Key Points
-
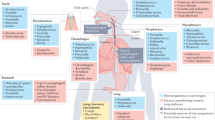
The respiratory system consists of the upper respiratory tract (the nasal cavity, pharynx and larynx) and the lower respiratory tract, including the conducting airway (the trachea and bronchi) and the respiratory zone (the alveoli). The composition of the airway, in terms of its constituent epithelial cell types and resident myeloid and lymphoid cell types, depends on its diameter.
-
Airway cells are the first responders to invading pathogens. They have multiple functions, which include; providing a physical barrier, acting as innate sensors that secrete first-order cytokines and serving as effectors of antimicrobial defences.
-
Following respiratory infection by viral, bacterial, fungal and protozoan pathogens, type 1 immune responses are engaged. These types of infection are recognized by pattern recognition receptors in sensor cells such as airway epithelial cells, macrophages, dendritic cells and plasmacytoid dendritic cells.
-
Infection by helminths or inhalation of allergens results in the engagement of the type 2 immune responses. Epithelial cells and mast cells detect the activities of the helminths and allergens, and secrete cytokines that stimulate the next tier of the immune response.
-
Sensor cells secrete distinctfirst-order cytokines in response to pathogens and activate tissue-resident lymphocytes to secrete second-order cytokines. These cytokines, in turn, activate various types of effector cells to initiate pathogen elimination and tissue repair.
-
Various internal and external factors can alter the effectiveness of the signals mediated by the sensors and effectors, and can tip the balance away from antimicrobial host defences and towards pathological inflammation. Strategies to improve disease tolerance may be needed to combat infectious diseases in this setting.
Abstract
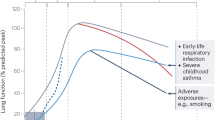
The respiratory immune response consists of multiple tiers of cellular responses that are engaged in a sequential manner in order to control infections. The stepwise engagement of effector functions with progressively increasing host fitness costs limits tissue damage. In addition, specific mechanisms are in place to promote disease tolerance in response to respiratory infections. Environmental factors, obesity and the ageing process can alter the efficiency and regulation of this tiered response, increasing pathology and mortality as a result. In this Review, we describe the cell types that coordinate pathogen clearance and tissue repair through the serial secretion of cytokines, and discuss how the environment and comorbidity influence this response.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Iwasaki, A. & Medzhitov, R. Control of adaptive immunity by the innate immune system. Nat. Immunol. 16, 343–353 (2015).
Morgan, O. W. et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A (H1N1) disease. PLoS ONE 5, e9694 (2010).
Thompson, W. W. et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 289, 179–186 (2003).
Braciale, T. J., Sun, J. & Kim, T. S. Regulating the adaptive immune response to respiratory virus infection. Nat. Rev. Immunol. 12, 295–305 (2012).
Kotton, D. N. & Morrisey, E. E. Lung regeneration: mechanisms, applications and emerging stem cell populations. Nat. Med. 20, 822–832 (2014).
Rock, J. R., Randell, S. H. & Hogan, B. L. Airway basal stem cells: a perspective on their roles in epithelial homeostasis and remodeling. Dis. Model. Mech. 3, 545–556 (2010).
Curran, D. R. & Cohn, L. Advances in mucous cell metaplasia: a plug for mucus as a therapeutic focus in chronic airway disease. Am. J. Respir. Cell Mol. Biol. 42, 268–275 (2010).
Suarez, C. J., Dintzis, S. M. & Frevert, C. W. in Comparative Anatomy and Histology: A Mouse and Human Atlas. (eds Treuting, P. M., Dintzis, S., Liggitt, D. & Frevert, C. W.) Ch. 9 (Elsevier, 2012).
Perdiguero, E. G. et al. Tissue-resident macrophages originate from yolk-sac-derived erythro-myeloid progenitors. Nature 518, 547–551 (2015).
Guilliams, M. et al. Alveolar macrophages develop from fetal monocytes that differentiate into long-lived cells in the first week of life via GM-CSF. J. Exp. Med. 210, 1977–1992 (2013).
Hussell, T. & Bell, T. J. Alveolar macrophages: plasticity in a tissue-specific context. Nat. Rev. Immunol. 14, 81–93 (2014).
Westphalen, K. et al. Sessile alveolar macrophages communicate with alveolar epithelium to modulate immunity. Nature 506, 503–506 (2014).
Mordstein, M. et al. Lambda interferon renders epithelial cells of the respiratory and gastrointestinal tracts resistant to viral infections. J. Virol. 84, 5670–5677 (2010).
Khaitov, M. R. et al. Respiratory virus induction of alpha-, beta- and lambda-interferons in bronchial epithelial cells and peripheral blood mononuclear cells. Allergy 64, 375–386 (2009).
Odendall, C. et al. Diverse intracellular pathogens activate type III interferon expression from peroxisomes. Nat. Immunol. 15, 717–726 (2014).
Odendall, C. & Kagan, J. C. The unique regulation and functions of type III interferons in antiviral immunity. Curr. Opin. Virol. 12, 47–52 (2015).
