Key Points
-
There has been a dramatic increase in the incidence of oesophageal adenocarcinoma (OAC) and intestinal-type gastric cancer (GC) arising near the gastric–oesophageal junction (GOJ).
-
OAC and intestinal-type GC share many common molecular features.
-
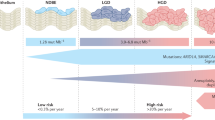
OAC and intestinal-type GC are derived from the inflammation–metaplasia cascade that occurs in the oesophageal epithelium in OAC and in the gastric epithelium in intestinal-type GC.
-
Barrett oesophagus and OAC may originate from gastric stem cells derived from the cardia.
Abstract
Over recent decades we have witnessed a shift in the anatomical distribution of gastric cancer (GC), which increasingly originates from the proximal stomach near the junction with the oesophagus. In parallel, there has been a dramatic rise in the incidence of oesophageal adenocarcinoma (OAC) in the lower oesophagus, which is associated with antecedent Barrett oesophagus (BO). In this context, there has been uncertainty regarding the characterization of adenocarcinomas spanning the area from the lower oesophagus to the distal stomach. Most relevant to this discussion is the distinction, if any, between OAC and intestinal-type GC of the proximal stomach. It is therefore timely to review our current understanding of OAC and intestinal-type GC, integrating advances from cell-of-origin studies and comprehensive genomic alteration analyses, ultimately enabling better insight into the relationship between these two cancers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Wingo, P. A. et al. Long-term trends in cancer mortality in the United States, 1930–1998. Cancer 97, 3133–3275 (2003).
Lauren, P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol. Microbiol. Scand. 64, 31–49 (1965).
Umar, S. B. & Fleischer, S. D. Esophageal cancer: epidemiology, pathogenesis and prevention. Nat. Rev. Gastroenterol. Hepatol. 5, 517–526 (2008).
Brown, L. M., Devesa, S. S. & Chow, W. H. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J. Natl Cancer Inst. 100, 1184–1187 (2008).
Demeester, S. R. Epidemiology and biology of esophageal cancer. Gastrointest. Cancer Res. 3, S2–S5 (2009).
Rustgi, A. K. & El-Serag, H. B. Esophageal carcinoma. N. Engl. J. Med. 371, 2499–2509 (2014).
Barrett, N. R. Chronic peptic ulcer of the oesophagus and 'oesophagitis'. Br. J. Surg. 38, 175–182 (1950).
Falk, G. W. et al. Barrett's esophagus: prevalence–incidence and etiology–origins. Ann. NY Acad. Sci. 1232, 1–17 (2011).
Devesa, S. S. & Fraumeni, J. F. Jr. The rising incidence of gastric cardia cancer. J. Natl Cancer Inst. 91, 747–749 (1999).
Deans, C. et al. Cancer of the gastric cardia is rising in incidence in an Asian population and is associated with adverse outcome. World J. Surg. 35, 617–624 (2011).
Sons, H. U. & Borchard, F. Cancer of the distal esophagus and cardia. Incidence, tumorous infiltration, and metastatic spread. Ann. Surg. 203, 188–195 (1986).
Blot, W. J., Devesa, S. S., Kneller, R. W. & Fraumeni, J. F. Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 265, 1287–1289 (1991).
Correa, P., Haenszel, W., Cuello, C., Tannenbaum, S. & Archer, M. A model for gastric cancer epidemiology. Lancet 2, 58–60 (1975).
Marshall, B. J. & Warren, J. R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet 1, 1311–1315 (1984).
Bertuccio, P. et al. Recent patterns in gastric cancer: a global overview. Int. J. Cancer 125, 666–673 (2009).
Wadhwa, R. et al. Gastric cancer-molecular and clinical dimensions. Nat. Rev. Clin. Oncol. 10, 643–655 (2013).
Bosetti, C. et al. Trends in cancer mortality in the Americas, 1970–2000. Ann. Oncol. 16, 489–511 (2005).
Lavery, D. L. et al. The stem cell organisation, and the proliferative and gene expression profile of Barrett's epithelium, replicates pyloric-type gastric glands. Gut 63, 1854–1863 (2014). Using detailed histopathological techniques, the authors reported the similarity between BO glands and gastric glands.
Mesquita, P. et al. Metaplasia—a transdifferentiation process that facilitates cancer development: the model of gastric intestinal metaplasia. Crit. Rev. Oncog. 12, 3–26 (2006).
