Key Points
-
Haemangioma and focal nodular hyperplasia are the two most frequent benign liver lesions and only exceptionally require treatment, specific advice or follow-up
-
Hepatocellular adenoma, which now frequently occurs in obese females, is a heterogeneous liver lesion at risk of bleeding and malignant transformation according to the patients' gender and the pathological subtype and size of the tumour
-
In women, the low risk of complications associated with hepatocellular adenomas of <5 cm allows conservative management with regular follow-up
-
The accuracy of MRI now limits the use of biopsy for the diagnosis of hepatocellular adenoma, focal nodular hyperplasia or haemangioma
-
The uncertainty of imaging diagnosis for inflammatory pseudotumours of the liver, angiomyolipomas or in a setting of abnormal underlying liver parenchyma still justifies the routine use of liver biopsy
Abstract
More and more asymptomatic benign liver tumours are discovered incidentally and can be divided into regenerative lesions and true neoplastic lesions. The most common regenerative lesions include hemangioma, focal nodular hyperplasia and inflammatory pseudotumours of the liver. Neoplastic lesions include hepatocellular adenomas and angiomyolipomas. Regenerative lesions rarely increase in volume, do not yield a higher risk of complications and usually do not require treatment. By contrast, hepatocellular adenomas and angiomyolipomas can increase in volume and are associated with a risk of complications. Large hepatocellular adenomas (>5 cm in diameter) are undoubtedly associated with a risk of bleeding and malignant transformation, particularly the inflammatory (also known as telangiectatic) and β-catenin mutated subtypes. Accurate diagnosis needs to be obtained to select patients eligible for surgical resection. MRI has markedly improved diagnosis and can identify the major hepatocellular adenomas subtypes. The use of biopsy results to inform the indication for resection remains questionable. However, when diagnosis remains uncertain after imaging, percutaneous biopsy could help improve diagnostic accuracy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Choi, B. Y. & Nguyen, M. H. The diagnosis and management of benign hepatic tumours. J. Clin. Gastroenterol. 39, 401–412 (2005).
Nault, J. C., Bioulac Sage, P. & Zucman Rossi, J. Hepatocellular benign tumours – from molecular classification to personalized clinical care. Gastroenterology 144, 888–902 (2013).
Colli, A. et al. Elective surgery for benign liver tumours. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD005164. http://dx.doi.org/10.1002/14651858.CD005164.pub2.
Dokmak, S. et al. A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology 137, 1698–1705 (2009).
Deneve, J. L. et al. Liver cell adenoma: a multicenter analysis of risk factors for rupture and malignancy. Ann. Surg. Oncol. 16, 640–648 (2009).
Toro, A. et al. What is changing in indications and treatment of hepatic hemangiomas. A review. Ann. Hepatol. 13, 327–339 (2014).
Semelka, R. C. & Sofka, C. M. Hepatic hemangiomas. Magn. Reson. Imaging Clin. N. Am. 5, 241–253 (1997).
Vilgrain, V., Zappa, M., Hakimé, A., Sibert, A. & Vullierme, M. P. Liver imaging: pitfalls, pseudolesions and pseudotumours. J. Radiol. 88, 1104–1120 (2007).
Gandolfi, L. et al. Natural history of hepatic haemangiomas: clinical and ultrasound study. Gut 32, 677–680 (1991).
Trotter, J. F. & Everson, G. T. Benign focal lesions of the liver. Clin. Liver Dis. 5, 17–42 (2001).
Belghiti, J., Dokmak, S., Vilgrain, V. & Paradis, V. in Blumgart's Surgery of the Liver, Biliary Tract and Pancreas Ch. 79A (ed. Jarnagin, W. R.) 1250–1267 (Elsevier Saunders, 2012).
Lerner, S. M. et al. Giant cavernous liver hemangiomas: effect of operative approach on outcome. Arch. Surg. 139, 818–821 (2004).
