Key Points
-
A useful clinical biomarker must have an exact and well-defined context of use, generally linked to a therapeutic consequence, and every new biomarker identified must be validated in independent studies
-
Proteomic studies have detected initial sets of biomarkers that have demonstrated potential in the context of kidney disease, but they have not yet been fully integrated into clinical use
-
High-dimensional classifiers based on multiple, well-defined biomarkers generally outperform individual markers, because such classifiers account for disease complexity and molecular heterogeneity
-
Guidance from professional, clinical and scientific societies on the clinical use of biomarkers and their development would substantially improve clinical biomarker research
-
The lack of appropriate samples in sufficient numbers is a major barrier to the further development of effective proteomic biomarkers; publicly funded biobanks could substantially improve this situation
-
Evaluation of proteomics data employing systems biology approaches has the potential to yield information that cannot be established using proteomics alone
Abstract
Proteomic biomarkers offer the hope of improving the management of patients with kidney diseases by enabling more accurate and earlier detection of renal pathology than is possible with currently available biomarkers, serum creatinine and urinary albumin. In addition, proteomic biomarkers could also be useful to define the most suitable therapeutic targets in a given patient or disease setting. This Review describes the current status of proteomic and protein biomarkers in the context of kidney diseases. The valuable lessons learned from early clinical studies of potential proteomic biomarkers in kidney disease are presented to give context to the newly identified biomarkers, which have potential for actual clinical implementation. This article also includes an overview of protein-based biomarker candidates that are undergoing development for use in nephrology, focusing on those with the greatest potential for clinical implementation. Relevant issues and problems associated with the discovery, validation and clinical application of proteomic biomarkers are discussed, along with suggestions for solutions that might help to guide the design of future proteomic studies. These improvements might remove some of the current obstacles to the utilization of proteomic biomarkers, with potentially beneficial results.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Biomarkers definitions working group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 69, 89 (2001).
Stevens, L. A. & Levey, A. S. Measured GFR as a confirmatory test for estimated GFR. J. Am. Soc. Nephrol. 20, 2305–2313 (2009).
Gross, J. L. et al., Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 28, 164–176 (2005).
Naresh, C. N. et al. Day-to-day variability in spot urine albumin-creatinine ratio. Am. J. Kidney Dis. 62, 1095–1101 (2013).
Mischak, H., Vlahou, A. & Ioannidis, J. P. Technical aspects and inter-laboratory variability in native peptide profiling: the CE-MS experience. Clin. Biochem. 46, 432–443 (2013).
Perkins, B. A. et al. In patients with type 1 diabetes and new-onset microalbuminuria the development of advanced chronic kidney disease may not require progression to proteinuria. Kidney Int. 77, 57–64 (2010).
Zachwieja, J. et al. Normal-range albuminuria does not exclude nephropathy in diabetic children. Pediatr. Nephrol. 25, 1445–1451 (2010).
van der Tol, A. et al. Towards a rational screening strategy for albuminuria: results from the unreferred renal insufficiency trial. PLoS ONE 5, e13328 (2010).
Halbesma, N. et al. Macroalbuminuria is a better risk marker than low estimated GFR to identify individuals at risk for accelerated GFR loss in population screening. J. Am. Soc. Nephrol. 17, 2582–2590 (2006).
El Nahas, A. M. & Bello, A. K. Chronic kidney disease: the global challenge. Lancet 365, 331–340 (2005).
Kronenberg, F. Emerging risk factors and markers of chronic kidney disease progression. Nat. Rev. Nephrol. 5, 677–689 (2009).
Fassett, R. G. et al. Biomarkers in chronic kidney disease: a review. Kidney Int. 80, 806–821 (2011).
Hojs, R. et al. Serum cystatin C as an endogenous marker of renal function in patients with mild to moderate impairment of kidney function. Nephrol. Dial. Transplant. 21, 1855–1862 (2006).
O'Riordan, S. E. et al. Cystatin C improves the detection of mild renal dysfunction in older patients. Ann. Clin. Biochem. 40, 648–655 (2003).
