Key Points
-
Streptococcus agalactiae or Group B Streptococcus (GBS) is an important pathogen that affects neonates, peripartum women and the elderly worldwide. Prenatal maternal screening for GBS and antibiotic treatment has reduced the rate of neonatal GBS disease but the best long-term solution for control of the disease is vaccination.
-
Several GBS vaccine candidates have been developed, including conjugate vaccines prepared by linking purified capsular polysaccharide to proteins. Conjugate vaccines have been prepared against all nine currently identified GBS serotypes.
-
Human clinical trials with several conjugate vaccines have successfully completed phase I and II testing with promising results. In addition, a type III conjugate vaccine has been found to be safe and immunogenic in pregnant women.
-
Reverse vaccinology has revealed new GBS protein antigens that are immunogenic and efficacious in preclinical studies involving mice. Further advances in GBS vaccine development are likely through combining genomics with newer proteomic technologies.
Abstract
An ongoing public health challenge is to develop vaccines that are effective against infectious diseases that have global relevance. Vaccines against serotypes of group B Streptococcus (GBS) that are prevalent in the United States and Europe are not optimally efficacious against serotypes common to other parts of the world. New technologies and innovative approaches are being used to identify GBS antigens that overcome serotype-specificity and that could form the basis of a globally effective vaccine against this opportunistic pathogen. This Review highlights efforts towards this goal and describes a template that can be followed to develop vaccines against other bacterial pathogens.
Similar content being viewed by others
Main
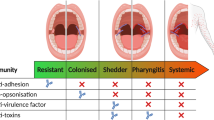
Group B Streptococcus (GBS), also referred to as Streptococcus agalactiae , is a Gram-positive, opportunistic pathogen that colonizes the gastrointestinal and genitourinary tracts of up to 50% of healthy adults1,2. This microorganism causes pneumonia, septicaemia and meningitis in neonates, is responsible for significant morbidity in pregnant women and the elderly, and is a serious cause of mortality in immunocompromised adults3,4. GBS can also colonize the mammary glands of ruminants, where the organism can survive for extended periods, causing clinical and subclinical mastitis, which affects milk quality and quantity5. GBS has been isolated from other animals including dogs, horses, guinea pigs and even fish6.
Human isolates of GBS express a capsular polysaccharide (CPS), a major virulence factor that helps the microorganism evade host defence mechanisms7. Isolates of GBS can be divided into nine CPS serotypes (Ia Ib, II, III, IV, V, VI, VII and VIII) each antigenically and structurally unique. In the 1930s, Rebecca Lancefield established that protection against GBS infection in mice could be achieved using CPS-specific polyclonal rabbit serum8,9. CPS-tetanus toxoid conjugate vaccines effective against all nine currently identified GBS serotypes have been prepared and were shown to induce functionally active CPS-specific IgG10. Clinical trials of conjugate vaccines prepared with purified CPS types Ia, Ib, II, III and V have demonstrated that these preparations are safe and immunogenic11,12. Not unexpectedly, these preparations do not offer protection against other GBS serotypes, such as type VIII, prevalent in other regions of the world13. As an alternative to CPS-based vaccines, a number of groups have explored the development of vaccines based on antigenic proteins. So far, however, the protein antigens investigated have been restricted to particular serotypes and no complete cross-serotype protection has been achieved14. To address this need, efforts are ongoing to develop a universally effective vaccine for GBS disease that exploits the recently acquired genomic sequences of GBS strains, and to then use this information to identify new candidate antigens of global relevance.
It is now possible to determine the complete genome sequence of a pathogen in a short period of time and at a relatively low cost. The generated genomic information can then be used to screen the inclusive set of potential proteins encoded by microorganisms in search of vaccine candidates — an approach referred to as reverse vaccinology15 (Fig. 1). This genome-wide in silico prediction process typically targets approximately 10–25% of all genome-encoded proteins and necessitates high-throughput cloning and recombinant protein expression for target validation. Today, the reverse vaccinology approach to vaccine development is being used to tackle infections caused by streptococci, Chlamydiae spp., staphylococci, Plasmodium falciparum and bioterrorism-associated agents including Yersinia pestis .
A schematic demonstration of the essential steps required for vaccine development using the conventional approach (a), and reverse vaccinology (b). *Although DNA vaccines are potentially useful, in the case of Group B Streptococcus they have not been tested and are unlikely to be available in the short term. Reproduced with permission from Ref. 15 © (2000) Elsevier.
Indeed, the elucidation of the genome sequences of GBS type V, III, Ia and five additional isolates16,17,18, coupled with the development of new technologies including multigenome screening, proteomics, DNA microarray and bioinformatics tools19,20,21,22,23, is allowing researchers to overcome the serotype limitation of earlier vaccine preparations in the search for a universally effective vaccine against GBS.
GBS disease burden
Puerperal sepsis has been described for centuries, and ancient Indian texts from as early as 1500 BC have noted that good hygiene leads to a reduction in perinatal disease24,25. Vaginal colonization of GBS has been reported to occur in about 12–27% of women in north Africa, India, the Middle East, Pakistan, Thailand, Saudi Arabia and the United States26. Vaginal GBS colonization during pregnancy increases instances of premature delivery and perinatal transmission of the organism. GBS is also a leading cause of chorioamnionitis and is one of several bacteria now thought to enhance the risk of preterm rupture of membranes27,28. GBS disease in neonates has been divided into early onset and late-onset disease. In early onset disease (the first 6 days of life), the neonate is usually infected by exposure to GBS before or during the birth process29. Some early onset infections can occur when the neonate is exposed to GBS during passage through the birth canal, but most early onset infections are probably caused by ascending movement of the organism from the maternal genital area through ruptured membranes into the amniotic fluid. Here, the organism multiplies and ultimately colonizes the respiratory tract of the foetus28. As a consequence, pneumonia can develop and the bacteria can disseminate in to the bloodstream causing septicaemia. Bloodstream dissemination allows the bacteria to reach multiple anatomical sites, where subsequent tissue penetration can result in meningitis and osteomyelitis29,30,31. This disease progression indicates that GBS has to adhere, invade and transcytose several epithelial and endothelial cell barriers to cause disease, and various groups have demonstrated that GBS attaches to and invades numerous transformed human tissues in vitro, including epithelial cells, endothelial cells and macrophages32,33,34,35,36,37,38,39,40,41,42,43. GBS is also associated with intra-uterine infections that can result in mid-gestation miscarriage episodes with intact membranes44.
Although the ability to invade human cells in vitro, does not always reflect the in vivo situation, observations made in a monkey model of infection indicate that the ability of GBS to invade cells in culture is relevant to human infection31. In a recent study, we have shown that the increased in vitro invasiveness of GBS grown in the presence of oxygen, correlates with increased virulence in a neonatal mouse infection model39. This finding indicates that the degree of invasiveness measured in vitro has relevance to virulence in this animal model of GBS disease.