Erdogan, D. et al. Management of liver hemangiomas according to size and symptoms. J. Gastroenterol. Hepatol. 22, 1953–1958 (2007).
Bornman, P. C. et al. Giant hepatic hemangiomas: diagnostic and therapeutic dilemnas. Surgery 101, 445–449 (1987).
Pateron, D. et al. Giant hemangioma of the liver with pain, fever, and abnormal liver tests: report of two cases. Dig. Dis. Sci. 36, 524–527 (1991).
Pol, B. et al. Inflammatory process complicating giant hemangioma of the liver: a report of three cases. Liver Transpl. Surg. 4, 204–207 (1998).
Hall, G. W. Kasabach-Merritt syndrome: pathogenesis and management. Br. J. Haematol. 112, 851–862 (2001).
Concejero, A. M., Chen, C. L., Chen, T. Y., Eng., H. L. & Kuo, F. Y. Giant cavernous hemangioma of the liver with coagulopathy: adult Kasabach-Merritt syndrome. Surgery 145, 245–247 (2009).
Corigliano, N. et al. Hemoperitoneum from a spontaneous rupture of a giant hemangioma of the liver: report of a case. Surg. Today 33, 459–463 (2003).
Plackett, T. P. & Lin-Hurtubise, K. M. Hepatic hemangiomas and parachuting. Aviat. Space Environ. Med. 79, 986–988 (2008).
Quaia, E., Bertolotto, M. & Dalla Palma, L. Characterization of liver hemangiomas with pulse inversion harmonic imaging. Eur. Radiol. 12, 537–544 (2002).
Semelka, R. C. et al. Hepatic hemangiomas: a multi-institutional study of appearance on T2-weighted and serial gadolinium-enhanced gradient-echo MR images. Radiology 192, 401–406 (1994).
Danet, I. M., Semelka, R. C., Braga, L., Armao, D. & Woosley, J. T. Giant hemangioma of the liver: MR imaging characteristics in 24 patients. Magn. Reson. Imaging 21, 95–101 (2003).
Coumbaras, M. et al. CT and MR imaging features of pathologically proven atypical giant hemangioma of the liver. AJR Am. J. Roentgenol. 179, 1457–1463 (2002).
Caldironi, M. W. et al. Echo-guided fine-needle biopsy for the diagnosis of hepatic angioma. A report on 114 cases. Minerva Chir. 53, 505–509 (1998).
Yoon, S. S. et al. Diagnosis, management and outcomes of 115 patients with hepatic hemangioma. J. Am. Coll. Surg. 197, 392–402 (2003).
Duxbury, M. S. & Garden, O. J. Giant haemangioma of the liver: observation or resection? Dig. Surg. 27, 7–11 (2010).
Herman, P. et al. Management of hepatic hemangiomas: a 14-year experience. J. Gastrointest. Surg. 9, 853–859 (2005).
Gedaly, R., Pomposelli, J. J., Pomfret, E. A., Lewis, W. D. & Jenkins, R. L. Cavernous hemangioma of the liver: anatomic resection vs. enucleation. Arch. Surg. 134, 407–411 (1999).
Jiang, W. S. et al. Laparoscope hepatectomy for hepatic hemangioma: a report of 18 cases. Zhonghua Wai Ke Za Zhi 45, 1311–1313 (2007).
Fu, X. H. et al. Enucleation of liver hemangiomas: is there a difference in surgical outcomes for centrally or peripherally located lesions? Am. J. Surg. 198, 184–187 (2009).
Ferraz, A. A. et al. Liver transplant for the treatment of giant hepatic hemangioma. Liver Transpl. 10, 1436–1437 (2004).
Ercolani, G., Grazi, G. L. & Pinna, A. D. Liver transplantation for benign hepatic tumours: a systematic review. Dig. Surg. 27, 68–75 (2010).
Gaspar, L. et al. Radiation therapy in the unresectable cavernous hemangioma of the liver. Radiother. Oncol. 29, 45–50 (1993).
