Key Points
-
The discovery of the V617F mutation in Janus kinase 2 (JAK2) in 2005 provided, for the first time, a molecular taxonomic nexus that definitively linked the myeloproliferative neoplasms (MPNs) polycythaemia vera, essential thrombocythaemia and primary myelofibrosis.
-
JAK2V617F is constitutively activated, and so also provides the rationale for the development of small molecular mass compounds targeted at disrupting such activity in the mutated enzyme.
-
A growing number of JAK inhibitors are being developed for the treatment of MPNs; the JAK1 and JAK2 inhibitor ruxolitinib and the selective JAK2 inhibitor TG101348 are furthest along in clinical development, but many others are undergoing clinical testing.
-
JAK2 inhibitors produce remarkable improvements in spleen size and constitutional symptoms of MPNs but have limited activity in improving cytopaenias, decreasing the mutant JAK2V617F allelic burden or improving marrow fibrosis.
-
The mechanism of action of JAK inhibitors in patients with MPNs is not fully understood as responses are seen both in patients with and without the JAK2V617F mutation.
-
Recently reported knock-in mouse models, in which JAK2V617F is expressed from the endogenous promoter, will become invaluable tools for the development of novel therapies for MPNs and for gaining further understanding of the biology of these malignancies.
-
A series of novel mutant alleles (TET2, ASXL1, CBL, IDH1/IDH2, IKZF1, EZH2 and LNK) have been reported in the last 24 months in subsets of patients with MPNs. However, the role of these alleles in those malignancies remains to be determined.
-
Because JAKs are involved in the pathogenesis of inflammatory and immune-mediated disorders, JAK inhibitors are also being tested in clinical trials for these indications and have shown remarkable results in rheumatoid arthritis and psoriasis as well as in prevention of allograft rejection.
Abstract
Recent advances in our understanding of the pathogenesis of the Philadelphia chromosome-negative myeloproliferative neoplasms, polycythaemia vera, essential thrombocythaemia and myelofibrosis have led to the identification of the mutation V617F in Janus kinase (JAK) as a potential therapeutic target. This information has prompted the development of ATP-competitive JAK2 inhibitors. Therapy with JAK2 inhibitors may induce rapid and marked reductions in spleen size and can lead to remarkable improvements in constitutional symptoms and overall quality of life. Because JAKs are involved in the pathogenesis of inflammatory and immune-mediated disorders, JAK inhibitors are also being tested in clinical trials in patients with rheumatoid arthritis and psoriasis, as well as for the treatment of other autoimmune diseases and for the prevention of allograft rejection. Preliminary results indicate that these agents hold great promise for the treatment of JAK-driven disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
25 March 2011
The information presented in Table 2 on the compound SB1518 was incorrect; the correct information is provided, and has been corrected online.
References
Spivak, J. L. The chronic myeloproliferative disorders: clonality and clinical heterogeneity. Semin. Hematol. 41, 1–5 (2004).
Tefferi, A. & Vardiman, J. W. Classification and diagnosis of myeloproliferative neoplasms: the World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia 22, 14–22 (2008).
Spivak, J. L. Polycythemia vera: myths, mechanisms, and management. Blood 100, 4272–4290 (2002).
Beer, P. A. & Green, A. R. Pathogenesis and management of essential thrombocythemia. Hematology Am. Soc. Hematol. Educ. Program 2009, 621–628 (2009).
Finazzi, G. & Barbui, T. How I treat patients with polycythemia vera. Blood 109, 5104–5111 (2007).
Passamonti, F. et al. A dynamic prognostic model to predict survival in primary myelofibrosis: a study by the IWG-MRT (International Working Group for Myeloproliferative Neoplasms Research and Treatment). Blood 115, 1703–1708 (2010).
Schindler, C. & Darnell, J. E. Jr. Transcriptional responses to polypeptide ligands: the JAK-STAT pathway. Annu. Rev. Biochem. 64, 621–651 (1995).
Prchal, J. F. & Axelrad, A. A. Letter: Bone-marrow responses in polycythemia vera. N. Engl. J. Med. 290, 1382 (1974).
Lutton, J. D. & Levere, R. D. Endogenous erythroid colony formation by peripheral blood mononuclear cells from patients with myelofibrosis and polycythemia vera. Acta Haematol. 62, 94–99 (1979).
Adamson, J. W., Fialkow, P. J., Murphy S., Prchal, J. F. & Steinmann, L. Polycythemia vera: stem-cell and probable clonal origin of the disease. N. Engl. J. Med. 295, 913–916 (1976).
