Key Points
-
Disruption of the fibrous cap on vulnerable atherosclerotic coronary plaques leads to exposure of the thrombogenic lipid core to the bloodstream, and is responsible for two-thirds of all coronary events
-
In approximately one-third of patients with acute coronary syndrome (ACS), the thrombus develops after intimal erosion without fibrous cap rupture
-
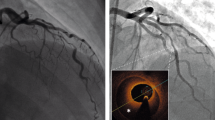
Advances in plaque imaging have allowed clinicians to treat patients with ACS based not only on clinical manifestations, angiographic characteristics, and biomarker data, but also on plaque morphology
-
The use of optical coherence tomography without angiographically obvious plaque rupture can assist in identification and characterization of the culprit lesion plaque morphology
-
Conservative pharmacologic treatment without revascularization might be appropriate in some patients with an intact fibrous cap
Abstract
The latest advances in plaque imaging have provided clinicians with opportunities to treat acute coronary syndrome (ACS) and provide individualized treatment recommendations based not only on clinical manifestations, angiographic characteristics, and biomarker data, but also on the findings of plaque morphology. Although a substantial proportion of ACS events originate from plaques with an intact fibrous cap (IFC), clinicians predominantly equate ACS with plaque rupture arising from thin-cap fibroatheromas. In this Review, we discuss the recent advances in our understanding of plaque morphology in ACS with IFC, reviewing contemporary data from intravascular imaging. We also explore whether use of such imaging might provide a roadmap for more effective management of patients with ACS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Naghavi, M. et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part II. Circulation 108, 1772–1778 (2003).
Jia, H. et al. In vivo diagnosis of plaque erosion and calcified nodule in patients with acute coronary syndrome by intravascular optical coherence tomography. J. Am. Coll. Cardiol. 62, 1748–1758 (2013).
Shmilovich, H. et al. Vulnerable plaque features on coronary CT angiography as markers of inducible regional myocardial hypoperfusion from severe coronary artery stenoses. Atherosclerosis 219, 588–595 (2011).
Kato, K. et al. Nonculprit plaques in patients with acute coronary syndromes have more vulnerable features compared with those with non-acute coronary syndromes: a 3-vessel optical coherence tomography study. Circ. Cardiovasc. Imaging 5, 433–440 (2012).
Suh, W. M., Seto, A. H., Margey, R. J., Cruz-Gonzalez, I. & Jang, I. K. Intravascular detection of the vulnerable plaque. Circ. Cardiovasc. Imaging 4, 169–178 (2011).
Vancraeynest, D., Pasquet, A., Roelants, V., Gerber, B. L. & Vanoverschelde, J. L. Imaging the vulnerable plaque. J. Am. Coll. Cardiol. 57, 1961–1979 (2011).
Goldstein, J. A. et al. Detection of lipid-core plaques by intracoronary near-infrared spectroscopy identifies high risk of periprocedural myocardial infarction. Circ. Cardiovasc. Interv. 4, 429–437 (2011).
Ozaki, Y. et al. Thin-cap fibroatheroma as high-risk plaque for microvascular obstruction in patients with acute coronary syndrome. Circ. Cardiovasc. Imaging 4, 620–627 (2011).
Virmani, R., Kolodgie, F. D., Burke, A. P., Farb, A. & Schwartz, S. M. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler. Thromb. Vasc. Biol. 20, 1262–1275 (2000).
Davies, M. J. The pathophysiology of acute coronary syndromes. Heart 83, 361–366 (2000).
Falk, E., Shah, P. K. & Fuster, V. Coronary plaque disruption. Circulation 92, 657–671 (1995).
Bentzon, J. F., Otsuka, F., Virmani, R. & Falk, E. Mechanisms of plaque formation and rupture. Circ. Res. 114, 1852–1866 (2014).
Falk, E., Nakano, M., Bentzon, J. F., Finn, A. V. & Virmani, R. Update on acute coronary syndromes: the pathologists' view. Eur. Heart J. 34, 719–728 (2013).
Farb, A. et al. Coronary plaque erosion without rupture into a lipid core. A frequent cause of coronary thrombosis in sudden coronary death. Circulation 93, 1354–1363 (1996).
Prati, F. et al. Expert review document part 2: methodology, terminology and clinical applications of optical coherence tomography for the assessment of interventional procedures. Eur. Heart J. 33, 2513–2520 (2012).
Prati, F. et al. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. Eur. Heart J. 31, 401–415 (2010).
Arbustini, E. et al. Plaque erosion is a major substrate for coronary thrombosis in acute myocardial infarction. Heart 82, 269–272 (1999).
Stary, H. C. et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 92, 1355–1374 (1995).
Stary, H. C. et al. A definition of initial, fatty streak, and intermediate lesions of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 89, 2462–2478 (1994).
Stary, H. C. Composition and classification of human atherosclerotic lesions. Virchows Arch. A Pathol. Anat. Histopathol. 421, 277–290 (1992).
Stary, H. C. et al. A definition of the intima of human arteries and of its atherosclerosis-prone regions. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 85, 391–405 (1992).