Ueki, I. F. et al. Respiratory virus-induced EGFR activation suppresses IRF1-dependent interferon λ and antiviral defense in airway epithelium. J. Exp. Med. 210, 1929–1936 (2013).
Sugimoto, N., Mitoma, H., Kim, T., Hanabuchi, S. & Liu, Y. J. Helicase proteins DHX29 and RIG-I cosense cytosolic nucleic acids in the human airway system. Proc. Natl Acad. Sci. USA 111, 7747–7752 (2014).
Liu, Y. J. IPC: professional type 1 interferon-producing cells and plasmacytoid dendritic cell precursors. Annu. Rev. Immunol. 23, 275–306 (2005).
Wang, H., Peters, N. & Schwarze, J. Plasmacytoid dendritic cells limit viral replication, pulmonary inflammation, and airway hyperresponsiveness in respiratory syncytial virus infection. J. Immunol. 177, 6263–6270 (2006).
Kaminski, M. M., Ohnemus, A., Cornitescu, M. & Staeheli, P. Plasmacytoid dendritic cells and Toll-like receptor 7-dependent signalling promote efficient protection of mice against highly virulent influenza A virus. J. Gen. Virol. 93, 555–559 (2012).
Juarez, E. et al. Differential expression of Toll-like receptors on human alveolar macrophages and autologous peripheral monocytes. Respir. Res. 11, 2 (2010).
Goritzka, M. et al. Alveolar macrophage-derived type I interferons orchestrate innate immunity to RSV through recruitment of antiviral monocytes. J. Exp. Med. 212, 699–714 (2015). This study uses a mouse respiratory syncytial virus system to show that type I IFNs released from alveolar macrophages induce the expression of CCL2, which is necessary for inflammatory monocyte recruitment and viral clearance.
Happel, K. I. et al. Divergent roles of IL-23 and IL-12 in host defense against Klebsiella pneumoniae. J. Exp. Med. 202, 761–769 (2005).
Neyt, K. & Lambrecht, B. N. The role of lung dendritic cell subsets in immunity to respiratory viruses. Immunol. Rev. 255, 57–67 (2013).
Thornton, E. E. et al. Spatiotemporally separated antigen uptake by alveolar dendritic cells and airway presentation to T cells in the lung. J. Exp. Med. 209, 1183–1199 (2012).
Vermaelen, K. Y., Carro-Muino, I., Lambrecht, B. N. & Pauwels, R. A. Specific migratory dendritic cells rapidly transport antigen from the airways to the thoracic lymph nodes. J. Exp. Med. 193, 51–60 (2001).
Persson, E. K. et al. IRF4 transcription-factor-dependent CD103+ CD11b+ dendritic cells drive mucosal T helper 17 cell differentiation. Immunity 38, 958–969 (2013).
Bafica, A. et al. TLR9 regulates Th1 responses and cooperates with TLR2 in mediating optimal resistance to Mycobacterium tuberculosis. J. Exp. Med. 202, 1715–1724 (2005).
Kandasamy, M. et al. Complement mediated signaling on pulmonary CD103+ dendritic cells is critical for their migratory function in response to influenza infection. PLoS Pathog. 9, e1003115 (2013).
Ichinohe, T. et al. Microbiota regulates immune defense against respiratory tract influenza A virus infection. Proc. Natl Acad. Sci. USA 108, 5354–5359 (2011).
Chen, I. Y. & Ichinohe, T. Response of host inflammasomes to viral infection. Trends Microbiol. 23, 55–63 (2015).
von Moltke, J., Ayres, J. S., Kofoed, E. M., Chavarria-Smith, J. & Vance, R. E. Recognition of bacteria by inflammasomes. Annu. Rev. Immunol. 31, 73–106 (2013).
Hammad, H. et al. House dust mite allergen induces asthma via Toll-like receptor 4 triggering of airway structural cells. Nat. Med. 15, 410–416 (2009).
Nathan, A. T., Peterson, E. A., Chakir, J. & Wills-Karp, M. Innate immune responses of airway epithelium to house dust mite are mediated through β-glucan-dependent pathways. J. Allergy Clin. Immunol. 123, 612–618 (2009).
Voehringer, D. Protective and pathological roles of mast cells and basophils. Nat. Rev. Immunol. 13, 362–375 (2013).
Allakhverdi, Z. et al. Thymic stromal lymphopoietin is released by human epithelial cells in response to microbes, trauma, or inflammation and potently activates mast cells. J. Exp. Med. 204, 253–258 (2007).
Moussion, C., Ortega, N. & Girard, J.-P. The IL-1-like cytokine IL-33 is constitutively expressed in the nucleus of endothelial cells and epithelial cells in vivo: a novel 'alarmin'? PLoS ONE 3, e3331 (2008).
Byers, D. E. et al. Long-term IL-33-producing epithelial progenitor cells in chronic obstructive lung disease. J. Clin. Invest. 123, 3967–3982 (2013).
