Abstract
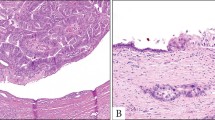
Cystic pancreatic neoplasms are increasingly recognized, with intraductal papillary mucinous neoplasms of the pancreas (IPMNs) being the most frequently observed type. IPMNs are characterized by mucin production and epithelial growth within the pancreatic ducts, and are generally differentiated according to location: main pancreatic duct, its major side branches, or both (mixed type). IPMNs vary from benign to malignant and are considered precursor lesions of pancreatic adenocarcinoma. However, the exact time to neoplastic transformation and whether all IPMNs progress to malignant tumors is unclear. Surgical resection is warranted for all main-duct and mixed-type IPMNs (they harbor a high risk of malignancy of ∼70%). By contrast, branch-duct IPMNs progress to cancer in only ∼30% of cases. Thus, according to current guidelines (Sendai criteria), asymptomatic side-branch IPMNs <3 cm in size without suspicious radiological features (such as size progression) can be treated conservatively. Lately, even this approach has become controversial, owing to a number of Sendai-negative IPMNs showing malignant transformation. Although most IPMNs should be resected by standard oncological procedures (including lymphadenectomy), small Sendai-negative IPMNs can be treated with limited resections. This Review summarizes current knowledge of the treatment of IPMNs, with a particular focus on surgical approaches to this disease.
Key Points
-
According to modern thin-slice abdominal imaging or endoscopic ultrasonography, intraductal papillary mucinous neoplasms of the pancreas (IPMNs) can be distinguished into three types: main duct, branch duct, or mixed
-
Currently, all three IPMN types are considered precursors to invasive adenocarcinoma of the pancreas with varying risks of malignant transformation
-
Owing to their high rates of malignancy, main-duct IPMNs and mixed-type IPMNs should be oncologically resected whenever the patient is an adequate candidate for surgery
-
According to current treatment guidelines (Sendai criteria), asymptomatic branch-duct IPMNs <3 cm in size without suspicious radiological features can be treated conservatively
-
Surgery for small branch-duct IPMNs remains controversial; malignant transformation even in small branch-duct IPMNs without suspicious features is increasingly reported, in which case, the Sendai criteria should be re-evaluated
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hivet, M., Maisel, A., Horiot, A. & Conte, J. Diffuse villous carcinoma of Wirsung's duct. Total pancreatectomy [French]. Med. Chir. Dig. 4, 159–623 (1975).
Kloppel, G. Clinicopathologic view of intraductal papillary-mucinous tumor of the pancreas. Hepatogastroenterology 45, 1981–1985 (1998).
Haban, G. Papillomatosis and carcinoma of the ductal system of the pancreas. Virchows Arch. A Pathol. Anat. 297, 207–220 (1936).
Kloppel, G., Kosmahl, M. & Luttges, J. Intraductal neoplasms of the pancreas: cystic and common [German]. Pathologe 26, 31–36 (2005).
Ohashi, K. et al. Four cases of mucous secreting pancreatic cancer. Prog. Dig. Endosc. 20, 348–351 (1982).
Agostini, S. et al. Mucinous pancreatic duct ectasia in the body of the pancreas. Radiology 170, 815–816 (1989).
Payan, M. J. et al. Villous adenoma of the main pancreatic duct: a potentially malignant tumor? Am. J. Gastroenterol. 85, 459–463 (1990).
Sessa, F. et al. Intraductal papillary-mucinous tumours represent a distinct group of pancreatic neoplasms: an investigation of tumour cell differentiation and K-ras, p53 and c-erbB-2 abnormalities in 26 patients. Virchows Arch. 425, 357–367 (1994).
Morohoshi, T., Kanda, M., Asanuma, K. & Kloppel, G. Intraductal papillary neoplasms of the pancreas. A clinicopathologic study of six patients. Cancer 64, 1329–1335 (1989).
Tanaka, M. et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 6, 17–32 (2006).
Kloppel, G., Solcia, E., Longnecker, D. S. & Sobin, L. H. in World Health Organization International Histological Classification of Tumours 2nd ed. 15–21 (Springer, Berlin, 1996).
Bosman, F. T., Carneiro, F., Hruban, R. H. & Theise, N. D. (eds) WHO Classification of Tumours of the Digestive System. (WHO Press, Switzerland, 2010).
Volkan Adsay, N. Cystic lesions of the pancreas. Mod. Pathol. 20 (Suppl. 1), S71–S93 (2007).
Hruben, R. H., Pitman, M. B. & Klimstra, D. S. in Tumors of the Pancreas 4th edn 75–110, (American Registry of Pathlogy, Washington, 2007).
