Abstract
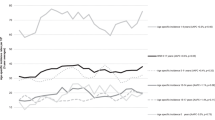
Although the survival rate for adolescents and young adults (AYA) with acute lymphoblastic leukemia (ALL) has steadily improved over the past several decades, it still lags behind that of younger children. This Review explores the reasons for this discrepancy and potential solutions, focusing on patients aged 15–22 years. Recent studies that compared the outcome of AYA patients with ALL treated on pediatric or adult clinical trials have shown substantially better outcomes for this patient population obtained with the pediatric trials. Excellent early results have been obtained for patients with ALL aged up to 40–60 years who were treated in adult study groups with pediatric-based regimens. Targeting biological and socio-political features unique to AYA ALL has reduced the 'AYA gap' and has provided the foundation for basic science and translational and clinical AYA initiatives that are charged with the task of discovering further methods to improve the outcome of AYA with ALL.
Key Points
-
Comparative studies have demonstrated superior outcomes for patients with acute lymphoblastic leukemia (ALL) aged 15–21 years who were treated using pediatric regimens rather than adult regimens
-
Pediatric ALL therapy has traditionally included higher doses of non-myelosuppressive drugs, early and frequent central nervous system prophylaxis and the use of re-induction and long maintenance phases
-
Implementation of pediatric therapy concepts in adult trials have improved outcomes for patients with ALL aged up to 60 years
-
With modern chemotherapy regimens, there is no role for routine use of hematopoietic stem-cell transplantation as consolidation in first remission for patients with ALL aged 15–21 years
-
The overall survival for adolescents and young adults (AYA) with ALL continues to lag behind that of younger children
-
Possible explanations for this 'AYA gap' include differences in tumor biology and the unique social and psychological needs of the AYA population
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Pulte, D., Gondos, A. & Brenner, H. Trends in 5- and 10-year survival after diagnosis with childhood hematologic malignancies in the United States, 1990–2004 J. Natl. Cancer Inst. 100, 1301–1309 (2008).
Pulte, D., Gondos, A. & Brenner, H. Improvement in survival in younger patients with acute lymphoblastic leukemia from the 1980s to the early 21st century. Blood 113, 1408–1411 (2009).
Pollock, B. H. & Birch, J. M. Registration and classification of adolescent and young adult cancer cases. Pediatr. Blood Cancer 50 (Suppl. 5), 1090–1093 (2008).
Bleyer, A., Budd, T. & Montello, M. Adolescents and young adults with cancer: the scope of the problem and criticality of clinical trials. Cancer 107 (Suppl. 7), 1645–1655 (2006).
Albritton K. H., Wiggins C. H., Nelson H. E & Weeks J. C. Site of oncologic specialty care for older adolescents in Utah. J. Clin. Oncol. 25, 4616–4621 (2007).
Howell D. L., Ward. K. C., Austin H. D., Young J. L, Woods W. G. Access to pediatric cancer care by age, race, and diagnosis, and outcomes of cancer treatment in pediatric and adolescent patients in the state of Georgia. J. Clin. Oncol. 25, 4610–4615 (2007).
Yeager, N. D. Hoshaw-Woodard S., Ruymann F. B., Termuhlen A. Patterns of care among adolescents with malignancy in Ohio. J. Pediatr. Hematol. Oncol. 28, 17–22 (2006).
Adam, M. et al. Access to specialized pediatric cancer care in Switzerland. Pediatr. Blood Cancer 54, 721–727 (2010).
Klein-Geltink, J., Shaw A. K., Morrison H I., Barr R. D., Greenberg M. L. Use of pediatric versus adult oncology treatment centers by adolescents 15–19 years old: the Canadian Childhood Cancer Surveillance and Control Program. Eur. J. Cancer 41, 404–410 (2005).
Meadows, A. T. et al. Survival in childhood acute lymphocytic leukemia: effect of protocol and place of treatment. Cancer Invest. 1, 49–55 (1983).
Stiller, C. A. & Eatock, E. M. Patterns of care and survival for children with acute lymphoblastic leukaemia diagnosed between 1980 and 1994. Arch. Dis. Child. 81, 202–208 (1999).
Fern, L. A. & Whelan, J. S. Recruitment of adolescents and young adults to cancer clinical trials--international comparisons, barriers, and implications. Semin. Oncol. 37, e1–8 (2010).
Boissel, N. et al. Should adolescents with acute lymphoblastic leukemia be treated as old children or young adults? Comparison of the French FRALLE-93 and LALA-94 trials. J. Clin. Oncol. 21, 774–780 (2003).