Haenuki, Y. et al. A critical role of IL-33 in experimental allergic rhinitis. J. Allergy Clin. Immunol. 130, 184–194. e111 (2012).
Snelgrove, R. J. et al. Alternaria-derived serine protease activity drives IL-33-mediated asthma exacerbations. J. Allergy Clin. Immunol. 134, 583–592. e586 (2014).
Lüthi, A. U. et al. Suppression of interleukin-33 bioactivity through proteolysis by apoptotic caspases. Immunity 31, 84–98 (2009).
Kakkar, R., Hei, H., Dobner, S. & Lee, R. T. Interleukin 33 as a mechanically responsive cytokine secreted by living cells. J. Biol. Chem. 287, 6941–6948 (2012).
Kouzaki, H., O'Grady, S. M., Lawrence, C. B. & Kita, H. Proteases induce production of thymic stromal lymphopoietin by airway epithelial cells through protease-activated receptor-2. J. Immunol. 183, 1427–1434 (2009).
Barlow, J. L. et al. IL-33 is more potent than IL-25 in provoking IL-13-producing nuocytes (type 2 innate lymphoid cells) and airway contraction. J. Allergy Clin. Immunol. 132, 933–941 (2013).
Tamachi, T. et al. IL-25 enhances allergic airway inflammation by amplifying a TH2 cell-dependent pathway in mice. J. Allergy Clin. Immunol. 118, 606–614 (2006).
Mohapatra, A. et al. Group 2 innate lymphoid cells utilize the IRF4–IL-9 module to coordinate epithelial cell maintenance of lung homeostasis. Mucosal Immunol. 9, 275–286 (2016).
Denney, L. et al. Pulmonary epithelial cell-derived cytokine TGF-β1 is a critical cofactor for enhanced innate lymphoid cell function. Immunity 43, 945–958 (2015). This study shows that TGF β is released from AECs upon allergen exposure, and is necessary for ILC2 proliferation and cytokine production and for subsequent type 2 immunity.
Kotas, M. E. & Medzhitov, R. Homeostasis, inflammation, and disease susceptibility. Cell 160, 816–827 (2015).
De Grove, K. C. et al. Characterization and quantification of innate lymphoid cell subsets in human lung. PLoS ONE 11, e0145961 (2016).
Van Maele, L. et al. Activation of type 3 innate lymphoid cells and interleukin 22 secretion in the lungs during Streptococcus pneumoniae infection. J. Infect. Dis. 210, 493–503 (2014).
Pribul, P. K. et al. Alveolar macrophages are a major determinant of early responses to viral lung infection but do not influence subsequent disease development. J. Virol. 82, 4441–4448 (2008).
Zhou, G., Juang, S. W. W. & Kane, K. P. NK cells exacerbate the pathology of influenza virus infection in mice. Eur. J. Immunol. 43, 929–938 (2013).
Kumar, P., Thakar, M. S., Ouyang, W. & Malarkannan, S. IL-22 from conventional NK cells is epithelial regenerative and inflammation protective during influenza infection. Mucosal Immunol. 6, 69–82 (2013).
Coquet, J. M. et al. Diverse cytokine production by NKT cell subsets and identification of an IL-17- producing CD4−NK1.1− NKT cell population. Proc. Natl Acad. Sci. USA 105, 11287–11292 (2008).
Brigl, M. et al. Innate and cytokine-driven signals, rather than microbial antigens, dominate in natural killer T cell activation during microbial infection. J. Exp. Med. 208, 1163–1177 (2011).
Paget, C. et al. Interleukin-22 is produced by invariant natural killer T lymphocytes during influenza A virus infection: potential role in protection against lung epithelial damages. J. Biol. Chem. 287, 8816–8829 (2012).
Sutton, C. E. et al. Interleukin-1 and IL-23 induce innate IL-17 production from γδ T cells, amplifying Th17 responses and autoimmunity. Immunity 31, 331–341 (2009).
Lockhart, E., Green, A. M. & Flynn, J. L. IL-17 production is dominated by γδ T cells rather than CD4 T cells during Mycobacterium tuberculosis infection. J. Immunol. 177, 4662–4669 (2006).
Skeen, M. J. & Ziegler, H. K. Activation of gamma delta T cells for production of IFN-gamma is mediated by bacteria via macrophage-derived cytokines IL-1 and IL-12. J. Immunol. 154, 5832–5841 (1995). References 59 and 60 show that γδ T cells are the main source of the second-order cytokine IL-17, which is induced in response to the first-order cytokines IL-1 and IL-23.
Teijaro, J. R. et al. Cutting edge: tissue-retentive lung memory CD4 T cells mediate optimal protection to respiratory virus infection. J. Immunol. 187, 5510–5514 (2011).
Mjösberg, J. M. et al. Human IL-25-and IL-33-responsive type 2 innate lymphoid cells are defined by expression of CRTH2 and CD161. Nat. Immunol. 12, 1055–1062 (2011).
Neill, D. R. et al. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature 464, 1367–1370 (2010).
