Abstract
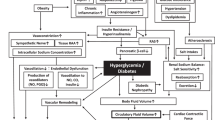
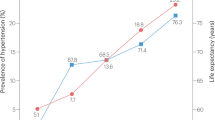
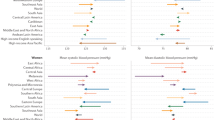
The term prehypertension was coined in 1939 in the context of early studies that linked high blood pressure recorded during physical examination for life insurance purposes to subsequent morbidity and mortality. These studies demonstrated that individuals with blood pressure >120/80 mmHg, but <140/90 mmHg—the accepted value for the lower limit of the hypertensive range—had an increased risk of hypertension, cardiovascular disease and early death from cardiovascular causes. The prehypertension classification of blood pressure was later used by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure to define a group of individuals at increased risk of cardiovascular events because of elevated blood pressure, an increased burden of other risk factors such as obesity, diabetes mellitus, dyslipidemia, and inflammatory markers, and evidence of organ damage for example, microalbuminuria, retinal arteriolar narrowing, increased carotid arterial intima-media thickness, left ventricular hypertrophy and coronary artery disease. Nonpharmacological treatment with lifestyle modifications such as weight loss, dietary modification and increased physical activity is recommended for all patients with prehypertension as these approaches effectively reduce risk of cardiovascular events. Pharmacological therapy is indicated for some patients with prehypertension who have specific comorbidities, including diabetes mellitus, chronic kidney disease and coronary artery disease.
Key Points
-
Prehypertension is highly prevalent and is associated with the traditional cardiovascular risk factors linked to hypertension, such as obesity, diabetes mellitus and dyslipidemia
-
Patients with prehypertension (120–139/80–89 mmHg) have an increased risk of cardiovascular morbidity and mortality compared with patients who have normal blood pressure (<120/80 mmHg)
-
Lifestyle modifications are recommended for all patients with prehypertension and effectively reduce cardiovascular risk
-
Outcome studies are needed to establish the value of pharmacologic therapy for the treatment of prehypertension
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Robinson, S. C. & Brucer, M. Range of normal blood pressure: a statistical and clinical study of 11,383 persons. Arch. Intern. Med. 64, 409–444 (1939).
Chobanian, A. V. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42, 1206–1252 (2003).
Lewington, S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Vasan, R. S., Larson, M. G., Leip, E. P., Kannel, W. B. & Levy, D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 358, 1682–1686 (2001).
Vasan, R. S. et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA 287, 1003–1010 (2002).
Elliott, W. J. & Black, H. R. Prehypertension. Nat. Clin. Pract. Cardiovasc. Med. 4, 538–548 (2007).
Mancia, G. et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 25, 1105–1187 (2007).
Wang, Y. & Wang, Q. J. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch. Intern. Med. 164, 2126–2134 (2004).
Lloyd-Jones, D. et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119, e21–e181 (2009).
Ostchega, Y., Yoon, S. S., Hughes, J. & Louis, T. Hypertension awareness, treatment, and control—continued disparities in adults: United States, 2005–2006. NCHS Data Brief 1–8 (2008).
Greenlund, K. J., Croft, J. B. & Mensah, G. A. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Arch. Intern. Med. 164, 2113–2118 (2004).
Mainous, A. G. 3rd, Everett, C. J., Liszka, H., King, D. E. & Egan, B. M. Prehypertension and mortality in a nationally representative cohort. Am. J. Cardiol. 94, 1496–1500 (2004).
Hsia, J. et al. Prehypertension and cardiovascular disease risk in the Women's Health Initiative. Circulation 115, 855–860 (2007).
Grotto, I., Grossman, E., Huerta, M. & Sharabi, Y. Prevalence of prehypertension and associated cardiovascular risk profiles among young Israeli adults. Hypertension 48, 254–259 (2006).
Zhang, Y. et al. Prehypertension, diabetes, and cardiovascular disease risk in a population-based sample: the Strong Heart Study. Hypertension 47, 410–414 (2006).
