Abstract
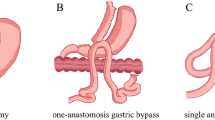
Bariatric surgery, through its efficacy and improved safety, is emerging as an important and broadly available treatment for people with severe and complex obesity that has not responded adequately to other therapy. Established procedures, such as Roux-en-Y gastric bypass and adjustable gastric banding, account for more than 80% of bariatric surgical procedures globally. Sleeve gastrectomy has emerged as a stand-alone procedure. Truly malabsoptive procedures, such as biliopancreatic diversion and its duodenal switch variant, have a diminishing role as primary procedures, but remain an option for patients who do not respond adequately to less disruptive procedures. The procedures vary considerably in their postoperative morbidity and mortality; pattern and extent of weight loss; nature and severity of long-term complications; and nutritional requirements and risks. There is no perfect procedure—an informed risk and benefit assessment should be made by each patient. Gastroenterologists also need to be familiar with the risks and benefits of current and emerging procedures as they are likely to be increasingly involved in the integrated care of these patients.
Key Points
-
Bariatric surgery has an established role in achieving sustained weight loss, improving obesity-related conditions and saving lives
-
During the past decade there has been a major increase in the use of bariatric surgery and a reduction in postoperative morbidity and mortality
-
There is no perfect bariatric procedure; selection is based on local availability, the balance of risks and benefits for an individual, and ultimately patient choice
-
The nature of bariatric surgery places the gastroenterologist on the front line for detecting and evaluating surgical complications
-
Interventions to the gut can lead to major changes in energy balance and metabolism; future research will be guided by an improved understanding of the mechanisms involved
-
Gastroenterologists will be increasingly involved in the development and implementation of a range of novel endoluminal bariatric and metabolic procedures
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Alverdy, J. C. et al. Bariatric surgery: a history of empiricism, a future in science. J. Gastrointest. Surg. 13, 465–477 (2009).
Picot, J. et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol. Assess. 13, 1–190, 215–357, iii–iv (2009).
Finkelstein, E. A. & Brown, D. S. A cost-benefit simulation model of coverage for bariatric surgery among full-time employees. Am. J. Manag. Care 11, 641–646 (2005).
Whitaker, R. C., Wright, J. A., Pepe, M. S., Seidel, K. D. & Dietz, W. H. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 337, 869–873 (1997).
Schwartz, M. W. et al. Is the energy homeostasis system inherently biased toward weight gain? Diabetes 52, 232–238 (2003).
Rosenbaum, M. et al. Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. J. Clin. Invest. 115, 3579–3586 (2005).
Rosenbaum, M., Kissileff, H. R., Mayer, L. E., Hirsch, J. & Leibel, R. L. Energy intake in weight-reduced humans. Brain Res. 1350, 95–102 (2010).
Buchwald, H. & Oien, D. M. Metabolic/bariatric surgery Worldwide 2008. Obes. Surg. 19, 1605–1611 (2008).
Buchwald, H. & Williams, S. E. Bariatric surgery worldwide 2003. Obes. Surg. 14, 1157–1164 (2003).
DeMaria, E. J., Pate, V., Warthen, M. & Winegar, D. A. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg. Obes. Relat. Dis. 6, 347–355 (2010).
Christou, N. V. et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann. Surg. 240, 416–423 (2004).
[No authors listed]. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am. J. Clin. Nutr. 55 (2 Suppl.), 615S–619S (1992).
National Institute for Health and Clinical Excellence. Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children. NICE [online], (2006).
Dixon, J. B., Zimmet, P., Alberti, K. G. & Rubino, F. Bariatric surgery: an IDF statement for obese Type 2 diabetes. Diabet. Med. 28, 628–642 (2011).
Sharma, A. M. & Kushner, R. F. A proposed clinical staging system for obesity. Int. J. Obes. (Lond.) 33, 289–295 (2009).
Sharma, A. M. M, M, M & M: a mnemonic for assessing obesity. Obes. Rev. 11, 808–809 (2010).
Dixon, J. B. Referral for a bariatric surgical consultation: it is time to set a standard of care. Obes. Surg. 19, 641–644 (2008).
