Key Points
-
Contrast-enhanced MRI is a noninvasive, clinically useful technique for accurate quantification and localization of myocardial fibrotic burden
-
Late-gadolinium enhancement imaging can be used to identify the presence, pattern, and size of replacement or focal fibrosis, and has proven prognostic capacity
-
T1 mapping allows for the accurate quantitation of diffuse and infiltrative interstitial fibrosis, and has tremendous prognostic potential in a wide variety of ischaemic and nonischaemic diseases
-
Additional studies are needed to further define the prognostic relevance of late-gadolinium enhancement, T1 mapping, or both techniques used simultaneously, across different pathologies
Abstract
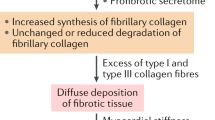
Fibrotic remodelling of the extracellular matrix is a healing mechanism necessary immediately after myocardial injury. However, prolonged increase in myocardial fibrotic activity results in stiffening of the myocardium and heralds adverse outcomes related to systolic and diastolic dysfunction, as well as arrhythmogenesis. Cardiac MRI provides a noninvasive phenotyping tool for accurate and easy detection and quantification of myocardial fibrosis by probing the retention of gadolinium-contrast agent in myocardial tissue. Late-gadolinium enhancement (LGE) cardiac MRI has been used extensively in a large number of studies for measurement of myocardial scarring. T1 mapping, a fairly new technique that can be used to identify the exact T1 value of the tissue, provides a direct measurement of the extracellular volume fraction of the myocardium. In contrast to LGE, T1 mapping can be used to measure diffuse myocardial fibrosis and differentiate between disease processes. In this Review, we describe the basic principles of imaging myocardial fibrosis using contrast-enhanced MRI and summarize its use for prognostic purposes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Weber, K. T., Sun, Y., Bhattacharya, S. K., Ahokas, R. A. & Gerling, I. C. Myofibroblast-mediated mechanisms of pathological remodelling of the heart. Nat. Rev. Cardiol. 10, 15–26 (2013).
Kong, P., Christia, P. & Frangogiannis, N. G. The pathogenesis of cardiac fibrosis. Cell. Mol. Life Sci. 71, 549–574 (2014).
Mewton, N., Liu, C. Y., Croisille, P., Bluemke, D. & Lima, J. A. C. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 57, 891–903 (2011).
Anversa, P., Hiler, B., Ricci, R., Guideri, G. & Olivetti, G. Myocyte cell loss and myocyte hypertrophy in the aging rat heart. J. Am. Coll. Cardiol. 8, 1441–1448 (1986).
Anversa, P. & Nadal-Ginard, B. Myocyte renewal and ventricular remodelling. Nature 415, 240–243 (2002).
Weber, K. T., Brilla, C. G. & Janicki, J. S. Myocardial fibrosis: functional significance and regulatory factors. Cardiovasc. Res. 27, 341–348 (1993).
Weber, K. T. & Brilla, C. G. Pathological hypertrophy and cardiac interstitium. Fibrosis and renin-angiotensin-aldosterone system. Circulation 83, 1849–1865 (1991).
Deichmann, R. & Hasse, A. Quantification of T1 values by snapshot-flash NMR imaging. J. Magn. Reson. 96, 608–612 (1992).
Judd, R. M., Atalay, M. K., Rottman, G. A. & Zerhouni, E. A. Effects of myocardial water exchange on T1 enhancement during bolus administration of MR contrast agents. Magn. Reson. Med. 33, 215–223 (1995).
Manning, W. J., Atkinson, D. J., Grossman, W., Paulin, S. & Edelman, R. R. First-pass nuclear magnetic resonance imaging studies using gadolinium-DTPA in patients with coronary artery disease. J. Am. Coll. Cardiol. 18, 959–965 (1991).
Goldfarb, J. W., Arnold, S. & Roth, M. Gadolinium pharmacokinetics of chronic myocardial infarcts: Implications for late gadolinium-enhanced infarct imaging. J. Magn. Reson. Imaging 30, 763–770 (2009).
Klein, C. et al. Mechanism of late gadolinium enhancement in patients with acute myocardial infarction. J. Cardiovasc. Magn. Reson. 9, 653–658 (2007).