Madero, M. Sarnak, M. J. & Stevens, L. A. Serum cystatin C as a marker of glomerular filtration rate. Curr. Opin. Nephrol. Hypertens. 15, 610–616 (2006).
Grubb, A. et al. A cystatin C-based formula without anthropometric variables estimates glomerular filtration rate better than creatinine clearance using the Cockcroft-Gault formula. Scand. J. Clin. Lab. Invest. 65, 153–162 (2005).
Conti, M. et al. Urinary cystatin C as a specific marker of tubular dysfunction. Clin. Chem. Lab. Med. 44, 288–291 (2006).
Menon, V. et al. Cystatin C as a risk factor for outcomes in chronic kidney disease. Ann. Intern. Med. 147, 19–27 (2007).
Astor, B. C. et al. Novel markers of kidney function as predictors of ESRD, cardiovascular disease, and mortality in the general population. Am. J. Kidney Dis. 59, 653–662 (2012).
Peralta, C. A. et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA 305, 1545–1552 (2011).
Peralta, C. A. et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications. J. Am. Soc. Nephrol. 22, 147–155 (2011).
Jeon, Y. K. et al. Cystatin C as an early biomarker of nephropathy in patients with type 2 diabetes. J. Korean Med. Sci. 26, 258–263 (2011).
Malyszko, J. et al. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in non-diabetic patients with stage 2–4 chronic kidney disease. Ren. Fail. 30, 625–628 (2008).
Smith, E. R. et al. Urinary neutrophil gelatinase-associated lipocalin may aid prediction of renal decline in patients with non-proteinuric Stages 3 and 4 chronic kidney disease (CKD). Nephrol. Dial. Transplant. 28, 1569–1579 (2013).
Bolignano, D. et al. Neutrophil gelatinase-associated lipocalin reflects the severity of renal impairment in subjects affected by chronic kidney disease. Kidney Blood Press. Res. 31, 255–258 (2008).
Bolignano, D. et al. Neutrophil gelatinase-associated lipocalin in patients with autosomal-dominant polycystic kidney disease. Am. J. Nephrol. 27, 373–378 (2007).
Makris, K. et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) as an early marker of acute kidney injury in critically ill multiple trauma patients. Clin. Chem. Lab. Med. 47, 79–82 (2009).
Zappitelli, M. et al. Urine neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in critically ill children: a prospective cohort study. Crit. Care 11, R84 (2007).
Bolignano, D. et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a marker of kidney damage. Am. J. Kidney Dis. 52, 595–605 (2008).
Haase, M. et al. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: a systematic review and meta-analysis. Am. J. Kidney Dis. 54, 1012–1024 (2009).
Niemann, C. U. et al. Acute kidney injury during liver transplantation as determined by neutrophil gelatinase-associated lipocalin. Liver Transpl. 15, 1852–1860 (2009).
Viau, A. et al. Lipocalin 2 is essential for chronic kidney disease progression in mice and humans. J. Clin. Invest. 120, 4065–4076 (2010).
Mitsnefes, M. M. et al. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in children with chronic kidney disease. Pediatr. Nephrol. 22, 101–108 (2007).
Bolignano, D. et al. Neutrophil gelatinase-associated lipocalin (NGAL) and progression of chronic kidney disease. Clin. J. Am. Soc. Nephrol. 4, 337–344 (2009).
Bolignano, D., Coppolino, G., Lacquaniti, A. & Buemi, M. From kidney to cardiovascular diseases: NGAL as a biomarker beyond the confines of nephrology. Eur. J. Clin. Invest. 40, 273–276 (2010).
Bolignano, D. et al. Neutrophil gelatinase-associated lipocalin (NGAL) in human neoplasias: a new protein enters the scene. Cancer Lett. 288, 10–16 (2010).
Parikh, C. R., Lu, J. C., Coca, S. G. & Devarajan, P. Tubular proteinuria in acute kidney injury: a critical evaluation of current status and future promise. Ann. Clin. Biochem. 47, 301–312 (2010).