Gilliland, D. G., Blanchard, K. L., Levy J., Perrin S. & Bunn, H. F. Clonality in myeloproliferative disorders: analysis by means of the polymerase chain reaction. Proc. Natl Acad. Sci. USA 88, 6848–6852 (1991).
el Kassar, N., Hetet, G., Li, Y., Briere J. & Grandchamp, B. Clonal analysis of haemopoietic cells in essential thrombocythaemia. Br. J. Haematol. 90, 131–137 (1995).
Tsukamoto, N. et al. Clonality in chronic myeloproliferative disorders defined by X-chromosome linked probes: demonstration of heterogeneity in lineage involvement. Br. J. Haematol. 86, 253–258 (1994).
Neubauer, H. et al. Jak2 deficiency defines an essential developmental checkpoint in definitive hematopoiesis. Cell 93, 397–409 (1998).
Parganas, E. et al. Jak2 is essential for signaling through a variety of cytokine receptors. Cell 93, 85–395 (1998).
Levine, R. L., Pardanani, A., Tefferi, A. & Gilliland, D. G. Role of JAK2 in the pathogenesis and therapy of myeloproliferative disorders. Nature Rev. Cancer 7, 673–683 (2007).
Moliterno, A. R., Hankins, W. D. & Spivak, J. L. Impaired expression of the thrombopoietin receptor by platelets from patients with polycythemia vera. N. Engl. J. Med. 338, 572–580 (1998).
Baxter, E. J. et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 365, 1054–1061 (2005).
James, C. et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 434, 1144–1148 (2005).
Kralovics, R. et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N. Engl. J. Med. 352, 1779–1790 (2005).
Levine, R. L. et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 7, 387–397 (2005).
Zhao, R. et al. Identification of an acquired JAK2 mutation in polycythemia vera. J. Biol. Chem. 280, 22788–22792 (2005). References 18–22 provide the first description of the recurrent somatic mutation (JAK2V617F) in patients with PV, PMF and ET, thus molecularly linking all three disorders.
Lu, X. et al. Expression of a homodimeric type I cytokine receptor is required for JAK2V617F-mediated transformation. Proc. Natl Acad. Sci. USA 102, 18962–18967 (2005).
Dusa, A. et al. Substitution of pseudokinase domain residue Val-617 by large non-polar amino acids causes activation of JAK2. J. Biol. Chem. 283, 12941–12948 (2008).
Scott, L. M. et al. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N. Engl. J. Med. 356, 459–468 (2007). This is the first description of mutations mapping to exon 12 of the JAK2 gene in patients with PV who do not carry the JAK2V617F mutation.
Pietra, D. et al. Somatic mutations of JAK2 exon 12 in patients with JAK2 (V617F)-negative myeloproliferative disorders. Blood 111, 1686–1689 (2008).
Pardanani, A., Lasho, T. L., Finke, C., Hanson, C. A. & Tefferi, A. Prevalence and clinicopathologic correlates of JAK2 exon 12 mutations in JAK2V617F-negative polycythemia vera. Leukemia 21, 1960–1963 (2007).
Wang, Y. L. et al. JAK2 mutations are present in all cases of polycythemia vera. Leukemia 22, 1289 (2008).
Jones, A. V. et al. JAK2 haplotype is a major risk factor for the development of myeloproliferative neoplasms. Nature Genet. 41, 446–449 (2009).
Kilpivaara, O. et al. A germline JAK2 SNP is associated with predisposition to the development of JAK2V617F-positive myeloproliferative neoplasms. Nature Genet. 41, 455–459 (2009).
Olcaydu, D. et al. A common JAK2 haplotype confers susceptibility to myeloproliferative neoplasms. Nature Genet. 41, 450–454 (2009). References 29–31 describe the association between a specific haplotype and a high susceptibility risk to developing JAK2V617F-positive MPNs.
Saharinen, P., Takaluoma, K. & Silvennoinen, O. Regulation of the Jak2 tyrosine kinase by its pseudokinase domain. Mol. Cell Biol. 20, 3387–3395 (2000).
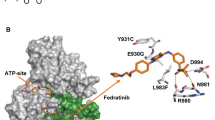
Lucet, I. S. et al. The structural basis of Janus kinase 2 inhibition by a potent and specific pan-Janus kinase inhibitor. Blood 107, 176–183 (2006).
Silva, M. et al. Expression of Bcl-x in erythroid precursors from patients with polycythemia vera. N. Engl. J. Med. 338, 564–571 (1998).
Jamieson, C. H. et al. The JAK2 V617F mutation occurs in hematopoietic stem cells in polycythemia vera and predisposes toward erythroid differentiation. Proc. Natl Acad. Sci. USA 103, 6224–6229 (2006).
