Key Points
-
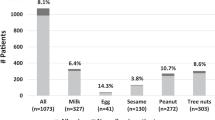
There are many forms of food allergy, the most common of which are IgE mediated. Common IgE-mediated food allergies include those to peanuts, tree nuts, cow's milk, egg, soy, wheat, shellfish and fish.
-
The immune system normally develops tolerance to food proteins, at least in part due to the actions of CD4+ regulatory T cells.
-
Food allergy develops when the immune system mounts a T helper 2 (TH2) cell-mediated response against food epitopes. TH2 cell sensitization may occur initially at the skin, rather than in the gastrointestinal tract.
-
The early introduction of potentially allergenic foods may prevent the development of food allergies.
-
Patients with established food allergy may become desensitized to food allergens by oral immunotherapy, which is thought to involve a shift from allergen-specific TH2 cells to CD4+ regulatory T cells, anergic cells and apoptotic cells. Typically, patients must continue regular consumption of food allergen to maintain desensitization.
-
Some desensitized individuals proceed to develop sustained unresponsiveness and no longer require regular ingestion of food allergen to maintain immune system nonresponsiveness. The mechanism and predictors of the transition from desensitization to apparent tolerance are unknown.
Abstract
Food allergy is a pathological, potentially deadly, immune reaction triggered by normally innocuous food protein antigens. The prevalence of food allergies is rising and the standard of care is not optimal, consisting of food-allergen avoidance and treatment of allergen-induced systemic reactions with adrenaline. Thus, accurate diagnosis, prevention and treatment are pressing needs, research into which has been catalysed by technological advances that are enabling a mechanistic understanding of food allergy at the cellular and molecular levels. We discuss the diagnosis and treatment of IgE-mediated food allergy in the context of the immune mechanisms associated with healthy tolerance to common foods, the inflammatory response underlying most food allergies, and immunotherapy-induced desensitization. We highlight promising research advances, therapeutic innovations and the challenges that remain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Thomsen, S. F. Epidemiology and natural history of atopic diseases. Eur. Clin. Respir. J. 2, 24642 (2015).
Anto, J. M. et al. Understanding the complexity of IgE-related phenotypes from childhood to young adulthood: a Mechanisms of the Development of Allergy (MeDALL) seminar. J. Allergy Clin. Immunol. 129, 943–954 (2012).
Alduraywish, S. A. et al. The march from early life food sensitization to allergic disease: a systematic review and meta-analyses of birth cohort studies. Allergy 71, 77–89 (2016).
Hill, D. A., Grundmeier, R. W., Ram, G. & Spergel, J. M. The epidemiologic characteristics of healthcare provider-diagnosed eczema, asthma, allergic rhinitis, and food allergy in children: a retrospective cohort study. BMC Pediatr. 16, 133 (2016).
Prescott, S. L. et al. A global survey of changing patterns of food allergy burden in children. World Allergy Organ. J. 6, 21 (2013).
Gupta, R. et al. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 167, 1026–1031 (2013).
Koplin, J. J., Mills, E. N. & Allen, K. J. Epidemiology of food allergy and food-induced anaphylaxis: is there really a Western world epidemic? Curr. Opin. Allergy Clin. Immunol. 15, 409–416 (2015).
Branum, A. M. & Lukacs, S. L. Food allergy among U. S. children: trends in prevalence and hospitalizations. NCHS data brief, no 10. Hyattsville, MD: National Center for Health Statistics (2008).
Jackson, K. D., Howie, L. D. & Akinbami, L. J. Trends in allergic conditions among children: United States, 1997–2011. CDC NCHS data brief, no 121. Hyattsville, MD: National Center for Health Statistics (2013).
Gupta, R. S. et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics 128, e9–e17 (2011).
Turner, P. J. et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992–2012. J. Allergy Clin. Immunol. 135, 956–963 (2015).
Mullins, R. J., Wainstein, B. K., Barnes, E. H., Liew, W. K. & Campbell, D. E. Increases in anaphylaxis fatalities in Australia 1997 to 2013. Clin. Exp. Allergy 46, 1099–1110 (2016).
Fox, A. T., Sasieni, P., du Toit, G., Syed, H. & Lack, G. Household peanut consumption as a risk factor for the development of peanut allergy. J. Allergy Clin. Immunol. 123, 417–423 (2009).
Brough, H. A. et al. Peanut protein in household dust is related to household peanut consumption and is biologically active. J. Allergy Clin. Immunol. 132, 630–638 (2013).
Benedé, S., Blázquez, A. B., Chiang, D., Tordesillas, L. & Berin, M. C. The rise of food allergy: environmental factors and emerging treatments. EBioMedicine 7, 27–34 (2016).
Boyce, J. A. et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J. Allergy Clin. Immunol. 126, S1-58 (2010).
Chinthrajah, R. S. et al. Diagnosis of food allergy. Pediatr. Clin. North Am. 62, 1393–1408 (2015).
Obeng, B. B. et al. Food allergy in Ghanaian schoolchildren: data on sensitization and reported food allergy. Int. Arch. Allergy Immunol. 155, 63–73 (2011).
Lee, A. J., Thalayasingam, M. & Lee, B. W. Food allergy in Asia: how does it compare? Asia Pac. Allergy 3, 3–14 (2013).