Vaidya, V. S. et al. Regression of microalbuminuria in type 1 diabetes is associated with lower levels of urinary tubular injury biomarkers, kidney injury molecule-1, and N-acetyl-beta-D-glucosaminidase. Kidney Int. 79, 464–470 (2011).
Nauta, F. L. et al. Glomerular and tubular damage markers are elevated in patients with diabetes. Diabetes Care. 34, 975–981 (2011).
Washburn, K. K. et al. Urinary interleukin-18 is an acute kidney injury biomarker in critically ill children. Nephrol. Dial. Transplant. 23, 566–572 (2008).
Wagener, G. et al. Urinary neutrophil gelatinase-associated lipocalin and acute kidney injury after cardiac surgery. Am. J. Kidney Dis. 52, 425–433 (2008).
Metzger, J. et al. Urinary excretion of twenty peptides forms an early and accurate diagnostic pattern of acute kidney injury. Kidney Int. 78, 1252–1262 (2010).
Siew, E. D. et al. Urine neutrophil gelatinase-associated lipocalin moderately predicts acute kidney injury in critically ill adults. J. Am. Soc. Nephrol. 20, 1823–1832 (2009).
Haase, M. et al., Urinary interleukin-18 does not predict acute kidney injury after adult cardiac surgery: a prospective observational cohort study. Crit. Care 12, R96 (2008).
Martensson, J. et al. Neutrophil gelatinase-associated lipocalin in adult septic patients with and without acute kidney injury. Intensive Care Med. 36, 1333–1340 (2010).
Shlipak, M. G. et al. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation 107, 87–92 (2003).
Oberg, B. P. et al. Increased prevalence of oxidant stress and inflammation in patients with moderate to severe chronic kidney disease. Kidney Int. 65, 1009–1016 (2004).
Tong, M. et al. Plasma pentraxin 3 in patients with chronic kidney disease: associations with renal function, protein-energy wasting, cardiovascular disease, and mortality. Clin. J. Am. Soc. Nephrol. 2, 889–897 (2007).
Axelsson, J. et al. Elevated resistin levels in chronic kidney disease are associated with decreased glomerular filtration rate and inflammation, but not with insulin resistance. Kidney Int. 69, 596–604 (2006).
Fried, L. et al. Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J. Am. Soc. Nephrol. 15, 3184–3191 (2004).
Tonelli, M. et al. Biomarkers of inflammation and progression of chronic kidney disease. Kidney Int. 68, 237–245 (2005).
Menon, V. et al. Relationship between C-reactive protein, albumin, and cardiovascular disease in patients with chronic kidney disease. Am. J. Kidney Dis. 42, 44–52 (2003).
Orenes-Pinero, E. et al. β-Trace protein: from GFR marker to cardiovascular risk predictor. Clin. J. Am. Soc. Nephrol. 8, 873–881 (2013).
Lewis, J. R. et al. Elevated osteoprotegerin predicts declining renal function in elderly women: a 10-year prospective cohort study. Am. J. Nephrol. 39, 66–74 (2014).
Saulnier, P. J. et al. Association of serum concentration of TNFR1 with all-cause mortality in patients with type 2 diabetes and chronic kidney disease: follow- up of the SURDIAGENE cohort. Diabetes Care 37, 1425–1431 (2014).
Desjardins, L. et al. FGF23 is independently associated with vascular calcification but not bone mineral density in patients at various CKD stages. Osteoporos. Int. 23, 2017–2025 (2012).
Shimamura, Y. et al. Serum levels of soluble secreted α-Klotho are decreased in the early stages of chronic kidney disease, making it a probable novel biomarker for early diagnosis. Clin. Exp. Nephrol. 16, 722–729 (2012).
Devaraj, S., Syed, B., Chien, A. & Jialal, I. Validation of an immunoassay for soluble klotho protein decreased levels in diabetes and increased levels in chronic kidney disease. Am. J. Clin. Pathol. 137, 479–485 (2012).