Paull, A. et al. The histologic spectrum of Barrett's esophagus. N. Engl. J. Med. 295, 476–480 (1976).
Mutoh, H. et al. Cdx1 induced intestinal metaplasia in the transgenic mouse stomach: comparative study with Cdx2 transgenic mice. Gut 53, 1416–1423 (2004).
Silberg, D. G. et al. CDX1 protein expression in normal, metaplastic, and neoplastic human alimentary tract epithelium. Gastroenterology 113, 478–486 (1997).
Vallbohmer, D. et al. Cdx-2 expression in squamous and metaplastic columnar epithelia of the esophagus. Dis. Esophagus 19, 260–266 (2006).
Wong, N. A. et al. CDX1 is an important molecular mediator of Barrett's metaplasia. Proc. Natl Acad. Sci. USA 102, 7565–7570 (2005).
Parsonnet, J. et al. Helicobacter pylori infection and the risk of gastric carcinoma. N. Engl. J. Med. 325, 1127–1131 (1991).
Huang, J. Q., Sridhar, S., Chen, Y. & Hunt, R. H. Meta-analysis of the relationship between Helicobacter pylori seropositivity and gastric cancer. Gastroenterology 114, 1169–1179 (1998).
Helicobacter and Cancer Collaborative Group. Gastric cancer and Helicobacter pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut 49, 347–353 (2001).
Carneiro, F. et al. Model of the early development of diffuse gastric cancer in E-cadherin mutation carriers and its implications for patient screening. J. Pathol. 203, 681–687 (2004).
Blaser, M. J. Hypothesis: the changing relationships of Helicobacter pylori and humans: implications for health and disease. J. Infect. Dis. 179, 1523–1530 (1999).
Hansen, S., Melby, K. K., Aase, S., Jellum, E. & Vollset, S. E. Helicobacter pylori infection and risk of cardia cancer and non-cardia gastric cancer. A nested case-control study. Scand. J. Gastroenterol. 34, 353–360 (1999).
Chow, W. H. et al. An inverse relation between cagA+ strains of Helicobacter pylori infection and risk of esophageal and gastric cardia adenocarcinoma. Cancer Res. 58, 588–590 (1998).
Wu, I. C. et al. Association between Helicobacter pylori seropositivity and digestive tract cancers. World J. Gastroenterol. 15, 5465–5471 (2009).
Bornschein, J. et al. H. pylori infection is a key risk factor for proximal gastric cancer. Dig. Dis. Sci. 55, 3124–3131 (2010).
Morales, T. G., Sampliner, R. E. & Bhattacharyya, A. Intestinal metaplasia of the gastric cardia. Am. J. Gastroenterol. 92, 414–418 (1997).
Hackelsberger, A. et al. Prevalence and pattern of Helicobacter pylori gastritis in the gastric cardia. Am. J. Gastroenterol. 92, 2220–2224 (1997).
Goldblum, J. R. et al. Inflammation and intestinal metaplasia of the gastric cardia: the role of gastroesophageal reflux and H. pylori infection. Gastroenterology 114, 633–639 (1998).
Morini, S. et al. Gastric cardia inflammation: role of Helicobacter pylori infection and symptoms of gastroesophageal reflux disease. Am. J. Gastroenterol. 96, 2337–2340 (2001).
Quante, M. et al. Bile acid and inflammation activate gastric cardia stem cells in a mouse model of Barrett-like metaplasia. Cancer Cell 21, 36–51 (2012). In this work the authors developed a mouse model of BO, and demonstrated that BO is derived from gastric cardia stem cells.
Merry, A. H., Schouten, L. J., Goldbohm, R. A. & van den Brandt, P. A. Body mass index, height and risk of adenocarcinoma of the oesophagus and gastric cardia: a prospective cohort study. Gut 56, 1503–1511 (2007).
Lagergren, J., Bergstrom, R. & Nyren, O. Association between body mass and adenocarcinoma of the esophagus and gastric cardia. Ann. Intern. Med. 130, 883–890 (1999).
Hampel, H., Abraham, N. S. & El-Serag, H. B. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann. Intern. Med. 143, 199–211 (2005).
Thrift, A. P. et al. Obesity and risk of esophageal adenocarcinoma and Barrett's esophagus: a Mendelian randomization study. J. Natl Cancer Inst. 106, dju252 (2014).
Kendall, B. J. et al. The risk of Barrett's esophagus associated with abdominal obesity in males and females. Int. J. Cancer 132, 2192–2199 (2013).