Stone, K. D., Prussin, C. & Metcalfe, D. D. IgE, mast cells, basophils, and eosinophils. J. Allergy Clin. Immunol. 125, S73–S80 (2010).
Sampson, H. A. et al. Second symposium on the definition and management of anaphylaxis: summary report — Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J. Allergy Clin. Immunol. 117, 391–397 (2006).
Ivkovic´-Jurekovic´, I. Oral allergy syndrome in children. Int. Dent. J. 65, 164–168 (2015).
Hurlburt, B. K. et al. Structure and function of the peanut panallergen Ara h 8. J. Biol. Chem. 288, 36890–36901 (2013).
Asarnoj, A. et al. Peanut component Ara h 8 sensitization and tolerance to peanut. J. Allergy Clin. Immunol. 130, 468–472 (2012).
Hofmann, C. et al. Cor a 1-reactive T cells and IgE are predominantly cross-reactive to Bet v 1 in patients with birch pollen-associated food allergy to hazelnut. J. Allergy Clin. Immunol. 131, 1384–1392 (2013).
Commins, S. P., Jerath, M. R., Cox, K., Erickson, L. D. & Platts-Mills, T. Delayed anaphylaxis to α-gal, an oligosaccharide in mammalian meat. Allergol. Int. 65, 16–20 (2016).
Steinke, J. W., Platts-Mills, T. A. & Commins, S. P. The alpha-gal story: lessons learned from connecting the dots. J. Allergy Clin. Immunol. 135, 589–596 (2015).
Sidbury, R. et al. Guidelines of care for the management of atopic dermatitis: section 4. Prevention of disease flares and use of adjunctive therapies and approaches. J. Am. Acad. Dermatol. 71, 1218–1233 (2014).
Spergel, J. M. Nonimmunoglobulin e-mediated immune reactions to foods. AAllergy Asthma Clin. Immunol. 2, 78–85 (2006).
Zuo, L. & Rothenberg, M. E. Gastrointestinal eosinophilia. Immunol. Allergy Clin. North Am. 27, 443–455 (2007).
Simon, D. et al. Eosinophilic esophagitis is characterized by a non-IgE-mediated food hypersensitivity. Allergy 71, 611–620 (2016).
Nowak-Wegrzyn, A., Katz, Y., Mehr, S. S. & Koletzko, S. Non-IgE-mediated gastrointestinal food allergy. J. Allergy Clin. Immunol. 135, 1114–1124 (2015).
Berin, M. C. & Sampson, H. A. Mucosal immunology of food allergy. Curr. Biol. 23, R389–R400 (2013).
du Toit, G., Tsakok, T., Lack, S. & Lack, G. Prevention of food allergy. J. Allergy Clin. Immunol. 137, 998–1010 (2016).
Pabst, O. & Mowat, A. M. Oral tolerance to food protein. Mucosal Immunol. 5, 232–239 (2012).
Menard, S., Cerf-Bensussan, N. & Heyman, M. Multiple facets of intestinal permeability and epithelial handling of dietary antigens. Mucosal Immunol. 3, 247–259 (2010).
McDole, J. R. et al. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature 483, 345–349 (2012).
Mabbott, N. A., Donaldson, D. S., Ohno, H., Williams, I. R. & Mahajan, A. Microfold (M) cells: important immunosurveillance posts in the intestinal epithelium. Mucosal Immunol. 6, 666–677 (2013).
Rescigno, M. et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat. Immunol. 2, 361–367 (2001).
Niess, J. H. et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science 307, 254–258 (2005).
Chinthrajah, R. S., Hernandez, J. D., Boyd, S. D., Galli, S. J. & Nadeau, K. C. Molecular and cellular mechanisms of food allergy and food tolerance. J. Allergy Clin. Immunol. 137, 984–997 (2016).
Warshaw, A. L., Walker, W. A. & Isselbacher, K. J. Protein uptake by the intestine: evidence for absorption of intact macromolecules. Gastroenterology 66, 987–992 (1974).
Steinbach, E. C. & Plevy, S. E. The role of macrophages and dendritic cells in the initiation of inflammation in IBD. Inflamm. Bowel Dis. 20, 166–175 (2014).
Mazzini, E., Massimiliano, L., Penna, G. & Rescigno, M. Oral tolerance can be established via gap junction transfer of fed antigens from CX3CR1+ macrophages to CD103+ dendritic cells. Immunity 40, 248–261 (2014). CX 3 CR1+ macrophages capture food antigens and transfer them to CD103+ DCs in a connexin 43- dependent manner, cooperating in the process of antigen capture and presentation that contributes to T reg cell differentiation involved in tolerance.
Schulz, O. et al. Intestinal CD103+, but not CX3CR1+, antigen sampling cells migrate in lymph and serve classical dendritic cell functions. J. Exp. Med. 206, 3101–3114 (2009).
Coombes, J. L. et al. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-β- and retinoic acid-dependent mechanism. J. Exp. Med. 204, 1757–1764 (2007).
Persson, E. K., Scott, C. L., Mowat, A. M. & Agace, W. W. Dendritic cell subsets in the intestinal lamina propria: ontogeny and function. Eur. J. Immunol. 43, 3098–3107 (2013).