King, D. E., Egan, B. M., Mainous, A. G. 3rd & Geesey, M. E. Elevation of C-reactive protein in people with prehypertension. J. Clin. Hypertens. (Greenwich) 6, 562–568 (2004).
Chrysohoou, C., Pitsavos, C., Panagiotakos, D. B., Skoumas, J. & Stefanadis, C. Association between prehypertension status and inflammatory markers related to atherosclerotic disease: The ATTICA Study. Am. J. Hypertens. 17, 568–573 (2004).
Kannel, W. B. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA 275, 1571–1576 (1996).
Leung, H. et al. Relationships between age, blood pressure, and retinal vessel diameters in an older population. Invest. Ophthalmol. Vis. Sci. 44, 2900–2904 (2003).
Wong, T. Y., Klein, R., Klein, B. E., Meuer, S. M. & Hubbard, L. D. Retinal vessel diameters and their associations with age and blood pressure. Invest. Ophthalmol. Vis. Sci. 44, 4644–4650 (2003).
Ikram, M. K. et al. Retinal vessel diameters and risk of hypertension: the Rotterdam Study. Hypertension 47, 189–194 (2006).
Chen, J. et al. The metabolic syndrome and chronic kidney disease in U. S. adults. Ann. Intern. Med. 140, 167–174 (2004).
Bianchi, S., Bigazzi, R. & Campese, V. M. Microalbuminuria in essential hypertension: significance, pathophysiology, and therapeutic implications. Am. J. Kidney Dis. 34, 973–995 (1999).
Lee, J. E. et al. Serum uric acid is associated with microalbuminuria in prehypertension. Hypertension 47, 962–967 (2006).
Deckert, T., Feldt-Rasmussen, B., Borch-Johnsen, K., Jensen, T. & Kofoed-Enevoldsen, A. Albuminuria reflects widespread vascular damage. The Steno hypothesis. Diabetologia 32, 219–226 (1989).
Manios, E. et al. Impact of prehypertension on common carotid artery intima-media thickness and left ventricular mass. Stroke 40, 1515–1518 (2009).
Pletcher, M. J. et al. Prehypertension during young adulthood and coronary calcium later in life. Ann. Intern. Med. 149, 91–99 (2008).
Markus, M. R. et al. Implications of persistent prehypertension for ageing-related changes in left ventricular geometry and function: the MONICA/KORA Augsburg study. J. Hypertens. 26, 2040–2049 (2008).
Vasan, R. S. et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N. Engl. J. Med. 345, 1291–1297 (2001).
Qureshi, A. I., Suri, M. F., Kirmani, J. F., Divani, A. A. & Mohammad, Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke 36, 1859–1863 (2005).
Hansen, T. W. et al. Cardiovascular outcome in relation to progression to hypertension in the Copenhagen MONICA cohort. Am. J. Hypertens. 20, 483–491 (2007).
Marquez-Celedonio, F. G. et al. Clinical effect of lifestyle modification on cardiovascular risk in prehypertensives: PREHIPER I study [Spanish]. Rev. Esp. Cardiol. 62, 86–90 (2009).
Elmer, P. J. et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann. Intern. Med. 144, 485–495 (2006).
Appel, L. J. et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 336, 1117–1124 (1997).
Svetkey, L. P. Management of prehypertension. Hypertension 45, 1056–1061 (2005).
Sacks, F. M. et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 344, 3–10 (2001).
Maruthur, N. M., Wang, N. Y. & Appel, L. J. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation 119, 2026–2031 (2009).
Appel, L. J. et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 294, 2455–2464 (2005).
Cook, N. R. et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ 334, 885–888 (2007).
Chobanian, A. V. Prehypertension revisited. Hypertension 48, 812–814 (2006).
Puska, P. et al. The community-based strategy to prevent coronary heart disease: conclusions from the ten years of the North Karelia project. Annu. Rev. Public Health 6, 147–193 (1985).