Ramanujachar, R. et al. Adolescents with acute lymphoblastic leukaemia: outcome on UK national pediatric (ALL97) and adult (UKALLXII/E2993) trials. Pediatr. Blood Cancer 48, 254–261 (2007).
de Bont, J. M. et al. Significant difference in outcome for adolescents with acute lymphoblastic leukemia treated on pediatric vs adult protocols in the Netherlands. Leukemia 18, 2032–2035 (2004).
Stock, W. et al. What determines the outcomes for adolescents and young adults with acute lymphoblastic leukemia treated on cooperative group protocols? A comparison of Children's Cancer Group and Cancer and Leukemia Group B studies. Blood 112, 1646–1654 (2008).
Usvasalo, A. et al. Acute lymphoblastic leukemia in adolescents and young adults in Finland. Hematologica 93, 1161–1168 (2008).
Chessells, J. M. et al. The impact of age on outcome in lymphoblastic leukaemia; MRC UKALL X and XA compared: a report from the MRC Pediatric and Adult Working Parties. Leukemia 12, 463–473 (1998).
Harrison, C. J. Cytogenetics of pediatric and adolescent acute lymphoblastic leukaemia. Br. J. Hematol. 144, 147–156 (2009).
Nachman, J. et al. Young adults 16–21 years of age at diagnosis entered on Childrens Cancer Group acute lymphoblastic leukemia and acute myeloblastic leukemia protocols. Results of treatment. Cancer 71 (Suppl. 10), 3377–3385 (1993).
Schiffer, C. A. Differences in outcome in adolescents with acute lymphoblastic leukemia: a consequence of better regimens? Better doctors? Both? J. Clin. Oncol. 21, 760–761 (2003).
US National Library of Medicine. ClinicalTrials.gov [online], (2011).
Barry, E. et al. Favorable outcome for adolescents with acute lymphoblastic leukemia treated on Dana-Farber Cancer Institute Acute Lymphoblastic Leukemia Consortium Protocols. J. Clin. Oncol. 25, 813–819 (2007).
Nachman, J. B. et al. Young adults with acute lymphoblastic leukemia have an excellent outcome with chemotherapy alone and benefit from intensive postinduction treatment: a report from the children's oncology group. J. Clin. Oncol. 27, 5189–5194 (2009).
Pui, C. H. et al. Improved prognosis for older adolescents with acute lymphoblastic leukemia. J. Clin. Oncol. 29, 386–391 (2011).
DeAngelo, D. J. et al. A multicenter phase II study using a dose intensified pediatric regimen in adults with untreated acute lymphoblastic leukemia [abstract]. Blood 110, 587 (2007).
Huguet, F. et al. Pediatric-inspired therapy in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia: the GRAALL-2003 study. J. Clin. Oncol. 27 911–918 (2009).
Storring, J. M. et al. Treatment of adults with BCR-ABL negative acute lymphoblastic leukaemia with a modified pediatric regimen. Br. J. Hematol. 146, 76–85 (2009).
Thomas, D. A. et al. Chemoimmunotherapy with a modified hyper-CVAD and rituximab regimen improves outcome in de novo Philadelphia chromosome-negative precursor B-lineage acute lymphoblastic leukemia. J. Clin. Oncol. 28, 3880–3889 (2010).
Ribera, J. M. et al. Comparison of the results of the treatment of adolescents and young adults with standard-risk acute lymphoblastic leukemia with the Programa Español de Tratamiento en Hematología pediatric-based protocol ALL-96. J. Clin. Oncol. 26, 1843–1849 (2008).
Forman, S. J. Allogeneic hematopoietic cell transplantation for acute lymphoblastic leukemia in adults. Hematol. Oncol. Clin. North Am. 23, 1011–1031 (2009).
Hahn, T. et al. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute lymphoblastic leukemia in adults: an evidence-based review. Biol. Blood Marrow Transplant. 12, 1–30 (2006).
Mattison, R. J. & Larson, R. A. Role of allogeneic hematopoietic cell transplantation in adults with acute lymphoblastic leukemia. Curr. Opin. Oncol. 21, 601–608 (2009).
Goldstone, A. H. et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the International ALL Trial (MRC UKALL XII/ECOG E2993). Blood 111, 1827–1833 (2008).
Rowe, J. M. et al. Induction therapy for adults with acute lymphoblastic leukemia: results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood 106, 3760–3767 (2005).
Pui, C. H. et al. Improved prognosis for older adolescents with acute lymphoblastic leukemia. J. Clin. Oncol. 29, 386–391 (2011).
Greaves, M. F. & Wiemels, J. Origins of chromosome translocations in childhood leukaemia. Nat. Rev. Cancer 3, 639–649 (2003).
