W. H. & Bennett, G. J. Functional deficits in peripheral nerve mitochondria in rats with paclitaxel- and oxaliplatin-evoked painful peripheral neuropathy. Exp. Neurol. 232, 154–161 (2011).
Pascual, D., Goicoechea, C., Burgos, E. & Martin, M. I. Antinociceptive effect of three common analgesic drugs on peripheral neuropathy induced by paclitaxel in rats. Pharmacol. Biochem. Behav. 95, 331–337 (2010).
Flatters, S. J. & Bennett, G. J. Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain 109, 150–161 (2004).
Hara, T. et al. Effect of paclitaxel on transient receptor potential vanilloid 1 in rat dorsal root ganglion. Pain 154, 882–889 (2013).
Alessandri-Haber, N. et al. Transient receptor potential vanilloid 4 is essential in chemotherapy-induced neuropathic pain in the rat. J. Neurosci. 24, 4444–4452 (2004).
Xiao, W. H. & Bennett, G. J. Effects of mitochondrial poisons on the neuropathic pain produced by the chemotherapeutic agents, paclitaxel and oxaliplatin. Pain 153, 704–709 (2012).
Doyle, T. et al. Targeting the overproduction of peroxynitrite for the prevention and reversal of paclitaxel-induced neuropathic pain. J. Neurosci. 32, 6149–6160 (2012).
Costa, R. et al. Anti-nociceptive effect of kinin B1 and B2 receptor antagonists on peripheral neuropathy induced by paclitaxel in mice. Br. J. Pharmacol. 164, 681–693 (2011).
Janes, K. et al. The development and maintenance of paclitaxel-induced neuropathic pain require activation of the sphingosine 1-phosphate receptor subtype 1. J. Biol. Chem. 289, 21082–21097 (2014).
Zhang, H., Yoon, S. Y., Zhang, H. & Dougherty, P. M. Evidence that spinal astrocytes but not microglia contribute to the pathogenesis of paclitaxel-induced painful neuropathy. J. Pain 13, 293–303 (2012).
Peters, C. M. et al. Intravenous paclitaxel administration in the rat induces a peripheral sensory neuropathy characterized by macrophage infiltration and injury to sensory neurons and their supporting cells. Exp. Neurol. 203, 42–54 (2007).
Nishida, K. et al. Up-regulation of matrix metalloproteinase-3 in the dorsal root ganglion of rats with paclitaxel-induced neuropathy. Cancer Sci. 99, 1618–1625 (2008).
Leveque, D. & Jehl, F. Molecular pharmacokinetics of catharanthus (vinca) alkaloids. J. Clin. Pharmacol. 47, 579–588 (2007).
Broyl, A. et al. Mechanisms of peripheral neuropathy associated with bortezomib and vincristine in patients with newly diagnosed multiple myeloma: a prospective analysis of data from the HOVON-65/GMMG-HD4 trial. Lancet Oncol. 11, 1057–1065 (2010).
Thibault, K. et al. Structural and molecular alterations of primary afferent fibres in the spinal dorsal horn in vincristine-induced neuropathy in rat. J. Mol. Neurosci. 51, 880–892 (2013).
Thibault, K. et al. Serotonin 5-HT2A receptor involvement and Fos expression at the spinal level in vincristine-induced neuropathy in the rat. Pain 140, 305–322 (2008).
Hansen, N. et al. Serotonin transporter deficiency protects mice from mechanical allodynia and heat hyperalgesia in vincristine neuropathy. Neurosci. Lett. 495, 93–97 (2011).
Kamei, J., Tamura, N. & Saitoh, A. Possible involvement of the spinal nitric oxide/cGMP pathway in vincristine-induced painful neuropathy in mice. Pain 117, 112–120 (2005).
Bujalska, M. & Gumulka, S. W. Effect of cyclooxygenase and nitric oxide synthase inhibitors on vincristine induced hyperalgesia in rats. Pharmacol. Rep. 60, 735–741 (2008).
Old, E. A. et al. Monocytes expressing CX3CR1 orchestrate the development of vincristine-induced pain. J. Clin. Invest. 124, 2023–2036 (2014).