Sun, C. M. et al. Small intestine lamina propria dendritic cells promote de novo generation of Foxp3 T reg cells via retinoic acid. J. Exp. Med. 204, 1775–1785 (2007).
Bakdash, G., Vogelpoel, L. T., van Capel, T. M., Kapsenberg, M. L. & de Jong, E. C. Retinoic acid primes human dendritic cells to induce gut-homing, IL-10-producing regulatory T cells. Mucosal Immunol. 8, 265–278 (2015).
Mucida, D. et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science 317, 256–260 (2007).
Worbs, T. et al. Oral tolerance originates in the intestinal immune system and relies on antigen carriage by dendritic cells. J. Exp. Med. 203, 519–527 (2006).
Kraus, T. A. et al. Induction of mucosal tolerance in Peyer's patch-deficient, ligated small bowel loops. J. Clin. Invest. 115, 2234–2243 (2005).
Spahn, T. W. et al. Mesenteric lymph nodes are critical for the induction of high-dose oral tolerance in the absence of Peyer's patches. Eur. J. Immunol. 32, 1109–1113 (2002).
Fujihashi, K. et al. Peyer's patches are required for oral tolerance to proteins. Proc. Natl Acad. Sci. USA 98, 3310–3315 (2001).
Hadeiba, H. et al. CCR9 expression defines tolerogenic plasmacytoid dendritic cells able to suppress acute graft-versus-host disease. Nat. Immunol. 9, 1253–1260 (2008).
Evans, T. I. & Reeves, R. K. All-trans-retinoic acid imprints expression of the gut-homing marker α4β7 while suppressing lymph node homing of dendritic cells. Clin. Vaccine Immunol. 20, 1642–1646 (2013).
Cassani, B. et al. Gut-tropic T cells that express integrin α4β7 and CCR9 are required for induction of oral immune tolerance in mice. Gastroenterology 141, 2109–2118 (2011).
Murai, M. et al. Interleukin 10 acts on regulatory T cells to maintain expression of the transcription factor Foxp3 and suppressive function in mice with colitis. Nat. Immunol. 10, 1178–1184 (2009).
Hadis, U. et al. Intestinal tolerance requires gut homing and expansion of FoxP3+ regulatory T cells in the lamina propria. Immunity 34, 237–246 (2011).
Kim, K. S. et al. Dietary antigens limit mucosal immunity by inducing regulatory T cells in the small intestine. Science 351, 858–863 (2016).
Syed, A. et al. Peanut oral immunotherapy results in increased antigen-induced regulatory T-cell function and hypomethylation of forkhead box protein 3 (FOXP3). J. Allergy Clin. Immunol. 133, 500–510 (2014). Hypomethylation of the FOXP3 locus of antigen-induced T reg cells may predict the achievement of operationally defined clinical tolerance during peanut OIT.
Noval Rivas, M. et al. Regulatory T cell reprogramming toward a Th2-cell-like lineage impairs oral tolerance and promotes food allergy. Immunity 42, 512–523 (2015). IL-4R signalling drives T reg cell reprogramming into T H 2-like cells and interferes with T reg cell-mediated suppression of mast cell activation and expansion; IL-4R inhibition has a role in T reg cell induction and the enforcement of tolerance, as shown in mouse models.
Van Overtvelt, L. et al. Assessment of Bet v 1-specific CD4+ T cell responses in allergic and nonallergic individuals using MHC class II peptide tetramers. J. Immunol. 180, 4514–4522 (2008).
Turcanu, V., Maleki, S. J. & Lack, G. Characterization of lymphocyte responses to peanuts in normal children, peanut-allergic children, and allergic children who acquired tolerance to peanuts. J. Clin. Invest. 111, 1065–1072 (2003).
Pulendran, B. & Artis, D. New paradigms in type 2 immunity. Science 337, 431–435 (2012).
Galli, S. J. & Tsai, M. IgE and mast cells in allergic disease. Nat. Med. 18, 693–704 (2012).
Oyoshi, M. K., Oettgen, H. C., Chatila, T. A., Geha, R. S. & Bryce, P. J. Food allergy: insights into etiology, prevention, and treatment provided by murine models. J. Allergy Clin. Immunol. 133, 309–317 (2014).
Paul, W. E. & Zhu, J. How are TH2-type immune responses initiated and amplified? Nat. Rev. Immunol. 10, 225–235 (2010).
Han, H., Thelen, T. D., Comeau, M. R. & Ziegler, S. F. Thymic stromal lymphopoietin-mediated epicutaneous inflammation promotes acute diarrhea and anaphylaxis. J. Clin. Invest. 124, 5442–5452 (2014).
Tordesillas, L. et al. Skin exposure promotes a Th2-dependent sensitization to peanut allergens. J. Clin. Invest. 124, 4965–4975 (2014).
Oyoshi, M. K., Larson, R. P., Ziegler, S. F. & Geha, R. S. Mechanical injury polarizes skin dendritic cells to elicit a TH2 response by inducing cutaneous thymic stromal lymphopoietin expression. J. Allergy Clin. Immunol. 126, 976–984 (2010).