Late-onset neonatal disease (7–90 days) occurs less frequently than early onset disease; however, this rate has not declined in the United States despite the implementation of prophylactic measures. The two most common clinical manifestations of late-onset disease are meningitis and bacteraemia. The mortality rate for late-onset neonatal disease is 2–6%, which is significantly lower than the rate of 10% for early onset infections29,45,46. Importantly, morbidity is high, as approximately 50% of neonates who survive GBS infection suffer complications, including neurological sequelae, cortical blindness, deafness, uncontrolled seizures, hydrocephalus, hearing loss, and speech and language delay29.
Incidence of neonatal disease
In 2002, revised guidelines for the prevention of perinatal invasive GBS disease were issued by CDC, the American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics (AAP)47,48. These guidelines recommend universal screening of pregnant women for rectovaginal GBS colonization at 35–37 weeks gestation. In the United States, the case-fatality ratios are now much lower than in the 1970's (over 50%) and the 1980's (15–25%)45,49. The prevalence of early onset GBS disease declined from 2.0 per 1,000 live births in 1990 to 0.6 per 1000 by 2001–2002 and 0.3 per 1,000 in 2004 (Ref. 50). In the United Kingdom and Ireland during 1996–2004, late-onset disease incidence varied little, averaging 0.35 per 1,000 live births, with annual rates ranging from 0.29 to 0.39 per 1,000 live births and 0.7 cases per 1,000 live births51. In the United States mortality rates were reported to be between 4 and 6% (Ref. 52) and ∼10% in the United Kingdom51. It has been suggested that the rate of neonatal disease is considerably underestimated because the requirement for positive cultures from blood or cerebrospinal fluid under-represents the true burden of disease53.
During the 1990's there was a decline in the incidence of neonatal GBS disease in the United States, probably as a result of the introduction of surveillance programmes and intrapartum antibiotic prophylaxis45,54,55. The widespread use of antibiotic prophylaxis to lower the incidence of GBS disease can be problematic, because this measure has been accompanied by an increase in the incidence of early onset sepsis caused by Escherichia coli 56. Stoll et al. compared the distribution of microorganisms causing early onset sepsis in very-low-birth-weight neonates in the period from 1991 to 1993 with that in the period from 1998 to 2000 — before and after the intrapartum use of antibiotics became widespread. Their analysis revealed that between the two periods, the incidence of early onset GBS sepsis dropped by 4.2 episodes per 1000 live births, but that the incidence of E. coli sepsis increased by a similar amount — 3.6 episodes per 1000 live births — with little net reduction in the overall incidence of early onset sepsis. These findings relate the increase in early onset E. coli sepsis to the antibiotics used to prevent GBS sepsis. A conclusion from this study was that immunization with a GBS vaccine has the potential to prevent GBS sepsis without engendering antibiotic resistance. In addition, the use of a vaccine also has the potential to overcome two associated problems in which antibiotic therapy has made little impact: the occurrence of preterm delivery and serious illness following neonatal sepsis56,57.
The apparent lower incidence of significant clinical disease due to GBS in less-developed countries is puzzling. It is possible that the role of GBS has been underestimated because of inadequate culture techniques and microbiological methods58,59. In addition, the low rates of invasive GBS disease reported in developing countries (for example, in India or Gambia) could be due to the combination of several factors, including the prevalence of less virulent strains, higher levels of transplacentally acquired protective antibody in serum or unrecognized/undetermined causes of early neonatal or premature deaths and stillbirths24. In addition, another important point to note is that in developing countries a large proportion of deliveries occur in rural settings outside health centres, which increase the probability that infants who develop sepsis due to GBS infection at birth will not survive. These fatalities would result in an inaccurate measure of the incidence of early onset cases. Since exposure to the organism seems to be similar in pregnant women in developing and developed countries58, the failure to recognize GBS as an important cause of neonatal sepsis in developing countries could also reflect either insufficient surveillance or true population differences. It is not known whether human genetic factors have a role in susceptibility to GBS disease. It is of interest to note, however, that in 1999 the incidence of neonatal GBS bacteraemia in India was 0.17 per 1,000 live births60, whereas a rate of 2.6 per 1,000 live births was reported in 1991 among babies born to native Indians living in South Africa61. Although these studies were done almost a decade apart, and were not designed to address the impact of genetics on susceptibility to disease, they do offer some insight into the role of healthcare services and environmental influences on disease rates.
The increased incidence of GBS disease among non-pregnant and elderly adults is discussed in detail elsewhere1,62. Invasive GBS disease in the non-pregnant, adult population has been documented in several countries, including the United States, France, Taiwan and Spain with incidence rates ranging from 4.4 to 23 cases per 100,000 adults. The higher rates of incidence occur in patients that are 60 years of age or older. Primary bacteraemia is the most common form of invasive disease, followed by skin and soft-tissue infection, pneumonia and urinary-tract infections. Risk factors for adult GBS disease include diabetes mellitus, cardiovascular disease, liver disease and cancer, and infections can be community- or nosocomially acquired. In a population-based survey, the incidence of invasive GBS disease among nursing home residents aged 65 years or older was 72.3 per 100,000 compared with 17.5 per 100,000 in age-matched non-nursing home residents4. GBS serotypes Ia, III, and V predominate in these patients with similar colonization rates (21.7%) to that of younger patients63. These epidemiological findings, which increase the target population for an efficacious vaccine, have undoubted implications for GBS vaccine development and implementation.
Vaccine development: conventional approaches
The current status of GBS vaccine development programmes are summarized in Table 1. As discussed above, the principal difficulty in developing globally effective GBS vaccines is the existence of several serotypes with different geographical distributions and the heterogeneous cross-reactivity between serotypes — a vaccine suitable for Asian or European populations might not be suitable for African populations26,64. Problems include the need to serotype GBS isolates prevalent in different developing countries. Administration of the vaccine to pregnant women is also a problem because of fear of risks of birth defects and the potential for subsequent liability26. In addition, there is considerable discussion among the experts in this field without consensus regarding the most appropriate section of the population to immunize — non-pregnant adolescents or pregnant women in the third trimester. Finally, given the current use of antibiotics both in prophylaxis and in the treatment of neonatal GBS disease, it is not feasible to design a placebo-controlled, double-blind, randomized clinical trial to determine efficacy of a GBS vaccine. One possible solution to this problem is to use functional antibody measurements as a correlate of immunity and protective levels for each serotype, calculated from paired umbilical-cord blood from case-control samples.