Raymond, E., Faivre, S., Woynarowski, J. M. & Chaney, S. G. Oxaliplatin: mechanism of action and antineoplastic activity. Semin. Oncol. 25, 4–12 (1998).
Gamelin, L. et al. Predictive factors of oxaliplatin neurotoxicity: the involvement of the oxalate outcome pathway. Clin. Cancer Res 13, 6359–6368 (2007).
Sakurai, M. et al. Oxaliplatin-induced neuropathy in the rat: involvement of oxalate in cold hyperalgesia but not mechanical allodynia. Pain 147, 165–174 (2009).
Trevisan, G. et al. Novel therapeutic strategy to prevent chemotherapy-induced persistent sensory neuropathy by TRPA1 blockade. Cancer Res. 73, 3120–3131 (2013).
Descoeur, J. et al. Oxaliplatin-induced cold hypersensitivity is due to remodelling of ion channel expression in nociceptors. EMBO Mol. Med. 3, 266–278 (2011).
Anand, U., Otto, W. R. & Anand, P. Sensitization of capsaicin and icilin responses in oxaliplatin treated adult rat DRG neurons. Mol. Pain 6, 82 (2010).
Sittl, R. et al. Anticancer drug oxaliplatin induces acute cooling-aggravated neuropathy via sodium channel subtype NaV1.6-resurgent and persistent current. Proc. Natl Acad. Sci. USA 109, 6704–6709 (2012).
Deuis, J. R. et al. An animal model of oxaliplatin-induced cold allodynia reveals a crucial role for NaV1.6 in peripheral pain pathways. Pain 154, 1749–1757 (2013).
Scuteri, A. et al. NGF protects dorsal root ganglion neurons from oxaliplatin by modulating JNK/Sapk and ERK1/2. Neurosci. Lett. 486, 141–145 (2010).
Wang, D. & Lippard, S. J. Cellular processing of platinum anticancer drugs. Nat. Rev. Drug Discov. 4, 307–320 (2005).
Di Cesare Mannelli, L. et al. Morphologic features and glial activation in rat oxaliplatin-dependent neuropathic pain. J. Pain 14, 1585–1600 (2013).
Joseph, E. K., Chen, X., Bogen, O. & Levine, J. D. Oxaliplatin acts on IB4-positive nociceptors to induce an oxidative stress-dependent acute painful peripheral neuropathy. J. Pain 9, 463–472 (2008).
Jong, N. N., Nakanishi, T., Liu, J. J., Tamai, I. & McKeage, M. J. Oxaliplatin transport mediated by organic cation/carnitine transporters OCTN1 and OCTN2 in overexpressing human embryonic kidney 293 cells and rat dorsal root ganglion neurons. J. Pharmacol. Exp. Ther. 338, 537–547 (2011).
Sprowl, J. A. et al. Oxaliplatin-induced neurotoxicity is dependent on the organic cation transporter OCT2. Proc. Natl Acad. Sci. USA 110, 11199–11204 (2013).
Massicot, F. et al. P2X7 cell death receptor activation and mitochondrial impairment in oxaliplatin-induced apoptosis and neuronal injury: cellular mechanisms and approach. PLoS ONE 8, e66830 (2013).
Mihara, Y. et al. Involvement of spinal NR2B-containing NMDA receptors in oxaliplatin-induced mechanical allodynia in rats. Mol. Pain 7, 8 (2011).
Warwick, R. A. & Hanani, M. The contribution of satellite glial cells to chemotherapy-induced neuropathic pain. Eur. J. Pain 17, 571–580 (2013).
Yoon, S. Y., Robinson, C. R., Zhang, H. & Dougherty, P. M. Spinal astrocyte gap junctions contribute to oxaliplatin-induced mechanical hypersensitivity. J. Pain 14, 205–214 (2013).
Robinson, C. R., Zhang, H. & Dougherty, P. M. Astrocytes, but not microglia, are activated in oxaliplatin and bortezomib-induced peripheral neuropathy in the rat. Neuroscience 274, 308–317 (2014).