Yang, P. et al. Overweight, obesity and gastric cancer risk: results from a meta-analysis of cohort studies. Eur. J. Cancer 45, 2867–2873 (2009).
Lin, X. J. et al. Body mass index and risk of gastric cancer: a meta-analysis. Jpn J. Clin. Oncol. 44, 783–791 (2014).
Chen, Y. et al. Body mass index and risk of gastric cancer: a meta-analysis of a population with more than ten million from 24 prospective studies. Cancer Epidemiol. Biomarkers Prev. 22, 1395–1408 (2013).
Ericksen, R. E. et al. Obesity accelerates Helicobacter felis-induced gastric carcinogenesis by enhancing immature myeloid cell trafficking and TH17 response. Gut 63, 385–394 (2014).
Chandar, A. K. et al. Association of serum levels of adipokines and insulin with risk of Barrett's esophagus: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 13, 2241–2255 (2015).
El-Omar, E. M. et al. The role of interleukin-1 polymorphisms in the pathogenesis of gastric cancer. Nature 412, 99 (2001).
El-Omar, E. M. et al. Increased risk of noncardia gastric cancer associated with proinflammatory cytokine gene polymorphisms. Gastroenterology 124, 1193–1201 (2003).
Persson, C., Canedo, P., Machado, J. C., El-Omar, E. M. & Forman, D. Polymorphisms in inflammatory response genes and their association with gastric cancer: a HuGE systematic review and meta-analyses. Am. J. Epidemiol. 173, 259–270 (2011).
Furuta, T. et al. Interleukin 1β polymorphisms increase risk of hypochlorhydria and atrophic gastritis and reduce risk of duodenal ulcer recurrence in Japan. Gastroenterology 123, 92–105 (2002).
Tu, S. et al. Overexpression of interleukin-1β induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell 14, 408–419 (2008).
Levine, D. M. et al. A genome-wide association study identifies new susceptibility loci for esophageal adenocarcinoma and Barrett's esophagus. Nat. Genet. 45, 1487–1493 (2013).
Palles, C. et al. Polymorphisms near TBX5 and GDF7 are associated with increased risk for Barrett's esophagus. Gastroenterology 148, 367–378 (2015).
Shibata, W. et al. Stromal cell-derived factor-1 overexpression induces gastric dysplasia through expansion of stromal myofibroblasts and epithelial progenitors. Gut 62, 192–200 (2013).
Okumura, T. et al. K-ras mutation targeted to gastric tissue progenitor cells results in chronic inflammation, an altered microenvironment, and progression to intraepithelial neoplasia. Cancer Res. 70, 8435–8445 (2010).
Hayakawa, Y. et al. Mist1 expressing gastric stem cells maintain the normal and neoplastic gastric epithelium and are supported by a perivascular stem cell niche. Cancer Cell 28, 800–814 (2015). This study revealed that gastric isthmus stem cells in the corpus can give rise to intestinal-type and diffuse-type cancers.
Zhao, C. M. et al. Denervation suppresses gastric tumorigenesis. Sci. Transl Med. 6, 250ra115 (2014).
Quante, M. et al. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell 19, 257–272 (2011).
Poulsen, A. H. et al. Proton pump inhibitors and risk of gastric cancer: a population-based cohort study. Br. J. Cancer 100, 1503–1507 (2009).
Ahn, J. S., Eom, C. S., Jeon, C. Y. & Park, S. M. Acid suppressive drugs and gastric cancer: a meta-analysis of observational studies. World J. Gastroenterol. 19, 2560–2568 (2013).
Malesci, A. et al. Partial regression of Barrett's esophagus by long-term therapy with high-dose omeprazole. Gastrointest. Endosc. 44, 700–705 (1996).
Gore, S. et al. Regression of columnar lined (Barrett's) oesophagus with continuous omeprazole therapy. Aliment. Pharmacol. Ther. 7, 623–628 (1993).
Peters, F. T. et al. Endoscopic regression of Barrett's oesophagus during omeprazole treatment; a randomised double blind study. Gut 45, 489–494 (1999).
Hvid-Jensen, F., Pedersen, L., Funch-Jensen, P. & Drewes, A. M. Proton pump inhibitor use may not prevent high-grade dysplasia and oesophageal adenocarcinoma in Barrett's oesophagus: a nationwide study of 9883 patients. Aliment. Pharmacol. Ther. 39, 984–991 (2014).