Jerosch-Herold, M., Sheridan, D. & Kushner, J. Cardiac magnetic resonance imaging of myocardial contrast uptake and blood flow in patients affected with idiopathic or familial dilated cardiomyopathy. Am. J. Physiol. Heart Circ. Physiol. 295, H1234–H1242 (2008).
Kim, R. J., Chen, E. L., Lima, J. A. C. & Judd, R. M. Myocardial Gd-DTPA kinetics determine MRI contrast enhancement and reflect the extent and severity of myocardial injury after acute reperfused infarction. Circulation 94, 3318–3326 (1996).
Simonetti, O. P. et al. An improved MR imaging technique for the visualization of myocardial infarction. Radiology 218, 215–223 (2001).
Huber, A. et al. Determining myocardial viability in myocardial infarct. Comparison of single and multisclice MRI techniques with TurboFlash and TrueFISP sequences [German]. Radiologe 44, 146–151 (2004).
Kellman, P., Arai, A. E., McVeigh, E. R. & Aletras, A. H. Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement. Magn. Reson. Med. 47, 372–383 (2002).
Wagner, A. et al. Effects of time, dose, and inversion time for acute myocardial infarct size measurements based on magnetic resonance imaging-delayed contrast enhancement. J. Am. Coll. Cardiol. 47, 2027–2033 (2006).
Kim, R. J. et al. Performance of delayed-enhancement magnetic resonance imaging with gadoversetamide contrast for the detection and assessment of myocardial infarction: an international, multicenter, double-blinded, randomized trial. Circulation 117, 629–637 (2008).
Kwong, R. Y. & Farzaneh-Far, A. Measuring myocardial scar by CMR. JACC Cardiovasc. Imaging 4, 157–160 (2011).
Judd, R. M. et al. Physiological basis of myocardial contrast enhancement in fast magnetic resonance images of 2-day-old reperfused canine infarcts. Circulation 92, 1902–1910 (1995).
Lima, J. A. et al. Regional heterogeneity of human myocardial infarcts demonstrated by contrast-enhanced MRI. Potential mechanisms. Circulation 92, 1117–1125 (1995).
Amado, L. C. et al. Accurate and objective infarct sizing by contrast-enhanced magnetic resonance imaging in a canine myocardial infarction model. J. Am. Coll. Cardiol. 44, 2383–2389 (2004).
Flett, A. S. et al. Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc. Imaging 4, 150–156 (2011).
Spiewak, M. et al. Comparison of different quantification methods of late gadolinium enhancement in patients with hypertrophic cardiomyopathy. Eur. J. Radiol. 74, e149–e153 (2010).
White, S. K., Flett, A. S. & Moon, J. C. Automated scar quantification by CMR: a step in the right direction. J. Thorac. Dis. 5, 381–382 (2013).
Kramer, C. M., Barkhausen, J., Flamm, S. D., Kim, R. J. & Nagel, E. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J. Cardiovasc. Magn. Reson. 15, 91 (2013).
Hundley, W. G. et al. Society for Cardiovascular Magnetic Resonance guidelines for reporting cardiovascular magnetic resonance examinations. J. Cardiovasc. Magn. Reson. 11, 5 (2009).
Schulz-Menger, J. et al. Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) board of trustees task force on standardized post processing. J. Cardiovasc. Magn. Reson. 15, 35 (2013).
Wu, E. et al. Visualisation of presence, location, and transmural extent of healed Q-wave and non-Q-wave myocardial infarction. Lancet 357, 21–28 (2001).
Azevedo, C. F. et al. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J. Am. Coll. Cardiol. 56, 278–287 (2010).
Moon, J. C. C. et al. The histologic basis of late gadolinium enhancement cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 43, 2260–2264 (2004).
Kim, R. et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N. Engl. J. Med. 343, 1445–1453 (2000).
Kim, R. et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 100, 1992–2002 (1999).
Wagner, A. et al. Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet 361, 374–379 (2003).
Shah, D. J. et al. Prevalence of regional myocardial thinning and relationship with myocardial scarring in patients with coronary artery disease. JAMA 309, 909–918 (2013).
Choi, K. M. et al. Transmural extent of acute myocardial infarction predicts long-term improvement in contractile function. Circulation 104, 1101–1107 (2001).
Gerber, B. L. et al. Prognostic value of myocardial viability by delayed-enhanced magnetic resonance in patients with coronary artery disease and low ejection fraction: impact of revascularization therapy. J. Am. Coll. Cardiol. 59, 825–835 (2012).
