Abstract
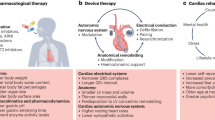
Men and women with heart failure display important differences in clinical characteristics that might affect their responses to pharmacological and nonpharmacological therapies. In women, heart failure is associated with a higher frequency of hypertension, nonischemic cardiomyopathy and left bundle branch block than in men. Subgroup analyses of data from randomized clinical trials suggest that these differences result in a differential response to heart failure therapies, including a somewhat better response to β-blockers, a worse prognosis with digoxin therapy, and a lower survival benefit with implantable cardioverter-defibrillators in women. Importantly, female patients with heart failure also derive significantly greater improvements in cardiac volumes from cardiac resynchronization therapy than do male patients, and this treatment is associated with reduced risks of all-cause mortality and heart failure events among women with mild symptoms. These data suggest that sex-related differences might exist in response to both medical and device therapies for patients with heart failure.
Key Points
-
Women with heart failure demonstrate important differences in clinical characteristics compared with men, including a higher frequency of hypertension, nonischemic etiologies of cardiomyopathy, and left bundle branch block
-
Sex-related differences in clinical characteristics could result in differential responses to medical and device therapies; however, current data are limited to retrospective subgroup analyses in small numbers of women
-
Women with heart failure respond better to β-blockers, but have a worse prognosis with digoxin, than men; angiotensin-converting-enzyme inhibitors and angiotensin-receptor blockers are equally effective in both sexes
-
Implantable cardioverter-defibrillator therapy might be associated with a lower survival benefit in women than in men with heart failure
-
Women demonstrate a significantly more favorable echocardiographic response to cardiac resynchronization therapy than men, regardless of their heart failure functional class
-
In women with mild heart failure, cardiac resynchronization therapy results in pronounced reductions in all-cause mortality and heart failure events that are significantly greater than the corresponding reductions in men
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Roger, V. L. et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 123, e18–e209 (2011).
Dickstein, K. et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur. Heart J. 29, 2388–2442 (2008).
Roger, V. L. et al. Trends in heart failure incidence and survival in a community-based population. JAMA 292, 344–350 (2004).
Levy, D. et al. Long-term trends in the incidence of and survival with heart failure. N. Engl. J. Med. 347, 1397–1402 (2002).
Barsheshet, A. et al. Effect of bundle branch block patterns on mortality in hospitalized patients with heart failure. Am. J. Cardiol. 101, 1303–1308 (2008).
Redfield, M. M. et al. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 289, 194–202 (2003).
Levy, D., Larson, M. G., Vasan, R. S., Kannel, W. B. & Ho, K. K. The progression from hypertension to congestive heart failure. JAMA 275, 1557–1562 (1996).
Adams, K. F. Jr. et al. Gender differences in survival in advanced heart failure. Insights from the FIRST study. Circulation 99, 1816–1821 (1999).
Ghali, J. K., Pina, I. L., Gottlieb, S. S., Deedwania, P. C. & Wikstrand, J. C. Metoprolol CR/XL in female patients with heart failure: analysis of the experience in Metoprolol Extended-Release Randomized Intervention Trial in Heart Failure (MERIT-HF). Circulation 105, 1585–1591 (2002).
De Maria, R. et al. Comparison of clinical findings in idiopathic dilated cardiomyopathy in women versus men. The Italian Multicenter Cardiomyopathy Study Group (SPIC). Am. J. Cardiol. 72, 580–585 (1993).
Simon, T., Mary-Krause, M., Funck-Brentano, C. & Jaillon, P. Sex differences in the prognosis of congestive heart failure: results from the Cardiac Insufficiency Bisoprolol Study (CIBIS II). Circulation 103, 375–380 (2001).
Ghali, J. K. et al. Gender differences in advanced heart failure: insights from the BEST study. J. Am. Coll. Cardiol. 42, 2128–2134 (2003).
Adams, K. F. Jr. et al. Relation between gender, etiology and survival in patients with symptomatic heart failure. J. Am. Coll. Cardiol. 28, 1781–1788 (1996).
Lund, L. H. & Mancini, D. Heart failure in women. Med. Clin. North Am. 88, 1321–1345 (2004).
Hsich, E. M. & Pina, I. L. Heart failure in women: a need for prospective data. J. Am. Coll. Cardiol. 54, 491–498 (2009).
Konhilas, J. P. & Leinwand, L. A. The effects of biological sex and diet on the development of heart failure. Circulation 116, 2747–2759 (2007).
Jain, M. et al. Influence of gender on the response to hemodynamic overload after myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 283, H2544–H2550 (2002).
Cavasin, M. A., Tao, Z., Menon, S. & Yang, X. P. Gender differences in cardiac function during early remodeling after acute myocardial infarction in mice. Life Sci. 75, 2181–2192 (2004).