Ishii, T., Bruno, E., Hoffman R. & Xu, M. Involvement of various hematopoietic-cell lineages by the JAK2V617F mutation in polycythemia vera. Blood 108, 3128–3134 (2006).
Delhommeau, F. et al. Evidence that the JAK2 G1849T (V617F) mutation occurs in a lymphomyeloid progenitor in polycythemia vera and idiopathic myelofibrosis. Blood 109, 71–77 (2007).
Lacout, C. et al. JAK2V617F expression in murine hematopoietic cells leads to MPD mimicking human PV with secondary myelofibrosis. Blood 108, 1652–1660 (2006).
Wernig, G. et al. Expression of Jak2V617F causes a polycythemia vera-like disease with associated myelofibrosis in a murine bone marrow transplant model. Blood 107, 4274–4281 (2006).
Zaleskas, V. M. et al. Molecular pathogenesis and therapy of polycythemia induced in mice by JAK2 V617F. PLoS ONE 1, e18 (2006).
Lippert, E. et al. The JAK2-V617F mutation is frequently present at diagnosis in patients with essential thrombocythemia and polycythemia vera. Blood 108, 1865–1867 (2006).
Tiedt, R. et al. Ratio of mutant JAK2-V617F to wild-type Jak2 determines the MPD phenotypes in transgenic mice. Blood 111, 3931–3940 (2008).
Nussenzveig, R. H. et al. Imatinib mesylate therapy for polycythemia vera: final result of a phase II study initiated in 2009. Int. J. Hematol. 90, 58–63 (2001).
Shi, J. et al. An open-label assessment of the effects of CYP3A4 inhibitors on the PK/PD of INCB018424 in healthy subjects. J. Clin. Pharmacol. 49, (Abstr. 10) (2009).
Shi, J. et al. An open-label assessment of the effects of rifampin, a potent CYP3A4 inducer on the PK/PD of INCB018424 in healthy subjects. J. Clin. Pharmacol. 49, (Abstr. 9) (2009).
Verstovsek, S. et al. INCB018424, an oral, selective JAK2 inhibitor, shows significant clinical activity in a phase I/II study in patients with primary myelofibrosis (PMF) and post polycythemia vera/essential thrombocythemia myelofibrosis (post-PV/ET MF). Blood 110, Abstr. 558 (2007).
Verstovsek, S. et al. Safety and efficacy of a JAK1 & JAK2 inhibitor, INCB018424, in myelofibrosis. N. Engl. J. Med. 363, 1117–1127 (2010). This report describes the remarkable clinical activity of the oral JAK1 and JAK2 inhibitor INCB018424 (now known as ruxolitinib) in patients with post-ET or post-PV myelofibrosis.
Verstovsek, S. et al. A phase 2 study of INCB018424, an oral, selective JAK1/JAK2 inhibitor, in patients with advanced polycythemia vera and essential thrombocythemia refractory to hydroxyurea. Blood 114, Abstr. 311 (2009).
Barosi, G. et al. Response criteria for essential thrombocythemia and polycythemia vera: results of a European LeukemiaNet consensus conference. Blood 113, 4829–4833 (2009).
Wernig, G. et al. Efficacy of TG101348, a selective JAK2 inhibitor, in treatment of a murine model of JAK2V617F-induced polycythemia vera. Cancer Cell 13, 311–320 (2008).
Pardanani, A. JAK2 inhibitor therapy in myeloproliferative disorders: rationale, preclinical studies and ongoing clinical trials. Leukemia 22, 23–30 (2008).
Pardanani, A. et al. TG101209, a small molecule JAK2-selective kinase inhibitor potently inhibits myeloproliferative disorder-associated JAK2V617F and MPLW515L/K mutations. Leukemia 21, 1658–1668 (2007).
Pardanani, A. et al. A phase I study of TG101348, a selective JAK2 inhibitor, in myelofibrosis: clinical response is accompanied by significant reduction in JAK2V617F allele burden. Blood 114, Abstr. 755 (2009).
Hexner, E. O. et al. Lestaurtinib (CEP701) is a JAK2 inhibitor that suppresses JAK2/STAT5 signaling and the proliferation of primary erythroid cells from patients with myeloproliferative disorders. Blood 111, 5663–5671 (2008).
Knapper, S. et al. A phase 2 trial of the FLT3 inhibitor lestaurtinib (CEP701) as first-line treatment for older patients with acute myeloid leukemia not considered fit for intensive chemotherapy. Blood 108, 3262–3270 (2006).
