Abstract
Improvements in the sensitivity of the serum TSH assay have revolutionized our strategies for investigating thyroid function and firmly established TSH as the first-line thyroid function test for most clinical situations, including pregnancy. As a single hormone determination, serum TSH provides the most sensitive index to reliably detect thyroid function abnormalities. Normal thyroid function is important to ensure the best possible pregnancy outcome; in addition, disorders of the thyroid gland are relatively frequent in women of childbearing age. The aim of this article is, therefore, to present relevant information on analytical, as well as clinical, aspects regarding serum TSH determination and its usefulness to detect subtle thyroid function abnormalities associated with the pregnant state, namely overt and subclinical hypothyroidism and hyperthyroidism. As these disorders are associated with poor pregnancy outcome, the authors of the present article are in favor of serum TSH measurement for all pregnant women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Spencer, C. A. et al. Applications of a new chemiluninometric thyrotropin assay to subnormal measurement. J. Clin. Endocrinol. Metab. 70, 453–460 (1990).
Baloch, Z. et al. Laboratory medicine practice guidelines: Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 13, 3–126 (2003).
Mandel, S. J., Spencer, C. A. & Hollowell, J. G. Are detection and treatment of thyroid insufficiency in pregnancy feasible? Thyroid 15, 44–53 (2005).
Abalovich, M. et al. Management of thyroid dysfunction during pregnancy and postpartum: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 92 (8 Suppl.), S1–S47 (2007).
Glinoer, D. The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr. Rev. 18, 404–433 (1997).
Dashe, J. S. et al. Thyroid-stimulating hormone in singleton and twin pregnancy: importance of gestational age-specific reference ranges. Obstet. Gynecol. 106, 753–757 (2005).
Wartofsky, L. & Dickey, R. A. The evidence for a narrower thyrotropin reference range is compelling. J. Clin. Endocrinol. Metab. 90, 5483–5488 (2005).
Emerson, C. H. Circulating thyroid stimulating hormones: why, when, and what to measure. Thyroid 19, 1–3 (2009).
Soldin, O. P., Soldin, D. & Sastoque, M. S. Gestation-specific thyroxine and thyroid stimulating hormone levels in the United States and worldwide. Ther. Drug Monit. 29, 553–559 (2007).
Lambert-Messerlian, G. et al. First- and second-trimester thyroid hormone reference data in pregnant women: a FaSTER (First- and Second-Trimester Evaluation of Risk for aneuploidy) Research Consortium study. Am. J. Obstet. Gynecol. 199, 62.e1–62.e6 (2008).
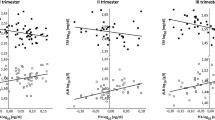
Glinoer, D. et al. Regulation of maternal thyroid during pregnancy. J. Clin. Endocrinol. Metab. 71, 276–287 (1990).
Glinoer, D. et al. Serum levels of intact human chorionic gonadotropin (HCG) and its free alpha and beta subunits, in relation to maternal thyroid stimulation during normal pregnancy. J. Endocrinol. Invest. 16, 881–888 (1993).
Glinoer, D. & Delange, F. The potential repercussions of maternal, fetal, and neonatal hypothyroxinemia on the progeny. Thyroid 10, 871–887 (2000).
Glinoer, D., Riahi, M., Grün, J. P. & Kinthaert, J. Risk of subclinical hypothyroidism in pregnant women with asymptomatic autoimmune thyroid disorders. J. Clin. Endocrinol. Metab. 79, 197–204 (1994).
Spencer, C. A., Hollowell, J. G., Kazarosyan, M. & Braverman, L. E. National Health and Nutrition Examination Survey III thyroid-stimulating hormone (TSH)-thyroperoxidase antibody relationships demonstrate that TSH upper reference limits may be skewed by occult thyroid dysfunction. J. Clin. Endocrinol. Metab. 92, 4236–4240 (2007).