Follath, F., Cleland, J. G., Klein, W. & Murphy, R. Etiology and response to drug treatment in heart failure. J. Am. Coll. Cardiol. 32, 1167–1172 (1998).
Andersson, B. & Waagstein, F. Spectrum and outcome of congestive heart failure in a hospitalized population. Am. Heart J. 126, 632–640 (1993).
Bart, B. A. et al. Clinical determinants of mortality in patients with angiographically diagnosed ischemic or nonischemic cardiomyopathy. J. Am. Coll. Cardiol. 30, 1002–1008 (1997).
Felker, G. M., Shaw, L. K. & O'Connor, C. M. A standardized definition of ischemic cardiomyopathy for use in clinical research. J. Am. Coll. Cardiol. 39, 210–218 (2002).
Barsheshet, A. et al. Response to preventive cardiac resynchronization therapy in patients with ischaemic and nonischaemic cardiomyopathy in MADIT-CRT. Eur. Heart J. 32, 1622–1630 (2011).
Vasan, R. S. et al. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J. Am. Coll. Cardiol. 33, 1948–1955 (1999).
Masoudi, F. A. et al. Gender, age, and heart failure with preserved left ventricular systolic function. J. Am. Coll. Cardiol. 41, 217–223 (2003).
Gilligan, D. M., Badar, D. M., Panza, J. A., Quyyumi, A. A. & Cannon, R. O. 3rd. Acute vascular effects of estrogen in postmenopausal women. Circulation 90, 786–791 (1994).
Ylikorkala, O., Orpana, A., Puolakka, J., Pyorala, T. & Viinikka, L. Postmenopausal hormonal replacement decreases plasma levels of endothelin-1. J. Clin. Endocrinol. Metab. 80, 3384–3387 (1995).
Saitta, A. et al. Randomized, double-blind, placebo-controlled study on effects of raloxifene and hormone replacement therapy on plasma no concentrations, endothelin-1 levels, and endothelium-dependent vasodilation in postmenopausal women. Arterioscler. Thromb. Vasc. Biol. 21, 1512–1519 (2001).
Landahl, S., Bengtsson, C., Sigurdsson, J. A., Svanborg, A. & Svärdsudd, K. Age-related changes in blood pressure. Hypertension 8, 1044–1049 (1986).
Gebara, O. C. et al. Association between increased estrogen status and increased fibrinolytic potential in the Framingham Offspring Study. Circulation 91, 1952–1958 (1995).
Packer, M. et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U. S. Carvedilol Heart Failure Study Group. N. Engl. J. Med. 334, 1349–1355 (1996).
Packer, M. et al. Effect of carvedilol on survival in severe chronic heart failure. N. Engl. J. Med. 344, 1651–1658 (2001).
Hunt, S. A. et al. 2009 Focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration with the International Society for Heart and Lung Transplantation. J. Am. Coll. Cardiol. 53, e1–e90 (2009).
[No authors listed] Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N. Engl. J. Med. 316, 1429–1435 (1987).
Garg, R. & Yusuf, S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA 273, 1450–1456 (1995).
Shekelle, P. G. et al. Efficacy of angiotensin-converting enzyme inhibitors and β-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J. Am. Coll. Cardiol. 41, 1529–1538 (2003).
Young, J. B. et al. Mortality and morbidity reduction with candesartan in patients with chronic heart failure and left ventricular systolic dysfunction: results of the CHARM low-left ventricular ejection fraction trials. Circulation 110, 2618–2626 (2004).
Cohn, J. N. & Tognoni, G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N. Engl. J. Med. 345, 1667–1675 (2001).
Pitt, B. et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N. Engl. J. Med. 341, 709–717 (1999).
Pitt, B. et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N. Engl. J. Med. 348, 1309–1321 (2003).
Zannad, F. et al. Eplerenone in patients with systolic heart failure and mild symptoms. N. Engl. J. Med. 364, 11–21 (2011).
The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N. Engl. J. Med. 336, 525–533 (1997).
Rathore, S. S., Wang, Y. & Krumholz, H. M. Sex-based differences in the effect of digoxin for the treatment of heart failure. N. Engl. J. Med. 347, 1403–1411 (2002).
Moss, A. J. et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N. Engl. J. Med. 335, 1933–1940 (1996).
Buxton, A. E. et al. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N. Engl. J. Med. 341, 1882–1890 (1999).
Moss, A. J. et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N. Engl. J. Med. 346, 877–883 (2002).
Kadish, A. et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N. Engl. J. Med. 350, 2151–2158 (2004).
Bardy, G. H. et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. Engl. J. Med. 352, 225–237 (2005).