Bast, A. & Haenen, G. R. Ten misconceptions about antioxidants. Trends Pharmacol. Sci. 34, 430–436 (2013).
Kim, H. K., Zhang, Y. P., Gwak, Y. S. & Abdi, S. Phenyl N-tert-butylnitrone, a free radical scavenger, reduces mechanical allodynia in chemotherapy-induced neuropathic pain in rats. Anesthesiology 112, 432–439 (2010).
Argyriou, A. A. et al. Preventing paclitaxel-induced peripheral neuropathy: a phase II trial of vitamin E supplementation. J. Pain Symptom Manage. 32, 237–244 (2006).
Argyriou, A. A. et al. Vitamin E for prophylaxis against chemotherapy-induced neuropathy: a randomized controlled trial. Neurology 64, 26–31 (2005).
Pace, A. et al. Vitamin E neuroprotection for cisplatin neuropathy: a randomized, placebo-controlled trial. Neurology 74, 762–766 (2010).
Kottschade, L. A. et al. The use of vitamin E for the prevention of chemotherapy-induced peripheral neuropathy: results of a randomized phase III clinical trial. Support. Care Cancer 19, 1769–1777 (2011).
Halpner, A. D., Handelman, G. J., Harris, J. M., Belmont, C. A. & Blumberg, J. B. Protection by vitamin C of loss of vitamin E in cultured rat hepatocytes. Arch. Biochem. Biophys. 359, 305–309 (1998).
Lu, R., Kallenborn-Gerhardt, W., Geisslinger, G. & Schmidtko, A. Additive antinociceptive effects of a combination of vitamin C and vitamin E after peripheral nerve injury. PLoS ONE 6, e29240 (2011).
Milla, P. et al. Administration of reduced glutathione in FOLFOX4 adjuvant treatment for colorectal cancer: effect on oxaliplatin pharmacokinetics, Pt-DNA adduct formation, and neurotoxicity. Anticancer Drugs 20, 396–402 (2009).
Planting, A. S. et al. Randomized study of a short course of weekly cisplatin with or without amifostine in advanced head and neck cancer. EORTC Head and Neck Cooperative Group. Ann. Oncol. 10, 693–700 (1999).
Albers, J. W., Chaudhry, V., Cavaletti, G. & Donehower, R. C. Interventions for preventing neuropathy caused by cisplatin and related compounds. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD005228. http://dx.doi.org/10.1002/14651858.CD005228.pub3.
Leal, A. D. et al. North Central Cancer Treatment Group/Alliance trial N08CA-the use of glutathione for prevention of paclitaxel/carboplatin-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled study. Cancer 120, 1890–1897 (2014).
Hershman, D. L. et al. Randomized double-blind placebo-controlled trial of acetyl-L-carnitine for the prevention of taxane-induced neuropathy in women undergoing adjuvant breast cancer therapy. J. Clin. Oncol. 31, 2627–2633 (2013).
Guo, Y. et al. Oral alpha-lipoic acid to prevent chemotherapy-induced peripheral neuropathy: a randomized, double-blind, placebo-controlled trial. Support. Care Cancer 22, 1223–1231 (2014).
Goraca, A. et al. Lipoic acid—biological activity and therapeutic potential. Pharmacol. Rep. 63, 849–858 (2011).
Arrieta, O. et al. Retinoic acid reduces chemotherapy-induced neuropathy in an animal model and patients with lung cancer. Neurology 77, 987–995 (2011).
Yin, S. et al. Retinoids activate the irritant receptor TRPV1 and produce sensory hypersensitivity. J. Clin. Invest. 123, 3941–3951 (2013).
Coriat, R. et al. Treatment of oxaliplatin-induced peripheral neuropathy by intravenous mangafodipir. J. Clin. Invest. 124, 262–272 (2014).
Schmitz, G. & Ecker, J. The opposing effects of n-3 and n-6 fatty acids. Prog. Lipid Res. 47, 147–155 (2008).
Ji, R. R., Xu, Z. Z., Strichartz, G. & Serhan, C. N. Emerging roles of resolvins in the resolution of inflammation and pain. Trends Neurosci. 34, 599–609 (2011).