Reading, N. G., Forbes, A., Nunnerley, H. B. & Williams, R. Hepatic haemangioma: a critical review of diagnosis and management. Q. J. Med. 67, 431–445 (1988).
Park, S. Y. et al. Symptomatic-enlarging hepatic hemangiomas are effectively treated by percutaneous ultrasonography-guided radiofrequency ablation. J. Hepatol. 54, 559–565 (2011).
Wanless, I. R. Benign liver tumours. Clin. Liver Dis. 6, 513–552 (2002).
Vilgrain, V. Focal nodular hyperplasia. Eur. J. Radiol. 58, 236–245 (2006).
Mathieu, D. et al. Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology 118, 560–564 (2000).
Wanless, I. R., Mawdsley, C. & Adams, R. On the pathogenesis of focal nodular hyperplasia. Hepatology 5, 1194–1200 (1985).
Kuo, Y. H. et al. Natural course of hepatic focal nodular hyperplasia: a long-term follow-up study with sonography. J. Clin. Ultrasound 37, 132–137 (2009).
Wanless, I. R. et al. Multiple focal nodular hyperplasia of the liver associated with vascular malformations of various organs and neoplasia of the brain: a new syndrome. Mod. Pathol. 2, 456–462 (1989).
Paradis, V. et al. A quantitative gene expression study suggests a role for angiopoietins in focal nodular hyperplasia. Gastroenterology 124, 651–659 (2003).
Rebouissou, S., Bioulac-Sage, P. & Zucman-Rossi, J. Molecular pathogenesis of focal nodular hyperplasia and hepatocellular adenoma. J. Hepatol. 48, 163–170 (2008).
Bioulac-Sage, P. et al. Over-expression of glutamine synthetase in focal nodular hyperplasia: a novel easy diagnostic tool in surgical pathology. Liver Int. 29, 459–465 (2009).
Belghiti, J. et al. Resection of presumed benign liver tumours. Br. J. Surg. 80, 380–383 (1993).
Chandler, T. M., Heran, M. K., Chang, S. D., Parvez, A. & Harris, A. C. Multiples focal nodular hyperplasia lesions of the liver associated with congenital absence of the portal vein. Magn. Reson. Imaging 29, 881–886 (2011).
Paradis, V. et al. Telangiectatic focal nodular hyperplasia: a variant of hepatocellular adenoma. Gastroenterology 126, 1323–1329 (2004).
Vilgrain, V. et al. Focal nodular hyperplasia of the liver: MR imaging and pathologic correlation in 37 patients. Radiology 184, 1–6 (1992).
Buetow, P. C., Pantongrag-Brown, L., Buck, J. L., Ros, P. R. & Goodman, Z. D. Focal nodular hyperplasia of the liver: radiologic-pathologic correlation. Radiographics 16, 369–388 (1996).
Brancatelli, G. et al. Focal nodular hyperplasia: CT findings with emphasis on multiphasic helical CT in 78 patients. Radiology 219, 61–68 (2001).
Kim, T. et al. Hepatic nodular lesions associated with abnormal development of the portal vein. AJR Am. J. Roentgenol. 183, 1333–1338 (2004).
Mortelé, K. J., Praet, M., Van Vlierberghe, H., Kunnen, M. & Ros, P. R. CT and MR imaging findings in focal nodular hyperplasia of the liver: radiologic-pathologic correlation. AJR Am. J. Roentgenol. 175, 687–692 (2000).
Kehagias, D. et al. Focal nodular hyperplasia: imaging findings. Eur. Radiol. 11, 202–212 (2001).
Ba-Ssalamah, A. et al. Atypical focal nodular hyperplasia of the liver: imaging features of nonspecific and liver-specific MR contrast agents. AJR Am. J. Roentgenol. 179, 1447–1456 (2002).
Grazioli, L., Morana, G., Kirchin, M. A. & Schneider, G. Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study. Radiology 236, 166–177 (2005).