Romero, J., Xue, X., Gonzalez, W. & Garcia, M. J. CMR imaging assessing viability in patients with chronic ventricular dysfunction due to coronary artery disease: a meta-analysis of prospective trials. JACC Cardiovasc. Imaging 5, 494–508 (2012).
Kelle, S. et al. Prognostic value of myocardial infarct size and contractile reserve using magnetic resonance imaging. J. Am. Coll. Cardiol. 54, 1770–1777 (2009).
Roes, S. D. et al. Comparison of myocardial infarct size assessed with contrast-enhanced magnetic resonance imaging and left ventricular function and volumes to predict mortality in patients with healed myocardial infarction. Am. J. Cardiol. 100, 930–936 (2007).
Krittayaphong, R., Saiviroonporn, P., Boonyasirinant, T. & Udompunturak, S. Prevalence and prognosis of myocardial scar in patients with known or suspected coronary artery disease and normal wall motion. J. Cardiovasc. Magn. Reson. 13, 2 (2011).
Kwong, R. et al. Impact of unrecognized myocardial scar detected by cardiac magnetic resonance imaging on event-free survival in patients presenting with signs or symptoms of coronary artery disease. Circulation 113, 2733–2743 (2006).
Bello, D. et al. Cardiac magnetic resonance imaging: infarct size is an independent predictor of mortality in patients with coronary artery disease. Magn. Reson. Imaging 29, 50–56 (2011).
Tarantini, G. et al. Duration of ischemia is a major determinant of transmurality and severe microvascular obstruction after primary angioplasty: a study performed with contrast-enhanced magnetic resonance. J. Am. Coll. Cardiol. 46, 1229–1235 (2005).
Francone, M. et al. Impact of primary coronary angioplasty delay on myocardial salvage, infarct size, and microvascular damage in patients with ST-segment elevation myocardial infarction: insight from cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 54, 2145–2153 (2009).
Ingkanisorn, W. P., Rhoads, K. L., Aletras, A. H., Kellman, P. & Arai, A. E. Gadolinium delayed enhancement cardiovascular magnetic resonance correlates with clinical measures of myocardial infarction. J. Am. Coll. Cardiol. 43, 2253–2259 (2004).
Baks, T. et al. Effects of primary angioplasty for acute myocardial infarction on early and late infarct size and left ventricular wall characteristics. J. Am. Coll. Cardiol. 47, 40–44 (2006).
Larose, E. et al. Predicting late myocardial recovery and outcomes in the early hours of ST-segment elevation myocardial infarction traditional measures compared with microvascular obstruction, salvaged myocardium, and necrosis characteristics by cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 55, 2459–2469 (2010).
Wu, K. C. et al. Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation 97, 765–772 (1998).
Hadamitzky, M. et al. Prognostic value of late gadolinium enhancement in cardiovascular magnetic resonance imaging after acute ST-elevation myocardial infarction in comparison with single-photon emission tomography using Tc99m-Sestamibi. Eur. Heart J. Cardiovasc. Imaging 15, 216–225 (2014).
Cochet, A. A. et al. Major prognostic impact of persistent microvascular obstruction as assessed by contrast-enhanced cardiac magnetic resonance in reperfused acute myocardial infarction. Eur. Radiol. 19, 2117–2126 (2009).
de Waha, S. et al. Impact of early vs. late microvascular obstruction assessed by magnetic resonance imaging on long-term outcome after ST-elevation myocardial infarction: a comparison with traditional prognostic markers. Eur. Heart J. 31, 2660–2668 (2010).
Steel, K. et al. Complementary prognostic values of stress myocardial perfusion and late gadolinium enhancement imaging by cardiac magnetic resonance in patients with known or suspected coronary artery disease. Circulation 120, 1390–1400 (2009).
Eitel, I. et al. Prognostic significance and determinants of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. J. Am. Coll. Cardiol. 55, 2470–2479 (2010).
Schmidt, A. et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Circulation 115, 2006–2014 (2007).
Bello, D. et al. Infarct morphology identifies patients with substrate for sustained ventricular tachycardia. J. Am. Coll. Cardiol. 45, 1104–1108 (2005).
Roes, S. D. et al. Infarct tissue heterogeneity assessed with contrast-enhanced MRI predicts spontaneous ventricular arrhythmia in patients with ischemic cardiomyopathy and implantable cardioverter-defibrillator. Circ. Cardiovasc. Imaging 2, 183–190 (2009).