Serhan, C. N., Chiang, N. & Van Dyke, T. E. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat. Rev. Immunol. 8, 349–361 (2008).
Ghoreishi, Z. et al. Omega-3 fatty acids are protective against paclitaxel-induced peripheral neuropathy: a randomized double-blind placebo controlled trial. BMC Cancer 12, 355 (2012).
Amara, S. Oral glutamine for the prevention of chemotherapy-induced peripheral neuropathy. Ann. Pharmacother. 42, 1481–1485 (2008).
Grolleau, F. et al. A possible explanation for a neurotoxic effect of the anticancer agent oxaliplatin on neuronal voltage-gated sodium channels. J. Neurophysiol. 85, 2293–2297 (2001).
Gamelin, L. et al. Prevention of oxaliplatin-related neurotoxicity by calcium and magnesium infusions: a retrospective study of 161 patients receiving oxaliplatin combined with 5-fluorouracil and leucovorin for advanced colorectal cancer. Clin. Cancer Res. 10, 4055–4061 (2004).
Ishibashi, K., Okada, N., Miyazaki, T., Sano, M. & Ishida, H. Effect of calcium and magnesium on neurotoxicity and blood platinum concentrations in patients receiving mFOLFOX6 therapy: a prospective randomized study. Int. J. Clin. Onc. 15, 82–87 (2010).
Loprinzi, C. L. et al. Phase III randomized, placebo-controlled, double-blind study of intravenous calcium and magnesium to prevent oxaliplatin-induced sensory neurotoxicity (N08CB/Alliance). J. Clin. Oncol. 32, 997–1005 (2014).
Plane, J. M., Shen, Y., Pleasure, D. E. & Deng, W. Prospects for minocycline neuroprotection. Arch. Neurol. 67, 1442–1448 (2010).
Sayin, V. I. et al. Antioxidants accelerate lung cancer progression in mice. Sci. Transl. Med. 6, 221ra15 (2014).
Watson, C. P., Moulin, D., Watt-Watson, J., Gordon, A. & Eisenhoffer, J. Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy. Pain 105, 71–78 (2003).
Sindrup, S. H. et al. Tramadol relieves pain and allodynia in polyneuropathy: a randomised, double-blind, controlled trial. Pain 83, 85–90 (1999).
McNicol, E. D., Midbari, A. & Eisenberg, E. Opioids for neuropathic pain. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD006146. http://dx.doi.org/10.1002/14651858.CD006146.pub2.
Smith, E. M. et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA 309, 1359–1367 (2013).
Weiner, M., Sarantopoulos, C. & Gordon, E. Transdermal buprenorphine controls central neuropathic pain. J. Opioid Manag. 8, 414–415 (2012).
Camu, F., Shi, L. & Vanlersberghe, C. The role of COX-2 inhibitors in pain modulation. Drugs 63 (Suppl. 1), 1–7 (2003).
Hammack, J. E. et al. Phase III evaluation of nortriptyline for alleviation of symptoms of cis-platinum-induced peripheral neuropathy. Pain 98, 195–203 (2002).
Marchand, F. et al. Evidence for an antihyperalgesic effect of venlafaxine in vincristine-induced neuropathy in rat. Brain Res. 980, 117–120 (2003).
Durand, J. P. et al. Efficacy of venlafaxine for the prevention and relief of oxaliplatin-induced acute neurotoxicity: results of EFFOX, a randomized, double-blind, placebo-controlled phase III trial. Ann. Oncol. 23, 200–205 (2012).
Rao, R. D. et al. Efficacy of lamotrigine in the management of chemotherapy-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled trial, N01C3. Cancer 112, 2802–2808 (2008).
Wilson, R. H. et al. Acute oxaliplatin-induced peripheral nerve hyperexcitability. J. Clin. Oncol. 20, 1767–1774 (2002).
Saif, M. W., Syrigos, K., Kaley, K. & Isufi, I. Role of pregabalin in treatment of oxaliplatin-induced sensory neuropathy. Anticancer Res. 30, 2927–2933 (2010).