Singh, S., Garg, S. K., Singh, P. P., Iyer, P. G. & El-Serag, H. B. Acid-suppressive medications and risk of oesophageal adenocarcinoma in patients with Barrett's oesophagus: a systematic review and meta-analysis. Gut 63, 1229–1237 (2014).
Obszynska, J. A. et al. Long-term proton pump induced hypergastrinaemia does induce lineage-specific restitution but not clonal expansion in benign Barrett's oesophagus in vivo. Gut 59, 156–163 (2010).
Lundell, L., Vieth, M., Gibson, F., Nagy, P. & Kahrilas, P. J. Systematic review: the effects of long-term proton pump inhibitor use on serum gastrin levels and gastric histology. Aliment. Pharmacol. Ther. 42, 649–663 (2015).
Haigh, C. R. et al. Gastrin induces proliferation in Barrett's metaplasia through activation of the CCK2 receptor. Gastroenterology 124, 615–625 (2003).
Hoffmann, K. M., Gibril, F., Entsuah, L. K., Serrano, J. & Jensen, R. T. Patients with multiple endocrine neoplasia type 1 with gastrinomas have an increased risk of severe esophageal disease including stricture and the premalignant condition, Barrett's esophagus. J. Clin. Endocrinol. Metab. 91, 204–212 (2006).
Wang, J. S. et al. Elevated serum gastrin is associated with a history of advanced neoplasia in Barrett's esophagus. Am. J. Gastroenterol. 105, 1039–1045 (2010).
Green, D. A. et al. Correlation between serum gastrin and cellular proliferation in Barrett's esophagus. Therap. Adv. Gastroenterol. 4, 89–94 (2011).
Zavros, Y. et al. Chronic gastritis in the hypochlorhydric gastrin-deficient mouse progresses to adenocarcinoma. Oncogene 24, 2354–2366 (2005).
Tomita, H. et al. Inhibition of gastric carcinogenesis by the hormone gastrin is mediated by suppression of TFF1 epigenetic silencing. Gastroenterology 140, 879–891 (2011).
Sharma, P. et al. A critical review of the diagnosis and management of Barrett's esophagus: the AGA Chicago Workshop. Gastroenterology 127, 310–330 (2004).
Robertson, E. V. et al. Central obesity in asymptomatic volunteers is associated with increased intrasphincteric acid reflux and lengthening of the cardiac mucosa. Gastroenterology 145, 730–739 (2013).
Cassaro, M. et al. Topographic patterns of intestinal metaplasia and gastric cancer. Am. J. Gastroenterol. 95, 1431–1438 (2000).
Chandrasoma, P. T., Der, R., Ma, Y., Dalton, P. & Taira, M. Histology of the gastroesophageal junction: an autopsy study. Am. J. Surg. Pathol. 24, 402–409 (2000).
Genta, R. M., Huberman, R. M. & Graham, D. Y. The gastric cardia in Helicobacter pylori infection. Hum. Pathol. 25, 915–919 (1994).
Chandrasoma, P. T. et al. Distribution and significance of epithelial types in columnar-lined esophagus. Am. J. Surg. Pathol. 25, 1188–1193 (2001).
McDonald, S. A. et al. Mechanisms of field cancerization in the human stomach: the expansion and spread of mutated gastric stem cells. Gastroenterology 134, 500–510 (2008).
Leedham, S. J. et al. Individual crypt genetic heterogeneity and the origin of metaplastic glandular epithelium in human Barrett's oesophagus. Gut 57, 1041–1048 (2008).
Maley, C. C. et al. Selectively advantageous mutations and hitchhikers in neoplasms: 16 lesions are selected in Barrett's esophagus. Cancer Res. 64, 3414–3427 (2004).
Nicholson, A. M. et al. Barrett's metaplasia glands are clonal, contain multiple stem cells and share a common squamous progenitor. Gut 61, 1380–1389 (2012). With the use of human tissue, the authors reported that BO glands expand clonally and multiple clones from multiple stem cells are involved in BO lesions.
Paulson, T. G. et al. Neosquamous epithelium does not typically arise from Barrett's epithelium. Clin. Cancer Res. 12, 1701–1706 (2006).
Nam, K. T. et al. Mature chief cells are cryptic progenitors for metaplasia in the stomach. Gastroenterology 139, 2028–2037 (2010).