Hammerschmidt, S. I. et al. Retinoic acid induces homing of protective T and B cells to the gut after subcutaneous immunization in mice. J. Clin. Invest. 121, 3051–3061 (2011).
Burks, A. W. et al. Update on allergy immunotherapy: American Academy of Allergy, Asthma and Immunology/European Academy of Allergy and Clinical Immunology/PRACTALL consensus report. J. Allergy Clin. Immunol. 131, 1288–1296 (2013).
Jones, S. M. et al. Clinical efficacy and immune regulation with peanut oral immunotherapy. J. Allergy Clin. Immunol. 124, 292–300 (2009).
Akdis, M. & Akdis, C. A. Mechanisms of allergen-specific immunotherapy: multiple suppressor factors at work in immune tolerance to allergens. J. Allergy Clin. Immunol. 133, 621–631 (2014).
Akdis, C. A. & Akdis, M. Mechanisms of allergen-specific immunotherapy and immune tolerance to allergens. World Allergy Organ. J. 8, 17 (2015).
Ryan, J. F. et al. Successful immunotherapy induces previously unidentified allergen-specific CD4+ T-cell subsets. Proc. Natl Acad. Sci. USA 113, E1286–E1295 (2016). Antigen-specific CD4+ T cells transition from allergic and regulatory phenotypes to an anergic T H 2-cell phenotype that is largely absent in both pretreatment participants and healthy controls, as patients develop sustained unresponsiveness via OIT.
Wambre, E. et al. Specific immunotherapy modifies allergen-specific CD4+ T-cell responses in an epitope-dependent manner. J. Allergy Clin. Immunol. 133, 872–879 (2014). In allergen-specific immunotherapy, allergen-specific T H 2 cells are preferentially deleted whereas the frequencies of T H 1 and Tr1 cells are not significantly changed.
Wambre, E. Effect of allergen-specific immunotherapy on CD4+ T cells. Curr. Opin. Allergy Clin. Immunol. 15, 581–587 (2015).
Kwok, W. W. Modulation of Peanut-specific humoral and cellular responses pre- and post-oral immunotherapy. Clin. Exp. Allergy 45, 1146–1149 (2015).
Gutgemann, I., Fahrer, A. M., Altman, J. D., Davis, M. M. & Chien, Y. H. Induction of rapid T cell activation and tolerance by systemic presentation of an orally administered antigen. Immunity 8, 667–673 (1998).
Wisniewski, J. A. et al. Analysis of cytokine production by peanut-reactive T cells identifies residual Th2 effectors in highly allergic children who received peanut oral immunotherapy. Clin. Exp. Allergy 45, 1201–1213 (2015).
Itoh, N., Itagaki, Y. & Kurihara, K. Rush specific oral tolerance induction in school-age children with severe egg allergy: one year follow up. Allergol. Int. 59, 43–51 (2010).
Berin, M. C. & Shreffler, W. G. Mechanisms underlying induction of tolerance to foods. Immunol. Allergy Clin. North Am. 36, 87–102 (2016).
Dioszeghy, V. et al. Differences in phenotype, homing properties and suppressive activities of regulatory T cells induced by epicutaneous, oral or sublingual immunotherapy in mice sensitized to peanut. Cell. Mol. Immunol. 13, 1–13 (2016).
Sugimoto, M. et al. Differential response in allergen-specific IgE, IgGs, and IgA levels for predicting outcome of oral immunotherapy. Pediatr. Allergy Immunol. 27, 276–282 (2016).
Burton, O. T. et al. Oral immunotherapy induces IgG antibodies that act through FcγRIIb to suppress IgE-mediated hypersensitivity. J. Allergy Clin. Immunol. 134, 1310–1317 (2014). IgG in sera from patients with peanut allergies undergoing OIT suppresses peanut-induced basophil activation.
Santos, A. F. et al. IgG4 inhibits peanut-induced basophil and mast cell activation in peanut-tolerant children sensitized to peanut major allergens. J. Allergy Clin. Immunol. 135, 1249–1256 (2015).
Hoh, R. A. et al. Single B-cell deconvolution of peanut-specific antibody responses in allergic patients. J. Allergy Clin. Immunol. 137, 157–167 (2016).
van de Veen, W. et al. IgG4 production is confined to human IL-10-producing regulatory B cells that suppress antigen-specific immune responses. J. Allergy Clin. Immunol. 131, 1204–1212 (2013).
Konstantinou, G. N. et al. Egg-white-specific IgA and IgA2 antibodies in egg-allergic children: is there a role in tolerance induction? Pediatr. Allergy Immunol. 25, 64–70 (2014).
Hamilton, R., G. & Adkinson, N. F. Jr. In vitro assays for the diagnosis of IgE-mediated disorders. J. Allergy Clin. Immunol. 114, 213–225 (2004).
Spergel, J. M. et al. Food allergy in infants with atopic dermatitis: limitations of food-specific IgE measurements. Pediatrics 136, e1530–e1538 (2015).
Roberts, G. & Lack, G. Diagnosing peanut allergy with skin prick and specific IgE testing. J. Allergy Clin. Immunol. 115, 1291–1296 (2005).
Kattan, J. D. & Wang, J. Allergen component testing for food allergy: ready for prime time? Curr. Allergy Asthma Rep. 13, 58–63 (2013).