Argyriou, A. A. et al. Efficacy of oxcarbazepine for prophylaxis against cumulative oxaliplatin-induced neuropathy. Neurology 67, 2253–2255 (2006).
Attal, N. et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur. J. Neurol. 17, 1113–e88 (2010).
Mou, J. et al. Efficacy of Qutenza® (capsaicin) 8% patch for neuropathic pain: a meta-analysis of the Qutenza Clinical Trials Database. Pain 154, 1632–1639 (2013).
Maihofner, C. G. & Heskamp, M. L. Treatment of peripheral neuropathic pain by topical capsaicin: Impact of pre-existing pain in the QUEPP-study. Eur. J. Pain 18, 671–679 (2014).
Barton, D. L. et al. A double-blind, placebo-controlled trial of a topical treatment for chemotherapy-induced peripheral neuropathy: NCCTG trial N06CA. Support. Care Cancer 19, 833–841 (2011).
Gewandter, J. S. et al. A phase III randomized, placebo-controlled study of topical amitriptyline and ketamine for chemotherapy-induced peripheral neuropathy (CIPN): a University of Rochester CCOP study of 462 cancer survivors. Support. Care Cancer 22, 1807–1814 (2014).
Kalliomaki, J. et al. A randomized, double-blind, placebo-controlled trial of a chemokine receptor 2 (CCR2) antagonist in posttraumatic neuralgia. Pain 154, 761–767 (2013).
Anand, P. et al. Clinical trial of the p38 MAP kinase inhibitor dilmapimod in neuropathic pain following nerve injury. Eur. J. Pain 15, 1040–1048 (2011).
Santos, E., Shaunak, S., Renowden, S. & Scolding, N. J. Treatment of refractory neurosarcoidosis with infliximab. J. Neurol. Neurosurg. Psychiatry 81, 241–246 (2010).
Dinarello, C. A., Simon, A. & van der Meer, J. W. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat. Rev. Drug Discov. 11, 633–652 (2012).
Alten, R. & Maleitzke, T. Tocilizumab: a novel humanized anti-interleukin 6 (IL-6) receptor antibody for the treatment of patients with non-RA systemic, inflammatory rheumatic diseases. Ann. Med. 45, 357–363 (2013).
Rasmussen, L. & Arvin, A. Chemotherapy-induced immunosuppression. Environ. Health Perspect. 43, 21–25 (1982).
Delforge, M. et al. Treatment-related peripheral neuropathy in multiple myeloma: the challenge continues. Lancet Oncol. 11, 1086–1095 (2010).
Chaudhry, V., Cornblath, D. R., Polydefkis, M., Ferguson, A. & Borrello, I. Characteristics of bortezomib- and thalidomide-induced peripheral neuropathy. J. Peripher. Nerv. Syst. 13, 275–282 (2008).
Chaudhry, V. et al. Thalidomide-induced neuropathy. Neurology 59, 1872–1875 (2002).
Laaksonen, S., Remes, K., Koskela, K., Voipio-Pulkki, L. M. & Falck, B. Thalidomide therapy and polyneuropathy in myeloma patients. Electromyogr. Clin. Neurophysiol. 45, 75–86 (2005).
Argyriou, A. A., Iconomou, G. & Kalofonos, H. P. Bortezomib-induced peripheral neuropathy in multiple myeloma: a comprehensive review of the literature. Blood 112, 1593–1599 (2008).
Mo, M., Erdelyi, I., Szigeti-Buck, K., Benbow, J. H. & Ehrlich, B. E. Prevention of paclitaxel-induced peripheral neuropathy by lithium pretreatment. FASEB J. 26, 4696–4709 (2012).
Ledeboer, A., Hutchinson, M. R., Watkins, L. R. & Johnson, K. W. Ibudilast (AV-411). A new class therapeutic candidate for neuropathic pain and opioid withdrawal syndromes. Expert Opin. Investig. Drugs 16, 935–950 (2007).
Cata, J. P., Weng, H. R. & Dougherty, P. M. The effects of thalidomide and minocycline on taxol-induced hyperalgesia in rats. Brain Res. 1229, 100–110 (2008).