Aguiar, R. C. et al. TEL-AML1 fusion in acute lymphoblastic leukaemia of adults. M. R. C. Adult Leukaemia Working Party. Br. J. Hematol. 95, 673–677 (1996).
Borkhardt, A. et al. Incidence and clinical relevance of TEL/AML1 fusion genes in children with acute lymphoblastic leukemia enrolled in the German and Italian multicenter therapy trials. Associazione Italiana Ematologia Oncologia Pediatrica and the Berlin–Frankfurt–Munster Study Group. Blood 90, 571–577 (1997).
Secker-Walker, L. M. et al. Philadelphia positive acute lymphoblastic leukemia in adults: age distribution, BCR breakpoint and prognostic significance. Leukemia 5, 196–199 (1991).
Robinson, H. M. et al. Amplification of AML1 in acute lymphoblastic leukemia is associated with a poor outcome. Leukemia 17, 2249–2250 (2003).
Rubnitz, J. E. et al. TEL gene rearrangement in acute lymphoblastic leukemia: a new genetic marker with prognostic significance. J. Clin. Oncol. 15, 1150–1157 (1997).
Rubnitz, J. E. et al. Prospective analysis of TEL gene rearrangements in childhood acute lymphoblastic leukemia: a Children's Oncology Group study. J. Clin. Oncol. 26, 2186–2191 (2008).
Burmeister, T. et al. Clinical features and prognostic implications of TCF3-PBX1 and ETV6-RUNX1 in adult acute lymphoblastic leukemia. Hematologica 95, 241–246 (2010).
Moorman, A. V. et al. Outcome heterogeneity in childhood high-hyperdiploid acute lymphoblastic leukemia. Blood 102, 2756–2762 (2003).
Möricke, A. et al. Prognostic impact of age in children and adolescents with acute lymphoblastic leukemia: data from the trials ALL-BFM 86, 90, and 95. Klin. Padiatr. 217, 310–320 (2005).
Pieters, R. et al. Clinical relevance of in vitro drug resistance testing in childhood acute lymphoblastic leukemia: the state of the art. Med. Pediatr. Oncol. 22, 299–308 (1994).
Roman-Gomez, J. et al. Promoter hypermethylation of cancer-related genes: a strong independent prognostic factor in acute lymphoblastic leukemia. Blood 104, 2492–2498 (2004).
Raetz, A. E. et al. Cytogenetic and early-response characteristics of adolescents and young adults with acute lymphoblastic leukemia (ALL): a Children's Oncology Group (COG) study [abstract]. J. Clin. Oncol., 28 (Suppl.15), 9509 (2010).
Kearney, S. L. et al. Clinical course and outcome in children with acute lymphoblastic leukemia and asparaginase-associated pancreatitis. Pediatr. Blood Cancer 53, 162–167 (2009).
Athale, U. H. et al. Thromboembolism in children with acute lymphoblastic leukaemia treated on Dana-Farber Cancer Institute protocols: effect of age and risk stratification of disease. Br. J. Hematol. 129, 803–810 (2005).
McNeer, J. L. & Nachman, J. B. The optimal use of steroids in pediatric acute lymphoblastic leukaemia: no easy answers. Br. J. Hematol. 149, 638–652 (2010).
Mattano, L. A. Jr, et al. Osteonecrosis as a complication of treating acute lymphoblastic leukemia in children: a report from the Children's Cancer Group. J. Clin. Oncol. 18, 3262–3272 (2000).
Rubnitz, J. E. et al. Death during induction therapy and first remission of acute leukemia in childhood: the St. Jude experience. Cancer 101, 1677–1684 (2004).
Kearns, G. L. et al. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N. Engl. J. Med. 349, 1157–1167 (2003).
Lambert, G. H. et al. The effect of age, gender, and sexual maturation on the caffeine breath test. Dev. Pharmacol. Ther. 9, 375–388 (1986).
Takahashi, H. et al. Developmental changes in pharmacokinetics and pharmacodynamics of warfarin enantiomers in Japanese children. Clin. Pharmacol. Ther. 68, 541–555 (2000).
Aumente, D. et al. Population pharmacokinetics of high-dose methotrexate in children with acute lymphoblastic leukaemia. Clin. Pharmacokinet. 45, 1227–1238 (2006).
Donelli, M. G. et al. Pharmacokinetics of HD-MTX in infants, children, and adolescents with non-B acute lymphoblastic leukemia. Med. Pediatr. Oncol. 24, 154–159 (1995).
Friedman, I. M. & Litt, I. F. Adolescents' compliance with therapeutic regimens. Psychological and social aspects and intervention. J. Adolesc. Health Care 8, 52–67 (1987).