Smith, B. D. et al. Single-agent CEP-701, a novel FLT3 inhibitor, shows biologic and clinical activity in patients with relapsed or refractory acute myeloid leukemia. Blood 103, 3669–3676 (2004).
Marshall, J. L. et al. Phase I trial of orally administered CEP-701, a novel neurotrophin receptor-linked tyrosine kinase inhibitor. Invest. New Drugs 23, 31–37 (2005).
Santos, F. P. et al. Phase 2 study of CEP-701, an orally available JAK2 inhibitor, in patients with primary or post-polycythemia vera/essential thrombocythemia myelofibrosis. Blood 115, 1131–1136 (2010).
Hexner, E. et al. A multicenter, open label Phase I/II study of CEP701 (Lestaurtinib) in adults with myelofibrosis; a report on phase I: a study of the myeloproliferative disorders research consortium. Blood 114, Abstr. 754 (2009).
Paquette, R. et al. A phase I study of XL019, a selective JAK2 inhibitor, in patients with polycythemia vera. Blood 112, Abstr. 2810 (2008).
Shah, N. et al. A phase I study of XL019, a selective JAK2 inhibitor, in patients with primary myelofibrosis, post-polycythemia vera, or post-essential thrombocythemia myelofibrosis. Blood 112, Abstr. 98 (2008).
Verstovsek, S. et al. Phase I dose-escalation trial of SB1518, a novel JAK2/FLT3 inhibitor, in acute and chronic myeloid diseases, including primary or post-essential thrombocythemia/polycythemia vera myelofibrosis. Blood 114, Abstr. 3905 (2009).
Hedvat, M. et al. The JAK2 inhibitor AZD1480 potently blocks Stat3 signaling and oncogenesis in solid tumors. Cancer Cell 16, 487–497 (2009).
Pardanani, A. et al. CYT387, a selective JAK1/JAK2 inhibitor: in vitro assessment of kinase selectivity and preclinical studies using cell lines and primary cells from polycythemia vera patients. Leukemia 23, 1441–1445 (2009).
Tyner, J. W. et al. CYT387, a novel JAK2 inhibitor, induces hematologic responses and normalizes inflammatory cytokines in murine myeloproliferative neoplasms. Blood 115, 5232–5240 (2010).
Pardanani, A. et al. A Phase I/II study of CYT387, an oral JAK-1/2 inhibitor, in myelofibrosis: significant response rates in anemia, splenomegaly, and constitutional symptoms. Blood 117, Abstr. 460 (2010).
Changelian, P. S. et al. Prevention of organ allograft rejection by a specific Janus kinase 3 inhibitor. Science 302, 875–878 (2003).
Williams, N. K. et al. Dissecting specificity in the Janus kinases: the structures of JAK-specific inhibitors complexed to the JAK1 and JAK2 protein tyrosine kinase domains. J. Mol. Biol. 387, 219–232 (2009).
Jiang, J. K. et al. Examining the chirality, conformation and selective kinase inhibition of 3-(3R, 4R)-4-methyl-3-(methyl(7H-pyrrolo[2, 3-d]pyrimidin-4-yl)amino)piperi din-1-yl)-3-oxopropanenitrile (CP-690,550). J. Med. Chem. 51, 8012–8018 (2008).
Yabu, J. M. & Vincenti, F. Novel immunosuppression: small molecules and biologics. Semin. Nephrol. 27, 479–486 (2007).
Manshouri, T. et al. The JAK kinase inhibitor CP-690, 550 suppresses the growth of human polycythemia vera cells carrying the JAK2V617F mutation. Cancer Sci. 99, 1265–1273 (2008).
Lacronique, V. et al. A TEL-JAK2 fusion protein with constitutive kinase activity in human leukemia. Science 278, 1309–1312 (1997).
Peeters, P. et al. Fusion of TEL, the ETS-variant gene 6 (ETV6), to the receptor-associated kinase JAK2 as a result of t(9;12) in a lymphoid and t(9;15;12) in a myeloid leukemia. Blood 90, 2535–2540 (1997).
Schwaller, J. et al. Transformation of hematopoietic cell lines to growth-factor independence and induction of a fatal myelo- and lymphoproliferative disease in mice by retrovirally transduced TEL/JAK2 fusion genes. EMBO J. 17, 5321–5333 (1998).
Ho, J. M., Beattie, B. K., Squire, J. A., Frank, D. A. & Barber, D. L. Fusion of the ets transcription factor TEL to Jak2 results in constitutive Jak-Stat signaling. Blood 93, 4354–4364 (1999).
Ward, A. C., Touw, I. & Yoshimura, A. The Jak-Stat pathway in normal and perturbed hematopoiesis. Blood 95, 19–29 (2000).