Tuano, K. S. & Davis, C. M. Utility of component-resolved diagnostics in food allergy. Curr. Allergy Asthma Rep. 15, 32 (2015).
Santos, A. F. et al. Basophil activation test discriminates between allergy and tolerance in peanut-sensitized children. J. Allergy Clin. Immunol. 134, 645–652 (2014).
Suratannon, N., Ngamphaiboon, J., Wongpiyabovorn, J., Puripokai, P. & Chatchatee, P. Component-resolved diagnostics for the evaluation of peanut allergy in a low-prevalence area. Pediatr. Allergy Immunol. 24, 665–670 (2013).
Wright, B. L. et al. Component-resolved analysis of IgA, IgE, and IgG4 during egg OIT identifies markers associated with sustained unresponsiveness. Allergy 71, 1552–1560 (2016).
Lack, G. Update on risk factors for food allergy. J. Allergy Clin. Immunol. 129, 1187–1197 (2012).
Bunyavanich, S. et al. Peanut, milk, and wheat intake during pregnancy is associated with reduced allergy and asthma in children. J. Allergy Clin. Immunol. 133, 1373–1382 (2014).
Roduit, C. et al. Increased food diversity in the first year of life is inversely associated with allergic diseases. J. Allergy Clin. Immunol. 133, 1056–1064 (2014).
Du Toit, G. et al. Effect of avoidance on peanut allergy after early peanut consumption. N. Engl. J. Med. 374, 1435–1443 (2016).
Du Toit, G. et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 372, 803–813 (2015).
Fleischer, D. M. et al. Consensus communication on early peanut introduction and the prevention of peanut allergy in high-risk infants. J. Allergy Clin. Immunol. 136, 258–261 (2015).
Perkin, M. R. et al. Enquiring About Tolerance (EAT) study: feasibility of an early allergenic food introduction regimen. J. Allergy Clin. Immunol. 137, 1477–1486 (2016).
Kramer, M. S. & Kakuma, R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Cochrane Database Syst. Rev. 9, CD000133 (2012).
Gensollen, T., Iyer, S. S., Kasper, D. L. & Blumberg, R. S. How colonization by microbiota in early life shapes the immune system. Science 352, 539–544 (2016).
Shen, N. & Clemente, J. C. Engineering the microbiome: a novel approach to immunotherapy for allergic and immune diseases. Curr. Allergy Asthma Rep. 15, 39 (2015).
Metsala, J. et al. Mother's and offspring's use of antibiotics and infant allergy to cow's milk. Epidemiology 24, 303–309 (2013).
Berni Canani, R. et al. Lactobacillus rhamnosus GG-supplemented formula expands butyrate-producing bacterial strains in food allergic infants. ISME J. 10, 742–750 (2016).
Ling, Z. et al. Altered fecal microbiota composition associated with food allergy in infants. Appl. Environ. Microbiol. 80, 2546–2554 (2014).
Azad, M. B. et al. Infant gut microbiota and food sensitization: associations in the first year of life. Clin. Exp. Allergy 45, 632–643 (2015).
Marrs, T. et al. Is there an association between microbial exposure and food allergy? A systematic review. Pediatr. Allergy Immunol. 24, 311–320 (2013).
Fiocchi, A. et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): probiotics. World Allergy Organ. J. 8, 4 (2015).
Vassallo, M. F. & Camargo, C. A. Jr. Potential mechanisms for the hypothesized link between sunshine, vitamin D, and food allergy in children. J. Allergy Clin. Immunol. 126, 217–222 (2010).
Allen, K. J. & Koplin, J. J. Prospects for prevention of food allergy. J. Allergy Clin. Immunol. Pract. 4, 215–220 (2016).
Koplin, J. J. et al. The impact of family history of allergy on risk of food allergy: a population-based study of infants. Int. J. Environ. Res. Public Health 10, 5364–5377 (2013).
Marenholz, I. et al. Filaggrin loss-of-function mutations predispose to phenotypes involved in the atopic march. J. Allergy Clin. Immunol. 118, 866–871 (2006).
Venkataraman, D. et al. Filaggrin loss-of-function mutations are associated with food allergy in childhood and adolescence. J. Allergy Clin. Immunol. 134, 876–882 (2014).
Horimukai, K. et al. Application of moisturizer to neonates prevents development of atopic dermatitis. J. Allergy Clin. Immunol. 134, 824–830 (2014).
Leung, D. Y. & Guttman-Yassky, E. Deciphering the complexities of atopic dermatitis: shifting paradigms in treatment approaches. J. Allergy Clin. Immunol. 134, 769–779 (2014).
Marenholz, I. et al. Meta-analysis identifies seven susceptibility loci involved in the atopic march. Nat. Commun. 6, 8804 (2015).
Ho, M. H., Wong, W. H. & Chang, C. Clinical spectrum of food allergies: a comprehensive review. Clin. Rev. Allergy Immunol. 46, 225–240 (2014).
Lieberman, P. Biphasic anaphylactic reactions. Ann. Allergy Asthma Immunol. 95, 217–226 (2005).