Scott, P. A. et al. The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators. Circ. Arrhythm. Electrophysiol. 4, 324–330 (2011).
Yan, A. T. et al. Characterization of the peri-infarct zone by contrast-enhanced cardiac magnetic resonance imaging is a powerful predictor of post-myocardial infarction mortality. Circulation 114, 32–39 (2006).
McCrohon, J. A. et al. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation 108, 54–59 (2003).
Mahrholdt, H., Wagner, A., Judd, R. M., Sechtem, U. & Kim, R. J. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur. Heart J. 26, 1461–1474 (2005).
Lehrke, S. et al. Use of cardiovascular magnetic resonance for risk stratification in chronic heart failure: prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy. Heart 97, 727–732 (2011).
Wu, K. C. et al. Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J. Am. Coll. Cardiol. 51, 2414–2421 (2008).
Perazzolo Marra, M. et al. Impact of the presence and amount of myocardial fibrosis by cardiac magnetic resonance on arrhythmic outcome and sudden cardiac death in nonischemic dilated cardiomyopathy. Heart Rhythm. 11, 856–863 (2014).
Iles, L. et al. Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. J. Am. Coll. Cardiol. 57, 821–828 (2011).
Moon, J. C. et al. Myocardial late gadolinium enhancement cardiovascular magnetic resonance in hypertrophic cardiomyopathy caused by mutations in troponin I. Heart 91, 1036–1040 (2005).
Kwon, D. H. et al. Cardiac magnetic resonance detection of myocardial scarring in hypertrophic cardiomyopathy: correlation with histopathology and prevalence of ventricular tachycardia. J. Am. Coll. Cardiol. 54, 242–249 (2009).
Bruder, O. et al. Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 56, 875–887 (2010).
O'Hanlon, R. et al. Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 56, 867–874 (2010).
Adabag, A. S. et al. Occurrence and frequency of arrhythmias in hypertrophic cardiomyopathy in relation to delayed enhancement on cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 51, 1369–1374 (2008).
Rubinshtein, R. et al. Characteristics and clinical significance of late gadolinium enhancement by contrast-enhanced magnetic resonance imaging in patients with hypertrophic cardiomyopathy. Circ. Heart Fail. 3, 51–58 (2010).
Green, J. J., Berger, J. S., Kramer, C. M. & Salerno, M. Prognostic value of late gadolinium enhancement in clinical outcomes for hypertrophic cardiomyopathy. JACC Cardiovasc. Imaging 5, 370–377 (2012).
Ismail, T. F. et al. Role of late gadolinium enhancement cardiovascular magnetic resonance in the risk stratification of hypertrophic cardiomyopathy. Heart http://dx.doi.org/10.1136/heartjnl-2013-305471.
Austin, B. A. et al. Delayed hyper-enhancement magnetic resonance imaging provides incremental diagnostic and prognostic utility in suspected cardiac amyloidosis. JACC Cardiovasc. Imaging 2, 1369–1377 (2009).
Maceira, A. M., Prasad, S. K., Hawkins, P. N., Roughton, M. & Pennell, D. J. Cardiovascular magnetic resonance and prognosis in cardiac amyloidosis. J. Cardiovasc. Magn. Reson. 10, 54 (2008).
Ruberg, F. L. et al. Diagnostic and prognostic utility of cardiovascular magnetic resonance imaging in light-chain cardiac amyloidosis. Am. J. Cardiol. 103, 544–549 (2009).
Rochitte, C. E. et al. Myocardial delayed enhancement by magnetic resonance imaging in patients with Chagas' disease: a marker of disease severity. J. Am. Coll. Cardiol. 46, 1553–1558 (2005).
Schumm, J. et al. Cardiovascular magnetic resonance risk stratification in patients with clinically suspected myocarditis. J. Cardiovasc. Magn. Reson. 16, 14 (2014).
Ferreira, V. M. et al. T1 mapping for the diagnosis of acute myocarditis using CMR: comparison to T2-weighted and late gadolinium enhanced imaging. JACC Cardiovasc. Imaging 6, 1048–1058 (2013).
Mahrholdt, H. et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation 114, 1581–1590 (2006).