Halim, T. Y., Krauss, R. H., Sun, A. C. & Takei, F. Lung natural helper cells are a critical source of Th2 cell-type cytokines in protease allergen-induced airway inflammation. Immunity 36, 451–463 (2012).
Huang, Y. et al. IL-25-responsive, lineage-negative KLRG1hi cells are multipotential “inflammatory” type 2 innate lymphoid cells. Nat. Immunol. 16, 161–169 (2015).
Saenz, S. A. et al. IL-25 simultaneously elicits distinct populations of innate lymphoid cells and multipotent progenitor type 2 (MPPtype2) cells. J. Exp. Med. 210, 1823–1837 (2013).
Ohne, Y. et al. IL-1 is a critical regulator of group 2 innate lymphoid cell function and plasticity. Nat. Immunol. 17, 646–655 (2016).
Turner, J.-E. et al. IL-9-mediated survival of type 2 innate lymphoid cells promotes damage control in helminth-induced lung inflammation. J. Exp. Med. 210, 2951–2965 (2013).
Terashima, A. et al. A novel subset of mouse NKT cells bearing the IL-17 receptor B responds to IL-25 and contributes to airway hyperreactivity. J. Exp. Med. 205, 2727–2733 (2008).
Akbari, O. et al. Essential role of NKT cells producing IL-4 and IL-13 in the development of allergen-induced airway hyperreactivity. Nat. Med. 9, 582–588 (2003).
Pichavant, M. et al. Ozone exposure in a mouse model induces airway hyperreactivity that requires the presence of natural killer T cells and IL-17. J. Exp. Med. 205, 385–393 (2008).
Nagata, Y., Kamijuku, H., Taniguchi, M., Ziegler, S. & Seino, K.-I. Differential role of thymic stromal lymphopoietin in the induction of airway hyperreactivity and Th2 immune response in antigen-induced asthma with respect to natural killer T cell function. Int. Arch. Allergy Immunol. 144, 305–314 (2007).
Smithgall, M. D. et al. IL-33 amplifies both Th1-and Th2-type responses through its activity on human basophils, allergen-reactive Th2 cells, iNKT and NK cells. Int. Immunol. 20, 1019–1030 (2008).
Scanlon, S. T. et al. Airborne lipid antigens mobilize resident intravascular NKT cells to induce allergic airway inflammation. J. Exp. Med. 208, 2113–2124 (2011).
Kaplan, M. H., Hufford, M. M. & Olson, M. R. The development and in vivo function of T helper 9 cells. Nat. Rev. Immunol. 15, 295–307 (2015).
Yao, W. et al. Interleukin-9 is required for allergic airway inflammation mediated by the cytokine TSLP. Immunity 38, 360–372 (2013).
Kearley, J. et al. IL-9 governs allergen-induced mast cell numbers in the lung and chronic remodeling of the airways. Am. J. Respir. Crit. Care Med. 183, 865–875 (2011).
Coquet, J. M. et al. Interleukin-21-producing CD4+ Tcells promote Type 2 immunity to house dust mites. Immunity 43, 318–330 (2015).
Angkasekwinai, P., Chang, S. H., Thapa, M., Watarai, H. & Dong, C. Regulation of IL-9 expression by IL-25 signaling. Nat. Immunol. 11, 250–256 (2010).
Omori, M. & Ziegler, S. Induction of IL-4 expression in CD4+ T cells by thymic stromal lymphopoietin. J. Immunol. 178, 1396–1404 (2007).
Schmitz, J. et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity 23, 479–490 (2005). This study established IL-33 as a member of the IL-1 family, and demonstrated its signalling paradigm and its role in the eventual induction of second-order cytokines and type 2 immunity.
Nizzoli, G. et al. Human CD1c+ dendritic cells secrete high levels of IL-12 and potently prime cytotoxic T-cell responses. Blood 122, 932–942 (2013).
Aujla, S. J. et al. IL-22 mediates mucosal host defense against Gram-negative bacterial pneumonia. Nat. Med. 14, 275–281 (2008).
Aldridge, J. R. Jr. et al. TNF/iNOS-producing dendritic cells are the necessary evil of lethal influenza virus infection. Proc. Natl Acad. Sci. USA 106, 5306–5311 (2009).
Maus, U. A. et al. Monocytes are potent facilitators of alveolar neutrophil emigration during lung inflammation: role of the CCL2–CCR2 axis. J. Immunol. 170, 3273–3278 (2003).
Espinosa, V. et al. Inflammatory monocytes orchestrate innate antifungal immunity in the lung. PLoS Pathog. 10, e1003940 (2014).
Lin, K. L., Suzuki, Y., Nakano, H., Ramsburg, E. & Gunn, M. D. CCR2+ monocyte-derived dendritic cells and exudate macrophages produce influenza-induced pulmonary immune pathology and mortality. J. Immunol. 180, 2562–2572 (2008).
Landsman, L. & Jung, S. Lung macrophages serve as obligatory intermediate between blood monocytes and alveolar macrophages. J. Immunol. 179, 3488–3494 (2007).