Capsular polysaccharide-based vaccines. As discussed above, experiments demonstrating the protective nature of polysaccharide-specific antibody can be traced back to the 1930s when it was reported that protection against GBS infections in mice could be achieved by using CPS-specific polyclonal rabbit serum8,9. Studies done in the 1970s demonstrated an unambiguous association between low levels of maternal antibody to type III CPS and susceptibility of the newborn to GBS disease65. This study also showed that CPS-specific antibody was transferred from mother to newborn, a finding that provided additional rationale for developing a vaccine based on the CPS antigen expressed by GBS. In the 1980s the first human clinical trials were conducted with purified native CPS from GBS. These trials demonstrated the safety of the antigen but also highlighted the need to improve the immunogenicity of the CPS, as only 60% of the recipients of the type III CPS vaccine showed significant IgG responses66,67. Consequently, to improve efficacy, the first GBS conjugate vaccines were prepared with serotype III coupled to tetanus toxoid (TT). Conjugate vaccines based on all nine currently identified GBS serotypes have been prepared and tested pre-clinically, although there is little or no cross protection between serotypes. As such, capsular conjugate vaccines of this type will need to be multivalent in order to provide sufficient coverage against the prevalent serotypes. In a murine model of infection, up to four TT-conjugated serotypes (Ia, Ib, II and III) were successfully combined68. Human trials have been carried out on a combination of two serotypes (II and III), and these studies have demonstrated immunogenicity and reactogenicity equivalent to that of each monovalent vaccine69. However, in order to achieve a 95% population coverage in Europe or North America, five serotypes would need to be included (Ia, Ib, II, III and V) in a multivalent vaccine, although there are other regions (for example, Japan) where such a multivalent vaccine would not be appropriate, owing to a different distribution of serotypes13,40.
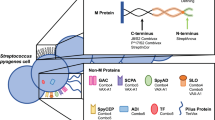
Protein-based vaccines. Until quite recently, only a limited number of GBS proteins were investigated as potential vaccine candidates, including the tandem-repeat-containing α and β components of the C protein complex, Rib, Sip and C5a peptidase14,70,71,72,73.
The ability of the C-protein complex to elicit antibodies that provide passive protection in an animal model indicates that these antigens are important virulence factors in human infection. Antibodies to this complex have also been detected in the sera of both mothers and their newborn infants74. Further research revealed that the C-protein complex from type II GBS could be one factor contributing to bacterial resistance to opsonization75, and GBS strains that express these proteins can resist intracellular killing by phagocytes76. It was also suggested that these proteins, in combination with either type-specific capsular polysaccharides or oligosaccharides, could function as an adjuvant to stimulate capsular antibody response and provide additional antigenic determinants to the vaccine77.
Rib, a surface protein that elicits protective immunity and has a similar structure and sequence to the α component of the C protein, is expressed in almost all type III GBS strains. Conversely, the α protein is rarely expressed by strains of this serotype78. For this reason, it was proposed that a combination of Rib and the α component of the C protein could form the basis of a vaccine, as most virulent strains express one of these two proteins.
Sip is a ∼45-kDa protein of unknown function that is located on the cell surface of GBS. Interestingly, this protein has been identified in GBS strains from every serotype and is efficiently recognized by specific antibodies. More importantly, immunization with the recombinant Sip protein protected CD-1 mice against lethal challenges with six GBS strains from serotypes Ia/c, Ib, II/R, III, V and VI. Furthermore, it was observed that this highly conserved protein induces cross-protective immunity against infections caused by different GBS serotypes, highlighting the potential of Sip as a universal GBS vaccine candidate72.
The C5a peptidase is a cell-surface-localized serine protease that inactivates human C5a, a neutrophil chemoattractant produced during complement activation. The protein was first identified in Streptococcus pyogenes 79 (termed SCPA80 or ScpA81) and was subsequently described in GBS82 (termed SCPB80 or ScpB81). As SCPB/ScpB is a conserved, cell-surface-localized protein, this antigen is an attractive vaccine candidate. Immunization of mice with purified SCPB/ScpB resulted in enhanced clearance of bacteria from the lungs of mice that were inoculated intranasally with GBS80. Although this study used only a single GBS strain with the uncommon serotype VI, the results indicate that SCPB/ScpB has potential as a vaccine candidate, even if the antibodies produced did not inhibit the enzymatic activity of the surface-localized protein.
Of the proteins discussed above, only Sip and C5a peptidase are conserved at the gene level in most of the GBS isolates16, and no systematic analysis of the level of cross-protection generated by these proteins has been undertaken. The identification of proteins located on the outer surface of GBS cells is an approach that has been used to find new potential protein-based vaccine candidates. One surface-expressed protein, LmbP (laminin-binding protein) is present on the surface of all GBS strains and has been proposed as a vaccine candidate83; however, progress on the development of this protein as a vaccine candidate is unknown84. Another protein, termed LrrG (leucine-rich repeat protein), is a highly conserved, cell-surface-located protein antigen that was found to induce protection against experimental GBS infection in mice. Consequently, it was proposed that this protein was a highly promising candidate antigen for potential use in a GBS vaccine85.
GBS vaccine development: new approaches
Despite the many studies that are focused on developing a GBS vaccine using conventional approaches, including the cultivation of pathogens and the identification of highly immunogenic and protective antigens using standard biochemical and microbiological techniques, little success has been achieved in terms of developing a vaccine that is globally effective. However, recent years have witnessed the welcome emergence of genomics, proteomics, gene expression and in silico technologies that are presenting exciting new opportunities in the hunt for an effective and globally relevant GBS vaccine.
The first significant steps forward in this new era were the publication of the complete genome sequences of GBS serotype III strain NEM316 (Ref. 17) and GBS serotype type V strain 2603 V/R (Ref. 16). The recent publication of GBS serotype Ia strain A909, together with the draft genomes of 5 additional strains, has significantly increased the value of this approach — a knowledge of the genetic blueprints and the comparative power of eight GBS strains, from the major clonal complexes responsible of neonatal infections, has huge potential in the search for novel and globally prevalent vaccine candidates. Table 2 summarizes how current technologies are being exploited to identify new GBS vaccine candidates.
Genomic and gene-expression approaches. Genomic-based technologies have many advantages compared with conventional approaches, which can be time-consuming and can only usually identify abundant antigens that are expressible under in vitro culture conditions. Genomics allows antigen candidates to be identified on the basis of sequence conservation in different serotypes and strains of a given pathogen, and by predicting the surface exposure of a protein. Tettelin et al. compared the predicted protein sets of S. agalactiae, S. pyogenes and Streptococcus pneumoniae . This analysis revealed that approximately 50% of the genes are homologous, indicating substantial overlap in the virulence mechanisms used by these pathogens15. In terms of vaccine development, the identification of shared virulence factors and protective antigens could support a concept of combined vaccination approaches. Although, the sequence of a single genome does not reflect how genetic variability drives pathogenesis within a bacterial species, and is a limitation regarding genome-wide screens for vaccine candidates or for antimicrobial targets, the identification of universal GBS vaccine candidates by multigenome analysis and screening has been reported19. In this approach the genome sequences of eight GBS strains belonging to different serotypes of GBS were analysed and compared. This study revealed that 1,811 genes (∼80% of each genome) were shared by all strains — the 'core' genome — and 765 genes were not present in all strains — the 'variable' genome86. Using in silico analysis, genes encoding putative surface-associated and secreted proteins were identified from these two subgenomes. A total of 589 proteins were identified (396 'core' genes and 193 'variable' genes), of which 312 were successfully expressed, purified and used to immunize mice. A combination of four proteins, Sip (SAG0032), present in the core subgenome, and three other putative, surface-associated proteins (SAG1408, SAG0645, SAG0649), from the variable subgenome, elicited protection in infant mice and their combination proved highly protective against a large panel of GBS strains, including all circulating serotypes.