Salemi, V. M. et al. Late gadolinium enhancement magnetic resonance imaging in the diagnosis and prognosis of endomyocardial fibrosis patients. Circ. Cardiovasc. Imaging 4, 304–311 (2011).
Neilan, T. G. et al. The incidence, pattern, and prognostic value of left ventricular myocardial scar by late gadolinium enhancement in patients with atrial fibrillation. J. Am. Coll. Cardiol. 62, 2205–2214 (2013).
Krittayaphong, R. et al. Prognostic value of late gadolinium enhancement in hypertensive patients with known or suspected coronary artery disease. Int. J. Cardiovasc. Imaging 26 (Suppl. 1), 123–131 (2010).
Kwong, R. et al. Incidence and prognostic implication of unrecognized myocardial scar characterized by cardiac magnetic resonance in diabetic patients without clinical evidence of myocardial infarction. Circulation 118, 1011–1020 (2008).
Schelbert, E. B. et al. Prevalence and prognosis of unrecognized myocardial infarction determined by cardiac magnetic resonance in older adults. JAMA 308, 890–896 (2012).
Ebeling Barbier, C., Bjerner, T., Johansson, L., Lind, L. & Ahlström, H. Myocardial scars more frequent than expected: magnetic resonance imaging detects potential risk group. J. Am. Coll. Cardiol. 48, 765–771 (2006).
Venkatesh, B. A. et al. Association of longitudinal changes in left ventricular structure and function with myocardial fibrosis: the multi-ethnic study of atherosclerosis study. Hypertension 64, 508–515 (2014).
Imai, M. et al. Multi-Ethnic Study of Atherosclerosis: association between left atrial function using tissue tracking from cine MR imaging and myocardial fibrosis. Radiology http://dx.doi.org/10.1148/radiol.14131971.
Moreo, A. et al. Influence of myocardial fibrosis on left ventricular diastolic function: noninvasive assessment by cardiac magnetic resonance and echo. Circ. Cardiovasc. Imaging 2, 437–443 (2009).
Donekal, S. et al. Interstitial fibrosis, left ventricular remodeling, and myocardial mechanical behavior in a population-based multiethnic cohort: the Multi-Ethnic Study of Atherosclerosis (MESA) study. Circ. Cardiovasc. Imaging 7, 292–302 (2014).
Turkbey, E. B. et al. Myocardial structure, function, and scar in patients with type 1 diabetes mellitus. Circulation 124, 1737–1746 (2011).
Akoum, N. et al. Atrial fibrosis quantified using late gadolinium enhancement MRI is associated with sinus node dysfunction requiring pacemaker implant. J. Cardiovasc. Electrophysiol. 23, 44–50 (2012).
Daccarett, M. et al. Association of left atrial fibrosis detected by delayed-enhancement magnetic resonance imaging and the risk of stroke in patients with atrial fibrillation. J. Am. Coll. Cardiol. 57, 831–838 (2011).
McGann, C. et al. Atrial fibrillation ablation outcome is predicted by left atrial remodeling on MRI. Circ. Arrhythm. Electrophysiol. 7, 23–30 (2014).
Oakes, R. S. et al. Detection and quantification of left atrial structural remodeling with delayed-enhancement magnetic resonance imaging in patients with atrial fibrillation. Circulation 119, 1758–1767 (2009).
Babu-Narayan, S. V. et al. Late gadolinium enhancement cardiovascular magnetic resonance of the systemic right ventricle in adults with previous atrial redirection surgery for transposition of the great arteries. Circulation 111, 2091–2098 (2005).
Chen, C. A. et al. Circulating biomarkers of collagen type I metabolism mark the right ventricular fibrosis and adverse markers of clinical outcome in adults with repaired tetralogy of Fallot. Int. J. Cardiol. 167, 2963–2968 (2013).
Arheden, H., Saeed, M. & Higgins, C. Measurement of the distribution volume of gadopentetate dimeglumine at echo-planar MR imaging to quantify myocardial infarction: comparison with 99mTc-DTPA autoradiography in rats. Radiology 211, 698–708 (1999).
Look, D. C. & Locker, D. R. Time saving in measurement of NMR and EPR relaxation times. Rev. Sci. Instrum. 41, 250–251 (1970).
Messroghli, D. et al. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn. Reson. Med. 52, 141–146 (2004).
Chow, K. et al. Saturation recovery single-shot acquisition (SASHA) for myocardial T1 mapping. Magn. Reson. Med. 71, 2082–2095 (2014).