Lilleyman, J. S. & Lennard, L. Non-compliance with oral chemotherapy in childhood leukaemia. BMJ 313, 1219–1220 (1996).
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353, 487–497 (2005).
Bhatia, S. et al. Non-adherence to oral 6-mercaptopurine (6MP) explains ethnic differences in disease-free survival in children with acute lymphoblastic leukemia (ALL)—a Children's Oncology Group (COG) study (AALL03N1) [abstract]. 52nd ASH Annual Meeting and Exposition. (Orlando, FL, 2010)
Pritchard, M. T. et al. Understanding medication adherence in pediatric acute lymphoblastic leukemia: a review. J. Pediatr. Hematol. Oncol. 28, 816–823 (2006).
Schmiegelow, K. et al. The degree of myelosuppression during maintenance therapy of adolescents with B-lineage intermediate risk acute lymphoblastic leukemia predicts risk of relapse. Leukemia 24, 715–720 (2010).
Fishman, E. Aging out of coverage: young adults with special health needs. Health Aff. (Millwood). 20, 254–266 (2001).
Kogan, M. D. et al. Underinsurance among children in the United States. N. Engl. J. Med. 363, 841–851 (2010).
Martin, S. et al. Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist 12, 816–824 (2007).
Zebrack, B. Mathews-Bradshaw, B. & Siegel, S. Quality cancer care for adolescents and young adults: a position statement. J. Clin. Oncol. 28, 4862–4867 (2010).
Moghrabi, A. et al. Results of the Dana-Farber Cancer Institute ALL Consortium Protocol 95–01 for children with acute lymphoblastic leukemia. Blood 109, 896–904 (2007).
Vrooman, L. M. et al. Erwinia asparaginase after allergy to E. coli asparaginase in children with acute lymphoblastic leukemia. Pediatr. Blood Cancer 54, 199–205 (2010).
Smith, M. A. Update on developmental therapeutics for acute lymphoblastic leukemia. Curr. Hematol. Malig. Rep. 4, 175–182 (2009).
Styczynski, J. et al. In vitro drug resistance profiles of adult versus childhood acute lymphoblastic leukaemia. Br. J. Hematol. 110, 813–818 (2000).
Davidsen, M. L., Dalhoff, K. & Schmiegelow, K. Pharmacogenetics influence treatment efficacy in childhood acute lymphoblastic leukemia. J. Pediatr. Hematol. Oncol. 30, 831–849 (2008).
Harvey, R. C. et al. Identification of novel cluster groups in pediatric high-risk B-precursor acute lymphoblastic leukemia with gene expression profiling: correlation with genome-wide DNA copy number alterations, clinical characteristics, and outcome. Blood 116, 4874–4884 (2010).
Ferrari, A. et al. Starting an adolescent and young adult program: some success stories and some obstacles to overcome. J. Clin. Oncol. 4850–4857 (2010).
Collins, S. R. & Nicholson, J. L. Realizing health reform's potential: young adults and the Affordable Care Act of 2010. Issue Brief (Commonw. Fund) 101, 1–20 (2010).
Acknowledgements
S. P. Hunger is the Ergen Family Chair in Pediatric Cancer. E.S. Schafer is supported by an Alex's Lemonade Stand Foundation Young Investigator Award, the Optimist International Research Fellowship and National Cancer Institute grant 5KL2RR025006. C. P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape, LLC-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Contributions
Both authors contributed to researching the data for the article, discussions of the content, writing the article and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S. Hunger declares an association with the following company: Bristol-Myers Squibb. E. S. Schafer declares no competing interests.
CME AUTHOR
Charles P. Vega, MD, Associate Professor; Residency Director, Department of Family Medicine, University of California, Irvine
Disclosure: Charles P. Vega, MD, has disclosed no relevant financial relationships.
Rights and permissions
About this article
Cite this article
Schafer, E., Hunger, S. Optimal therapy for acute lymphoblastic leukemia in adolescents and young adults. Nat Rev Clin Oncol 8, 417–424 (2011). https://doi.org/10.1038/nrclinonc.2011.77
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2011.77
This article is cited by
-
Value of flow cytometry for MRD-based relapse prediction in B-cell precursor ALL in a multicenter setting
Leukemia (2021)
-
Clinical significance of minimal residual disease in young adults with standard-risk/Ph-negative precursor B-acute lymphoblastic leukemia: results of prospective study
Medical Oncology (2014)
-
Monitoring of minimal residual disease (MRD) is useful to predict prognosis of adult patients with Ph-negative ALL: results of a prospective study (ALL MRD2002 Study)
Journal of Hematology & Oncology (2013)
-
The Adolescent and Young Adult with Cancer: State of the Art-- Acute Leukemias
Current Oncology Reports (2013)