This study validated the usefulness of the multigenome analysis approach in the identification of potential vaccine candidates against highly variable pathogens, including GBS. Characterization of these newly identified vaccine antigens revealed that the three putative, surface-associated proteins can form a pilus- like structure extending from the bacterial surface20. Recent evidence indicates that pili are important virulence factors in Gram-positive bacterial pathogenesis that have been missed by conventional experimental approaches for a century87. The biogenesis of these extracellular appendages and how they interact with host cells is the focus of current research88,89 (for a detailed review on Gram-positive pili, please refer to Telford et al90). Interestingly, the use of Lactococcus lactis as a heterologous host to express GBS pili was recently shown to be a promising approach for the development of multivalent live vaccines91.
Mathematical extrapolation of the GBS genomic data indicates that the gene reservoir available for inclusion in the GBS pan-genome is vast, and that unique genes will continue to be identified even after the sequencing of hundreds of genomes18. Diversity among isolates also arises by homologous recombination leading to the exchange of complete loci encoding surface proteins, or of the internal part of genes encoding putative antigens, as was first described for the α-C/Rib family92. The combination of the different alleles at these multiple loci allows GBS strains to express different combinations of surface proteins, a strategy used by the pathogen to evade host immune mechanisms; however, this versatility will also have to be taken into consideration when designing a universal vaccine that is effective against GBS93.
To understand the mechanism by which pathogens cause disease, it is necessary to identify the genes that are required for the establishment and maintenance of an infection. In the past, large-scale screening to identify attenuated mutants was not attempted because of the lack of a suitable technology for the testing of individual mutants in animal models of infection. However, the technique of signature tag mutagenesis (STM) allows the screening of a large number of mutants in an animal model of infection94. STM can also be used to screen for bacterial gene products whose expression and function in vivo indicates their suitability as potential vaccine antigens. This technique has the advantage of reducing the potential selection bias inherent in screening mutants in just one type of in vitro test of virulence. STM technology has been applied to a range of different pathogens, including Legionella pneumophila , Salmonella typhimurium , Vibrio cholerae , Staphylococcus aureus , and S. pneumoniae, and has resulted in the discovery of new virulence genes and potential vaccine candidates95,96,97,98,99,100. In the case of GBS, an STM analysis revealed many putative virulence factors, including adhesins, various cell-wall components, transcriptional regulators and ORFs with no previously assigned function101. STM analysis also revealed GBS genomic loci that encode various functional gene classes, underscoring the diversity of bacterial processes required for the infection process. The significance of STM in terms of vaccine development is that protective vaccine components must be derived from proteins that are expressed under in vivo disease conditions. As many bacterial virulence factors and antigens are only expressed in vivo, experimental approaches that focus on in vitro-grown bacteria can overlook important protective antigens.
Proteomic approaches. Proteomics, in conjunction with genomic approaches, provides interesting insights into microbial pathogenesis at an organism level. There are several reasons for focusing on the analysis of proteins: first, the level of mRNA expression frequently does not represent the amount of 'active' protein in a cell102; second, the gene sequence does not give any information on post-translational modifications (PTMs) that could be essential for protein function and activity; and third, genome analysis does not provide information on dynamic cellular processes103. The application of proteomics to vaccine development provides interesting opportunities to elucidate both bacterial pathogenic mechanisms and new vaccine candidates (Fig. 2). Hughes and colleagues have used a proteomic approach (2-dimensional electrophoresis (2DE) and matrix-assisted laser desorption/ionization mass spectrometry (MALDI-MS) to identify the main surface-exposed proteins of GBS22. Of the 30 major spots identified as GBS specific on the 2DE gels, it was possible to identify 27 proteins. Six of these proteins — previously uncharacterized in GBS — were cloned and sequenced. Two of them, a carbamoyltransferase and a phosphoglycerate kinase, were successfully expressed as recombinant antigens and were used to raise antisera in rabbits. The antisera obtained were first used to verify the surface localization of the two antigens. They were also shown to provide protection against GBS bacterial challenge, demonstrating the successful application of one proteomic technology in identifying new potential vaccine candidates.
A schematic representation of a proteomic approach to identify expressed proteins. Proteins are separated either by 2-dimensional electrophoresis or SDS-PAGE. The protein bands or spots are then excised, subjected to in-gel digestion with trypsin (a), and the resulting peptides are separated by high-performance liquid chromatography (HPLC) (b). The eluting peptides are ionized by electrospray ionization, enter the mass spectrometer (c), and are fragmented to collect sequence information (MS/MS (tandem mass spectroscopy) spectrum) (d). The amino-acid sequence of a peptide is obtained by comparing the MS/MS spectrum of the ionized peptide with predicted spectra generated from protein-sequence databases (e). Obtaining the peptide sequence allows identification of the original protein (f). Figure supplied courtesy of Steven Gygi, Harvard University, Boston.
Technologies are also required that can quantitatively (and automatically) measure protein expression in different cells and tissues. Gygi et al. have described one approach, termed isotope coded affinity tag chromatography (ICAT), which provides a broadly applicable means for the quantitative cataloguing and comparison of protein expression in various normal and disease states, a task that is becoming increasingly important in the emerging field of proteomics104 (Fig. 3). The ability to quantify dynamic changes in protein-expression levels over time is also vital to gain a complete understanding of highly regulated and significantly timed cellular processes. These events can be further characterized by monitoring the fate of PTM proteins that might have a role in pathogenesis and ultimately assist in identifying a suitable vaccine candidate. To study PTM proteins, a technology termed absolute quantification of proteins and phosphoproteins (AQUA) was recently described105, which is useful as it allows the direct quantification of the levels of PTM proteins (Fig. 4).
a | The ICAT reagent consists of three elements: an affinity tag (biotin) used to isolate ICAT-labelled peptides; a linker that can incorporate stable isotopes; and a reactive group with specificity toward thiol groups (cysteines). The reagent exists in two forms: heavy (contains eight deuterium atoms) and light (contains no deuterium atoms). b | Two protein mixtures of two different cell states (for example, a pathogen culture grown in vivo versus a culture grown in vitro) are treated with the isotopically light and heavy ICAT reagents, respectively; an ICAT reagent is covalently attached to each cysteinyl residue in every protein. Proteins from cell state 1 are shown in green, and proteins from cell state 2 are shown in blue. The protein mixtures are combined, digested to peptides, and ICAT-labelled peptides are isolated using the biotin tag. These peptides are separated by microcapillary high-performance liquid chromatography. The ratios of the original amounts of proteins from the two cell states are strictly maintained in the peptide fragments. The relative quantification is determined by the ratio of the peptide pairs. Every other scan is devoted to fragmenting and then recording sequence information about an eluting peptide by MS/MS (tandem mass spectroscopy). The protein is identified by searching the recorded sequence information against large protein databases. ICAT, isotope coded affinity tag chromatography; LC-MS/MS, liquid chromatography tandem mass spectroscopy. Reproduced with permission from Nature Biotechnology Ref. 104 © (1999) Macmillan Publishers Ltd.