Weingärtner, S. et al. Heart-rate independent myocardial T1-mapping using combined saturation and inversion preparation pulses. J. Cardiovasc. Magn. Reson. 15, P46 (2013).
Amano, Y., Tachi, M. & Kumita, S. Three-dimensional Look-Locker MRI for evaluation of postcontrast myocardial and blood T1 values: comparison with two-dimensional Look-Locker and late gadolinium enhancement MRI. Acta Radiol. 54, 8–13 (2013).
Coniglio, A. et al. Multiple 3D inversion recovery imaging for volume T1 mapping of the heart. Magn. Reson. Med. 69, 163–170 (2013).
Xue, H. et al. Phase-sensitive inversion recovery for myocardial T1 mapping with motion correction and parametric fitting. Magn. Reson. Med. 69, 1408–1420 (2013).
Clique, H., Cheng, H.-L. M., Marie, P.-Y., Felblinger, J. & Beaumont, M. 3D myocardial T1 mapping at 3T using variable flip angle method: pilot study. Magn. Reson. Med. 71, 823–829 (2014).
Fontana, M. et al. Comparison of T1 mapping techniques for ECV quantification. Histological validation and reproducibility of ShMOLLI versus multibreath-hold T1 quantification equilibrium contrast CMR. J. Cardiovasc. Magn. Reson. 14, 88 (2012).
Roujol, S. et al. Accuracy, precision, and reproducibility of four T1 mapping sequences: a head-to-head comparison of MOLLI, ShMOLLI, SASHA, and SAPPHIRE. Radiology http://dx.doi.org/10.1148/radiol.14140296.
Piechnik, S. et al. Shortened modified Look-Locker inversion recovery (ShMOLLI) for clinical myocardial T1-mapping at 1.5 and 3 T within a 9 heartbeat breathhold. J. Cardiovasc. Magn. Reson. 12, 69 (2010).
Schelbert, E. et al. Myocardial extravascular extracellular volume fraction measurement by gadolinium cardiovascular magnetic resonance in humans: slow infusion versus bolus. J. Cardiovasc. Magn. Reson. 13, 16 (2011).
Kawel, N. et al. T1 mapping of the myocardium: intra-individual assessment of post-contrast T1 time evolution and extracellular volume fraction at 3T for Gd-DTPA and Gd-BOPTA. J. Cardiovasc. Magn. Reson. 14, 26 (2012).
Gai, N. et al. T1 mapping of the gadolinium-enhanced myocardium: adjustment for factors affecting interpatient comparison. Magn. Reson. Med. 65, 1407–1415 (2011).
Flett, A. et al. Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation 122, 138–144 (2010).
Knowles, B. R. et al. Pharmacokinetic modeling of delayed gadolinium enhancement in the myocardium. Magn. Reson. Med. 60, 1524–1530 (2008).
White, S. K. et al. T1 mapping for myocardial extracellular volume measurement by CMR: bolus only versus primed infusion technique. JACC Cardiovasc. Imaging 6, 955–962 (2013).
Kawel, N. et al. T1 mapping of the myocardium: intra-individual assessment of the effect of field strength, cardiac cycle and variation by myocardial region. J. Cardiovasc. Magn. Reson. 14, 27 (2012).
Raman, F. S. et al. Modified look-locker inversion recovery T1 mapping indices: assessment of accuracy and reproducibility between magnetic resonance scanners. J. Cardiovasc. Magn. Reson. 15, 64 (2013).
Shao, J., Nguyen, K.-L., Natsuaki, Y., Spottiswoode, B. & Hu, P. Instantaneous signal loss simulation (InSiL): an improved algorithm for myocardial T1 mapping using the MOLLI sequence. J. Magn. Reson. Imaging http://dx.doi.org/10.1002/jmri.24599.
Moon, J. C. et al. Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR working group of the European Society of Cardiology consensus statement. J. Cardiovasc. Magn. Reson. 15, 92 (2013).
Iles, L. et al. Evaluation of diffuse myocardial fibrosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J. Am. Coll. Cardiol. 52, 1574–1580 (2008).
Sibley, C. T. et al. T1 mapping in cardiomyopathy at cardiac MR: comparison with endomyocardial biopsy. Radiology 265, 724–732 (2012).