Tuomilehto, J. et al. Decline in cardiovascular mortality in North Karelia and other parts of Finland. Br. Med. J. (Clin. Res. Ed.) 293, 1068–1071 (1986).
Vartiainen, E. et al. Twenty-year trends in coronary risk factors in north Karelia and in other areas of Finland. Int. J. Epidemiol. 23, 495–504 (1994).
Vartiainen, E., Puska, P., Pekkanen, J., Tuomilehto, J. & Jousilahti, P. Changes in risk factors explain changes in mortality from ischaemic heart disease in Finland. BMJ 309, 23–27 (1994).
Vartiainen, E., Sarti, C., Tuomilehto, J. & Kuulasmaa, K. Do changes in cardiovascular risk factors explain changes in mortality from stroke in Finland? BMJ 310, 901–904 (1995).
Puska, P., Vartiainen, E., Tuomilehto, J., Salomaa, V. & Nissinen, A. Changes in premature deaths in Finland: successful long-term prevention of cardiovascular diseases. Bull. World Health Organ. 76, 419–425 (1998).
Laatikainen, T. et al. Sodium in the Finnish diet: 20-year trends in urinary sodium excretion among the adult population. Eur. J. Clin. Nutr. 60, 965–970 (2006).
Julius, S. et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N. Engl. J. Med. 354, 1685–1697 (2006).
Lüders, S. et al. The PHARAO study: prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: a prospective, randomized, controlled prevention trial of the German Hypertension League. J. Hypertens. 26, 1487–1496 (2008).
Skov, K. et al. Treatment of young subjects at high familial risk of future hypertension with an angiotensin-receptor blocker. Hypertension 50, 89–95 (2007).
Sipahi, I. et al. Effects of normal, pre-hypertensive, and hypertensive blood pressure levels on progression of coronary atherosclerosis. J. Am. Coll. Cardiol. 48, 833–838 (2006).
Rosendorff, C. et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation 115, 2761–2788 (2007).
Schunkert, H. Pharmacotherapy for prehypertension—mission accomplished? N. Engl. J. Med. 354, 1742–1744 (2006).
Harrap, S. B., Nicolaci, J. A. & Doyle, A. E. Persistent effects on blood pressure and renal haemodynamics following chronic angiotensin converting enzyme inhibition with perindopril. Clin. Exp. Pharmacol. Physiol. 13, 753–765 (1986).
Gillies, L. K., Lu, M., Wang, H. & Lee, R. M. AT1 receptor antagonist treatment caused persistent arterial functional changes in young spontaneously hypertensive rats. Hypertension 30, 1471–1478 (1997).
Wu, J. N. & Berecek, K. H. Prevention of genetic hypertension by early treatment of spontaneously hypertensive rats with the angiotensin converting enzyme inhibitor captopril. Hypertension 22, 139–146 (1993).
Acknowledgements
Charles P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Pimenta, E., Oparil, S. Prehypertension: epidemiology, consequences and treatment. Nat Rev Nephrol 6, 21–30 (2010). https://doi.org/10.1038/nrneph.2009.191
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2009.191
This article is cited by
-
Combined association of triglyceride-glucose index and systolic blood pressure with all-cause and cardiovascular mortality among the general population
Journal of Translational Medicine (2022)
-
Non-pharmacological management of hypertension: in the light of current research
Irish Journal of Medical Science (1971 -) (2019)
-
Hypertension Prevalence, Treatment, and Related Behaviors Among Asian Americans: An Examination by Method of Measurement and Disaggregated Subgroups
Journal of Racial and Ethnic Health Disparities (2019)
-
Effects of heart rate variability biofeedback on cardiovascular responses and autonomic sympathovagal modulation following stressor tasks in prehypertensives
Journal of Human Hypertension (2016)
-
Salt Sensitivity: Challenging and Controversial Phenotype of Primary Hypertension
Current Hypertension Reports (2016)