The AQUA strategy has two stages. Stage 1 involves the selection and standard synthesis of a peptide (or phosphopeptide (denoted here by pS)) from the protein of interest. During synthesis, stable isotopes are incorporated (for example, 13C, 15N) at a single amino-acid residue such as the leucine shown here (denoted by L*). These peptide internal standards (IS) are analysed by MS/MS (tandem mass spectroscopy) to examine peptide fragmentation patterns. The mass spectrometer is next set up to do a SRM (selected reaction monitoring) analysis in which a specific precursor-to-product ion transition is measured. Stage 2 is the implementation of the new peptide IS for precise sample protein quantification. Proteins are harvested from a biological sample (for example, bacteria isolated from the site of infection) and proteolysed with trypsin in the presence of the IS peptide and phosphopeptide. An LC–SRM (liquid chromatography–selected reaction monitoring) experiment then measures the abundance of a specific fragment ion from both the native peptide and the synthesized peptide as a function of reverse-phase chromatographic retention time. The absolute quantification of the protein of interest is determined by comparing the abundance of the known IS peptide with the native peptide. AQUA, absolute quantification. Reproduced with permission from Ref. 105. © (2003) National Academy of Sciences, USA.
The application of these technologies to the study of microbial pathogenesis should provide valuable insights into the molecular basis of infection and lead to the identification of potential vaccine candidates that could otherwise be missed using more conventional techniques. To the best of our knowledge, neither ICAT nor AQUA have been applied to the study of GBS pathogenesis and could be fruitful opportunities in the search for new and globally applicable vaccine candidates.
Conclusions and future prospects
As GBS is an important cause of neonatal infection throughout the world, it is imperative to design and implement an effective, global vaccine strategy. The current vaccine preparations for GBS are based on the serotypes and multilocus sequence types (MLST) prevalent in the United States and Europe, and target the hyper-virulent sequence type 17 (ST17)106. However, these vaccine preparations are not as effective in other regions because of the prevalence of different serotypes or virulent sequence types expressing a different repertoire of surface proteins. To ensure effective vaccine development, it will be important to continually monitor the distribution pattern of the prevalent serotypes and sequence types in all regions of the world, thereby ensuring the inclusion of the most relevant components in a global GBS vaccine.
Initial efforts applying a genomics approach to GBS vaccine development have led to the identification of new, highly conserved protein antigens that are expressed on the bacterial surface. One of the positive aspects of this methodology is that each of the antigens that demonstrate protection can be produced as a soluble recombinant protein in E. coli, a property that is a considerable asset for the commercial production of a vaccine. The reverse vaccinology approach reduces the time and cost required for the identification of suitable antigen candidates and provides new opportunities for those microbial diseases for which conventional vaccine-development approaches have failed107,87.
In conclusion, the successful use of multigenome screening methods coupled with the application of proteomics could be a template for the development of protein-based vaccines against human pathogens, such as GBS, for which vaccines are either not available or, if they do exist, are in need of significant improvement.
References
Schuchat, A. Epidemiology of group B streptococcal disease in the United States: shifting paradigms. Clin. Microbiol. Rev. 11, 497–513 (1998).
Hansan, S. M., Uldbjerg, N., Kilian, M. & Sorensen, U. B. Dynamics of Streptococcus agalactiae colonization in women during and after pregnancy and in their infants. J. Clin. Microbiol. 42, 83–89 (2004).
Dermer, P., Lee, C., Eggert, J. & Few, B. A history of neonatal group B streptococcus with its related morbidity and mortality rates in the United States. J. Pediatr. Nurs. 19, 357–363 (2004).
Edwards, M. S. & Baker, C. J. Group B Streptococcal infections in elderly adults. Clin. Infect. Dis. 41, 839–847 (2005). An excellent review providing in-depth information on GBS infection in elderly adults.
Keefe, G. P. Streptococcus agalactiae mastitis: a review. Can. Vet. J. 38, 429–437 (1997).
Vandamme, P., Devriese, L. A., Pot, B., Kersters, K. & Melin, P. Streptococcus difficile is a nonhemolytic group B, type Ib Streptococcus. Int. J. Syst. Bacteriol. 47, 81–85 (1997).
Rubens, C. E., Wessels, M. R., Heggen, L. M. & Kasper, D. L. Transposon mutagenesis of type III group B Streptococcus: correlation of capsule expression with virulence. Proc. Natl Acad. Sci. USA. 84, 7208–7212 (1987).
Lancefield, R. C. A serological differentiation of specific types of bovine hemolytic streptococci (group B). J. Exp. Med. 59, 441–458 (1934).
Lancefield, R. C. Two serological types of group B hemolytic streptococci with related, but not identical, typespecific substances. J. Exp. Med. 67, 25–40 (1938).
Paoletti, L. C. & Madoff, L. C. Vaccines to prevent neonatal GBS infection. Semi. Neonatal. 7, 315–323 (2002). This review describes the development of conjugate GBS vaccines against all clinically important serotypes and their performance in animal models (phase 1 and phase II clinical trials).
Paoletti, L. C. & Kasper, D. L. Conjugate vaccines against group B Streptococcus types IV and VII. J. Infect. Dis. 186, 123–126 (2002).
Paoletti, L. C., Madoff, L. C. & Kasper, D. L. in Gram-Positive Pathogens (eds Fischetti, V. A., Novick, R. P., Ferretti, J. J., Portony, D. A. & Rood, J. I.) 137–153 (ASM Press, Washington DC, 2000).
Lachenauer, C. S. et al. Serotypes VI and VIII predominate among group B streptococci isolated from pregnant Japanese women. J. Infect. Dis. 179, 1030–1033 (1999).
Lindahl, G., Stalhammar-Carlemalm, M. & Areschoug, T. Surface proteins of Streptococcus agalactiae and related proteins in other bacterial pathogens. Clin. Micro. Biol. Rev. 18, 102–127 (2005). This review summarizes the properties of GBS surface proteins (and related proteins in other bacterial pathogens) that have promise as potential vaccine candidates and are likely to have key roles during various stages of infection.
Rappuoli, R. Reverse vaccinology. Curr. Opin. Microbiol. 35, 445–450 (2000).
Tettelin, H. et al. Complete genome sequence and comparative genomic analysis of an emerging human pathogen, serotype V Streptococcus agalactiae. Proc. Natl Acad. Sci. USA 99, 12391–12396 (2002).
Glaser, P. et al. Genome sequence of Streptococcus agalactiae, a pathogen causing invasive neonatal disease. Mol. Microbiol. 45, 1499–1513 (2002).
Tettelin, H. et al. Genomic analysis of multiple pathogenic isolates of Streptococcus agalactiae: Implications for the microbial 'pan-genome'. Proc. Natl Acad. Sci. USA 102, 13950–13955 (2005). A comparative genome analysis of GBS strains that explores genetic variability and its implications for microbial pathogenesis.
Maione, D. et al. Identification of a universal Group B Streptococcus vaccine by multiple genome screen. Science. 309, 148–150 (2005). The first report using multiple genome screening as a strategy to identify GBS vaccine candidates. This article also shows the potential of this approach for other microorganisms with considerable genetic variability.