Mascherbauer, J. et al. Cardiac magnetic resonance postcontrast T1 time is associated with outcome in patients with heart failure and preserved ejection fraction. Circ. Cardiovasc. Imaging 6, 1056–1065 (2013).
Miller, C. A. et al. Comprehensive validation of cardiovascular magnetic resonance techniques for the assessment of myocardial extracellular volume. Circ. Cardiovasc. Imaging 6, 373–383 (2013).
Brooks, J., Kramer, C. M. & Salerno, M. Markedly increased volume of distribution of gadolinium in cardiac amyloidosis demonstrated by T1 mapping. J. Magn. Reson. Imaging 38, 1591–1595 (2013).
Kellman, P. et al. Extracellular volume fraction mapping in the myocardium, part 2: initial clinical experience. J. Cardiovasc. Magn. Reson. 14, 64 (2012).
Ntusi, N. A. et al. Subclinical myocardial inflammation and diffuse fibrosis are common in systemic sclerosis–a clinical study using myocardial T1-mapping and extracellular volume quantification. J. Cardiovasc. Magn. Reson. 16, 21 (2014).
Brouwer, W. P. et al. In-vivo T1 cardiovascular magnetic resonance study of diffuse myocardial fibrosis in hypertrophic cardiomyopathy. J. Cardiovasc. Magn. Reson. 16, 28 (2014).
Ellims, A. H. et al. Diffuse myocardial fibrosis in hypertrophic cardiomyopathy can be identified by cardiovascular magnetic resonance, and is associated with left ventricular diastolic dysfunction. J. Cardiovasc. Magn. Reson. 14, 76 (2012).
Fang, L. et al. Associations between fibrocytes and postcontrast myocardial T1 times in hypertrophic cardiomyopathy. J. Am. Heart Assoc. 2, e000270 (2013).
Tham, E. B. et al. Diffuse myocardial fibrosis by T1-mapping in children with subclinical anthracycline cardiotoxicity: relationship to exercise capacity, cumulative dose and remodeling. J. Cardiovasc. Magn. Reson. 15, 48 (2013).
Neilan, T. G. et al. Myocardial extracellular volume by cardiac magnetic resonance imaging in patients treated with anthracycline-based chemotherapy. Am. J. Cardiol. 111, 717–722 (2013).
Ugander, M. et al. Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur. Heart J. 33, 1268–1278 (2012).
Sado, D. M. et al. Cardiovascular magnetic resonance measurement of myocardial extracellular volume in health and disease. Heart 98, 1436–1441 (2012).
Liu, C.-Y. et al. Evaluation of age-related interstitial myocardial fibrosis with cardiac magnetic resonance contrast-enhanced T1 mapping: MESA (Multi-Ethnic Study of Atherosclerosis). J. Am. Coll. Cardiol. 62, 1280–1287 (2013).
Neilan, T. G. et al. Myocardial extracellular volume fraction from T1 measurements in healthy volunteers and mice: relationship to aging and cardiac dimensions. JACC Cardiovasc. Imaging 6, 672–683 (2013).
Olivetti, G. et al. Gender differences and aging: effects on the human heart. J. Am. Coll. Cardiol. 26, 1068–1079 (1995).
Scantlebury, D. C. & Borlaug, B. A. Why are women more likely than men to develop heart failure with preserved ejection fraction? Curr. Opin. Cardiol. 26, 562–568 (2011).
Ng, A. C. T. et al. Association between diffuse myocardial fibrosis by cardiac magnetic resonance contrast-enhanced T1 mapping and subclinical myocardial dysfunction in diabetic patients: a pilot study. Circ. Cardiovasc. Imaging 5, 51–59 (2012).
Rao, A. D. et al. Aldosterone and myocardial extracellular matrix expansion in type 2 diabetes mellitus. Am. J. Cardiol. 112, 73–78 (2013).
Jellis, C. et al. Association of imaging markers of myocardial fibrosis with metabolic and functional disturbances in early diabetic cardiomyopathy. Circ. Cardiovasc. Imaging 4, 693–702 (2011).
Wong, T. C. et al. Myocardial extracellular volume fraction quantified by cardiovascular magnetic resonance is increased in diabetes and associated with mortality and incident heart failure admission. Eur. Heart J. 35, 657–664 (2013).