Kimura, W., Nagai, H., Kuroda, A., Muto, T. & Esaki, Y. Analysis of small cystic lesions of the pancreas. Int. J. Pancreatol. 18, 197–206 (1995).
Kosmahl, M. et al. Cystic neoplasms of the pancreas and tumor-like lesions with cystic features: a review of 418 cases and a classification proposal. Virchows Arch. 445, 168–178 (2004).
Conlon, K. C. Intraductal papillary mucinous tumors of the pancreas. J. Clin. Oncol. 23, 4518–4523 (2005).
Fernandez-del Castillo, C. et al. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch. Surg. 138, 427–433 (2003).
Sarr, M. G. et al. Primary cystic neoplasms of the pancreas. Neoplastic disorders of emerging importance-current state-of-the-art and unanswered questions. J. Gastrointest. Surg. 7, 417–428 (2003).
Sohn, T. A. et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann. Surg. 239, 788–797 (2004).
Wada, K., Kozarek, R. A. & Traverso, L. W. Outcomes following resection of invasive and noninvasive intraductal papillary mucinous neoplasms of the pancreas. Am. J. Surg. 189, 632–636 (2005).
Spinelli, K. S. et al. Cystic pancreatic neoplasms: observe or operate. Ann. Surg. 239, 651–657 (2004).
Chiu, S. S. et al. Intraductal papillary mucinous tumour of the pancreas: differentiation of malignancy and benignancy by CT. Clin. Radiol. 61, 776–783 (2006).
Sahani, D. V. et al. Intraductal papillary mucinous neoplasm of pancreas: multi-detector row CT with 2D curved reformations--correlation with MRCP. Radiology 238, 560–569 (2006).
Irie, H. et al. MR cholangiopancreatographic differentiation of benign and malignant intraductal mucin-producing tumors of the pancreas. AJR Am. J. Roentgenol. 174, 1403–1408 (2000).
Kalra, M. K., Maher, M. M., Sahani, D. V., Digmurthy, S. & Saini, S. Current status of imaging in pancreatic diseases. J. Comput. Assist. Tomogr. 26, 661–675 (2002).
Waters, J. A. et al. CT vs MRCP: optimal classification of IPMN type and extent. J. Gastrointest. Surg. 12, 101–109 (2008).
Tollefson, M. K. et al. Intraductal papillary mucinous neoplasm: did it exist prior to 1980? Pancreas 26, e55–e58 (2003).
Laffan, T. A. et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am. J. Roentgenol. 191, 802–807 (2008).
de Jong, K. et al. High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin. Gastroenterol. Hepatol. 8, 806–811 (2010).
Salvia, R. et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann. Surg. 239, 678–685 (2004).
Kamisawa, T. et al. Long-term follow-up of intraductal papillary adenoma of the pancreas. J. Gastroenterol. 37, 868–873 (2002).
D'Angelica, M., Brennan, M. F., Suriawinata, A. A., Klimstra, D. & Conlon, K. C. Intraductal papillary mucinous neoplasms of the pancreas: an analysis of clinicopathologic features and outcome. Ann. Surg. 239, 400–408 (2004).
Rodriguez, J. R. et al. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology 133, 72–79 (2007).
Schmidt, C. M. et al. Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann. Surg. 246, 644–651 (2007).
Ingkakul, T. et al. Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Ann. Surg. 251, 70–75 (2010).
Sato, N. et al. STK11/LKB1 Peutz–Jeghers gene inactivation in intraductal papillary-mucinous neoplasms of the pancreas. Am. J. Pathol. 159, 2017–2022 (2001).
Chetty, R. et al. Intraductal papillary mucinous neoplasm of the pancreas in a patient with attenuated familial adenomatous polyposis. J. Clin. Pathol. 58, 97–101 (2005).
Yamaguchi, K., Yokohata, K., Noshiro, H., Chijiiwa, K. & Tanaka, M. Mucinous cystic neoplasm of the pancreas or intraductal papillary-mucinous tumour of the pancreas. Eur. J. Surg. 166, 141–148 (2000).
Eguchi, H. et al. Patients with pancreatic intraductal papillary mucinous neoplasms are at high risk of colorectal cancer development. Surgery 139, 749–754 (2006).
Reid-Lombardo, K. M., Mathis, K. L., Wood, C. M., Harmsen, W. S. & Sarr, M. G. Frequency of extrapancreatic neoplasms in intraductal papillary mucinous neoplasm of the pancreas: implications for management. Ann. Surg. 251, 64–69 (2010).