Lauer, P. et al. Genome analysis reveals pili in Group B Streptococcus. Science 309, 105 (2005).
Lamy, M. C. et al. CovS/CovR of group B streptococcus: a two component global regulatory system involved in virulence. Mol. Microbiol. 54, 1250–1268 (2004).
Hughes, M. J. et al. Identification of major outer surface proteins of Streptococcus agalactiae. Infect. Immun. 70, 1254–1259 (2002).
Sutcliffe, I. C. & Harrington, D. J. Lipoproteins of Mycobacterium tuberculosis: an abundant and functionally diverse class of cell envelope components. FEMS Microbiol. Rev. 28, 645–659 (2004).
Shet, A. & Ferrieri, P. Neonatal & maternal group B streptococcal infections: A comprehensive review. Indian J. Med. Res. 120, 141–150 (2004).
Kutumbiah, P. Ancient Indian medicine. (Orient Longman, Madras, 1962).
WHO. State of the art of vaccine research and development: Initiative for Vaccine Research [online] (2005).
Ferrieri, P., Cleary, P. P. & Seeds, A. E. Epidemiology of group B streptococcal carriage in pregnant women and newborn infants. J. Med. Microbiol. 10, 103–114 (1977).
Galask, R. P., Varner, M. W., Petzold, C. R. & Wilbur, S. L. Bacterial attachment to the chorioamniotic membranes. Am. J. Obstet. Gynecol. 148, 915–928 (1984).
Edwards, M. S. & Baker, C. J. in Infectious Diseases of the Fetus and the Newborn Infant (eds Remington, J. S. & Klein, J. O.) 1091–1156 (The W. B. Saunders Co., Philadelphia, 2001).
Nizet, V. & Rubens, C. E. In Gram-Positive Pathogens (eds Fischetti, V. A., Novick, R. P., Ferretti, J. J., Portnoy, D. A. & Rood, J. I.) 125–136 (ASM Press, Washington DC, 2000).
Rubens, C. E. et al. Pathophysiology and histopathology of group B streptococcal sepsis in Macaca nemestrina primates induced after intraamniotic inoculation: evidence for bacterial cellular invasion. J. Infect. Dis. 164, 320–330 (1991).
Gibson, R. L., Lee, M. K., Soderland, C., Chi, E. Y. & Rubens, C. E. Group B streptococci invade endothelial cells: type III capsular polysaccharide attenuates invasion. Infect. Immun. 61, 478–485 (1993).
Kallman, J. & Kihlstrom, E. Penetration of group B streptococci through polarized Madin-Darby canine kidney cells. Pediatr. Res. 42, 799–804 (1997).
Nizet, V. et al. Invasion of brain microvascular endothelial cells by group B streptococci. Infect. Immun. 65, 5074–5081 (1997).
Rubens, C. E., Smith, S., Hulse, M., Chi, E. Y. & van Belle, G. Respiratory epithelial cell invasion by group B streptococci. Infect. Immun. 60, 5157–5163 (1992).
Valentin-Weigand, P., Jungnitz, H., Zock, A., Rohde, M. & Chhatwal, G. S. Characterization of group B streptococcal invasion in HEp-2 epithelial cells. FEMS Microbiol. Lett. 147, 69–74 (1997).
Winram, S. B., Jonas, M., Chi, E. & Rubens, C. E. Characterization of group B streptococcal invasion of human chorion and amnion epithelial cells in vitro. Infect. Immun. 66, 4932–4941 (1998).
Malin, G. & Paoletti, L. C. Use of a dynamic in vitro attachment and invasion system (DIVAS) to determine influence of growth rate on invasion of respiratory epithelial cells by group B Streptococcus. Proc. Natl Acad. Sci. USA 98, 13335–13340 (2001).
Johri, A. K., Padilla, J., Malin, G. & Paoletti, L. C. Oxygen regulates invasiveness and virulence of group B streptococcus. Infect. Immun. 71, 6707–6711 (2003).
Mikamo, H., Johri, A. K., Paoletti, L. C., Madoff, L. C. & Onderdonk, A. B. Adherence to, invasion by, and cytokine production in response to serotype VIII group B Streptococci. Infect. Immun. 72, 4716–4722 (2004).
Johri, A. K., Patwardhan, V. & Paoletti, L. C. Growth rate and oxygen regulate the interaction of group B Streptococcus with polarized respiratory epithelial cells. Can. J. Microbiol. 51, 283–286 (2005).
Valentin-Weigand, P., Benkel, P., Rohde, M. & Chhatwal, G. S. Entry and intracellular survival of group B streptococci in J774 macrophages. Infect. Immun. 64, 2467–2473 (1996).
Bolduc, G. R., Baron, M. J., Gravekamp, C., Lachenauer, C. S. & Madoff, L. C. The α C mediates internalization of group B Streptococcus within cervical epithelial cells. Cell. Microbiol. 9, 751–758 (2002).
McDonald, H. M. & Chambers, H. M. Intrauterine infection and spontaneous midgestation abortion: is the spectrum of microorganisms similar to that in preterm labor. Infect. Dis. Obstet. Gynecol. 8, 220–227 (2000).
Schrag, S. J. et al. Group B streptococcal disease in the era of intrapartum antibiotic prophylaxis. N. Engl. J. Med. 342, 15–20 (2000).
Schuchat, A. Epidemiology of group B streptococcal disease in the United States: shifting paradigms. Clin. Microbiol. Rev. 11, 497–513 (1998).
CDC. Prevention of perinatal group B streptococcal disease: revised guidelines from CDC. MMWR Morb. Mortal. Wkly Rep. 51, 11 (2002).
Kainer, M., McCauley, T. & Craig, A. S. Prevention of early-onset group B streptococcal disease in newborn. Obset. Gynecol. 100, 1405–1412 (2002).
Gibbs, R. S., Schrag, S. & Schuchat, A. Perinatal infections due to group B streptococci. Obstet. Gynecol. 104, 1062–1076 (2004).
Law M. R. et al. The prevention of neonatal group B streptococcal disease: a report by a working group of the Medical Screening Society. J. Med. Screen. 12, 60–68 (2005).
Heath, P. T. et al. Group B streptococcal disease in UK and Irish infants younger than 90 days. Lancet. 363, 292–294 (2004).
Schrag, S. J. et al. A population-based comparison of strategies to prevent early-onset group B streptococcal disease in neonates. N. Engl. J. Med. 347, 233–239 (2002).
Luck, S. et al. Estimated early-onset group B streptococcal neonatal disease. Lancet 361, 1953–1954 (2003).
Moore, M. R., Schrag, S. J. & Schuchat, A. Effects of intrapartum antimicrobial prophylaxis for prevention of group B streptococcal disease on the incidence and ecology of early-onset neonatal sepsis. Lancet Infect. Dis. 3, 201–213 (2003).
Schrag, S. J. et al. Prenatal screening for infectious disease and opportunities for prevention. Obstet. Gynecol. 102, 753–760 (2003).