Chin, C. W. L. et al. Optimization and comparison of myocardial T1 techniques at 3T in patients with aortic stenosis. Eur. Heart J. Cardiovasc. Imaging 15, 556–565 (2013).
Flett, A. S. et al. Diffuse myocardial fibrosis in severe aortic stenosis: an equilibrium contrast cardiovascular magnetic resonance study. Eur. Heart J. Cardiovasc. Imaging 13, 819–826 (2012).
Marzluf, B. A. et al. Diffuse myocardial fibrosis by post-contrast T1-time predicts outcome in heart failure with preserved ejection fraction. J. Cardiovasc. Magn. Reson. 15, M6 (2013).
Ellims, A. H. et al. Diffuse myocardial fibrosis evaluated by post-contrast T1 mapping correlates with left ventricular stiffness. J. Am. Coll. Cardiol. 63, 1112–1118 (2014).
Puntmann, V. O. et al. Native myocardial T1 mapping by cardiovascular magnetic resonance imaging in subclinical cardiomyopathy in patients with systemic lupus erythematosus. Circ. Cardiovasc. Imaging 6, 295–301 (2013).
Neilan, T. G. et al. Myocardial extracellular volume expansion and the risk of recurrent atrial fibrillation after pulmonary vein isolation. JACC Cardiovasc. Imaging 7, 1–11 (2014).
Kellman, P., Wilson, J., Xue, H., Ugander, M. & Arai, A. Extracellular volume fraction mapping in the myocardium, part 1: evaluation of an automated method. J. Cardiovasc. Magn. Reson. 14, 64 (2012).
Chan, W. et al. Acute left ventricular remodeling following myocardial infarction: coupling of regional healing with remote extracellular matrix expansion. JACC Cardiovasc. Imaging 5, 884–893 (2012).
Pop, M. et al. in Statistical Atlases and Computational Models of the Heart (eds Camara, O. et al.) 326–335 (Springer, 2013).
Wong, T. C. et al. Association between extracellular matrix expansion quantified by cardiovascular magnetic resonance and short-term mortality. Circulation 126, 1206–1216 (2012).
Beinart, R. et al. Cardiac magnetic resonance T1 mapping of left atrial myocardium. Heart Rhythm 10, 1325–1331 (2013).
Kawel-Boehm, N. et al. In-vivo assessment of normal T1 values of the right-ventricular myocardium by cardiac MRI. Int. J. Cardiovasc. Imaging 30, 323–328 (2014).
Rehwald, W. G., Fieno, D. S., Chen, E.-L., Kim, R. J. & Judd, R. M. Myocardial magnetic resonance imaging contrast agent concentrations after reversible and irreversible ischemic injury. Circulation 105, 224–229 (2002).
Saeed, M., Higgins, C. B., Geschwind, J. F. & Wendland, M. F. T1-relaxation kinetics of extracellular, intracellular and intravascular MR contrast agents in normal and acutely reperfused infarcted myocardium using echo-planar MR imaging. Eur. Radiol. 10, 310–318 (2000).
Author information
Authors and Affiliations
Contributions
Both authors researched data for the article, contributed substantially to discussion of its content, wrote the manuscript, and reviewed and edited it before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Table 1
Studies demonstrating prognostic implications of LGE and T1 mapping (DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Ambale-Venkatesh, B., Lima, J. Cardiac MRI: a central prognostic tool in myocardial fibrosis. Nat Rev Cardiol 12, 18–29 (2015). https://doi.org/10.1038/nrcardio.2014.159
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2014.159
This article is cited by
-
Non-invasive left ventricular pressure-strain loop study on cardiac fibrosis in primary aldosteronism: a comparative study with cardiac magnetic resonance imaging
Hypertension Research (2024)
-
Präzisionsmedizin vertieft die personalisierte Medizin in der Kardiologie
Die Innere Medizin (2024)
-
Is myocardial fibrosis appropriately assessed by calibrated and 2D strain derived integrated backscatter?
Cardiovascular Ultrasound (2023)
-
Potential of non-contrast stress T1 mapping for the assessment of myocardial injury in hypertrophic cardiomyopathy
Journal of Cardiovascular Magnetic Resonance (2023)
-
Functional significance of myocardial activity at 18F-FAPI PET/CT in hypertrophic cardiomyopathy identified by cardiac magnetic resonance feature-tracking strain analysis
European Journal of Nuclear Medicine and Molecular Imaging (2023)