Kreisel, D. et al. In vivo two-photon imaging reveals monocyte-dependent neutrophil extravasation during pulmonary inflammation. Proc. Natl Acad. Sci. USA 107, 18073–18078 (2010).
Sun, K., Salmon, S. L., Lotz, S. A. & Metzger, D. W. Interleukin-12 promotes gamma interferon-dependent neutrophil recruitment in the lung and improves protection against respiratory Streptococcus pneumoniae infection. Infect. Immun. 75, 1196–1202 (2007).
Bradley, L. M., Douglass, M. F., Chatterjee, D., Akira, S. & Baaten, B. J. Matrix metalloprotease 9 mediates neutrophil migration into the airways in response to influenza virus-induced Toll-like receptor signaling. PLoS Pathog. 8, e1002641 (2012).
Yipp, B. G. & Kubes, P. NETosis: how vital is it? Blood 122, 2784–2794 (2013).
Pillai, P. S. et al. Mx1 reveals innate pathways to antiviral resistance and lethal influenza disease. Science 352, 463–466 (2016).
Bruns, S. et al. Production of extracellular traps against Aspergillus fumigatus in vitro and in infected lung tissue is dependent on invading neutrophils and influenced by hydrophobin RodA. PLoS Pathog. 6, e1000873 (2010).
Li, L. et al. Effects of Th2 cytokines on chemokine expression in the lung: IL-13 potently induces eotaxin expression by airway epithelial cells. J. Immunol. 162, 2477–2487 (1999).
Kuperman, D. A. et al. Direct effects of interleukin-13 on epithelial cells cause airway hyperreactivity and mucus overproduction in asthma. Nat. Med. 8, 885–889 (2002). This study demonstrates that signal transducer and activator of transcription 6 (STAT6)-mediated IL-13 signalling in epithelial cells is critical for effector functions associated with airway hyperreactivity, including enhanced mucus production.
Monticelli, L. A. et al. Innate lymphoid cells promote lung-tissue homeostasis after infection with influenza virus. Nat. Immunol. 12, 1045–1054 (2011).
Pope, S. M. et al. IL-13 induces eosinophil recruitment into the lung by an IL-5- and eotaxin-dependent mechanism. J. Allergy Clin. Immunol. 108, 594–601 (2001).
Wong, C. K., Hu, S., Cheung, P. F. Y. & Lam, C. W. K. Thymic stromal lymphopoietin induces chemotactic and prosurvival effects in eosinophils. Am. J. Respir. Cell Mol. Biol. 43, 305–315 (2010).
Rosenberg, H. F., Dyer, K. D. & Foster, P. S. Eosinophils: changing perspectives in health and disease. Nat. Rev. Immunol. 13, 9–22 (2013).
Wakahara, K. et al. Basophils are recruited to inflamed lungs and exacerbate memory Th2 responses in mice and humans. Allergy 68, 180–189 (2013).
Motomura, Y. et al. Basophil-derived interleukin-4 controls the function of natural helper cells, a member of ILC2s, in lung inflammation. Immunity 40, 758–771 (2014).
Sharma, M. & Bayry, J. Autoimmunity: basophils in autoimmune and inflammatory diseases. Nat. Rev. Rheumatol. 11, 129–131 (2015).
Siracusa, M. C. et al. TSLP promotes interleukin-3-independent basophil haematopoiesis and type 2 inflammation. Nature 477, 229–233 (2011).
Lantz, C. S. et al. Role for interleukin-3 in mast-cell and basophil development and in immunity to parasites. Nature 392, 90–93 (1998).
Ohnmacht, C. & Voehringer, D. Basophils protect against reinfection with hookworms independently of mast cells and memory Th2 cells. J. Immunol. 184, 344–350 (2010).
Roy, A. et al. Mast cell chymase degrades the alarmins heat shock protein 70, biglycan, HMGB1, and interleukin-33 (IL-33) and limits danger-induced inflammation. J. Biol. Chem. 289, 237–250 (2014).
Morita, H. et al. An interleukin-33–mast cell–interleukin-2 axis suppresses papain-induced allergic inflammation by promoting regulatory T cell numbers. Immunity 43, 175–186 (2015).
Lefrançais, E. et al. Central domain of IL-33 is cleaved by mast cell proteases for potent activation of group-2 innate lymphoid cells. Proc. Natl Acad. Sci. USA 111, 15502–15507 (2014).
Medzhitov, R., Schneider, D. S. & Soares, M. P. Disease tolerance as a defense strategy. Science 335, 936–941 (2012).
Jamieson, A. M. et al. Role of tissue protection in lethal respiratory viral–bacterial coinfection. Science 340, 1230–1234 (2013). This study uses an influenza virus–bacteria co-infection model system to demonstrate that disease lethality can occur in the absence of changes in effective pathogen burden or control owing to impaired disease tolerance mechanisms.
Sivaraman, V. et al. Yersinia pestis activates both IL-1β and IL-1 receptor antagonist to modulate lung inflammation during pneumonic plague. PLoS Pathog. 11, e1004688 (2015).