Mullighan, C. G. et al. JAK mutations in high-risk childhood acute lymphoblastic leukemia. Proc. Natl Acad. Sci. USA 106, 9414–9418 (2009).
Xiang, Z. et al. Identification of somatic JAK1 mutations in patients with acute myeloid leukemia. Blood 111, 4809–4812 (2008).
Walters, D. K. et al. Activating alleles of JAK3 in acute megakaryoblastic leukemia. Cancer Cell 10, 65–75 (2006).
Lee, J. W. et al. The JAK2 V617F mutation in de novo acute myelogenous leukemias. Oncogene 25, 1434–1436 (2006).
Jelinek, J. et al. JAK2 mutation 1849G>T is rare in acute leukemias but can be found in CMML, Philadelphia chromosome-negative CML, and megakaryocytic leukemia. Blood 106, 3370–3373 (2005).
Williams, R. T., Roussel, M. F. & Sherr, C. J. Arf gene loss enhances oncogenicity and limits imatinib response in mouse models of Bcr-Abl-induced acute lymphoblastic leukemia. Proc. Natl Acad. Sci. USA 103, 6688–6693 (2006).
Samanta, A. K. et al. Jak2 inhibition deactivates Lyn kinase through the SET-PP2A-SHP1 pathway, causing apoptosis in drug-resistant cells from chronic myelogenous leukemia patients. Oncogene 28, 1669–1681 (2009).
Vannucchi, A. M. et al. Clinical profile of homozygous JAK2V617F mutation in patients with polycythemia vera or essential thrombocythemia. Blood 110, 840–846 (2007).
Leonard, W. J. Cytokines and immunodeficiency diseases. Nature Rev. Immunol. 1, 200–208 (2001).
Kawamura, M. et al. Molecular cloning of L-JAK, a Janus family protein-tyrosine kinase expressed in natural killer cells and activated leukocytes. Proc. Natl Acad. Sci. USA 91, 6374–6378 (1994).
O'Shea, J. J., Pesu, M., Borie, D. C. & Changelian, P. S. A new modality for immunosuppression: targeting the JAK/STAT pathway. Nature Rev. Drug Discov. 3, 555–564 (2004).
Fridman, J. S. et al. Selective inhibition of JAK1 and JAK2 is efficacious in rodent models of arthritis: preclinical characterization of INCB028050. J. Immunol. 184, 5298–5307 (2010).
Kremer, J. M. et al. The safety and efficacy of a JAK inhibitor in patients with active rheumatoid arthritis: results of a double-blind, placebo-controlled phase IIa trial of three dosage levels of CP-690,550 versus placebo. Arthritis Rheum. 60, 1895–1905 (2009).
Coombs, J. H. et al. Improved pain, physical functioning and health status in patients with rheumatoid arthritis treated with CP-690,550, an orally active Janus kinase (JAK) inhibitor: results from a randomised, double-blind, placebo-controlled trial. Ann. Rheum. Dis. 69, 413–416 (2010).
Fleischmann, R. et al. Safety and efficacy after 24 week (wk) dosing of the oral JAK inhibitor CP-690550 (CP) as monotherapy in patients (pts) with active rheumatoid arthritis (RA). Arthritis Rheum. 60 (Suppl.10), 1924 (2009).
Kremer, J. et al. Safety and efficacy after 24 week (WK) dosing of the oral JAK inhibitor CP-690550 (CP) in combination with methrotrexate (MTX) in patients (PTS) with active rheumatoid arthritis (RA). Arthritis Rheum. 60 (Suppl.10), 1925 (2009). References 89–92 describe a series of randomized, double-blind Phase II studies demonstrating remarkable activity of the potent JAK inhibitor tasocitinib (CP 690550) in patients with rheumatoid arthritis.
Williams, W. et al. A randomized placebo-controlled study of INCB018424, a selective Janus kinase 1 & 2 (JAK1 & 2) inhibitor in rheumatoid arthritis (RA). Arthritis Rheum. 58, Abstr. 714 (2008).
Punwani, N. et al. Efficacy and safety of topical INCB018424, a selective Janus kinase 1 and 2 (JAK1 and 2) inhibitor in psoriasis. J. Am. Acad. Dermatol. 60, Abstr. 176 (2009).
Callis Duffin, K. et al. JAK 1 / Jak 2 inhibition: a novel mechanism in the treatment of chronic plaque psoriasis. in Society for Investigative Dermatology Meeting, Atlanta, Georgia, USA (2010).
Pesu, M. et al. Jak3, severe combined immunodeficiency, and a new class of immunosuppressive drugs. Immunol. Rev. 203, 127–142 (2005).