Stary, H. C. Natural history and histological classification of atherosclerotic lesions: an update. Arterioscler. Thromb. Vasc. Biol. 20, 1177–1178 (2000).
van der Wal, A. C., Becker, A. E., van der Loos, C. M. & Das, P. K. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation 89, 36–44 (1994).
Burke, A. P. et al. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation 97, 2110–2116 (1998).
Virmani, R., Burke, A. P. & Farb, A. Plaque rupture and plaque erosion. Thromb. Haemost. 82 (Suppl. 1), 1–3 (1999).
Henriques de Gouveia, R., van der Wal, A. C., van der Loos, C. M. & Becker, A. E. Sudden unexpected death in young adults. Discrepancies between initiation of acute plaque complications and the onset of acute coronary death. Eur. Heart J. 23, 1433–1440 (2002).
Burke, A. P. et al. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. N. Engl. J. Med. 336, 1276–1282 (1997).
Prati, F. et al. OCT-based diagnosis and management of STEMI associated with intact fibrous cap. JACC Cardiovasc. Imaging 6, 283–287 (2013).
Ozaki, Y. et al. Coronary CT angiographic characteristics of culprit lesions in acute coronary syndromes not related to plaque rupture as defined by optical coherence tomography and angioscopy. Eur. Heart J. 32, 2814–2823 (2011).
Yahagi, K. et al. Multiple simultaneous plaque erosion in 3 coronary arteries. JACC Cardiovasc. Imaging 7, 1172–1174 (2014).
Shin, E. et al. OCT-verified morphological characteristics of atherosclerotic plaques coronary artery spasm sites in vasospastic angina. JACC Cardiovasc. Imaging 8, 1059–1067 (2015).
Ohayon, J. et al. Necrotic core thickness and positive arterial remodeling index: emergent biomechanical factors for evaluating the risk of plaque rupture. Am. J. Physiol. Heart Circ. Physiol. 295, H717–H727 (2008).
Motoyama, S. et al. Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J. Am. Coll. Cardiol. 66, 337–346 (2015).
Motoyama, S. et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J. Am. Coll. Cardiol. 54, 49–57 (2009).
Narula, J. & Achenbach, S. Napkin-ring necrotic cores: defining circumferential extent of necrotic cores in unstable plaques. JACC Cardiovasc. Imaging 2, 1436–1438 (2009).
Kodama, T., Kondo, T., Oida, A., Fujimoto, S. & Narula, J. Computed tomographic angiography-verified plaque characteristics and slow-flow phenomenon during percutaneous coronary intervention. JACC Cardiovasc. Interv. 5, 636–643 (2012).
Yamagishi, M. et al. Morphology of vulnerable coronary plaque: insights from follow-up of patients examined by intravascular ultrasound before an acute coronary syndrome. J. Am. Coll. Cardiol. 35, 106–111 (2000).
Maehara, A., Mintz, G. S. & Weissman, N. J. Advances in intravascular imaging. Circ. Cardiovasc. Interv. 2, 482–490 (2009).
Guagliumi, G. et al. Mechanisms of atherothrombosis and vascular response to primary percutaneous coronary intervention in women versus men with acute myocardial infarction: results of the OCTAVIA study. JACC Cardiovasc. Interv. 7, 958–968 (2014).
Saia, F. et al. Eroded versus ruptured plaques at the culprit site of STEMI: in vivo pathophysiological features and response to primary PCI. JACC Cardiovasc. Imaging 8, 566–575 (2015).
Tearney, G. J. et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J. Am. Coll. Cardiol. 59, 1058–1072 (2012).
Mozaffarian, D. et al. Heart disease and stroke statistics — 2015 update: a report from the American Heart Association. Circulation 131, e29–e322 (2015).
McManus, D. D. et al. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am. J. Med. 124, 40–47 (2011).
Niccoli, G. et al. Plaque rupture and intact fibrous cap assessed by optical coherence tomography portend different outcomes in patients with acute coronary syndrome. Eur. Heart J. http://dx.doi.org/10.1093/eurheartj/ehv029 (2015).
Braunwald, E. Coronary plaque erosion: recognition and management. JACC Cardiovasc. Imaging 6, 288–289 (2013).
Alfonso, F. Spontaneous coronary artery dissection: new insights from the tip of the iceberg? Circulation 126, 667–670 (2012).
Baumgart, D. et al. Acute plaque rupture and myocardial stunning in patient with normal coronary arteriography. Lancet 346, 193–194 (1995).
Yip, A. & Saw, J. Spontaneous coronary artery dissection-A review. Cardiovasc. Diagn. Ther. 5, 37–48 (2015).
Goel, K. et al. Familial spontaneous coronary artery dissection: evidence for genetic susceptibility. JAMA Intern. Med. 175, 821–826 (2015).
Tweet, M. S. et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 126, 579–588 (2012).
Maehara, A. et al. Incidence, morphology, angiographic findings, and outcomes of intramural hematomas after percutaneous coronary interventions: an intravascular ultrasound study. Circulation 105, 2037–2042 (2002).
Saw, J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter. Cardiovasc. Interv. 84, 1115–1122 (2014).