Hussain, S. M. et al. Focal Nodular Hyperplasia: Findings at State-of-the-Art MR Imaging, US, CT, and Pathologic Analysis. Radiographics 24, 3–17 (2004).
Bertin, C. et al. Contrast-enhanced ultrasound of focal nodular hyperplasia: a matter of size. Eur. Radiol. http://dx.doi.org/10.1007/s00330-014-3280-0.
Kim, T. K., Jang, H. J., Burns, P. N., Murphy-Lavallee, J. & Wilson, S. R. Focal nodular hyperplasia and hepatic adenoma: differentiation with low-mechanical-index contrast-enhanced sonography. AJR Am. J. Roentgenol. 190, 58–66 (2008).
Soussan, M. et al. Incidental focal solid liver lesions: diagnostic performance of contrast-enhanced ultrasound and MR imaging. Eur. Radiol. 20, 1715–1725 (2010).
Fabre, A. et al. Histologic scoring of liver biopsy in focal nodular hyperplasia with atypical presentation. Hepatology 35, 414–420 (2002).
Makhlouf, H. R., Abdul-Al, H. M. & Goodman, Z. D. Diagnosis of focal nodular hyperplasia of the liver by needle biopsy. Hum. Pathol. 36, 1210–1216 (2005).
Bioulac-Sage, P. et al. Immunohistochemical markers on needle biopsies are helpful for the diagnosis of focal nodular hyperplasia and hepatocellular adenoma subtypes. Am. J. Surg. Pathol. 36, 1691–1699 (2012).
De Rave, S. & Hussain, S. M. A liver tumour as an incidental finding: differential diagnosis and treatment. Scand. J. Gastroenterol. Suppl. 236, 81–86 (2002).
Amesur, N., Hammond, J. S., Zajko, A. B., Geller, D. A. & Gamblin, T. C. Management of unresectable symptomatic focal nodular hyperplasia with arterial embolization. J. Vasc. Interv. Radiol. 20, 543–547 (2009).
Hedayati, P., VanSonnenberg, E., Shamos, R., Gillespie, T. & McMullen, W. Treatment of symptomatic focal nodular hyperplasia with percutaneous radiofrequency ablation. J. Vasc. Interv. Radiol. 21, 582–585 (2010).
Baum, J. K., Bookstein, J. J., Holtz, F. & Klein, E. W. Possible association between benign hepatomas and oral contraceptives. Lancet 302, 926–929 (1973).
Jeannot, E. et al. Association of CYP1B1 germ line mutations with hepatocyte nuclear factor 1alpha-mutated hepatocellular adenoma. Cancer Res. 67, 2611–2616 (2007).
Edmondson, H. A., Henderson, B. & Benton, B. Liver-cell adenomas associated with use of oral contraceptives. N. Engl. J. Med. 294, 470–472 (1976).
Rosenberg, L. The risk of liver neoplasia in relation to combined oral contraceptive use. Contraception 43, 643–652 (1991).
Gutiérrez Santiago, M., García Ibarbia, C., Nan Nan, D. N. & Hernández Hernández, J. L. Hepatic lesions and prolonged use of oral contraceptive. Rev. Clin. Esp. 207, 257–258 (2007).
Bühler, H. et al. Regression of liver cell adenoma. A follow-up study of three consecutive patients after discontinuation of oral contraceptive use. Gastroenterology 82, 775–782 (1982).
Velazquez, I. & Alter, B. P. Androgens and liver tumours: Fanconi's anemia and non-Fanconi's conditions. Am. J. Hematol. 77, 257–267 (2004).
Socas, L. et al. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: a report of two cases and a review of the literature. Br. J. Sports Med. 39, e27 (2005).
Bunchorntavakul, C. et al. Clinical features and natural history of hepatocellular adenomas: the impact of obesity. Aliment. Pharmacol. Ther. 34, 664–675 (2011).