Lundberg, S. et al. FGF23, Albuminuria, and disease progression in patients with chronic IgA nephropathy. Clin. J. Am. Soc. Nephrol. 7, 727–734 (2012).
Kim, H. R. et al. Circulating α-klotho levels in CKD and relationship to progression. Am. J. Kidney Dis. 61, 899–909 (2013).
Targher, G., Kendrick, J., Smits, G. & Chonchol, M. Relationship between serum gamma-glutamyltransferase and chronic kidney disease in the United States adult population. Findings from the National Health and Nutrition Examination Survey 2001–2006 Nutr. Metab. Cardiovasc. Dis. 20, 583–590 (2010).
Dieplinger, B. et al. Pro-A-type natriuretic peptide and pro-adrenomedullin predict progression of chronic kidney disease: the MMKD Study. Kidney Int. 75, 408–414 (2009).
Yilmaz, M. I. et al. Serum visfatin concentration and endothelial dysfunction in chronic kidney disease, Nephrol. Dial. Transplant. 23, 959–965 (2008).
Axelsson, J. et al. Circulating levels of visfatin/pre-B-cell colony-enhancing factor 1 in relation to genotype, GFR, body composition, and survival in patients with CKD. Am. J. Kidney Dis. 49, 237–244 (2007).
Lin, J., Hu, F. B. & Curhan, G. Serum adiponectin and renal dysfunction in men with type 2 diabetes. Diabetes Care 30, 239–244 (2007).
Bruchfeld, A. et al. High Mobility Group Box Protein-1 correlates with renal function in chronic kidney disease (CKD). Mol. Med. 14, 109–115 (2008).
Kamijo, A. et al. Clinical evaluation of urinary excretion of liver-type fatty acid-binding protein as a marker for the monitoring of chronic kidney disease: a multicenter trial. J. Lab. Clin. Med. 145, 125–133 (2005).
Nakamura, T. et al. Urinary excretion of liver-type fatty acid-binding protein in contrast medium-induced nephropathy. Am. J. Kidney Dis. 47, 439–444 (2006).
Ferguson, M. A. et al. Urinary liver-type fatty acid-binding protein predicts adverse outcomes in acute kidney injury. Kidney Int. 77, 708–714 (2010).
Vickery, S. et al. B-type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: relationship to renal function and left ventricular hypertrophy. Am. J. Kidney Dis. 46, 610–620 (2005).
Hutchison, C. A. et al. Quantitative assessment of serum and urinary polyclonal free light chains in patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 3, 1684–1690 (2008).
Yamamoto, T. et al. Urinary angiotensinogen as a marker of intrarenal angiotensin II activity associated with deterioration of renal function in patients with chronic kidney disease. J. Am. Soc. Nephrol. 18, 1558–1565 (2007).
Zhao, N. et al. The level of galactose-deficient IgA1 in the sera of patients with IgA nephropathy is associated with disease progression. Kidney Int. 82, 790–796 (2012).
Beisswenger, P. J. et al. Early progression of diabetic nephropathy correlates with methylglyoxal-derived advanced glycation end products. Diabetes Care 36, 3234–3239 (2013).
Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 69, 89–95 (2001).
Otu, H. H. et al. Prediction of diabetic nephropathy using urine proteomic profiling 10 years prior to development of nephropathy. Diabetes Care 30, 638–643 (2007).
Schaub, S. et al. Proteomic-based identification of cleaved urinary β2-microglobulin as a potential marker for acute tubular injury in renal allografts. Am. J. Transplant. 5, 729–738 (2005).
Wittke, S. et al. Detection of acute tubulointerstitial rejection by proteomic analysis of urinary samples in renal transplant recipients. Am. J. Transplant. 5, 2479–2488 (2005).
Rossing, K. et al. Impact of diabetic nephropathy and angiotensin II receptor blockade on urinary polypeptide patterns. Kidney Int. 68, 193–205 (2005).