Doitsh, G. et al. Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection. Nature 505, 509–514 (2014).
Wang, A. et al. Opposing effects of fasting metabolism on tissue tolerance in bacterial and viral inflammation. Cell 166, 1512–1525. e1512 (2016).
Foxman, E. F. et al. Temperature-dependent innate defense against the common cold virus limits viral replication at warm temperature in mouse airway cells. Proc. Natl Acad. Sci. USA 112, 827–832 (2015).
Foxman, E. F., Storer, J. A., Vanaja, K., Levchenko, A. & Iwasaki, A. Two interferon-independent double-stranded RNA-induced host defense strategies suppress the common cold virus at warm temperature. Proc. Natl Acad. Sci. USA 113, 8496–8501 (2016).
Jaspers, I. et al. Reduced expression of IRF7 in nasal epithelial cells from smokers after infection with influenza. Am. J. Respir. Cell Mol. Biol. 43, 368–375 (2010).
Bauer, C. M. et al. Cigarette smoke suppresses type I interferon-mediated antiviral immunity in lung fibroblast and epithelial cells. J. Interferon Cytokine Res. 28, 167–179 (2008).
Kearley, J. et al. Cigarette smoke silences innate lymphoid cell function and facilitates an exacerbated type I interleukin-33-dependent response to infection. Immunity 42, 566–579 (2015). This study shows how cigarette smoke alters IL-33 signalling by increasing epithelial IL-33 expression, decreasing ST2 expression on ILCs, and increasing ST2 expression on NK cells and macrophages; these effects predispose the lung to more readily engage inflammatory effector functions.
Lowery, E. M., Brubaker, A. L., Kuhlmann, E. & Kovacs, E. J. The aging lung. Clin. Interv. Aging 8, 1489–1496 (2013).
Shaw, A. C., Goldstein, D. R. & Montgomery, R. R. Age-dependent dysregulation of innate immunity. Nat. Rev. Immunol. 13, 875–887 (2013).
Zhao, J., Zhao, J., Legge, K. & Perlman, S. Age-related increases in PGD2 expression impair respiratory DC migration, resulting in diminished T cell responses upon respiratory virus infection in mice. J. Clin. Invest. 121, 4921–4930 (2011).
Beli, E. et al. Natural killer cell function is altered during the primary response of aged mice to influenza infection. Mech. Ageing Dev. 132, 503–510 (2011).
Gomez, C. R. et al. Advanced age exacerbates the pulmonary inflammatory response after lipopolysaccharide exposure. Crit. Care Med. 35, 246–251 (2007).
Brandes, M., Klauschen, F., Kuchen, S. & Germain, R. N. A systems analysis identifies a feedforward inflammatory circuit leading to lethal influenza infection. Cell 154, 197–212 (2013).
Camargo, C. A., Weiss, S. T., Zhang, S., Willett, W. C. & Speizer, F. E. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch. Intern. Med. 159, 2582–2588 (1999).
Manicone, A. M., Gong, K., Johnston, L. K. & Giannandrea, M. Diet-induced obesity alters myeloid cell populations in naïve and injured lung. Respir. Res. 17, 1–11 (2016).
Kim, H. Y. et al. Interleukin-17-producing innate lymphoid cells and the NLRP3 inflammasome facilitate obesity-associated airway hyperreactivity. Nat. Med. 20, 54–61 (2014). This study demonstrates that an increase in airway hyperreactivity in obese mice occurs as a consequence of NLRP3-mediated IL-1 β production, which, in turn, induces increased IL-17 production by ILC3s.
Ubags, N. D. et al. A comparative study of lung host defense in murine obesity models: insights into neutrophil function. Am. J. Respir. Cell Mol. Biol. 55, 188–200 (2016).
O'Brien, K. B. et al. Impaired wound healing predisposes obese mice to severe influenza virus infection. J. Infect. Dis. 205, 252–261 (2012).
Teran-Cabanillas, E., Montalvo-Corral, M., Caire-Juvera, G., Moya-Camarena, S. Y. & Hernández, J. Decreased interferon-α and interferon-β production in obesity and expression of suppressor of cytokine signaling. Nutrition 29, 207–212 (2013).
Besnard, A. G. et al. IL-33-activated dendritic cells are critical for allergic airway inflammation. Eur. J. Immunol. 41, 1675–1686 (2011).
Soumelis, V. et al. Human epithelial cells trigger dendritic cell-mediated allergic inflammation by producing TSLP. Nat. Immunol. 3, 673–680 (2002).
Halim, T. Y. F. et al. Group 2 innate lymphoid cells are critical for the initiation of adaptive T helper 2 cell-mediated allergic lung inflammation. Immunity 40, 425–435 (2014).
Plantinga, M. et al. Conventional and monocyte-derived CD11b+ dendritic cells initiate and maintain T helper 2 cell-mediated immunity to house dust mite allergen. Immunity 38, 322–335 (2013).
Kumamoto, Y. et al. CD301b+ dermal dendritic cells drive T helper 2 cell-mediated immunity. Immunity 39, 733–743 (2013).