Chang, C. Y., Hernandez-Prera, J. C., Roayaie, S., Schwartz, M. & Thung, S. N. Changing epidemiology of hepatocellular adenoma in the United States: review of the literature. Intern. J. Hepatol. 604860 (2013).
Bioulac-Sage, P., Taouji, S., Possenti, L. & Balabaud, C. Hepatocellular adenoma subtypes: the impact of overweight and obesity. Liver Int. 32, 1217–1221 (2012).
Brunt, E. M., Wolverson, M. K. & Di Bisceglie, A. M. Benign hepatocellular tumours (adenomatosis) in nonalcoholic steatohepatitis: a case report. Semin. Liver Dis. 25, 230–236 (2005).
Bioulac-Sage, P., Laumonier, H., Laurent, C., Zucman-Rossi, J. & Balabaud, C. Hepatocellular adenoma: what is new in 2008. Hepatol. Int. 2, 316–321 (2008).
Talente, G. M. et al. Glycogen storage disease in adults. Ann. Intern. Med. 120, 218–226 (1994).
Kawakatsu, M., Vilgrain, V., Belghiti, J., Flejou, J. F. & Nahum, H. Association of multiple liver cell adenomas with spontaneous intrahepatic portohepatic shunt. Abdom. Imaging 19, 438–440 (1994).
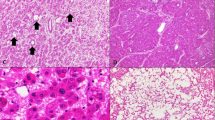
Zucman-Rossi, J. et al. Genotype-phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology 43, 515–524 (2006).
Bioulac-Sage, P. et al. Hepatocellular adenoma management and phenotypic classification: the Bordeaux experience. Hepatology 50, 481–489 (2009).
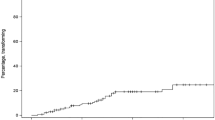
Farges, O. et al. Changing trends in malignant transformation of hepatocellular adenoma. Gut 60, 85–89 (2011).
Stoot, J. H., Coelen, R. J., De Jong, M. C. & Dejong, C. H. Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford) 12, 509–522 (2010).
Paradis, V. et al. Telangiectatic adenoma: an entity associated with increased body mass index and inflammation. Hepatology 46, 140–146 (2007).
Laumonier, H. et al. Hepatocellular adenomas: magnetic resonance imaging features as a function of molecular pathological classification. Hepatology 48, 808–818 (2008).
Ronot, M. et al. Hepatocellular adenomas: accuracy of magnetic resonance imaging and liver biopsy in subtype classification. Hepatology 53, 1182–1191 (2011).
Van Aalten, S. M. et al. Hepatocellular adenomas: correlation of MR imaging findings with pathologic subtype classification. Radiology 261, 172–181 (2011).
Terkivatan, T. & Ijzermans, J. N. Hepatocellular adenoma: Should phenotypic classification direct management? Nat. Rev. Gastroenterol. Hepatol. 6, 697–698 (2009).
Laumonier, H. et al. Role of contrast-enhanced sonography in differentiation of subtypes of hepatocellular adenoma: correlation with MRI findings. AJR Am. J. Roentgenol. 199, 341–348 (2012).
Bieze, M., Phoa, S. S., Verheij, J., van Lienden, K. P. & van Gulik, T. M. Risk factors for bleeding in hepatocellular adenoma. Br. J. Surg. 101, 847–855 (2014).
Stoot, J. H., Van der Linden, E., Terpstra, O. T. & Schaapherder, A. F. Life-saving therapy for haemorrhaging liver adenomas using selective arterial embolization. Br. J. Surg. 94, 1249–1253 (2007).
Fléjou, J. F. et al. Liver adenomatosis. An entity distinct from liver adenoma? Gastroenterology 89, 1132–1138 (1985).
Barthelemes, L. & Tait, I. S. Liver cell adenomas and liver cell adenomatosis. HBP 7, 186–196 (2005).