Mechanick, J. I. et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery Medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Endocr. Pract. 14 (Suppl. 1), 1–83 (2008).
Welbourn, R., Fiennes, A., Kinsman, R. & Walton, P. The United Kingdom National Bariatric Surgery Registry—First Registry Report to March 2010. The Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland [online], (2011).
Brethauer, S. A., Hammel, J. P. & Schauer, P. R. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg. Obes. Relat. Dis. 5, 469–475 (2009).
Himpens, J., Dobbeleir, J. & Peeters, G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann. Surg. 252, 319–324 (2010).
Bohdjalian, A. et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes. Surg. 20, 535–540 (2010).
Deitel, M., Gagner, M., Dixon, J. B., Himpens, J. & Madan, A. K. (Eds). Handbook of Obesity Surgery (FD-Communications Inc., Toronto, 2010).
Andersen, T., Pedersen, B. H., Henriksen, J. H. & Uhrenholdt, A. Pouch emptying of solid foods after gastroplasty for morbid obesity. Scand. J. Gastroenterol. 20, 1175–1179 (1985).
Burton, P. R. et al. Changes in satiety, supra- and infraband transit, and gastric emptying following laparoscopic adjustable gastric banding: a prospective follow-up study. Obes. Surg. 21, 217–223 (2011).
de Jong, J. R., van Ramshorst, B., Gooszen, H. G., Smout, A. J. & Tiel-Van Buul, M. M. Weight loss after laparoscopic adjustable gastric banding is not caused by altered gastric emptying. Obes. Surg. 19, 287–292 (2008).
Melissas, J. et al. Sleeve gastrectomy: a restrictive procedure? Obes. Surg. 17, 57–62 (2007).
Dixon, A. F., Dixon, J. B. & O'Brien, P. E. Laparoscopic adjustable gastric banding induces prolonged satiety: a randomized blind crossover study. J. Clin. Endocrinol. Metab. 90, 813–819 (2005).
Hallberg, D. Why the operation I prefer is adjustable gastric banding. Obes. Surg. 1, 187–188 (1991).
Kuzmak, L. I. A review of seven years' experience with silicone gastric banding. Obes. Surg. 1, 403–408 (1991).
le Roux, C. W. et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann. Surg. 243, 108–114 (2006).
Vetter, M. L., Cardillo, S., Rickels, M. R. & Iqbal, N. Narrative review: effect of bariatric surgery on type 2 diabetes mellitus. Ann. Intern. Med. 150, 94–103 (2009).
Pories, W. J. et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann. Surg. 222, 339–350 (1995).
Rubino, F. Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis. Diabetes Care 31 (Suppl. 2), S290–S296 (2008).
Cohen, R. V., Schiavon, C. A., Pinheiro, J. S., Correa, J. L. & Rubino, F. Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22–34 kg/m2: a report of 2 cases. Surg. Obes. Relat. Dis. 3, 195–197 (2007).
Holdstock, C., Zethelius, B., Sundbom, M., Karlsson, F. A. & Eden Engstrom, B. Postprandial changes in gut regulatory peptides in gastric bypass patients. Int. J. Obes. (Lond.) 32, 1640–1646 (2008).
Laferrere, B. et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 93, 2479–2485 (2008).
Strader, A. D., Clausen, T. R., Goodin, S. Z. & Wendt, D. Ileal interposition improves glucose tolerance in low dose streptozotocin-treated diabetic and euglycemic rats. Obes. Surg. 19, 96–104 (2009).
Wang, T. T. et al. Ileal transposition controls diabetes as well as modified duodenal jejunal bypass with better lipid lowering in a nonobese rat model of type II diabetes by increasing GLP-1. Ann. Surg. 247, 968–975 (2008).
Rubino, F. et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann. Surg. 244, 741–749 (2006).
Geloneze, B. et al. Surgery for nonobese type 2 diabetic patients: an interventional study with duodenal-jejunal exclusion. Obes. Surg. 19, 1077–1083 (2009).
Schouten, R. et al. A multicenter, randomized efficacy study of the EndoBarrier Gastrointestinal Liner for presurgical weight loss prior to bariatric surgery. Ann. Surg. 251, 236–243 (2010).