Hruban, R. H. et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am. J. Surg. Pathol. 28, 977–987 (2004).
Salvia, R. et al. Differences between main-duct and branch-duct intraductal papillary mucinous neoplasms of the pancreas. World J. Gastrointest. Surg. 2, 342–346 (2010).
Pelaez-Luna, M. et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am. J. Gastroenterol. 102, 1759–1764 (2007).
Basturk, O., Coban, I. & Adsay, N. V. Pancreatic cysts: pathologic classification, differential diagnosis, and clinical implications. Arch. Pathol. Lab. Med. 133, 423–438 (2009).
Tanno, S. et al. Pancreatic ductal adenocarcinomas in long-term follow-up patients with branch duct intraductal papillary mucinous neoplasms. Pancreas 39, 36–40 (2010).
Hruban, R. H. & Adsay, N. V. Molecular classification of neoplasms of the pancreas. Hum. Pathol. 40, 612–623 (2009).
Fritz, S. et al. Global genomic analysis of intraductal papillary mucinous neoplasms of the pancreas reveals significant molecular differences compared to ductal adenocarcinoma. Ann. Surg. 249, 440–447 (2009).
Z'Graggen, K. et al. Prevalence of activating K-ras mutations in the evolutionary stages of neoplasia in intraductal papillary mucinous tumors of the pancreas. Ann. Surg. 226, 491–498 (1997).
Fernandez-del Castillo, C. & Adsay, N. V. Intraductal papillary mucinous neoplasms of the pancreas. Gastroenterology 139, 708–713 (2010).
Adsay, N. V. et al. Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am. J. Surg. Pathol. 28, 839–848 (2004).
Luttges, J., Feyerabend, B., Buchelt, T., Pacena, M. & Kloppel, G. The mucin profile of noninvasive and invasive mucinous cystic neoplasms of the pancreas. Am. J. Surg. Pathol. 26, 466–471 (2002).
Nakamura, A. et al. New classification of pancreatic intraductal papillary-mucinous tumour by mucin expression: its relationship with potential for malignancy. J. Pathol. 197, 201–210 (2002).
Furukawa, T. et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 447, 794–799 (2005).
Mino-Kenudson, M. et al. Prognosis of invasive intraductal papillary mucinous neoplasm depends on histological and precursor epithelial subtypes. Gut 60, 1712–1720 (2011).
Luttges, J., Zamboni, G., Longnecker, D. & Kloppel, G. The immunohistochemical mucin expression pattern distinguishes different types of intraductal papillary mucinous neoplasms of the pancreas and determines their relationship to mucinous noncystic carcinoma and ductal adenocarcinoma. Am. J. Surg. Pathol. 25, 942–948 (2001).
Basturk, O. et al. Preferential expression of MUC6 in oncocytic and pancreatobiliary types of intraductal papillary neoplasms highlights a pyloropancreatic pathway, distinct from the intestinal pathway, in pancreatic carcinogenesis. Am. J. Surg. Pathol. 34, 364–370 (2010).
Salvia, R. et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut 56, 1086–1090 (2007).
Warshaw, A. L., Compton, C. C., Lewandrowski, K., Cardenosa, G. & Mueller, P. R. Cystic tumors of the pancreas. New clinical, radiologic, and pathologic observations in 67 patients. Ann. Surg. 212, 432–443 (1990).
Thompson, L. D., Becker, R. C., Przygodzki, R. M., Adair, C. F. & Heffess, C. S. Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases. Am. J. Surg. Pathol. 23, 1–16 (1999).
Nakagohri, T., Kenmochi, T., Kainuma, O., Tokoro, Y. & Asano, T. Intraductal papillary mucinous tumors of the pancreas. Am. J. Surg. 178, 344–347 (1999).
Falconi, M. et al. Clinicopathological features and treatment of intraductal papillary mucinous tumour of the pancreas. Br. J. Surg. 88, 376–381 (2001).
Tanaka, M. et al. International Consensus Guidelines for Management of Intraductal Papillary Mucinous Neoplasms and Mucinous Cystic Neoplasms of the Pancreas. Pancreatology 6, 17–32 (2005).
Sahani, D. V., Shah, Z. K., Catalano, O. A., Boland, G. W. & Brugge, W. R. Radiology of pancreatic adenocarcinoma: current status of imaging. J. Gastroenterol. Hepatol. 23, 23–33 (2008).
Ferrone, C. R. et al. Current trends in pancreatic cystic neoplasms. Arch. Surg. 144, 448–454 (2009).