Stoll, B. J. et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N. Engl. J. Med. 347, 240–247 (2002).
Eschenbach, D. A. Prevention of neonatal group B streptococcal infection. N. Engl. J. Med. 347, 280–281 (2002).
Stoll, B. J. & Schuchat, A. Maternal carriage of group B streptococci in developing countries. Pediatr. Infect. Dis. J. 17, 499–503 (1998).
Kishore, K., Deorari, A. K., Singh, M. & Bhujwala, R. A. Early onset neonatal sepsis: Vertical transmission from maternal genital tract. Indian Pediatr. 24, 45–48 (1987).
Kuruvilla, K. A., Thomas, N., Jesudasan, M. V. & Jana, A. K. Neonatal group B Streptococcal bacteraemia in India: ten years' experience. Acta. Paediatr. 88, 1031–1032 (1999).
Haffejee, I. E. et al. Neonatal group B streptococcal infections in Indian (Asian) babies in South Africa. J. Infect. 22, 225–231 (1991).
Trivalle, C. Presentation and management of group B streptococcal bacteremia in older persons. Clinical Geriatrics 8, 35–48 (2000).
Edwards, M. S., Rench, M. A., Palazzi, D. L. & Baker, C. J. Group B Streptococcal colonization and serotype-specific immunity in healthy elderly persons. Clin. Infect. Dis 40, 352–357 (2005).
Brigsten, A. K., Kasper, D. L., Baker, C. J., Jennings, H. J. & Guttomsen, H. K. Induction of cross reactive antibodies by immunization of healthy adults with type Ia and Ib group b streptococcal polysaccharide tetanus toxoid conjugate vaccines. J. Infect. Dis. 185, 1277–1284 (2002).
Baker, C. J. & Kasper, D. L. Correlation of maternal antibody deficiency with susceptibility to neonatal group B streptococcal infection. N. Engl. J. Med. 294, 753–756 (1976).
Baker, C. J. & Kasper, D. L. Vaccination as a measure for prevention of neonatal GBS infection. Antibiot. Chemother. 35, 281–290 (1985).
Baker, C. J. et al. Immunization of pregnant women with a polysaccharide vaccine of group B Streptococcus. N. Engl. J. Med. 319, 1180–1220 (1988).
Paoletti, L. C. et al. Neonatal mouse protection against infection with multiple group B streptococcal (GBS) serotypes by maternal immunization with a tetravalent GBS polysaccharide-tetanus toxoid conjugate vaccine. Infect. Immun. 62, 3236–3243 (1994).
Baker, C. J. & Edwards, M. S. Group B streptococcal conjugate vaccines. Arch. Dis. Child. 88, 375–378 (2003).
Madoff, L. C., Paoletti, L. C., Tai, J. Y. & Kasper, D. L. Maternal immunization of mice with group B streptococcal type III polysaccharide β C protein conjugate elicits protective antibody to multiple serotypes. J. Clin. Invest. 94, 286–292 (1994).
Stalhammar-Carlemalm, M., Stenberg, L. & Lindahl, G. Protein Rib: a novel group B streptococcal cell surface protein that confers protective immunity and is expressed by most strains causing invasive infections. J. Exp. Med. 177, 1593–1603 (1993).
Brodeur, B. R. et al. Identification of group B streptococcal Sip protein, which elicits cross-protective immunity. Infect. Immun. 68, 5610–5618 (2000).
Cheng, Q. B. et al. Antibody against surface-bound C5a peptidase is opsonic and initiates macrophage killing of group B streptococci. Infect. Immun. 69, 2302–2308 (2001).
Bevanger, L. The Ibc proteins of group B streptococci: isolation of the a and b antigens by immunosorbent chromatography and test for human serum antibodies against the two antigens. Acta Pathol. Microbiol. Immunol. Scand. B. 93, 113–119 (1985).
Payne, N. R. & Ferrieri, P. The relation of the Ibc protein antigen to the opsonization differences between strains of type II group B streptococci. J. Infect. Dis. 151, 672–681 (1985).
Payne, N. R., Kim, Y. & Ferrieri, P. Effects of differences in antibody and complement requirements on pahgocytic uptake and intacellular killing of 'c' protein-positive and negative strains of type II group B streptococci. Infect. Immun. 55, 1243–1251 (1987).
Michel, J. L., Madoff, L. C., Kling, D. E., Kasper, D. L. & Ausubel, F. M. Cloned α and β c-protein antigens of Group B Streptococci elicit protective immunity. Infect. Immun. 59, 2023–2028 (1991).
Musser, J. M., Mattingly, S. J., Quentin, R., Goudeau, A. & Selander, R. K. Identification of a high-virulence clone of type III Streptococcus agalaaiae (group B Streptococcus) causing invasive neonatal disease. Proc. Natl Acad. Sci. USA 86, 4731–4735 (1989).
Wexler, D. E., Chenoweth, D. E. & Cleary, P. P. Mechanism of action of the group A streptococcal C5a inactivator. Proc. Natl Acad. Sci. USA 82, 8144–8148 (1985).
Cheng, Q., Stafslien, D., Purushothaman, S. S. & Cleary, P. The group B streptococcal C5a peptidase is both a specific protease and an invasin. Infect. Immun. 70, 2408–2413 (2002).
Beckmann, C., Waggoner, J. D., Harris, T. O., Tamura, G. S. & Rubens, C. E. Identification of novel adhesins from group B streptococci by use of phage display reveals that C5a peptidase mediates fibronectin binding. Infect. Immun. 70, 2869–2876 (2002).
Chmouryguina, I., Suvorov, A., Ferrieri, P. & Cleary, P. P. Conservation of the C5a peptidase genes in group A and B streptococci. Infect. Immun. 64, 2387–2390 (1996).
Spellerberg, B. et al. Lmb, a protein with similarities to the LraI adhesin family, mediates attachment of Streptococcus agalactiae to human laminin. Infect. Immun. 67, 871–878 (1999).
Heath, P. T. & Feldman, R. G. Vaccination against Group B Streptococcus. Expert Rev. Vaccines 4, 207–218 (2005).
Seepersaud, R. et al. Characterization of a novel leucin rich repeat protein antigen from Group B streptococci that elicit protective immunity. Infect. Immun. 73, 1671–1683 (2003).
Lan, R. & Reeves, P. R. Intraspecies variation in bacterial genomes: the need for a species genome concept. Trends Microbiol. 8, 396–401 (2000).
Serruto, D. & Rappuoli, R. Post-genomic vaccine development. FEBS Letters. 580, 2985–2992 (2006).
Dramsi, S. et al. Assembly and role of pili in group B streptococci. Mol. Microbiol. 60, 1401–1413 (2006).
Rosini, R. et al. Identification of novel genomic islands coding for antigenic pilus-like structures in Streptococcus agalactiae. Mol. Microbiol. 61, 126–141 (2006).
Telford, J., Barocchi, M. A., Margarit, I., Rappuoli, R. & Grandi, G. Pili in Gram-positive pathogens. Nature Rev. Microbiol. 4, 509–519 (2006). A comprehensive review describing pili in Gram-positive pathogens.