Grün, J. P., Meuris, S., De Nayer, P. & Glinoer, D. The thyrotropic role of human chorionic gonadotrophin (hCG) in the early stages of twin (versus single) pregnancies. Clin. Endocrinol. (Oxf.) 46, 719–725 (1997).
McClain, M. R. et al. Sequential first- and second-trimester TSH, free thyroxine, and thyroid antibody measurements in women with known hypothyroidism: a FaSTER trial study. Am. J. Obstet. Gynecol. 199, 129.e1–129.e6 (2008).
Silvio, R., Swapp, K. J., La'ulu, S. L., Hansen-Suchy, K. & Roberts, W. L. Method specific second-trimester reference intervals for thyroid-stimulating hormone and free thyroxine. Clin. Biochem. 42, 750–753 (2009).
Krassas, G., Poppe, K. & Glinoer, D. Thyroid function and reproductive health. Endocrine Rev. (in press).
LeBeau, S. O. & Mandel, S. J. Thyroid disorders during pregnancy. Endocrinol. Metab. Clin. North Am. 35, 117–136 (2006).
Casey, B. M. et al. Subclinical hyperthyroidism and pregnancy outcomes. Obstet. Gynecol. 107, 337–341 (2006).
Glinoer, D., Rihai, M., Grün, J. P. & Kinthaert, J. Risk of subclinical hypothyroidism in pregnant women with asymptomatic autoimmune thyroid disorders. J. Clin. Endocrinol. Metab. 79, 197–204 (1994).
Casey, B. M. et al. Subclinical hypothyroidism and pregnancy outcomes. Obstet. Gynecol. 105, 239–245 (2005).
Vaidya, B. et al. Screening for thyroid disease in pregnancy: an audit. Clin. Med. 2, 599–600 (2002).
Vaidya, B. et al. Detection of thyroid dysfunction in early pregnancy: universal screening or targeted high-risk case finding? J. Clin. Endocrinol. Metab. 92, 203–207 (2007).
Männistö, T. et al. Thyroid dysfunction and autoantibodies during pregnancy as predictive factors of pregnancy complications and maternal morbidity in later life. J. Clin. Endocrinol. Metab. 95, 1084–1094 (2010).
ACOG News Release. Routine thyroid screening is not recommended for pregnant women [online], (2007).
Burman, K. D. Controversies surrounding pregnancy, maternal thyroid status, and fetal outcome. Thyroid 19, 323–326 (2009).
Abalovich, M. et al. Overt and subclinical hypothyroidism complicating pregnancy. Thyroid 12, 63–68 (2002).
Negro, R. et al. Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications. J. Clin. Endocrinol. Metab. 91, 2587–2591 (2006).
Author information
Authors and Affiliations
Contributions
D. Glinoer and C. A. Spencer researched the data for the article. D. Glinoer and C. A. Spencer provided a substantial contribution to discussions of the content. D. Glinoer and C. A. Spencer contributed equally to writing the article and to review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Glinoer, D., Spencer, C. Serum TSH determinations in pregnancy: how, when and why?. Nat Rev Endocrinol 6, 526–529 (2010). https://doi.org/10.1038/nrendo.2010.91
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2010.91
This article is cited by
-
Accurate interpretation of thyroid dysfunction during pregnancy: should we continue to use published guidelines instead of population-based gestation-specific reference intervals for the thyroid-stimulating hormone (TSH)?
BMC Pregnancy and Childbirth (2022)
-
Intercellular wireless communication network between mother and fetus in rat pregnancy-a study on directed and weighted network
Reproductive Biology and Endocrinology (2019)
-
Urinary iodine and thyroid determinants in pregnancy: a follow up study in Sri Lanka
BMC Pregnancy and Childbirth (2016)
-
Thyroid diseases during pregnancy: A number of important issues
Hormones (2015)
-
Thyroid dysfunction during pregnancy and in postpartum period: treatment and latest recommendations
Archives of Gynecology and Obstetrics (2014)