Schwitalla, S. et al. Intestinal tumorigenesis initiated by dedifferentiation and acquisition of stem-cell-like properties. Cell 152, 25–38 (2013).
Westphalen, C. B. et al. Long-lived intestinal tuft cells serve as colon cancer-initiating cells. J. Clin. Invest. 124, 1283–1295 (2014).
Sangiorgi, E. & Capecchi, M. R. Bmi1 is expressed in vivo in intestinal stem cells. Nat. Genet. 40, 915–920 (2008).
Barker, N. et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature 457, 608–611 (2009). In this work, the authors demonstrated that LGR5+ intestinal and colon stem cells are an origin of intestinal cancers in mice.
Asfaha, S. et al. Krt19+/Lgr5− cells are radioresistant cancer-initiating stem cells in the colon and intestine. Cell Stem Cell 16, 627–638 (2015).
Barker, N. et al. Lgr5(+ve) stem cells drive self-renewal in the stomach and build long-lived gastric units in vitro. Cell Stem Cell 6, 25–36 (2010). This study identified LGR5+ gastric stem cells at the base of antral and cardia glands in mice, and showed that they give rise to neoplasia.
Mills, J. C. & Shivdasani, R. A. Gastric epithelial stem cells. Gastroenterology 140, 412–424 (2011).
Goldenring, J. R., Nam, K. T., Wang, T. C., Mills, J. C. & Wright, N. A. Spasmolytic polypeptide-expressing metaplasia and intestinal metaplasia: time for reevaluation of metaplasias and the origins of gastric cancer. Gastroenterology 138, 2207–2210 (2010).
Barker, N. et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 449, 1003–1007 (2007).
Arnold, K. et al. Sox2+ adult stem and progenitor cells are important for tissue regeneration and survival of mice. Cell Stem Cell 9, 317–329 (2011).
Powell, A. E. et al. The pan-ErbB negative regulator Lrig1 is an intestinal stem cell marker that functions as a tumor suppressor. Cell 149, 146–158 (2012).
Hayakawa, Y. et al. CCK2R identifies and regulates gastric antral stem cell states and carcinogenesis. Gut 64, 544–553 (2014). This study identified CCKBR+ stem cells in mouse gastric antrum, and described progastrin-mediated interconversion between CCKBR+ and LGR5+ stem cells.
Yan, K. S. et al. The intestinal stem cell markers Bmi1 and Lgr5 identify two functionally distinct populations. Proc. Natl Acad. Sci. USA 109, 466–471 (2012).
Tian, H. et al. A reserve stem cell population in small intestine renders Lgr5-positive cells dispensable. Nature 478, 255–259 (2011).
Li, L. & Clevers, H. Coexistence of quiescent and active adult stem cells in mammals. Science 327, 542–545 (2010).
Karam, S. M. & Leblond, C. P. Dynamics of epithelial cells in the corpus of the mouse stomach. I. Identification of proliferative cell types and pinpointing of the stem cell. Anat. Rec. 236, 259–279 (1993).
Lee, E. R. & Leblond, C. P. Dynamic histology of the antral epithelium in the mouse stomach: II. Ultrastructure and renewal of isthmal cells. Am. J. Anat. 172, 205–224 (1985).
Nam, K. T. et al. Spasmolytic polypeptide-expressing metaplasia (SPEM) in the gastric oxyntic mucosa does not arise from Lgr5-expressing cells. Gut 61, 1678–1685 (2012).
Stange, D. E. et al. Differentiated troy+ chief cells act as reserve stem cells to generate all lineages of the stomach epithelium. Cell 155, 357–368 (2013).
Choi, E., Hendley, A. M., Bailey, J. M., Leach, S. D. & Goldenring, J. R. Expression of activated Ras in gastric chief cells of mice leads to the full spectrum of metaplastic lineage transitions. Gastroenterology 150, 918–930 (2016).
Leushacke, M., Ng, A., Galle, J., Loeffler, M. & Barker, N. Lgr5+ gastric stem cells divide symmetrically to effect epithelial homeostasis in the pylorus. Cell Rep. 5, 349–356 (2013).
Jang, B. G., Lee, B. L. & Kim, W. H. Distribution of LGR5+ cells and associated implications during the early stage of gastric tumorigenesis. PLoS ONE 8, e82390 (2013).
Simon, E. et al. The spatial distribution of LGR5+ cells correlates with gastric cancer progression. PLoS ONE 7, e35486 (2012).