Enrique, E. et al. Sublingual immunotherapy for hazelnut food allergy: a randomized, double-blind, placebo-controlled study with a standardized hazelnut extract. J. Allergy Clin. Immunol. 116, 1073–1079 (2005).
Fleischer, D. M. et al. Sublingual immunotherapy for peanut allergy: a randomized, double-blind, placebo-controlled multicenter trial. J. Allergy Clin. Immunol. 131, 119–127 (2013).
Burks, A. W. et al. Oral immunotherapy for treatment of egg allergy in children. N. Engl. J. Med. 367, 233–243 (2012).
Sindher, S., Fleischer, D. M. & Spergel, J. M. Advances in the treatment of food allergy: sublingual and epicutaneous immunotherapy. Immunol. Allergy Clin. North Am. 36, 39–54 (2016).
Pennington, L. F. et al. Structural basis of omalizumab therapy and omalizumab-mediated IgE exchange. Nat. Commun. 7, 11610 (2016). The crystal structure of the complex of IgE with omalizumab is presented and used to generate a mutant omalizumab-resistant IgE–Fc fragment which, in combination with omalizumab, more efficiently blocks basophil activation than does either agent alone.
Nadeau, K. C., Schneider, L. C., Hoyte, L., Borras, I. & Umetsu, D. T. Rapid oral desensitisation in combination with omalizumab therapy in patients with cow's milk allergy. J. Allergy Clin. Immunol. 127, 1622–1624 (2011).
Schneider, L. C. et al. A pilot study of omalizumab to facilitate rapid oral desensitisation in high-risk peanut-allergic patients. J. Allergy Clin. Immunol. 132, 1368–1374 (2013).
Wood, R. A. et al. A randomized, double-blind, placebo-controlled study of omalizumab combined with oral immunotherapy for the treatment of cow's milk allergy. J. Allergy Clin. Immunol. 137, 1103–1110 (2016).
Bégin, P. et al. Phase 1 results of safety and tolerability in a rush oral immunotherapy protocol to multiple foods using omalizumab. Allergy Asthma Clin. Immunol. 10, 7 (2014). The first study to use omalizumab with OIT to multiple allergens simultaneously demonstrates the safe and rapid desensitization of patients with multiple food allergies.
Logsdon, S. L. & Oettgen, H. C. Anti-IgE therapy: clinical utility and mechanistic insights. Curr. Top. Microbiol. Immunol. 388, 39–61 (2015).
Assa'ad, A. H. et al. An antibody against IL-5 reduces numbers of esophageal intraepithelial eosinophils in children with eosinophilic esophagitis. Gastroenterology 141, 1593–1604 (2011).
Spergel, J. M. et al. Reslizumab in children and adolescents with eosinophilic esophagitis: results of a double-blind, randomized, placebo-controlled trial. J. Allergy Clin. Immunol. 129, 456–463 (2012).
Cox, L., Compalati, E., Kundig, T. & Larche, M. New directions in immunotherapy. Curr. Allergy Asthma Rep. 13, 178–195 (2013).
Chu, D. K. et al. IL-33, but not thymic stromal lymphopoietin or IL-25, is central to mite and peanut allergic sensitization. J. Allergy Clin. Immunol. 131, 187–200 (2013).
Burton, O. T. et al. Immunoglobulin E signal inhibition during allergen ingestion leads to reversal of established food allergy and induction of regulatory T cells. Immunity 41, 141–151 (2014). In a mouse model, mutations in IL-4R α impaired T reg cell induction; a mast-cell-specific deletion of Syk , which is essential for Fc ɛ RI signalling, restored the induction of tolerance-promoting T reg cells.
Zitnik, S. E. et al. IL13 variants are associated with total serum IgE and early sensitization to food allergens in children with atopic dermatitis. Pediatr. Allergy Immunol. 20, 551–555 (2009).
Wenzel, S. et al. Dupilumab in persistent asthma with elevated eosinophil levels. N. Engl. J. Med. 368, 2455–2466 (2013).
Beck, L. A. et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N. Engl. J. Med. 371, 130–139 (2014).
Bae, M. J., Shin, H. S., Kim, E. K., Kim, J. & Shon, D. H. Oral administration of chitin and chitosan prevents peanut-induced anaphylaxis in a murine food allergy model. Int. J. Biol. Macromol. 61, 164–168 (2013).
Ibañez, A. E. et al. Unlipidated outer membrane protein Omp16 (U-Omp16) from Brucella spp. as nasal adjuvant induces a Th1 immune response and modulates the Th2 allergic response to cow's milk proteins. PLoS ONE 8, e69438 (2013).
Grela, F. et al. The TLR7 agonist R848 alleviates allergic inflammation by targeting invariant NKT cells to produce IFN-γ. J. Immunol. 186, 284–290 (2011).
Pali-Scholl, I. et al. Protamine nanoparticles with CpG-oligodeoxynucleotide prevent an allergen-induced Th2-response in BALB/c mice. Eur. J. Pharm. Biopharm. 85, 656–664 (2013).
Creticos, P. S. et al. Immunotherapy with a ragweed-toll-like receptor 9 agonist vaccine for allergic rhinitis. N. Engl. J. Med. 355, 1445–1455 (2006).