Zareba, W. et al. Clinical course and implantable cardioverter defibrillator therapy in postinfarction women with severe left ventricular dysfunction. J. Cardiovasc. Electrophysiol. 16, 1265–1270 (2005).
Ghanbari, H. et al. Effectiveness of implantable cardioverter-defibrillators for the primary prevention of sudden cardiac death in women with advanced heart failure: a meta-analysis of randomized controlled trials. Arch. Intern. Med. 169, 1500–1506 (2009).
Santangeli, P. et al. Gender differences in clinical outcome and primary prevention defibrillator benefit in patients with severe left ventricular dysfunction: a systematic review and meta-analysis. Heart Rhythm 7, 876–882 (2010).
Bristow, M. R. et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N. Engl. J. Med. 350, 2140–2150 (2004).
Cleland, J. G. et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 352, 1539–1549 (2005).
Chung, E. S. et al. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation 117, 2608–2616 (2008).
Moss, A. J. et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 361, 1329–1338 (2009).
St. John Sutton, M. et al. Cardiac resynchronization induces major structural and functional reverse remodeling in patients with New York Heart Association class I/II heart failure. Circulation 120, 1858–1865 (2009).
Tang, A. S. et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N. Engl. J. Med. 363, 2385–2395 (2010).
Arshad, A. et al. Cardiac resynchronization therapy is more effective in women than in men: the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy) trial. J. Am. Coll. Cardiol. 57, 813–820 (2011).
Daubert, C. et al. Prevention of disease progression by cardiac resynchronization therapy in patients with asymptomatic or mildly symptomatic left ventricular dysfunction: insights from the European cohort of the REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction) trial. J. Am. Coll. Cardiol. 54, 1837–1846 (2009).
Adelstein, E. C. & Saba, S. Usefulness of baseline electrocardiographic QRS complex pattern to predict response to cardiac resynchronization. Am. J. Cardiol. 103, 238–242 (2009).
Zareba, W. et al. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation 123, 1061–1072 (2011).
Marsan, N. A. et al. Comparison of time course of response to cardiac resynchronization therapy in patients with ischemic versus nonischemic cardiomyopathy. Am. J. Cardiol. 103, 690–694 (2009).
Wikstrom, G. et al. The effects of aetiology on outcome in patients treated with cardiac resynchronization therapy in the CARE-HF trial. Eur. Heart J. 30, 782–788 (2009).
St. John Sutton, M. G. et al. Sustained reverse left ventricular structural remodeling with cardiac resynchronization at one year is a function of etiology: quantitative Doppler echocardiographic evidence from the Multicenter InSync Randomized Clinical Evaluation (MIRACLE). Circulation 113, 266–272 (2006).
Crow, R. S., Hannan, P. J. & Folsom, A. R. Prognostic significance of corrected QT and corrected JT interval for incident coronary heart disease in a general population sample stratified by presence or absence of wide QRS complex: the ARIC study with 13 years of follow-up. Circulation 108, 1985–1989 (2003).
Boudina, S. & Abel, E. D. Diabetic cardiomyopathy revisited. Circulation 115, 3213–3223 (2007).
Hunt, S. A. et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J. Am. Coll. Cardiol. 46, e1–e82 (2005).
Abraham, W. T. et al. Cardiac resynchronization in chronic heart failure. N. Engl. J. Med. 346, 1845–1853 (2002).
Acknowledgements
A. Barsheshet's research is partly supported by funding from the Mirowski–Moss Career Development Award. I. Goldenberg's research is partly supported by the Mirowski Family Foundation.
Author information
Authors and Affiliations
Contributions
All four authors researched the data for the article and provided substantial contributions to discussions of its content. A. Barsheshet and A. Brenyo wrote the initial draft of the article, and I. Goldenberg and A. J. Moss developed the initial outline and revised the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
A. J. Moss declares that he has received grant or research support from Boston Scientific. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Barsheshet, A., Brenyo, A., Goldenberg, I. et al. Sex-related differences in patients' responses to heart failure therapy. Nat Rev Cardiol 9, 234–242 (2012). https://doi.org/10.1038/nrcardio.2012.10
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2012.10
This article is cited by
-
The spectrum of comorbidities at the initial diagnosis of heart failure a case control study
Scientific Reports (2022)
-
ADRB2 polymorphism Arg16Gly modifies the natural outcome of heart failure and dictates therapeutic response to β-blockers in patients with heart failure
Cell Discovery (2018)
-
Ageing-related cardiomyocyte functional decline is sex and angiotensin II dependent
AGE (2014)
-
Genetic Prediction of Heart Failure Incidence, Prognosis and Beta-blocker Response
Molecular Diagnosis & Therapy (2013)