Tesfaye, S. et al. Duloxetine and pregabalin: high-dose monotherapy or their combination? The “COMBO-DN study”—a multinational, randomized, double-blind, parallel-group study in patients with diabetic peripheral neuropathic pain. Pain 154, 2616–2625 (2013).
Xu, Z. Z. et al. Resolvins RvE1 and RvD1 attenuate inflammatory pain via central and peripheral actions. Nat. Med. 16, 592–597 (2010).
Tsujino, H. et al. Activating transcription factor 3 (ATF3) induction by axotomy in sensory and motoneurons: A novel neuronal marker of nerve injury. Mol. Cellular Neurosci. 15, 170–182 (2000).
Serhan, C. N. et al. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 26, 1755–1765 (2012).
Okubo, K. et al. Inhibition of T-type calcium channels and hydrogen sulfide-forming enzyme reverses paclitaxel-evoked neuropathic hyperalgesia in rats. Neuroscience 188, 148–156 (2011).
Schmidtko, A., Lotsch, J., Freynhagen, R. & Geisslinger, G. Ziconotide for treatment of severe chronic pain. Lancet 375, 1569–1577 (2010).
Kolosov, A., Goodchild, C. S. & Cooke, I. CNSB004 (leconotide) causes antihyperalgesia without side effects when given intravenously: a comparison with ziconotide in a rat model of diabetic neuropathic pain. Pain Med. 11, 262–273 (2010).
Emery, E. C., Young, G. T., Berrocoso, E. M., Chen, L. & McNaughton, P. A. HCN2 ion channels play a central role in inflammatory and neuropathic pain. Science 333, 1462–1466 (2011).
Hartrick, C. T. & Rodriguez Hernandez, J. R. Tapentadol for pain: a treatment evaluation. Expert Opin. Pharmacother. 13, 283–286 (2012).
Pascual, D., Goicoechea, C., Suardiaz, M. & Martin, M. I. A cannabinoid agonist, WIN 55,212-2, reduces neuropathic nociception induced by paclitaxel in rats. Pain 118, 23–34 (2005).
Deng, L. et al. The maintenance of cisplatin- and paclitaxel-induced mechanical and cold allodynia is suppressed by cannabinoid CB2 receptor activation and independent of CXCR4 signaling in models of chemotherapy-induced peripheral neuropathy. Mol. Pain 8, 71 (2012).
Deng, L. et al. Chronic cannabinoid receptor 2 activation reverses paclitaxel neuropathy without tolerance or cannabinoid receptor 1-dependent withdrawal. Biol. Psychiatry http://dx.doi.org/10.1016/j.biopsych.2014.04.009.
Guindon, J., Lai, Y., Takacs, S. M., Bradshaw, H. B. & Hohmann, A. G. Alterations in endocannabinoid tone following chemotherapy-induced peripheral neuropathy: effects of endocannabinoid deactivation inhibitors targeting fatty-acid amide hydrolase and monoacylglycerol lipase in comparison to reference analgesics following cisplatin treatment. Pharmacol. Res. 67, 94–109 (2013).
Lynch, M. E., Cesar-Rittenberg, P. & Hohmann, A. G. A double-blind, placebo-controlled, crossover pilot trial with extension using an oral mucosal cannabinoid extract for treatment of chemotherapy-induced neuropathic pain. J. Pain Symptom Manage. 47, 166–173 (2014).
Ward, S. J. et al. Cannabidiol inhibits paclitaxel-induced neuropathic pain through 5-HT1A receptors without diminishing nervous system function or chemotherapy efficacy. Br. J. Pharmacol. 171, 636–45 (2014).
Caprioli, A. et al. The novel reversible fatty acid amide hydrolase inhibitor ST4070 increases endocannabinoid brain levels and counteracts neuropathic pain in different animal models. J. Pharmacol. Exp. Ther. 342, 188–195 (2012).
Rehm, S. E. et al. A cross-sectional survey of 3035 patients with fibromyalgia: subgroups of patients with typical comorbidities and sensory symptom profiles. Rheumatology (Oxford) 49, 1146–1152 (2010).