Vidal, J. et al. Short-term effects of sleeve gastrectomy on type 2 diabetes mellitus in severely obese subjects. Obes. Surg. 17, 1069–1074 (2007).
Peterli, R. et al. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann. Surg. 250, 234–241 (2009).
Lee, W. J. et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch. Surg. 146, 143–148 (2011).
Dixon, J. B., Dixon, A. F. & O'Brien, P. E. Improvements in insulin sensitivity and beta-cell function (HOMA) with weight loss in the severely obese. Diabet. Med. 20, 127–134 (2003).
Dixon, J. B., Anderson, M., Cameron-Smith, D. & O'Brien, P. E. Sustained weight loss in obese subjects has benefits that are independent of attained weight. Obes. Res. 12, 1895–1902 (2004).
Buchwald, H. et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am. J. Med. 122, 248–256 (2009).
Dixon, J. B. et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 299, 316–323 (2008).
Dixon, J. B. & O'Brien, P. Health outcomes of severely obese type 2 diabetic subjects 1 year after laparoscopic adjustable gastric banding. Diabetes Care 25, 358–363 (2002).
Schauer, P. et al. Effect of laparoscopic roux-en Y gastric bypass on type 2 diabetes mellitis. Ann. Surg. 238, 467–485 (2003).
Dixon, J. B. Surgical treatment for obesity and its impact on non-alcoholic steatohepatitis. Clin. Liver Dis. 11, 141–154 (2007).
Kolotkin, R. L., Crosby, R. D., Gress, R. E., Hunt, S. C. & Adams, T. D. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg. Obes. Relat. Dis. 5, 250–256 (2009).
Dixon, J. B., Dixon, M. E. & O'Brien, P. E. Depression in association with severe obesity: changes with weight loss. Arch. Intern. Med. 163, 2058–2065 (2003).
Sjostrom, C. D., Peltonen, M., Wedel, H. & Sjostrom, L. Differentiated long-term effects of intentional weight loss on diabetes and hypertension. Hypertension 36, 20–25 (2000).
Dixon, J. B. & O'Brien, P. A disparity between conventional lipid and insulin resistance markers at body mass index levels greater than 34 kg/m2. Int. J. Obes. Relat. Metab. Disord. 25, 793–797 (2001).
Livingston, E. H., Chandalia, M. & Abate, N. Do current body mass index criteria for obesity surgery reflect cardiovascular risk? Surg. Obes. Relat. Dis. 3, 577–585 (2007).
Adams, T. D. et al. Long-term mortality after gastric bypass surgery. N. Engl. J. Med. 357, 753–761 (2007).
Tindle, H. A. et al. Risk of suicide after long-term follow-up from bariatric surgery. Am. J. Med. 123, 1036–1042 (2010).
Christensen, R., Kristensen, P. K., Bartels, E. M., Bliddal, H. & Astrup, A. Efficacy and safety of the weight-loss drug rimonabant: a meta-analysis of randomised trials. Lancet 370, 1706–1713 (2007).
Berthoud, H. R. Vagal and hormonal gut–brain communication: from satiation to satisfaction. Neurogastroenterol. Motil. 20 (Suppl. 1), 64–72 (2008).
Soeki, T. et al. Ghrelin suppresses cardiac sympathetic activity and prevents early left ventricular remodeling in rats with myocardial infarction. Am. J. Physiol. 294, H426–H432 (2008).
Rossi, F. et al. Ghrelin inhibits contraction and proliferation of human aortic smooth muscle cells by cAMP/PKA pathway activation. Atherosclerosis 203, 97–104 (2009).
Schwenke, D. O. et al. Early ghrelin treatment after myocardial infarction prevents an increase in cardiac sympathetic tone and reduces mortality. Endocrinology 149, 5172–5176 (2008).
Granata, R., Isgaard, J., Alloatti, G. & Ghigo, E. Cardiovascular actions of the ghrelin gene-derived peptides and growth hormone-releasing hormone. Exp. Biol. Med. (Maywood) 236, 505–514 (2011).
Lutter, M. et al. The orexigenic hormone ghrelin defends against depressive symptoms of chronic stress. Nat. Neurosci. 11, 752–753 (2008).