Quaedackers, M. E. et al. Monitoring of the immunomodulatory effect of CP-690,550 by analysis of the JAK/STAT pathway in kidney transplant patients. Transplantation 88, 1002–1009 (2009).
Busque, S. et al. Calcineurin-inhibitor-free immunosuppression based on the JAK inhibitor CP-690,550: a pilot study in de novo kidney allograft recipients. Am. J. Transplant 9, 1936–1945 (2009).
van Gurp, E. A. et al. The effect of the JAK inhibitor CP-690,550 on peripheral immune parameters in stable kidney allograft patients. Transplantation 87, 79–86 (2009).
van Gurp, E. et al. Phase 1 dose-escalation study of CP-690550 in stable renal allograft recipients: preliminary findings of safety, tolerability, effects on lymphocyte subsets and pharmacokinetics. Am. J. Transplant. 8, 1711–1718 (2008).
Borie, D. C. et al. Combined use of the JAK3 inhibitor CP-690,550 with mycophenolate mofetil to prevent kidney allograft rejection in nonhuman primates. Transplantation 80, 1756–1764 (2005).
Tefferi, A. Novel mutations and their functional and clinical relevance in myeloproliferative neoplasms: JAK2, MPL, TET2, ASXL1, CBL, IDH and IKZF1. Leukemia 24, 1128–1138 (2010).
Dawson, M. A. et al. JAK2 phosphorylates histone H3Y41 and excludes HP1α from chromatin. Nature 461, 819–822 (2009).
Wang, Y. et al. Cotreatment with panobinostat and JAK2 inhibitor TG101209 attenuates JAK2V617F levels and signaling and exerts synergistic cytotoxic effects against human myeloproliferative neoplastic cells. Blood 114, 5024–5033 (2009).
Marubayashi, S. et al. HSP90 is a therapeutic target in JAK2-dependent myeloproliferative neoplasms in mice and humans. J. Clin. Invest. 120, 3578–3593 (2010).
Di Nisio, M. et al. The haematocrit and platelet target in polycythemia vera. Br. J. Haematol. 136, 249–259 (2007).
Najean, Y. & Rain, J. D. Treatment of polycythemia vera: use of 32P alone or in combination with maintenance therapy using hydroxyurea in 461 patients greater than 65 years of age. The French Polycythemia Study Group. Blood 89, 2319–2327 (1997).
Cortelazzo, S. et al. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N. Engl. J. Med. 332, 1132–1136 (1995).
Harrison, C. N. et al. Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N. Engl. J. Med. 353, 33–45 (2005).
Barbui, T. et al. Practice guidelines for the therapy of essential thrombocythemia. A statement from the Italian Society of Hematology, the Italian Society of Experimental Hematology and the Italian Group for Bone Marrow Transplantation. Haematologica 89, 215–232 (2004).
Arana-Yi, C. et al. Advances in the therapy of chronic idiopathic myelofibrosis. Oncologist 11, 929–943 (2006).
Mesa, R. A. How I treat symptomatic splenomegaly in patients with myelofibrosis. Blood 113, 5394–5400 (2009).
Quintás-Cardama, A. et al. Lenalidomide plus prednisone results in durable clinical, histopathologic, and molecular responses in patients with myelofibrosis. J. Clin. Oncol. 27, 4760–4766 (2009).
Mesa, R. A. et al. Lenalidomide and prednisone for myelofibrosis: Eastern Cooperative Oncology Group (ECOG) phase-2 trial E4903. Blood 116, 4436–4438 (2010).
Cervantes, F. et al. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood 113, 2895–2901 (2009).
Bacigalupo, A. et al. Allogeneic hemopoietic SCT for patients with primary myelofibrosis: a predictive transplant score based on transfusion requirement, spleen size and donor type. Bone Marrow Transplant. 45, 458–463 (2010).
Stewart, W. A. et al. The role of allogeneic SCT in primary myelofibrosis: a British Society for Blood and Marrow Transplantation study. Bone Marrow Transplant. 45, 1587–1593 (2010).
Kroger, N. et al. Allogeneic stem cell transplantation after reduced-intensity conditioning in patients with myelofibrosis: a prospective, multicenter study of the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Blood 114, 5264–5270 (2009).
Kroger, N. & Mesa, R. A. Choosing between stem cell therapy and drugs in myelofibrosis. Leukemia 22, 474–486 (2008).
Rodig, S. J. et al. Disruption of the Jak1 gene demonstrates obligatory and nonredundant roles of the Jaks in cytokine-induced biologic responses. Cell 93, 373–383 (1998).