Becker, L., Huang, Q. & Mashimo, H. Immunostaining of Lgr5, an intestinal stem cell marker, in normal and premalignant human gastrointestinal tissue. Sci. World J. 8, 1168–1176 (2008).
Sigal, M. et al. Helicobacter pylori activates and expands Lgr5+ stem cells through direct colonization of the gastric glands. Gastroenterology 148, 1392–1404 (2015).
Schmitz, F. et al. Cellular expression of CCK-A and CCK-B/gastrin receptors in human gastric mucosa. Regul. Pept. 102, 101–110 (2001).
Goetze, J. P. et al. Characterization of gastrins and their receptor in solid human gastric adenocarcinomas. Scand. J. Gastroenterol. 48, 688–695 (2013).
Takamura, A. et al. High expression of gastrin receptor protein in injured mucosa of Helicobacter pylori-positive gastritis. Dig. Dis. Sci. 58, 634–640 (2013).
Souza, R. F., Krishnan, K. & Spechler, S. J. Acid, bile, and CDX: the ABCs of making Barrett's metaplasia. Am. J. Physiol. Gastrointest. Liver Physiol. 295, G211–G218 (2008).
Kaz, A. M., Grady, W. M., Stachler, M. D. & Bass, A. J. Genetic and epigenetic alterations in Barrett's esophagus and esophageal adenocarcinoma. Gastroenterol. Clin. North Am. 44, 473–489 (2015).
Srivastava, A. et al. High goblet cell count is inversely associated with ploidy abnormalities and risk of adenocarcinoma in Barrett's esophagus. PLoS ONE 10, e0133403 (2015).
Lavery, D. L. et al. Evolution of oesophageal adenocarcinoma from metaplastic columnar epithelium without goblet cells in Barrett's oesophagus. Gut http://dx.doi.org/10.1136/gutjnl-2015-310748 (2015).
He, J., Fang, Y. & Chen, X. Surgical models of gastroesophageal reflux with mice. J. Vis. Exp. 102, e53012 (2015).
Becker, L., Huang, Q. & Mashimo, H. Lgr5, an intestinal stem cell marker, is abnormally expressed in Barrett's esophagus and esophageal adenocarcinoma. Dis. Esophagus 23, 168–174 (2010).
Harris, J. C., Clarke, P. A., Awan, A., Jankowski, J. & Watson, S. A. An antiapoptotic role for gastrin and the gastrin/CCK-2 receptor in Barrett's esophagus. Cancer Res. 64, 1915–1919 (2004).
Ahnen, D. J. et al. The ulceration-associated cell lineage (UACL) reiterates the Brunner's gland differentiation programme but acquires the proliferative organization of the gastric gland. J. Pathol. 173, 317–326 (1994).
Abdulnour-Nakhoul, S. et al. Characterization of esophageal submucosal glands in pig tissue and cultures. Dig. Dis. Sci. 52, 3054–3065 (2007).
Wang, X. et al. Residual embryonic cells as precursors of a Barrett's-like metaplasia. Cell 145, 1023–1035 (2011). This study showed KRT7+ residual embryonic cells to be a potent origin of BO in mouse and human.
Xian, W., Ho, K. Y., Crum, C. P. & McKeon, F. Cellular origin of Barrett's esophagus: controversy and therapeutic implications. Gastroenterology 142, 1424–1430 (2012).
Becker, K. F. et al. Identification of eleven novel tumor-associated E-cadherin mutations. Mutations in brief no. 215. Hum. Mutat. 13, 171 (1999).
Huntsman, D. G. et al. Early gastric cancer in young, asymptomatic carriers of germ-line E-cadherin mutations. N. Engl. J. Med. 344, 1904–1909 (2001).
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature 513, 202–209 (2014). These authors performed comprehensive analysis in GC samples including whole-genomic sequence, gene expression and methylation arrays, and SCNA analysis, and identified four molecular subtypes.
Cristescu, R. et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat. Med. 21, 449–456 (2015). These authors identified four molecular subtypes in GCs and showed their correlation with different prognoses.
Stachler, M. D. et al. Paired exome analysis of Barrett's esophagus and adenocarcinoma. Nat. Genet. 47, 1047–1055 (2015). These authors analysed whole-exome sequencing in paired BO and OAC samples, and showed that TP53 mutations occur early in disease progression whereas genome doubling is a later event.