Cobey, F. C. & Salem, R. R. A review of liver masses in pregnancy and a proposed algorithm for their diagnosis and management. Am. J. Surg. 187, 181–191 (2004).
Noels, J. E. et al. Management of hepatocellular adenoma during pregnancy. J. Hepatol 54, 553–558 (2011).
Bioulac-Sage, P., Taouji, S., Le Bail, B., Possenti, L. & Balabaud, C. Value and limits of routine histology alone or combined with glutamine synthetase immunostaining in the diagnosis of hepatocellular adenoma subtypes on surgical specimens. Int. J. Hepatol. 417323 (2013).
Atwell, T. D. et al. Successful treatment of hepatocellular adenoma with percutaneous radiofrequency ablation. AJR Am. J. Roentgenol. 184, 828–831 (2005).
Van Aalten, S. M., Witjes, C. D., de Man, R. A., Ijzermans, J. N. & Terkivatan, T. Can a decision-making model be justified in the management of hepatocellular adenoma? Liver Int. 32, 28–37 (2012).
Terkivatan, T. et al. Treatment of ruptured hepatocellular adenoma. Br. J. Surg. 88, 207–209 (2001).
Marini, P., Vilgrain, V. & Belghiti, J. Management of spontaneous rupture of liver tumours. Dig. Surg. 19, 109–113 (2002).
Erdogan, D., van Delden, O. M., Busch, O. R., Gouma, D. J. & van Gulik, T. M. Selective transcatheter arterial embolization for treatment of bleeding complications or reduction of tumour mass of hepatocellular adenomas. Cardiovasc. Intervent. Radiol. 30, 1252–1258 (2007).
Huurman, V. A. & Schaapherder, A. F. Management of ruptured hepatocellular adenoma. Dig. Surg. 27, 56–60 (2010).
Kobayashi, S. et al. Two cases of hepatocellular adenomatosis treated with transcatheter arterial embolization. Hepatol. Int. 3, 416–420 (2009).
Deodhar, A., Brody, L. A., Covey, A. M., Brown, K. T. & Getrajdman, G. I. Bland embolization in the treatment of hepatic adenomas: preliminary experience. J. Vasc. Interv. Radiol. 22, 795–799 (2011).
Van Vledder, M. G. et al. Safety and efficacy of radiofrequency ablation for hepatocellular adenoma. J. Vasc. Interv. Radiol. 22, 787–793 (2011).
Van der Sluis, F. J. et al. Hepatocellular adenoma: cost-effectiveness of different treatment strategies. Radiology 252, 737–746 (2009).
Tsui, W. M. et al. Hepatic angiomyolipoma: a clinicopathologic study of 30 cases and delineation of unusual morphologic variants. Am. J. Surg. Pathol. 23, 34–48 (1999).
Yang, C. Y. et al. Management of hepatic angiomyolipoma. J. Gastrointest. Surg. 11, 452–457 (2007).
Zeng, J. P. et al. Hepatic angiomyolipoma: a clinical experience in diagnosis and treatment. Dig. Dis. Sci. 55, 3235–3240 (2010).
Zhou, Y. M. et al. Clinical features of hepatic angiomyolipoma. Hepatobiliary Pancreat. Dis. Int. 7, 284–287 (2008).
Hooper, L. D., Mergo, P. J. & Ros, P. R. Multiple hepatorenal angiomyolipomas: diagnosis with fat suppression, gadolinium-enhanced MRI. Abdom. Imaging 19, 549–551 (1994).
Rouquie, D. et al. Malignant-like angiomyolipoma of the liver: report of one case and review of the literature. Ann. Chir. 131, 338–341 (2006).
Dalle, I. et al. Malignant angiomyolipoma of the liver: a hitherto unreported variant. Histopathology 36, 443–450 (2000).
Arblade, S. et al. Hepatic angiomyolipoma simulating hepatocytic tumour, 3 cases. Gastroenterol. Clin. Biol. 20, 1022–1026 (1996).