Waters, J. A. & Schmidt, C. M. Intraductal papillary mucinous neoplasm—when to resect? Adv. Surg. 42, 87–108 (2008).
Pitman, M. B. et al. Pancreatic cysts: preoperative diagnosis and clinical management. Cancer Cytopathol. 118, 1–13 (2010).
Fritz, S., Warshaw, A. L. & Thayer, S. P. Management of mucin-producing cystic neoplasms of the pancreas. Oncologist 125–136 (2009).
Schnelldorfer, T. et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch. Surg. 143, 639–646 (2008).
Bendix Holme, J., Jacobsen, N. O., Rokkjaer, M. & Kruse, A. Total pancreatectomy in six patients with intraductal papillary mucinous tumour of the pancreas: the treatment of choice. HPB (Oxford) 3, 257–262 (2001).
Chari, S. T. et al. Study of recurrence after surgical resection of intraductal papillary mucinous neoplasm of the pancreas. Gastroenterology 123, 1500–1507 (2002).
Jang, J. Y. et al. Multicenter analysis of clinicopathologic features of intraductal papillary mucinous tumor of the pancreas: is it possible to predict the malignancy before surgery? Ann. Surg. Oncol. 12, 124–132 (2005).
Maire, F. et al. Prognosis of malignant intraductal papillary mucinous tumours of the pancreas after surgical resection. Comparison with pancreatic ductal adenocarcinoma. Gut 51, 717–722 (2002).
Tang, R. S. et al. Evaluation of the guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin. Gastroenterol. Hepatol. 6, 815–819 (2008).
Wasif, N. et al. Invasive intraductal papillary mucinous neoplasm versus sporadic pancreatic adenocarcinoma: a stage-matched comparison of outcomes. Cancer 116, 3369–3377 (2010).
Poultsides, G. A. et al. Histopathologic basis for the favorable survival after resection of intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma of the pancreas. Ann. Surg. 251, 470–476 (2010).
Jang, J. Y. et al. Treatment guidelines for branch duct type intraductal papillary mucinous neoplasms of the pancreas: when can we operate or observe? Ann. Surg. Oncol. 15, 199–205 (2008).
Sawai, Y. et al. Development of pancreatic cancers during long-term follow-up of side-branch intraductal papillary mucinous neoplasms. Endoscopy 42, 1077–1084 (2010).
Fritz, S. et al. Small (Sendai negative) branch-duct IPMNs: not harmless. Ann. Surg. (in press).
Gerke, H. et al. Endoscopic ultrasound and computer tomography are inaccurate methods of classifying cystic pancreatic lesions. Dig. Liver Dis. 38, 39–44 (2006).
Fritz, S. et al. Role of serum carbohydrate antigen 19–19 and carcinoembryonic antigen in distinguishing between benign and invasive intraductal papillary mucinous neoplasm of the pancreas. Br. J. Surg. 98, 104–110 (2011).
Crippa, S. et al. Mucin-producing neoplasms of the pancreas: an analysis of distinguishing clinical and epidemiologic characteristics. Clin. Gastroenterol. Hepatol. 8, 213–219 (2010).
Cameron, J. L., Riall, T. S., Coleman, J. & Belcher, K. A. One thousand consecutive pancreaticoduodenectomies. Ann. Surg. 244, 10–15 (2006).
Wagner, M. et al. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br. J. Surg. 91, 586–594 (2004).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, and reviewed and edited the manuscript before submission. J. Werner and B. W. Büchler made equal contributions to discussion of content, and J. Werner and S. Fritz wrote the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Werner, J., Fritz, S. & Büchler, M. Intraductal papillary mucinous neoplasms of the pancreas—a surgical disease. Nat Rev Gastroenterol Hepatol 9, 253–259 (2012). https://doi.org/10.1038/nrgastro.2012.31
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2012.31
This article is cited by
-
SDC1 and ITGA2 as novel prognostic biomarkers for PDAC related to IPMN
Scientific Reports (2023)
-
Carbohydrate antigen 125 supplements carbohydrate antigen 19-9 for the prediction of invasive intraductal papillary mucinous neoplasms of the pancreas
World Journal of Surgical Oncology (2022)
-
Intraduktale papillär-muzinöse Neoplasie des Seitengangs – Pro Resektion
Der Chirurg (2017)
-
Implications of Imaging Criteria for the Management and Treatment of Intraductal Papillary Mucinous Neoplasms – Benign versus Malignant Findings
European Radiology (2015)
-
Zufallsbefund zystischer Pankreastumor
MMW - Fortschritte der Medizin (2015)