Weissinger, E. M. et al. Proteomic patterns established with capillary electrophoresis and mass spectrometry for diagnostic purposes. Kidney Int. 65, 2426–2434 (2004).
Mischak, H. et al. Recommendations for biomarker identification and qualification in clinical proteomics. Sci. Transl. Med. 2, 46ps42 (2010).
Mischak, H. et al. Clinical proteomics: a need to define the field and to begin to set adequate standards. Proteomics Clin. Appl. 1, 148–156 (2007).
Mischak, H., Vlahou, A., Righetti, P. G. & Calvete, J. J. Putting value in biomarker research and reporting. J. Proteomics 96, A1–A3 (2014).
Manolis, E., Vamvakas, S. & Isaac, M. New pathway for qualification of novel methodologies in the European medicines agency. Proteomics Clin. Appl. 5, 248–255 (2011).
Vitzthum, F., Behrens, F., Anderson, N. L. & Shaw, J. H. Proteomics: from basic research to diagnostic application. A review of requirements & needs, J. Proteome. Res. 4, 1086–1097 (2005).
Petricoin, E. F. et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet 359, 572–577 (2002).
Baggerly, K. A., Morris, J. S. & Coombes, K. R. Reproducibility of SELDI-TOF protein patterns in serum: comparing datasets from different experiments. Bioinformatics 20, 777–785 (2002).
Sorace, J. M. & Zhan, M. A data review and re-assessment of ovarian cancer serum proteomic profiling. BMC Bioinformatics 4, 24 (2003).
Check, E. Running before we can walk. Nature 429, 496–497 (2004).
Dakna, M. et al. Addressing the challenge of defining valid proteomic biomarkers and classifiers. BMC Bioinformatics 11, 594 (2010).
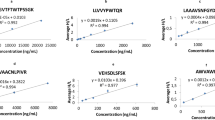
Jantos-Siwy, J. et al. Quantitative urinary proteome analysis for biomarker evaluation in chronic kidney disease. J. Proteome. Res. 8, 268–281 (2009).
Kistler, A. D. et al. Identification of a unique urinary biomarker profile in patients with autosomal dominant polycystic kidney disease. Kidney Int. 76, 89–96 (2009).
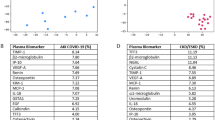
Snell-Bergeon, J. K. et al. Evaluation of urinary biomarkers for coronary artery disease, diabetes, and diabetic kidney disease. Diabetes Technol. Ther. 11, 1–9 (2009).
Rossing, K. et al. Urinary proteomics in diabetes and CKD. J. Am. Soc. Nephrol. 19, 1283–1290 (2008).
Haubitz, M. et al. Identification and validation of urinary biomarkers for differential diagnosis and evaluation of therapeutic intervention in ANCA associated vasculitis. Mol. Cell. Proteomics 8, 2296–2307 (2009).
Sharma, K. et al. Two-dimensional fluorescence difference gel electrophoresis analysis of the urine proteome in human diabetic nephropathy. Proteomics 5, 2648–2655 (2005).
Zürbig, P. et al. Biomarker discovery by CE-MS enables sequence analysis via MS/MS with platform-independent separation. Electrophoresis 27, 2111–2125 (2006).
Merchant, M. L. et al. Urinary peptidome may predict renal function decline in type 1 diabetes and microalbuminuria. J. Am. Soc. Nephrol. 20, 2065–2074 (2009).
Good, D. M. et al. Naturally occurring human urinary peptides for use in diagnosis of chronic kidney disease. Mol. Cell. Proteomics 9, 2424–2437 (2010).
Molin, L. et al. A comparison between MALDI-MS and CE-MS data for biomarker assessment in chronic kidney diseases. J. Proteomics 75, 5888–5897 (2012).
Lapolla, A. et al. A further investigation on a MALDI-based method for evaluation of markers of renal damage. J. Mass Spectrom. 44, 1754–1760 (2009).
Zurbig, P. et al. Urinary proteomics for early diagnosis in diabetic nephropathy. Diabetes 61, 3304–3313 (2012).