Lambert, E. et al. Ghrelin modulates sympathetic nervous system activity and stress response in lean and overweight men. Hypertension doi:10.1161/HYPERTENSIONAHA.111.171025.
Cummings, D. E. et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N. Engl. J. Med. 346, 1623–1630 (2002).
Berrington de Gonzalez, A. et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 363, 2211–2219 (2010).
Sjostrom, L. et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 357, 741–752 (2007).
Peeters, A. et al. Substantial intentional weight loss and mortality in the severely obese. Ann. Surg. 246, 1028–1033 (2007).
Busetto, L. et al. Comparative long-term mortality after laparoscopic adjustable gastric banding versus nonsurgical controls. Surg. Obes. Relat. Dis. 3, 496–502 (2007).
Colagiuri, S. et al. The cost of overweight and obesity in Australia. Med. J. Aust. 192, 260–264 (2010).
Tsai, A. G., Williamson, D. F. & Glick, H. A. Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obes. Rev. 12, 50–61 (2011).
Trogdon, J. G., Finkelstein, E. A., Hylands, T., Dellea, P. S. & Kamal-Bahl, S. J. Indirect costs of obesity: a review of the current literature. Obes. Rev. 9, 489–500 (2008).
Cremieux, P. Y. et al. A study on the economic impact of bariatric surgery. Am. J. Manag. Care 14, 589–596 (2008).
Keating, C. L. et al. Cost-effectiveness of surgically induced weight loss for the management of type 2 diabetes: modeled lifetime analysis. Diabetes Care 32, 567–574 (2009).
Finkelstein, E. A. & Brown, D. S. Return on investment for bariatric surgery. Am. J. Manag. Care 14, 561–562 (2008).
Flum, D. R. et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N. Engl. J. Med. 361, 445–454 (2009).
O'Brien, P. E. & Dixon, J. B. Pars flaccida versus perigastric pathways for the placement of the Lap-Band® system [abstract]. Obes. Surg. 13, 211 (2003).
Dolan, K., Finch, R. & Fielding, G. Laparoscopic gastric banding and crural repair in the obese patient with a hiatal hernia. Obes. Surg. 13, 772–775 (2003).
Singhal, R. et al. Band slippage and erosion after laparoscopic gastric banding: a meta-analysis. Surg. Endosc. 24, 2980–2986 (2010).
Gagner, M. Leaks after sleeve gastrectomy are associated with smaller bougies: prevention and treatment strategies. Surg. Laparosc. Endosc. Percutan. Tech. 20, 166–169 (2010).
Brethauer, S. A., Harris, J. L., Kroh, M. & Schauer, P. R. Laparoscopic gastric plication for treatment of severe obesity. Surg. Obes. Relat. Dis. 7, 15–22 (2011).
Rubino, F. & Marescaux, J. Effect of duodenal–jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann. Surg. 239, 1–11 (2004).
Strader, A. D. et al. Weight loss through ileal transposition is accompanied by increased ileal hormone secretion and synthesis in rats. Am. J. Physiol. Endocrinol. Metab. 288, E447–E453 (2005).
Lee, H. C., Kim, M. K., Kwon, H. S., Kim, E. & Song, K. H. Early changes in incretin secretion after laparoscopic duodenal-jejunal bypass surgery in type 2 diabetic patients. Obes. Surg. 20, 1530–1535 (2010).
Kasama, K. et al. Laparoscopic sleeve gastrectomy with duodenojejunal bypass: technique and preliminary results. Obes. Surg. doi:10.1007/s11695-009-9873-z.
Gagner, M. Laparoscopic sleeve gastrectomy with ileal interposition (SGIT): a modified duodenal switch for resolution of type 2 diabetes mellitus in lesser obese patients (BMI < 35). World J. Surg. 35, 109–110 (2011).
DePaula, A. L., Stival, A., Halpern, A. & Vencio, S. Thirty-day morbidity and mortality of the laparoscopic ileal interposition associated with sleeve gastrectomy for the treatment of type 2 diabetic patients with BMI <35: an analysis of 454 consecutive patients. World J. Surg. 35, 102–108 (2011).
Kumar, K. V. et al. Ileal interposition with sleeve gastrectomy for control of type 2 diabetes. Diabetes Technol. Ther. 11, 785–789 (2009).