Wang, Z. et al. Imaging features of hepatic angiomyolipomas on real-time contrast-enhanced ultrasound. Br. J. Radiol. 83, 411–418 (2010).
Sawai, J., Manabe, T., Yamanaka, Y., Kurahashi, S. & Kamiya, A. Angiomyolipoma of the liver: case report and collective review of cases diagnosed from fine needle aspiration biopsy specimens. J. Hepatobiliary Pancreat. Surg. 5, 333–338 (1998).
Ramon, J. et al. Renal angiomyolipoma: long-term results following selective arterial embolization. Eur. Urol. 55, 1155–1161 (2009).
Faddegon, S. & So, A. Treatment of angiomyolipoma at a tertiary care centre: the decision between surgery and angioembolization. Can. Urol. Assoc. 5, E138–E141 (2011).
Torzilli, G. et al. Inflammatory pseudotumours of the liver: prevalence and clinical impact in surgical patients. Hepatogastroenterology 37, 1118–1123 (2001).
Park, J. Y. et al. Clinical features, image findings, and prognosis of inflammatory pseudotumour of the liver: a multicenter experience of 45 cases. Gut Liver 8, 58–63 (2014).
Milias, K., Madhavan, K. K., Bellamy, C., Garden, O. J. & Parks, R. W. Inflammatory pseudotumours of the liver: experience of a specialist surgical unit. J. Gastroenterol. Hepatol. 24, 1562–1566 (2009).
Faraj, W. et al. Inflammatory pseudo-tumour of the liver: a rare pathological entity. World J. Surg. Oncol. 9, 5 (2011).
Goldsmith, P. J. et al. Inflammatory pseudotumours of the liver: a spectrum of presentation and management options. Eur. J. Surg. Oncol. 35, 1295–1298 (2009).
Deng, F. T. et al. Hilar inflammatory pseudotumour mimicking hilar cholangiocarcinoma. Hepatobiliary Pancreat. Dis. Int. 9, 219–221 (2010).
Zamir, D. et al. Inflammatory pseudotumour of the liver–a rare entity and a diagnostic challenge. Am. J. Gastroenterol. 93, 1538–1540 (1998).
Venkataraman, S., Semelka, R. C., Braga, L., Danet, I. M. & Woosley, J. T. Inflammatory myofibroblastic tumour of the hepatobiliary system: report of MR imaging appearance in four patients. Radiology 227, 758–763 (2003).
Abbey-Toby, A. et al. Pseudotumeur inflammatoire du foie: le diagnostic pré-opératoire est-il possible? Gastroenterol. Clin. Biol. 27, 883–890 (2003).
Maze, G. L., Lee, M. & Schenker, S. Inflammatory pseudotumour of the liver and pregnancy. Am. J. Gastroenterol. 94, 529–530 (1999).
Lévy, S. et al. Spontaneous regression of an inflammatory pseudotumour of the liver presenting as an obstructing malignant biliary tumour. Gastrointest. Endosc. 53, 371–374 (2001).
Clouet, M. et al. Imaging features of nodular regenerative hyperplasia of the liver mimicking hepatic metastases. Abdom. Imaging 24, 258–261 (1999).
Lim, D., Lee, S. Y., Lim, K. H. & Chan, C. Y. Hepatic adenoma mimicking a metastatic lesion on computed tomography-positron emission tomography scan. World J. Gastroenterol. 19, 4432–4436 (2013).
Bieze, M. et al. The use of 18F-fluoromethylcholine PET/CT in differentiating focal nodular hyperplasia from hepatocellular adenoma: a prospective study of diagnostic accuracy. Nucl. Med. Commun. 34, 146–154 (2013).
Sugito, K. et al. The clinical course in pediatric solid tumour patients with focal nodular hyperplasia of the liver. Int. J. Clin. Oncol. 16, 482–487 (2011).