Eleid, M. F. et al. Coronary artery tortuosity in spontaneous coronary artery dissection: angiographic characteristics and clinical implications. Circ. Cardiovasc. Interv. 7, 656–662 (2014).
Alfonso, F., Paulo, M., Lennie, V., Das-Neves, B. & Echavarria-Pinto, M. Fibromuscular dysplasia and spontaneous coronary artery dissection: coincidental association or causality? JACC Cardiovasc. Interv. 6, 638 (2013).
Saw, J. Spontaneous coronary artery dissection. Can. J. Cardiol. 29, 1027–1033 (2013).
Saw, J., Ricci, D., Starovoytov, A., Fox, R. & Buller, C. E. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc. Interv. 6, 44–52 (2013).
Saw, J. et al. Spontaneous coronary artery dissection in patients with fibromuscular dysplasia: a case series. Circ. Cardiovasc. Interv. 5, 134–137 (2012).
Alfonso, F. et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J. Am. Coll. Cardiol. 59, 1073–1079 (2012).
Maehara, A. et al. Intravascular ultrasound assessment of spontaneous coronary artery dissection. Am. J. Cardiol. 89, 466–468 (2002).
Giacoppo, D., Capodanno, D., Dangas, G. & Tamburino, C. Spontaneous coronary artery dissection. Int. J. Cardiol. 175, 8–20 (2014).
Paulo, M. et al. Combined use of OCT and IVUS in spontaneous coronary artery dissection. JACC Cardiovasc. Imaging 6, 830–832 (2013).
Erbel, R. et al. Intravascular ultrasound classification of atherosclerotic lesions according to American Heart Association recommendation. Coron. Artery Dis. 10, 489–499 (1999).
Arnold, J. R., West, N. E., van Gaal, W. J., Karamitsos, T. D. & Banning, A. P. The role of intravascular ultrasound in the management of spontaneous coronary artery dissection. Cardiovasc. Ultrasound 6, 24 (2008).
Nishiguchi, T. et al. Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome. Eur. Heart J. Acute Cardiovasc. Care http://dx.doi.org/10.1177/2048872613504310 (2013).
Sun, H. et al. Coronary microvascular spasm causes myocardial ischemia in patients with vasospastic angina. J. Am. Coll. Cardiol. 39, 847–851 (2002).
Hibino, H. & Kurachi, Y. A new insight into the pathogenesis of coronary vasospasm. Circ. Res. 98, 579–581 (2006).
Beltrame, J. F., Sasayama, S. & Maseri, A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J. Am. Coll. Cardiol. 33, 1442–1452 (1999).
Hung, M. J., Hu, P. & Hung, M. Y. Coronary artery spasm: review and update. Int. J. Med. Sci. 11, 1161–1171 (2014).
Bertrand, M. E. et al. Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary arteriography. Circulation 65, 1299–1306 (1982).
Radico, F., Cicchitti, V., Zimarino, M. & De Caterina, R. Angina pectoris and myocardial ischemia in the absence of obstructive coronary artery disease: practical considerations for diagnostic tests. JACC Cardiovasc. Interv. 7, 453–463 (2014).
Ong, P. et al. Coronary artery spasm as a frequent cause of acute coronary syndrome: the CASPAR (Coronary Artery Spasm in Patients With Acute Coronary Syndrome) Study. J. Am. Coll. Cardiol. 52, 523–527 (2008).
Nakayama, N. et al. Clinical features and prognosis of patients with coronary spasm-induced non-ST-segment elevation acute coronary syndrome. J. Am. Heart Assoc. 3, e000795 (2014).
Nakagawa, H. et al. Coronary spasm preferentially occurs at branch points: an angiographic comparison with atherosclerotic plaque. Circ. Cardiovasc. Interv. 2, 97–104 (2009).
Ong, P. et al. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation 129, 1723–1730 (2014).
Suwaidi, J. A. et al. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation 101, 948–954 (2000).
Hong, Y. J. et al. Plaque components at coronary sites with focal spasm in patients with variant angina: virtual histology-intravascular ultrasound analysis. Int. J. Cardiol. 144, 367–372 (2010).
Author information
Authors and Affiliations
Contributions
J.N. and S.S.K. substantially contributed to discussion of content, wrote, and reviewed and edited the manuscript before submission. G.W.S., M.S., R.V., and T.A. substantially contributed to discussion of content, and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Kanwar, S., Stone, G., Singh, M. et al. Acute coronary syndromes without coronary plaque rupture. Nat Rev Cardiol 13, 257–265 (2016). https://doi.org/10.1038/nrcardio.2016.19
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2016.19
This article is cited by
-
Artificial Intelligence in Intracoronary Imaging
Current Cardiology Reports (2020)
-
Sustained Placental Growth Factor-2 Treatment Does Not Aggravate Advanced Atherosclerosis in Ischemic Cardiomyopathy
Journal of Cardiovascular Translational Research (2017)
-
Advanced Imaging and Diagnostic Methods in the Assessment of Suspected Ischemic Heart Disease in Women
Current Cardiology Reports (2016)