Baron, R., Tolle, T. R., Gockel, U., Brosz, M. & Freynhagen, R. A cross-sectional cohort survey in 2100 patients with painful diabetic neuropathy and postherpetic neuralgia: differences in demographic data and sensory symptoms. Pain 146, 34–40 (2009).
Baron, R., Forster, M. & Binder, A. Subgrouping of patients with neuropathic pain according to pain-related sensory abnormalities: a first step to a stratified treatment approach. Lancet Neurol. 11, 999–1005 (2012).
Ji, R. R., Xu, Z. Z. & Gao, Y. J. Emerging targets in neuroinflammation-driven chronic pain. Nat. Rev. Drug Discov. 13, 533–548 (2014).
Tatsushima, Y. et al. Involvement of substance P in peripheral neuropathy induced by paclitaxel but not oxaliplatin. J. Pharmacol. Exp. Ther. 337, 226–235 (2011).
Acknowledgements
M.S., K.S. and G.G. have received funding from the Deutsche Forschungsgemeinschaft (German Research Association; grants SCHO817 and SFB1039 TP A08, A09 and Z01). R.B. and G.G. are part of the Europain Collaboration, which has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no. 115007, resources of which are composed of financial contribution from the European Union's Seventh Framework Programme (FP7/2007–2013) and the kind contribution of companies involved in the European Federation of Pharmaceutical Industries and Associations. G.G. has also received funding from the LOEWE-Programme of the State of Hessia (Anwedungsorientierte Arzneimittelforschung).
Author information
Authors and Affiliations
Contributions
M.S. searched the published work, discussed the content, wrote, edited and revised the article, designed all figures and assembled all tables, R.B. searched the literature, discussed the content, and wrote, edited and revised the article. K.S. and G.G. discussed the content, and wrote, edited and revised the article, figures and tables. All authors read and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
R.B. and G.G. are members of the IMI (Innovative Medicine Initiative of the EU) EuroPain collaboration, in which the following industry members are represented: Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Esteve, Gruenenthal, Pfizer, UCB Pharma and Sanofi Aventis. G.G. has received honoraria as a speaker from Gruenenthal, Mundipharma and Pfizer. He is a consultant for Abbvie. He has received research funding in the form of a grant from Mundipharma. R.B. has received honoraria as a speaker from Astellas, Bayer-Schering, Boehringer Ingelheim, Desitin, Eisai, Eli Lilly, Genzyme, Gruenenthal, Medtronic, Mundipharma, MSD, Pfizer, Sanofi Pasteur and Teva Pharma. He is also a consultant for Abbvie, Allergan, Astellas, AstraZeneca, Biogen Idec, Boehringer Ingelheim, Bristol-Myers Squibb, Eisai, Eli Lilly, Genzyme, Gruenenthal, Medtronic, Merck, Mundipharma, Novartis, Pfizer and Sanofi Pasteur. He has received research funding in the form of grants from Genzyme, Gruenenthal and Pfizer. M.S. and K.S. declare no competing interests.
Rights and permissions
About this article
Cite this article
Sisignano, M., Baron, R., Scholich, K. et al. Mechanism-based treatment for chemotherapy-induced peripheral neuropathic pain. Nat Rev Neurol 10, 694–707 (2014). https://doi.org/10.1038/nrneurol.2014.211
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2014.211
This article is cited by
-
Ropivacaine-loaded hydrogels for prolonged relief of chemotherapy-induced peripheral neuropathic pain and potentiated chemotherapy
Journal of Nanobiotechnology (2023)
-
Kinin B1 and B2 receptors mediate cancer pain associated with both the tumor and oncology therapy using aromatase inhibitors
Scientific Reports (2023)
-
Cebranopadol for the Treatment of Chronic Pain
Current Pain and Headache Reports (2023)
-
Daidzein attenuated paclitaxel-induced neuropathic pain via the down-regulation of TRPV1/P2Y and up-regulation of Nrf2/HO-1 signaling
Inflammopharmacology (2023)
-
Wnt3a/YTHDF1 Regulated Oxaliplatin-Induced Neuropathic Pain Via TNF-α/IL-18 Expression in the Spinal Cord
Cellular and Molecular Neurobiology (2023)