Donadon, M., Di Tommaso, L., Roncalli, M. & Torzilli, G. Multiple focal nodular hyperplasia induced by oxaliplatin-based chemotherapy. World J. Hepatol. 5, 340–344 (2013).
Mathieu, D., Zafrani, E. S., Anglade, M. C. & Dhumeaux, D. Association of focal nodular hyperplasia and hepatic hemangioma. Gastroenterology 97, 154–157 (1989).
Vilgrain, V. et al. Prevalence of hepatic hemangioma in patients with focal nodular hyperplasia: MR imaging analysis. Radiology 229, 75–79 (2003).
Laurent, C., Rillaud, H., Lepreux, S., Balabaud, C. & Bioulac-Sage, P. Association of adenoma and focal nodular hyperplasia: experience of a single French academic center. Comp. Hepatol. 23, 6 (2003).
Parente, D. B. et al. MR imaging of hypervascular lesions in the cirrhotic liver: a diagnostic dilemma. Radiographics 32, 767–787 (2012).
Caturelli, E. et al. Hemangioma-like lesions in chronic liver disease: diagnostic evaluation in patients. Radiology 220, 337–342 (2001).
Dodd. G. D. 3rd, Baron, R. L., Oliver, J. H. 3rd & Federle, M. P. Spectrum of imaging findings of the liver in end-stage cirrhosis: part II, focal abnormalities. AJR Am. J. Roentgenol. 173, 1185–1192 (1999).
Rubaltelli, L. et al. Targetlike appearance of pseudotumours in segment IV of the liver on sonography. AJR Am. J. Roentgenol. 178, 75–77 (2002).
Marsh, J. I., Gibney, R. G. & Li, D. K. Hepatic hemangioma in the presence of fatty infiltration: an atypical sonographic appearance. Gastrointest. Radiol. 14, 262–264 (1989).
Tom, W. W. et al. Hepatic pseudotumour due to nodular fatty sparing: the diagnosis role of opposed-phase MRI. AJR Am. J. Roentgenol. 183, 721–724 (2004).
Vilgrain, V. et al. Hepatic nodules in Budd–Chiari syndrome: imaging features. Radiology 210, 443–450 (1999).
Bureau, C. et al. Liver nodules resembling focal nodular hyperplasia after portal vein thrombosis. J. Hepatology 41, 499–500 (2004).
Buscarini, E. et al. High prevalence of hepatic focal nodular hyperplasia in subjects with hereditary hemorrhagic telangiectasia. Ultrasound Med. Biol. 30, 1089–1097 (2004).
Cazals-Hatem, D. et al. Arterial and portal circulation and parenchymal changes in Budd–Chiari syndrome: a study in 17 explanted livers. Hepatology 37, 510–519 (2003).
Author information
Authors and Affiliations
Contributions
J.B. and V.V. made a substantial contribution to discussion of content and writing the article. F.C. contributed substantially to writing the article and reviewing and/or editing the article before submission. V.P. substantially contributed to the discussion of content and reviewing and/or editing the article before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Belghiti, J., Cauchy, F., Paradis, V. et al. Diagnosis and management of solid benign liver lesions. Nat Rev Gastroenterol Hepatol 11, 737–749 (2014). https://doi.org/10.1038/nrgastro.2014.151
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2014.151
This article is cited by
-
Rare benign liver tumors that require differentiation from hepatocellular carcinoma: focus on diagnosis and treatment
Journal of Cancer Research and Clinical Oncology (2023)
-
Premorbid cancer and motor reserve in patients with Parkinson’s disease
Scientific Reports (2022)
-
A Comprehensive Review of Hepatic Hemangioma Management
Journal of Gastrointestinal Surgery (2022)
-
Malignant perivascular epithelioid cell neoplasm in the liver: report of a pediatric case
Surgical Case Reports (2021)
-
Hepatospecific MR contrast agent uptake on hepatobiliary phase can be used as a biomarker of marked β-catenin activation in hepatocellular adenoma
European Radiology (2021)