Patel, P., Holdich, T., Fischer von Weikersthal-Drachenberg, K. J. & Huber, B. Efficacy of a short course of specific immunotherapy in patients with allergic rhinoconjunctivitis to ragweed pollen. J. Allergy Clin. Immunol. 133, 121–129 (2014).
Hall, I. P. et al. Efficacy of BI 671800, an oral CRTH2 antagonist, in poorly controlled asthma as sole controller and in the presence of inhaled corticosteroid treatment. Pulm. Pharmacol. Ther. 32, 37–44 (2015).
Krug, N. et al. Efficacy of the oral chemoattractant receptor homologous molecule on TH2 cells antagonist BI 671800 in patients with seasonal allergic rhinitis. J. Allergy Clin. Immunol. 133, 414–419 (2014).
Roy, K., Mao, H. Q., Huang, S. K. & Leong, K. W. Oral gene delivery with chitosan — DNA nanoparticles generates immunologic protection in a murine model of peanut allergy. Nat. Med. 5, 387–391 (1999).
von Moltke, J., Ji, M., Liang, H. E. & Locksley, R. M. Tuft-cell-derived IL-25 regulates an intestinal ILC2- epithelial response circuit. Nature 529, 221–225 (2016).
Frossard, C. P., Asigbetse, K. E., Burger, D. & Eigenmann, P. A. Gut T cell receptor-γδ+ intraepithelial lymphocytes are activated selectively by cholera toxin to break oral tolerance in mice. Clin. Exp. Immunol. 180, 118–130 (2015).
Mishra, A., Schlotman, J., Wang, M. & Rothenberg, M. E. Critical role for adaptive T cell immunity in experimental eosinophilic esophagitis in mice. J. Leukoc. Biol. 81, 916–924 (2007).
Yamada, A. et al. Antigen-primed splenic CD8+ T cells impede the development of oral antigen-induced allergic diarrhea. J. Allergy Clin. Immunol. 123, 889–894 (2009).
Divekar, R. & Kita, H. Recent advances in epithelium-derived cytokines (IL-33, IL-25, and thymic stromal lymphopoietin) and allergic inflammation. Curr. Opin. Allergy Clin. Immunol. 15, 98–103 (2015).
Palmer, C. N. et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat. Genet. 38, 441–446 (2006).
Irvine, A. D., McLean, W. H. & Leung, D. Y. Filaggrin mutations associated with skin and allergic diseases. N. Engl. J. Med. 365, 1315–1327 (2011).
Lund, S. Walford, H. H. & Doherty, T. A. Type 2 innate lymphoid cells in allergic disease. Curr. Immunol. Rev. 9, 214–221 (2013).
Zhang, Y. et al. Cord blood monocyte-derived inflammatory cytokines suppress IL-2 and induce nonclassic “TH2-type” immunity associated with development of food allergy. Sci. Transl Med. 8, 321ra8 (2016).
Mortha, A. et al. Microbiota-dependent crosstalk between macrophages and ILC3 promotes intestinal homeostasis. Science 343, 1249288 (2014).
Zigmond, E. et al. Macrophage-restricted interleukin-10 receptor deficiency, but not IL-10 deficiency, causes severe spontaneous colitis. Immunity 40, 720–733 (2014).
Rosenblum, M. D., Way, S. S. & Abbas, A. K. Regulatory T cell memory. Nat. Rev. Immunol. 16, 90–101 (2016).
Sakaguchi, S., Yamaguchi, T., Nomura, T. & Ono, M. Regulatory T cells and immune tolerance. Cell 133, 775–787 (2008).
Frossard, C. P., Hauser, C. & Eigenmann, P. A. Antigen-specific secretory IgA antibodies in the gut are decreased in a mouse model of food allergy. J. Allergy Clin. Immunol. 114, 377–382 (2004).
Urb, M. & Sheppard, D. C. The role of mast cells in the defence against pathogens. PLoS Pathog. 8, e1002619 (2012).
Weiner, H. L., da Cunha, A. P., Quintana, F. & Wu, H. Oral tolerance. Immunol. Rev. 241, 241–259 (2011).
Crotty, S. T follicular helper cell differentiation, function, and roles in disease. Immunity 41, 529–542 (2014).
Chung, Y. et al. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat. Med. 17, 983–988 (2011).
Ballesteros-Tato, A. et al. T follicular helper cell plasticity shapes pathogenic T helper 2 cell-mediated immunity to inhaled house dust mite. Immunity 44, 259–273 (2016).
Hirota, K. et al. Plasticity of TH17 cells in Peyer's patches is responsible for the induction of T cell-dependent IgA responses. Nat. Immunol. 14, 372–379 (2013).
Ito, T. et al. TSLP-activated dendritic cells induce an inflammatory T helper type 2 cell response through OX40 ligand. J. Exp. Med. 202, 1213–1223 (2005).
Klose, C. S. & Artis, D. Innate lymphoid cells as regulators of immunity, inflammation and tissue homeostasis. Nat. Immunol. 17, 765–774 (2016).
Mirchandani, A. S. et al. Type 2 innate lymphoid cells drive CD4+ Th2 cell responses. J. Immunol. 192, 2442–2448 (2014).