Schanstra, J. P. et al. Diagnosis and prediction of CKD progression by assessment of urinary peptides. J. Am. Soc. Nephrol. http://dx.doi.org/10.1681/ASN.2014050423.
Gu, Y. M. et al. The urinary proteome as correlate and predictor of renal function in a population study. Nephrol. Dial. Transplant. 29, 2260–2268 (2014).
Argiles, A. et al. CKD273, a new proteomics classifier assessing CKD and its prognosis. PLoS ONE 8, e62837 (2013).
Roscioni, S. S. et al. A urinary peptide biomarker set predicts worsening of albuminuria in type 2 diabetes mellitus. Diabetologia 56, 259–267 (2013).
Andersen, S. et al. Urinary proteome analysis enables assessment of renoprotective treatment in type 2 diabetic patients with microalbuminuria. BMC Nephrol. 11, 29 (2010).
Nkuipou-Kenfack, E. et al., Assessment of metabolomic and proteomic biomarkers in detection and prognosis of progression of renal function in chronic kidney disease. PLoS ONE 9, e96955 (2014).
Siwy, J. et al. Multicentre prospective validation of a urinary peptidome-based classifier for the diagnosis of type 2 diabetic nephropathy. Nephrol. Dial. Transplant. 29, 1563–1570 (2014).
Alkhalaf, A. et al. Multicentric validation of proteomic biomarkers in urine specific for diabetic nephropathy. PLoS ONE 5, e13421 (2010).
Rossing, K. et al. The urinary proteome in diabetes and diabetes-associated complications: new ways to assess disease progression and evaluate therapy. Proteomics Clin. Appl. 2, 997–1007 (2008).
Zurbig, P. et al. The human urinary proteome reveals high similarity between kidney aging and chronic kidney disease. Proteomics 9, 2108–2117 (2009).
Anderson, N. L. & Anderson, N. G. The human plasma proteome: history, character, and diagnostic prospects. Mol. Cell Proteomics 1, 845–867 (2002).
Kolch, W., Neususs, C., Pelzing, M. & Mischak, H. Capillary electrophoresis-mass spectrometry as a powerful tool in clinical diagnosis and biomarker discovery. Mass Spectrom. Rev. 24, 959–977 (2005).
Thongboonkerd, V. & Malasit, P. Renal and urinary proteomics: current applications and challenges. Proteomics 5, 1033–1042 (2005).
Waikar, S. S., Sabbisetti, V. S. & Bonventre, J. V. Normalization of urinary biomarkers to creatinine during changes in glomerular filtration rate. Kidney Int. 78, 486–494 (2010).
Siwy, J. et al. Evaluation of the Zucker Diabetic Fatty (ZDF) rat as a model for human disease based on urinary peptidomic profiles. PLoS ONE 7, e51334 (2012).
Dominiczak, A. F. et al. Systems biology to battle vascular disease. Nephrol. Dial. Transplant. 25, 1019–1022 (2010).
Molina, F. et al. Systems biology: opening new avenues in clinical research. Nephrol. Dial. Transplant. 25, 1015–1018 (2010).
Fliser, D. et al. Advances in urinary proteome analysis and biomarker discovery. J. Am. Soc. Nephrol. 18, 1057–1071 (2007).
Dakna, M. et al. Technical, bioinformatical and statistical aspects of liquid chromatography-mass spectrometry (LC-MS) and capillary electrophoresis-mass spectrometry (CE-MS) based clinical proteomics: a critical assessment. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 877, 1250–1258 (2009).
Kolch, W., Mischak, H. & Pitt, A. R. The molecular make-up of a tumour: proteomics in cancer research. Clin. Sci. (Lond.) 108, 369–383 (2005).
Mullen, W. et al. Performance of different separation methods interfaced in the same MS-reflection TOF detector: A comparison of performance between CE versus HPLC for biomarker analysis. Electrophoresis 33, 567–574 (2012).