DePaula, A. L., Macedo, A. L., Mota, B. R. & Schraibman, V. Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21–29. Surg. Endosc. 23, 1313–1320 (2009).
Dumonceau, J. M. Evidence-based review of the Bioenterics intragastric balloon for weight loss. Obes. Surg. 18, 1611–1617 (2008).
Genco, A. et al. BioEnterics Intragastric Balloon: the Italian experience with 2,515 patients. Obes. Surg. 15, 1161–1164 (2005).
Tsesmeli, N. & Coumaros, D. The future of bariatrics: endoscopy, endoluminal surgery, and natural orifice transluminal endoscopic surgery. Endoscopy 42, 155–162 (2010).
Aronne, L. J. & Waitman, J. A. Gastric pacing is not enough: additional measures for an effective obesity treatment program. Obes. Surg. 14 (Suppl. 1), S23–S27 (2004).
Zhang, J. & Chen, J. D. Systematic review: applications and future of gastric electrical stimulation. Aliment. Pharmacol. Ther. 24, 991–1002 (2006).
Sanmiguel, C. P. et al. Gastric electrical stimulation with the TANTALUS System in obese type 2 diabetes patients: effect on weight and glycemic control. J. Diabetes Sci. Technol. 3, 964–970 (2009).
Camilleri, M. et al. Intra-abdominal vagal blocking (VBLOC therapy): clinical results with a new implantable medical device. Surgery 143, 723–731 (2008).
National Health and Medical Research Council. Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults. Australian Government Department of Health and Aging [online], (2003).
Fried, M. et al. Inter-disciplinary European guidelines on surgery of severe obesity. Int. J. Obes. (Lond.) 31, 569–577 (2007).
Logue, J. et al. Management of obesity: summary of SIGN guideline. BMJ 340, c154 (2010).
ADA. Standards of medical care in diabetes—2010. Diabetes Care 33 (Suppl. 1), S11–S61 (2010).
Chapman, A. et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic review. Surgery 135, 326–351 (2004).
Buchwald, H., Estok, R., Fahrbach, K., Banel, D. & Sledge, I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery 142, 621–632 (2007).
O'Brien, P., E., McPhail, T., Chaston, T. B. & Dixon, J. B. Systematic review of medium-term weight loss after bariatric operations. Obes. Surg. 16, 1032–1040 (2006).
Acknowledgements
We acknowledge the help of Toni McGee in reviewing, editing and preparing the manuscript for submission.
Author information
Authors and Affiliations
Contributions
J. B. Dixon and G. W. Lambert contributed to all aspects of this manuscript. M. P. Schlaich contributed to the research, discussion of content and editing of the manuscript. N. E. Straznicky and E. A. Lambert contributed to the discussion of content and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors receive research support from Abbott Pharmaceuticals, Allergan Inc., Ardian, Inc. and Scientific Intake. J. B. Dixon is a consultant for Allergan Inc., Metagenics and Scientific Intake, and is on the Medical Advisory Board for Optifast (Nestle Australia). M. P. Schlaich is on the Scientific Advisory Board for Abbott and Novartis.
Rights and permissions
About this article
Cite this article
Dixon, J., Straznicky, N., Lambert, E. et al. Surgical approaches to the treatment of obesity. Nat Rev Gastroenterol Hepatol 8, 429–437 (2011). https://doi.org/10.1038/nrgastro.2011.112
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2011.112
This article is cited by
-
Efficacy and safety of endoscopic sleeve gastroplasty and laparoscopic sleeve gastrectomy with 12+ months of adjuvant multidisciplinary support
BMC Primary Care (2022)
-
The Skeletal Consequences of Bariatric Surgery
Current Osteoporosis Reports (2020)
-
Impact of bariatric surgery on type 2 diabetes: contribution of inflammation and gut microbiome?
Seminars in Immunopathology (2019)
-
Serum IGF-binding protein 2 (IGFBP-2) concentrations change early after gastric bypass bariatric surgery revealing a possible marker of leptin sensitivity in obese subjects
Endocrine (2019)
-
A history of obesity leaves an inflammatory fingerprint in liver and adipose tissue
International Journal of Obesity (2018)