Nosaka, T. et al. Defective lymphoid development in mice lacking Jak3. Science 270, 800–802 (1995).
Karaghiosoff, M. et al. Partial impairment of cytokine responses in Tyk2-deficient mice. Immunity 13, 549–560 (2000).
Shimoda, K. et al. Tyk2 plays a restricted role in IFNα signaling, although it is required for IL-12-mediated T cell function. Immunity 13, 561–571 (2000).
Duerr, R. H. et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science 314, 1461–1463 (2006).
Burton, P. R. et al. Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nature Genet. 39, 1329–1337 (2007).
Pikman, Y. et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 3, e270 (2006).
Pardanani, A. D. et al. MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood 108, 3472–3476 (2006).
Vannucchi, A. M. et al. Characteristics and clinical correlates of MPL 515W>L/K mutation in essential thrombocythemia. Blood 112, 844–847 (2008).
Beer, P. A. et al. MPL mutations in myeloproliferative disorders: analysis of the PT-1 cohort. Blood 112, 141–149 (2008).
Chaligne, R. et al. Evidence for MPL W515L/K mutations in hematopoietic stem cells in primitive myelofibrosis. Blood 110, 3735–3743 (2007).
Pikman, Y. et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLOS Med. 3, e270 (2006).
Bersenev, A. et al. Lnk constrains myeloproliferative diseases in mice. J. Clin. Invest. 120, 2058–2069 (2010).
Oh, S. T. et al. Novel mutations in the inhibitory adaptor protein LNK drive JAK-STAT signaling in patients with myeloproliferative neoplasms. Blood 116, 988–992 (2010).
Lasho, T. L., Pardanani, A. & Tefferi, A. LNK mutations in JAK2 mutation-negative erythrocytosis. N. Engl. J. Med. 363, 1189–1190 (2010).
Dupont, S. et al. The JAK2 617V>F mutation triggers erythropoietin hypersensitivity and terminal erythroid amplification in primary cells from patients with polycythemia vera. Blood 110, 1013–1021 (2007).
Theocharides, A. et al. Leukemic blasts in transformed JAK2-V617F-positive myeloproliferative disorders are frequently negative for the JAK2-V617F mutation. Blood 110, 375–379 (2007).
Kralovics, R. et al. Acquisition of the V617F mutation of JAK2 is a late genetic event in a subset of patients with myeloproliferative disorders. Blood 108, 1377–1380 (2006).
Delhommeau, F. et al. Mutation in TET2 in myeloid cancers. N. Engl. J. Med. 360, 2289–2301 (2009). This study is the first to describe mutations in TET2 in patients with myeloid cancers and proposes TET2 mutations as antecedent molecular events to the acquisition of the JAK2V617F mutation.
Tahiliani, M. et al. Conversion of 5-methylcytosine to 5-hydroxymethylcytosine in mammalian DNA by MLL partner TET1. Science 324, 930–935 (2009).
Ito, S. et al. Role of Tet proteins in 5mC to 5hmC conversion, ES-cell self-renewal and inner cell mass specification. Nature 466, 1129–1133 (2010).
Tefferi, A. et al. TET2 mutations and their clinical correlates in polycythemia vera, essential thrombocythemia and myelofibrosis. Leukemia 23, 905–911 (2009).
Carbuccia, N. et al. Mutations of ASXL1 gene in myeloproliferative neoplasms. Leukemia 23, 2183–2186 (2009).
Abdel-Wahab, O. et al. Genetic analysis of transforming events that convert chronic myeloproliferative neoplasms to leukemias. Cancer Res. 70, 447–452 (2010).
Grand, F. H. et al. Frequent CBL mutations associated with 11q acquired uniparental disomy in myeloproliferative neoplasms. Blood 113, 6182–6192 (2009).
Green, A. & Beer, P. Somatic mutations of IDH1 and IDH2 in the leukemic transformation of myeloproliferative neoplasms. N. Engl. J. Med. 362, 369–370 (2010).
Pardanani, A. et al. IDH1 and IDH2 mutation analysis in chronic- and blast-phase myeloproliferative neoplasms. Leukemia 24, 1146–1151 (2010).
Tefferi, A. et al. IDH1 and IDH2 mutation studies in 1473 patients with chronic-, fibrotic- or blast-phase essential thrombocythemia, polycythemia vera or myelofibrosis. Leukemia 24, 1302–1309 (2010).
Jager, R. et al. Deletions of the transcription factor Ikaros in myeloproliferative neoplasms. Leukemia 24, 1290–1298 (2010).