Sehra, S. et al. TH9 cells are required for tissue mast cell accumulation during allergic inflammation. J. Allergy Clin. Immunol. 136, 433–440 (2015).
Blumchen, K. et al. Oral peanut immunotherapy in children with peanut anaphylaxis. J. Allergy Clin. Immunol. 126, 83–91 (2010).
Meiler, F., Klunker, S., Zimmermann, M., Akdis, C. A. & Akdis, M. Distinct regulation of IgE, IgG4 and IgA by T regulatory cells and toll-like receptors. Allergy 63, 1455–1463 (2008).
James, L. K. et al. Long-term tolerance after allergen immunotherapy is accompanied by selective persistence of blocking antibodies. J. Allergy Clin. Immunol. 127, 509–516 (2011).
Nouri-Aria, K. T. et al. Grass pollen immunotherapy induces mucosal and peripheral IL-10 responses and blocking IgG activity. J. Immunol. 172, 3252–3259 (2004).
Vignali, D. A., Collison, L. W. & Workman, C. J. How regulatory T cells work. Nat. Rev. Immunol. 8, 523–532 (2008).
Gri, G. et al. CD4+CD25+ regulatory T cells suppress mast cell degranulation and allergic responses through OX40–OX40L interaction. Immunity 29, 771–781 (2008).
Eigenmann, P. A. & Calza, A. M. Diagnosis of IgE-mediated food allergy among Swiss children with atopic dermatitis. Pediatr. Allergy Immunol. 11, 95–100 (2000).
Silverberg, J. I. & Simpson, E. L. Association between severe eczema in children and multiple comorbid conditions and increased healthcare utilization. Pediatr. Allergy Immunol. 24, 476–486 (2013).
Hruz, P. Epidemiology of eosinophilic esophagitis. Dig. Dis. 32, 40–47 (2014).
Cianferoni, A. & Spergel, J. Eosinophilic esophagitis: a comprehensive review. Clin. Rev. Allergy Immunol. 50, 159–174 (2016).
Cianferoni, A. & Spergel, J. M. Eosinophilic esophagitis and gastroenteritis. Curr. Allergy Asthma Rep. 15, 58 (2015).
Katz, Y., Goldberg, M. R., Rajuan, N., Cohen, A. & Leshno, M. The prevalence and natural course of food protein-induced enterocolitis syndrome to cow's milk: a large-scale, prospective population-based study. J. Allergy Clin. Immunol. 127, 647–653 (2011).
Elizur, A. et al. Cow's milk associated rectal bleeding: a population based prospective study. Pediatr. Allergy Immunol. 23, 766–770 (2012).
Dupont, C. et al. Cow's milk epicutaneous immunotherapy in children: a pilot trial of safety, acceptability, and impact on allergic reactivity. J. Allergy Clin. Immunol. 125, 1165–1167 (2010).
Wood, R. A. et al. A phase 1 study of heat/phenol-killed, E. coli-encapsulated, recombinant modified peanut proteins Ara h 1, Ara h 2, and Ara h 3 (EMP-123) for the treatment of peanut allergy. Allergy 68, 803–808 (2013).
Acknowledgements
The authors would like to acknowledge the assistance of T. A. Chatila, S. J. Galli, M. T. Graham, V. Sampath and J. M. Spergel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Atopic diseases
-
Disorders characterized by pathological immune responses to normally innocuous antigens.
- Oral food challenge
-
(OFC). Used for food allergy diagnosis. Under supervision, the patient is asked to consume small but increasing amounts of the suspected food allergen until a predetermined maximum dose is reached or a food allergic reaction is observed.
- IgE component testing
-
Purified allergen extracts or recombinant allergens are used to diagnose food allergies in a more accurate manner than is possible with crude allergen extracts.
- Sustained unresponsiveness
-
The state in which an individual with food allergy no longer requires regular ingestion of an allergen to maintain desensitization to it; phenotypically, it resembles the normal immune tolerance of a healthy individual but may be mechanistically distinct.
- Gut-associated lymphoid tissue
-
(GALT). The immune system of the gastrointestinal tract is collectively called the GALT; examples include the tonsils, Peyer's patches and lymphoid cells in the lamina propria.
- Type 1 regulatory T cells
-
(Tr1 cells). A subset of regulatory T cells that are FOXP3−. Tr1 cells mediate suppressive effects through IL-10 secretion.
- Type 2 innate lymphoid cells
-
(ILC2s). Cells that produce T helper 2 cell cytokines, such as IL-4, IL-5, IL-9 and IL-13, and are implicated in the development of allergic inflammation.
- Sublingual immunotherapy
-
(SLIT). An immunotherapeutic method in which the food allergen (in the form of a tablet or drops) is administered under the tongue.
- Regulatory B cells
-
(Breg cells). These cells support immune tolerance through secretion of the anti-inflammatory cytokines IL-10, IL-35 and TGFβ.
- H1 receptor blockers
-
H1 receptor antagonists that block histamine action, dampening allergic reactions.
Rights and permissions
About this article
Cite this article
Yu, W., Freeland, D. & Nadeau, K. Food allergy: immune mechanisms, diagnosis and immunotherapy. Nat Rev Immunol 16, 751–765 (2016). https://doi.org/10.1038/nri.2016.111
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2016.111