Dulak, A. M. et al. Gastrointestinal adenocarcinomas of the esophagus, stomach, and colon exhibit distinct patterns of genome instability and oncogenesis. Cancer Res. 72, 4383–4393 (2012).
Dulak, A. M. et al. Exome and whole-genome sequencing of esophageal adenocarcinoma identifies recurrent driver events and mutational complexity. Nat. Genet. 45, 478–486 (2013). These authors performed exome and whole-genome sequencing of OAC samples, and identified several new gene mutation signatures.
Gu, J. et al. Genome-wide catalogue of chromosomal aberrations in Barrett's esophagus and esophageal adenocarcinoma: a high-density single nucleotide polymorphism array analysis. Cancer Prev. Res. (Phila) 3, 1176–1186 (2010).
Huang, Y. et al. Altered messenger RNA and unique mutational profiles of p53 and Rb in human esophageal carcinomas. Cancer Res. 53, 1889–1894 (1993).
Kimchi, E. T. et al. Progression of Barrett's metaplasia to adenocarcinoma is associated with the suppression of the transcriptional programs of epidermal differentiation. Cancer Res. 65, 3146–3154 (2005).
Miller, C. T. et al. Gene amplification in esophageal adenocarcinomas and Barrett's with high-grade dysplasia. Clin. Cancer Res. 9, 4819–4825 (2003).
Enlow, J. M., Denlinger, C. E., Stroud, M. R., Ralston, J. S. & Reed, C. E. Adenocarcinoma of the esophagus with signet ring cell features portends a poor prognosis. Ann. Thorac. Surg. 96, 1927–1932 (2013).
Nafteux, P. R. et al. Signet ring cells in esophageal and gastroesophageal junction carcinomas have a more aggressive biological behavior. Ann. Surg. 260, 1023–1029 (2014).
Kalish, R. J., Clancy, P. E., Orringer, M. B. & Appelman, H. D. Clinical, epidemiologic, and morphologic comparison between adenocarcinomas arising in Barrett's esophageal mucosa and in the gastric cardia. Gastroenterology 86, 461–467 (1984).
Reid, B. J. et al. Predictors of progression in Barrett's esophagus II: baseline 17p (p53) loss of heterozygosity identifies a patient subset at increased risk for neoplastic progression. Am. J. Gastroenterol. 96, 2839–2848 (2001).
Farris, A. B. et al. Clinicopathologic and molecular profiles of microsatellite unstable Barrett esophagus-associated adenocarcinoma. Am. J. Surg. Pathol. 35, 647–655 (2011).
Van Beek, J. et al. EBV-positive gastric adenocarcinomas: a distinct clinicopathologic entity with a low frequency of lymph node involvement. J. Clin. Oncol. 22, 664–670 (2004).
Beroukhim, R. et al. The landscape of somatic copy-number alteration across human cancers. Nature 463, 899–905 (2010).
Nancarrow, D. J. et al. Genome-wide copy number analysis in esophageal adenocarcinoma using high-density single-nucleotide polymorphism arrays. Cancer Res. 68, 4163–4172 (2008).
Deng, N. et al. A comprehensive survey of genomic alterations in gastric cancer reveals systematic patterns of molecular exclusivity and co-occurrence among distinct therapeutic targets. Gut 61, 673–684 (2012).
Chia, N. Y. et al. Regulatory crosstalk between lineage-survival oncogenes KLF5, GATA4 and GATA6 cooperatively promotes gastric cancer development. Gut 64, 707–719 (2015).
Garraway, L. A. & Sellers, W. R. Lineage dependency and lineage-survival oncogenes in human cancer. Nat. Rev. Cancer 6, 593–602 (2006).
Lin, L. et al. Activation of GATA binding protein 6 (GATA6) sustains oncogenic lineage-survival in esophageal adenocarcinoma. Proc. Natl Acad. Sci. USA 109, 4251–4256 (2012).
Sulahian, R. et al. An integrative analysis reveals functional targets of GATA6 transcriptional regulation in gastric cancer. Oncogene 33, 5637–5648 (2014).
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013).
Polak, P. et al. Cell-of-origin chromatin organization shapes the mutational landscape of cancer. Nature 518, 360–364 (2015).
Agrawal, N. et al. Comparative genomic analysis of esophageal adenocarcinoma and squamous cell carcinoma. Cancer Discov. 2, 899–905 (2012).
Weaver, J. M. et al. Ordering of mutations in preinvasive disease stages of esophageal carcinogenesis. Nat. Genet. 46, 837–843 (2014).