Massacand, J. C. et al. Helminth products bypass the need for TSLP in Th2 immune responses by directly modulating dendritic cell function. Proc. Natl Acad. Sci. USA 106, 13968–13973 (2009).
Trompette, A. et al. Allergenicity resulting from functional mimicry of a Toll-like receptor complex protein. Nature 457, 585–588 (2009).
Shreffler, W. G. et al. The major glycoprotein allergen from Arachis hypogaea, Ara h 1, is a ligand of dendritic cell-specific ICAM-grabbing nonintegrin and acts as a Th2 adjuvant in vitro. J. Immunol. 177, 3677–3685 (2006).
Gern, J. E. The ABCs of rhinoviruses, wheezing, and asthma. J. Virol. 84, 7418–7426 (2010).
Wark, P. A. et al. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J. Exp. Med. 201, 937–947 (2005).
Contoli, M. et al. Role of deficient type III interferon-λ production in asthma exacerbations. Nat. Med. 12, 1023–1026 (2006).
Sykes, A. et al. Rhinovirus-induced interferon production is not deficient in well controlled asthma. Thorax 69, 240–246 (2014).
Edwards, M. R. et al. Impaired innate interferon induction in severe therapy resistant atopic asthmatic children. Mucosal Immunol. 6, 797–806 (2013).
Baraldo, S. et al. Deficient antiviral immune responses in childhood: distinct roles of atopy and asthma. J. Allergy Clin. Immunol. 130, 1307–1314 (2012).
Teo, S. M. et al. The infant nasopharyngeal microbiome impacts severity of lower respiratory infection and risk of asthma development. Cell Host Microbe 17, 704–715 (2015).
Headley, M. B. et al. Visualization of immediate immune responses to pioneer metastatic cells in the lung. Nature 531, 513–517 (2016).
Qian, B.-Z. et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 475, 222–225 (2011).
Spiegel, A. et al. Neutrophils suppress intraluminal NK-mediated tumor cell clearance and enhance extravasation of disseminated carcinoma cells. Cancer Discov. 6, 630–649 (2016).
Acuff, H. B., Carter, K. J., Fingleton, B., Gorden, D. L. & Matrisian, L. M. Matrix metalloproteinase-9 from bone marrow-derived cells contributes to survival but not growth of tumor cells in the lung microenvironment. Cancer Res. 66, 259–266 (2006).
Sharma, S. K. et al. Pulmonary alveolar macrophages contribute to the premetastatic niche by suppressing antitumor T cell responses in the lungs. J. Immunol. 194, 5529–5538 (2015).
Boers, J. E., Ambergen, A. W. & Thunnissen, F. B. Number and proliferation of clara cells in normal human airway epithelium. Am. J. Respir. Crit. Care Med. 159, 1585–1591 (1999).
Acknowledgements
The authors would like to thank the Howard Hughes Medical Institute and the US National Institutes of Health (NIH) for their support of research in the laboratory (grants AI054359 and HHSN272201100019C). E.F.F. was supported by funding from the NIH (grants T32 HL007974-11 and K08 AI119139-01). R.D.M. was supported by funding from the NIH (grants T32 AI007019-38 and T32 AI055403) and the Francis Trudeau Trainee Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- First-order cytokines
-
A group of cytokines released from the cells that initially sense the presence of a pathogen. These cytokines primarily function to alert tissue-resident lymphoid cell populations in order to coordinate an appropriate immune response to the pathogen.
- Innate lymphoid cells
-
(ILCs). A group of lymphoid cells that lack B and T cell receptors and are resident in a variety of different organs. They are a major source of second-order cytokines that maintain tissue homeostasis and promote effective microbial clearance.
- Second-order cytokines
-
A group of cytokines released from tissue-resident lymphoid cells in response to signals from first-order cytokines. These cytokines recruit effector cells, and activate effector and tissue-repair functions to help resolve infections.
- Type 1 immune responses
-
A group of related immune responses to viruses, bacteria, fungi and protozoa that are characterized by the cytokines interferon-γ, tumour necrosis factor, IL-17 and IL-22. These second-order cytokines are secreted by group 1 innate lymphoid cells, group 3 innate lymphoid cells, natural killer cells, natural killer T cells, innate-like lymphocytes, T helper 1 (TH1) cells and TH17 cells. Effectors also include cytotoxic T cells, which kill infected cells.
- Type 2 immune responses
-
A group of related immune responses to macroparasites, allergens and certain venoms that are characterized by the cytokines interleukin-4 (IL-4), IL-5, IL-9 and IL-13. These second-order cytokines are secreted by group 2 innate lymphoid cells, natural killer T cells, T helper 2 (TH2) cells and TH9 cells.
- Ciliated cells
-
The predominant cell type in the surface epithelium of the conducting airways. Cilia at the apical surface of these cells beat continuously in a coordinated manner to propel airway mucus towards the mouth and nose, where mucus (and entrapped particles) can be removed via coughing or swallowing.