Buccato, S. et al. Use of Lactococcus lactis expressing pili from group B Streptococcus as a broad-coverage vaccine against streptococcal disease. J. Infect. Dis. 194, 331–340 (2006).
Lachenauer, C. S. et al. Mosaicism in the a-like protein genes of group B streptococci. Proc. Natl Acad. Sci. USA 97, 9630–9635 (2000).
Brochet, M, et al. Genomic diversity and evolution within the species Streptococcus agalactiae. Microbes Infect. 8, 1227–1243 (2006).
Chiang, S. L., Mekalanos, J. J. & Holden, D. W. In vivo genetic analysis of bacterial virulence. Annu. Rev. Microbiol. 53, 129–154 (1999).
Hensel, M. et al. Simultaneous identification of bacterial virulence genes by negative selection. Science. 269, 400–403 (1995).
Chiang, S. L. & Mekalanos, J. J. Use of signature tagged mutagenesis to identify Vibrio cholerae genes critical for colonization. Mol. Microbiol. 27, 797–805 (1998).
Mei, J. M., Nourbakhsh, F., Ford, C. W. & Holden, D. W. Identification of Staphylococcus aureus virulence genes in a murine model of bacteraemia using signature-tagged mutagenesis. Mol. Microbiol. 26, 399–407 (1997).
Koulter, S. N. et al. Staphylococcus aureus genetic loci impacting growth and survival in multiple infection environments. Mol. Microbiol. 30, 393–404 (1998).
Polissi, A. et al. Large scale identification of virulence genes from Streptococcus pneumoniae Infect. Immun. 66, 5620–5629 (1998).
Edelstein, P. H., Edelstein, M. A., Higa, F. & Falkow, S. Discovery of virulence genes of Legionella pneumophila by using signature tagged mutagenesis in a guinea pig pneumonia model. Proc. Natl Acad. Sci. USA 96, 8190–8195 (1999).
Jones, A. L. Knoll, K. M. & Ruben, C. E. Identification of Streptococcus agalactiae virulence genes in the neonatal rat sepsis model using signature tagged mutagenesis. Mol. Microbiol. 37, 1444–1455 (2000).
Anderson, L. & Seilhammer, J. A Comparison of selected mRNA and protein abundances in human liver. Electrophoresis 18, 533–537 (1997).
Humphrey-Smith, I., Cordwell, S. J. & Blackstock, W. P. Proteome research: complementarity and limitations with respect to the RNA and DNA worlds. Electrophoresis 18, 1217–1242 (1997).
Gygi, S. P. et al. Quantitative analysis of complex protein mixing using isotope coded affinity tags Nature Biotechnol. 17, 994–999 (1999).
Gerber, S. A. et al. Absolute quantification of proteins and phosphorylation from cell lysates by tandem MS. Proc. Natl Acad. Sci. USA 100, 6940–6945 (2003).
Jones, N. et al. Multilocus sequencing typing system for group B Streptococcus J. Clin. Microbiol. 41, 2530–2536 (2003).
Mora, M., Veggi, D., Santini, L., Pizza, M. & Rappuoli, R. Reverse vaccinology Drug Discov. Today 8, 459–464 (2003).
Wessels, M. R. et al. Immunogenicity in animals of a polysaccharide-protein conjugate vaccine against type III group B Streptococcus. J. Clin. Investi. 86, 1428–1433 (1990).
Paoletti, L. C. et al. Group B Streptococcus type II polysaccharide-tetanus toxoid conjugate vaccines. Infect. Immun. 60, 4009–4014 (1992).
Paoletti, L. C. et al. Sythesis and preclinical evaluation of glycolconjugate vaccines against group B Streptococcus types VI and VIII. J. Infect. Dis. 180, 892–895 (1999).
Madoff, L. C., Michel, J. L., Gong, E. W., Rodewald, A. K. & Kasper, D. L. Protection of neonatal mice from Group B streptococcal infection by maternal immunization with βC protein. Infect. Immun. 60, 4989–4994 (1992).
Acknowledgements
This work was supported, in part, by a grant to A.K.J. from the Department of Biotechnology, Government of India, and a grant to L.C.P. from the National Institutes of Health, USA. The authors would also like to thank Jaylyn Olivo for editorial review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Related links
DATABASES
Entrez Genome Project
GBS serotype III strain NEM316
FURTHER INFORMATION
Glossary
- Puerperal sepsis
-
An infection of the female genital tract following childbirth, abortion or miscarriage.
- Perinatal disease
-
The passage of a disease-causing agent vertically from mother directly to baby during the perinatal period — the period immediately before and after birth. Transmission can also occur across the placenta or through breast milk.
- Chorioamnionitis
-
A serious infection of the placental tissues.
- Pan-genome
-
The pan-genome consists of the set of genes that represents the genetic diversity of a group of organisms.
- Signature tag mutagenesis
-
(STM). A functional genomics approach used to identify bacterial virulence genes by simultaneously screening multiple mutants in a single host animal. Avirulent (attenuated) mutants are identified by a negative selection method (failure to colonize the host).
- Post-translational modification
-
(PTM). The enzymatic processing of a polypeptide chain after translation from messenger RNA and after peptide-bond formation has occurred. For example, glycosylation, acylation, limited proteolysis, phosphorylation and isoprenylation.
- Multilocus sequence type
-
(MLST). An unambiguous procedure for characterizing isolates of bacterial species using the sequences of internal fragments of seven house-keeping genes. For each house-keeping gene, the different sequences that are present in a bacterial species are assigned as distinct alleles and, for each isolate, the alleles at each of the seven loci define the allelic profile, or sequence type.
- Hyper-virulent sequence type 17
-
(ST17). This is a homogeneous group of GBS isolates that contain a specific and conserved set of surface proteins, probably accounting for their high capacity to cause infections in newborns.
Rights and permissions
About this article
Cite this article
Johri, A., Paoletti, L., Glaser, P. et al. Group B Streptococcus: global incidence and vaccine development. Nat Rev Microbiol 4, 932–942 (2006). https://doi.org/10.1038/nrmicro1552
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrmicro1552
This article is cited by
-
Population genomics of Group B Streptococcus reveals the genetics of neonatal disease onset and meningeal invasion
Nature Communications (2022)
-
Virulence Profiles and Antimicrobial Resistance of Streptococcus agalactiae Infective and Colonizing Strains from Argentina
Current Microbiology (2022)
-
Prevalence, population structure, distribution of serotypes, pilus islands and resistance genes among erythromycin-resistant colonizing and invasive Streptococcus agalactiae isolates recovered from pregnant and non-pregnant women in Isfahan, Iran
BMC Microbiology (2021)
-
Trends in molecular characteristics and antimicrobial resistance of group B streptococci: a multicenter study in Serbia, 2015–2020
Scientific Reports (2021)
-
Persistence of group B Streptococcus vaginal colonization and prevalence of hypervirulent CC-17 clone correlate with the country of birth: a prospective 3-month follow-up cohort study
European Journal of Clinical Microbiology & Infectious Diseases (2021)