Ernst, T. et al. Inactivating mutations of the histone methyltransferase gene EZH2 in myeloid disorders. Nature Genet. 42, 722–726 (2010).
Bumm, T. G. et al. Characterization of murine JAK2V617F-positive myeloproliferative disease. Cancer Res. 66, 11156–11165 (2006).
Xing, S. et al. Transgenic expression of JAK2V617F causes myeloproliferative disorders in mice. Blood 111, 5109–5117 (2008).
Mullally, A. et al. Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell 17, 584–596 (2010).
Akada, H. et al. Conditional expression of heterozygous or homozygous Jak2V617F from its endogenous promoter induces a polycythemia vera-like disease. Blood 115, 3589–3597 (2010). References 152 and 153 describe mouse models of JAK2V617F-positive MPNs in which the mutant JAK2V617F is expressed from its endogenous promoter, and the authors suggest that JAK2 inhibitor therapy does not eradicate the disease-initiating cells.
Levine, R. L. & Gilliland, D. G. Myeloproliferative disorders. Blood 112, 2190–2198 (2008).
Morgan, K. J. & Gilliland, D. G. A role for JAK2 mutations in myeloproliferative diseases. Annu. Rev. Med. 59, 213–222 (2008).
Roder, S., Steimle, C., Meinhardt, G. & Pahl, H. L. STAT3 is constitutively active in some patients with polycythemia rubra vera. Exp. Hematol. 29, 694–702 (2001).
Komura, E. et al. Spontaneous STAT5 activation induces growth factor independence in idiopathic myelofibrosis: possible relationship with FKBP51 overexpression. Exp. Hematol. 31, 622–630 (2003).
Jamieson, C. H., Barroga, C. F. & Vainchenker, W. P. Miscreant myeloproliferative disorder stem cells. Leukemia 22, 2011–2019 (2008).
Kota, J., Caceres, N. & Constantinescu, S. N. Aberrant signal transduction pathways in myeloproliferative neoplasms. Leukemia 22, 1828–1840 (2008).
Quintás-Cardama, A. et al. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood 115, 3109–3117 (2010).
Ugo, V. et al. Multiple signaling pathways are involved in erythropoietin-independent differentiation of erythroid progenitors in polycythemia vera. Exp. Hematol. 32, 179–187 (2004).
Shi, S. et al. JAK signaling globally counteracts heterochromatic gene silencing. Nature Genet. 38, 1071–1076 (2006).
Liu, P. C. et al. Combined inhibition of Janus kinase 1/2 for the treatment of JAK2V617F-driven neoplasms: selective effects on mutant cells and improvements in measures of disease severity. Clin. Cancer Res. 15, 6891–6900 (2009).
Baffert, F. et al. Potent and selective inhibition of polycythemia by the quinoxaline JAK2 inhibitor NVP-BSK805. Mol. Cancer Ther. 9, 1945–1955 (2010).
Passamonti, F. et al. Molecular and clinical features of the myeloproliferative neoplasm associated with JAK2 exon 12 mutations. Blood 11 Jan 2011 [epub ahead of print]
Scott, L. M. et al. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N. Engl. J. Med. 356, 459–468 (2007).
Moliterno, A. R. et al. An open-label study of CEP-701 in patients with JAK2 V617F-positive PV and ET: update of 39 enrolled patients. Blood 114, Abstr. 753 (2009).
Seymour, F. et al. First report of the phase-I study of the novel oral JAK2 inhibitor sb1518 in patients with myelofibrosis. Haematologica 95 (Suppl. 2), Abstr. 1144 (2010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Srdan Verstovsek has received grant support from Incyte and AstraZeneca.
Related links
Rights and permissions
About this article
Cite this article
Quintás-Cardama, A., Kantarjian, H., Cortes, J. et al. Janus kinase inhibitors for the treatment of myeloproliferative neoplasias and beyond. Nat Rev Drug Discov 10, 127–140 (2011). https://doi.org/10.1038/nrd3264
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd3264
This article is cited by
-
Momelotinib: an emerging treatment for myelofibrosis patients with anemia
Journal of Hematology & Oncology (2022)
-
JAK2 inhibitor persistence in MPN: uncovering a central role of ERK activation
Blood Cancer Journal (2022)
-
The role of JAK inhibitors in hematopoietic cell transplantation
Bone Marrow Transplantation (2022)
-
SENP1-mediated deSUMOylation of JAK2 regulates its kinase activity and platinum drug resistance
Cell Death & Disease (2021)
-
NT157 has antineoplastic effects and inhibits IRS1/2 and STAT3/5 in JAK2V617F-positive myeloproliferative neoplasm cells
Signal Transduction and Targeted Therapy (2020)