- Goblet cells
-
Cells that produce airway mucins, the key components of the protective barrier that impedes pathogen entry into the airway epithelium.
- Club cells
-
Secretory cells (formerly known as Clara cells) that produce detoxifying and antimicrobial compounds that contribute to defence of the airway mucosa. Club cells have also been reported to function as progenitor cells with the ability to replicate and/or differentiate into ciliated cells.
- Basal cells
-
These cells function as regional progenitor cells of the airway epithelium and have the ability to proliferate in response to damage and differentiate into other surface epithelial cell types.
- Chronic obstructive pulmonary disease
-
A group of conditions — including chronic obstructive bronchitis and emphysema — characterized by the pathological limitation of airflow in the airway. It is most often caused by tobacco smoking, but can also be caused by other airborne irritants, such as coal dust, and occasionally by genetic abnormalities, such as α1-antitrypsin deficiency.
- Pattern recognition receptors
-
(PRRs). Germline-encoded receptors that recognize conserved pathogen-associated molecular patterns and activate signalling cascades that initiate an immune response.
- RIG-I-like receptors
-
(RLRs). A group of cytosolic pattern recognition receptors comprising retinoic acid-inducible gene I (RIG-I), melanoma differentiation-associated gene 5 (MDA5) and LGP2 (also known as DHX58), which recognize viral RNA in infected cells and initiate downstream inflammatory and interferon responses by signalling through mitochondrial antiviral signalling protein (MAVS).
- Plasmacytoid DCs
-
(pDCs). Specialized sensory cells that express Toll-like receptor 7 (TLR7) and TLR9, and rapidly produce large amounts of type I interferons in response to viral infection.
- Type I interferons
-
(Type I IFNs). Mammalian type I IFNs comprise IFNα (13 subtypes in humans), IFNβ, IFNκ, IFNδ, IFNε, IFNτ, IFNω and IFNζ. All these cytokines bind to and signal through the receptor consisting of the IFNα/β receptor 1 (IFNAR1)–IFNAR2 dimer and trigger the transcription of genes involved in antiviral defence (which are also known as IFN-stimulated genes).
- Type III IFNs
-
(Type III interferons). The type III IFNs IFNλ1, IFNλ2 and IFNλ3 are potent antiviral cytokines that are secreted by diverse cell types following pattern recognition receptor-mediated detection of viral infection. Upon binding to the IFNλ receptor (a heterodimer comprising interleukin-28 (IL-28) receptor subunit-α (also known as IFNλR1) and IL-10 receptor subunit-β), these IFNs trigger the transcription of genes involved in antiviral defence (which are also known as IFN-stimulated genes).
- Alarmins
-
Constitutively expressed molecules that are released upon cell membrane rupture and alert the immune system.
- Amphiregulin
-
(AREG). An epidermal growth factor (EGF)-like protein that promotes epithelial cell growth and tissue repair through EGF receptor signalling. AREG is important for promoting disease tolerance in lung infection models.
- Airway hyperresponsiveness
-
A pathological state in which narrowing of the conducting airways can be easily triggered. Airway hyperresponsiveness is a diagnostic feature of asthma and contributes to airway obstruction.
- Neutrophil extracellular traps
-
(NETs). An extracellular mesh of chromatin that contains histones, neutrophil-derived proteases and antimicrobial molecules. NETs are released from neutrophils in certain inflammatory scenarios, and are important for ensnaring and trapping extracellular pathogens.
- Chymase
-
A family of serine proteases that are primarily expressed by mast cells and released upon degranulation. They can initiate proteolytic degradation of numerous substrates, including IL-33 and the extracellular matrix.
- Disease tolerance
-
A host strategy for improving disease outcomes by improving tissue repair or reducing the detrimental impact of inflammatory signals.
- Metabolic syndrome
-
A set of risk factors — including obesity, elevated blood pressure and insulin resistance — that are associated with an increased risk of heart disease, diabetes and other negative clinical outcomes.
Rights and permissions
About this article
Cite this article
Iwasaki, A., Foxman, E. & Molony, R. Early local immune defences in the respiratory tract. Nat Rev Immunol 17, 7–20 (2017). https://doi.org/10.1038/nri.2016.117
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2016.117
This article is cited by
-
Airway and systemic biomarkers of health effects after short-term exposure to indoor ultrafine particles from cooking and candles – A randomized controlled double-blind crossover study among mild asthmatic subjects
Particle and Fibre Toxicology (2023)
-
Regeneration of tracheal neotissue in partially decellularized scaffolds
npj Regenerative Medicine (2023)
-
Remodeling and Restraining Lung Tissue Damage Through the Regulation of Respiratory Immune Responses
Tissue Engineering and Regenerative Medicine (2023)
-
A mammalian lung's immune system minimizes tissue damage by initiating five major sequential phases of defense
Clinical and Experimental Medicine (2023)
-
Myeloid DNA methyltransferase3b deficiency aggravates pulmonary fibrosis by enhancing profibrotic macrophage activation
Respiratory Research (2022)