Klein, J., Papadopoulos, T., Mischak, H. & Mullen, W. Comparison of CE-MS/MS and LC-MS/MS sequencing demonstrates significant complementarity in natural peptide identification. Electrophoresis 35, 1060–1064 (2014).
Wisniewski, J. R., Zougman, A., Nagaraj, N. & Mann, M. Universal sample preparation method for proteome analysis. Nat. Methods 6, 359–362 (2009).
Neiman, M. et al. Plasma profiling reveals human fibulin-1 as candidate marker for renal impairment. J. Proteome Res. 10, 4925–4934 (2011).
Gold, L. et al. Aptamer-based multiplexed proteomic technology for biomarker discovery. PLoS ONE 5, e15004 (2010).
Jin, Y. et al. A systems approach identifies HIPK2 as a key regulator of kidney fibrosis. Nat. Med. 18, 580–588 (2012).
He, J. C., Chuang, P. Y., Ma'ayan, A. & Iyengar, R. Systems biology of kidney diseases, Kidney Int. 81, 22–39 (2012).
Keller, B. J., Martini, S., Sedor, J. R. & Kretzler, M. A systems view of genetics in chronic kidney disease. Kidney Int. 81, 14–21 (2012).
Fechete, R. et al. Mapping of molecular pathways, biomarkers and drug targets for diabetic nephropathy. Proteomics Clin. Appl. 5, 354–366 (2011).
Husi, H. et al. A combinatorial approach of proteomics and systems biology in unravelling the mechanisms of acute kidney injury (AKI): involvement of NMDA receptor GRIN1 in murine AKI. BMC Syst. Biol. 7, 110 (2013).
Klein, J. et al. Proteasix: a tool for automated and large-scale prediction of proteases involved in naturally-occurring peptide generation. Proteomics 13, 1077–1082 (2013).
Acknowledgements
The authors' research is supported in part by the European Commission Seventh Framework Programme (FP7) projects Clinical and System–Omics for Identification of the Molecular Determinants of Established Chronic Kidney Disease (iMODE-CKD, PEOPLE-ITN-GA-2013-608332), Markers for Sub-Clinical Cardiovascular Risk Assessment (EU-MASCARA, HEALTH-2011 278,249), Systems Biology to Identify Molecular Targets for Vascular Disease Treatment (SysVasc, HEALTH-2013 603288) and Systems Biology: Towards Novel Chronic Kidney Disease Diagnosis and Treatment (SysKID HEALTH–F2–2009–241544). The authors are grateful to Gert Mayer, University of Innsbruck, Austria, and Claudia Pontillo, Mosaiques Diagnostics, Germany, for critically reviewing the manuscript and to Clemens Gutzeit for help with preparing the original artwork.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to writing this article, researching the data, reviewing and/or editing of the manuscript before submission, and discussion of its content.
Corresponding author
Ethics declarations
Competing interests
H.M. is the co-founder and co-owner of Mosaiques Diagnostics and DiaPat—companies that provide clinical proteomics services—and developed the CKD273 urinary proteomic classifier. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Mischak, H., Delles, C., Vlahou, A. et al. Proteomic biomarkers in kidney disease: issues in development and implementation. Nat Rev Nephrol 11, 221–232 (2015). https://doi.org/10.1038/nrneph.2014.247
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2014.247
This article is cited by
-
Aktuelles zu diagnostischen und prognostischen Biomarkern einer diabetischen Nephropathie
Die Diabetologie (2023)
-
PRYNT: a tool for prioritization of disease candidates from proteomics data using a combination of shortest-path and random walk algorithms
Scientific Reports (2021)
-
Multiplexed MRM-based protein quantification of putative prognostic biomarkers for chronic kidney disease progression in plasma
Scientific Reports (2020)
-
Importance of Identifying Novel Biomarkers of Microvascular Damage in Type 1 Diabetes
Molecular Diagnosis & Therapy (2020)
-
Relation of multi-marker panel to incident chronic kidney disease and rapid kidney function decline in African Americans: the Jackson Heart Study
BMC Nephrology (2018)