Barrett, M. T. et al. Molecular phenotype of spontaneously arising 4N (G2-tetraploid) intermediates of neoplastic progression in Barrett's esophagus. Cancer Res. 63, 4211–4217 (2003).
Chao, D. L. et al. Cell proliferation, cell cycle abnormalities, and cancer outcome in patients with Barrett's esophagus: a long-term prospective study. Clin. Cancer Res. 14, 6988–6995 (2008).
Ross-Innes, C. S. et al. Whole-genome sequencing provides new insights into the clonal architecture of Barrett's esophagus and esophageal adenocarcinoma. Nat. Genet. 47, 1038–1046 (2015). In this study, the authors performed whole-genome sequencing with paired BO and OAC samples, and revealed that BO is polyclonal, and highly mutated even in the absence of dysplasia.
Wang, K. et al. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat. Genet. 46, 573–582 (2014).
Guilford, P. et al. E-cadherin germline mutations in familial gastric cancer. Nature 392, 402–405 (1998).
Kakiuchi, M. et al. Recurrent gain-of-function mutations of RHOA in diffuse-type gastric carcinoma. Nat. Genet. 46, 583–587 (2014).
Li, X. et al. Temporal and spatial evolution of somatic chromosomal alterations: a case-cohort study of Barrett's esophagus. Cancer Prev. Res. (Phila) 7, 114–127 (2014).
Yamamoto, Y. et al. Mutational spectrum of Barrett's stem cells suggests paths to initiation of a precancerous lesion. Nat. Commun. 7, 10380 (2016).
Matsusaka, K. et al. Classification of Epstein–Barr virus-positive gastric cancers by definition of DNA methylation epigenotypes. Cancer Res. 71, 7187–7197 (2011).
Toyota, M. et al. Aberrant methylation in gastric cancer associated with the CpG island methylator phenotype. Cancer Res. 59, 5438–5442 (1999).
Niv, Y. Microsatellite instability and MLH1 promoter hypermethylation in colorectal cancer. World J. Gastroenterol. 13, 1767–1769 (2007).
Suzuki, H. et al. Distinct methylation pattern and microsatellite instability in sporadic gastric cancer. Int. J. Cancer 83, 309–313 (1999).
Xu, E. et al. Genome-wide methylation analysis shows similar patterns in Barrett's esophagus and esophageal adenocarcinoma. Carcinogenesis 34, 2750–2756 (2013).
Wu, W. et al. Hypomethylation of noncoding DNA regions and overexpression of the long noncoding RNA, AFAP1-AS1, in Barrett's esophagus and esophageal adenocarcinoma. Gastroenterology 144, 956–966 (2013).
Bian, Y. S., Osterheld, M. C., Fontolliet, C. & Bosman, F. T. & Benhattar, J. p16 inactivation by methylation of the CDKN2A promoter occurs early during neoplastic progression in Barrett's esophagus. Gastroenterology 122, 1113–1121 (2002).
Hansen, S. et al. Two distinct aetiologies of cardia cancer; evidence from premorbid serological markers of gastric atrophy and Helicobacter pylori status. Gut 56, 918–925 (2007).
Bosman, F. T., Carneiro, F., Hruban, R. H. & Theise, N. D. (eds) WHO Classification of Tumours of the Digestive System (IARC, 2010).
Hu, B. et al. Gastric cancer: classification, histology and application of molecular pathology. J. Gastrointest. Oncol. 3, 251–261 (2012).
Siewert, J. R. & Stein, H. J. Classification of adenocarcinoma of the oesophagogastric junction. Br. J. Surg. 85, 1457–1459 (1998).
Rodriguez, P. et al. BMP signaling in the development of the mouse esophagus and forestomach. Development 137, 4171–4176 (2010).
Pavlov, K. et al. Embryological signaling pathways in Barrett's metaplasia development and malignant transformation; mechanisms and therapeutic opportunities. Crit. Rev. Oncol. Hematol. 92, 25–37 (2014).
Kim, B. M., Buchner, G., Miletich, I., Sharpe, P. T. & Shivdasani, R. A. The stomach mesenchymal transcription factor Barx1 specifies gastric epithelial identity through inhibition of transient Wnt signaling. Dev. Cell 8, 611–622 (2005).
Noguchi, T. K. et al. Generation of stomach tissue from mouse embryonic stem cells. Nat. Cell Biol. 17, 984–993 (2015).
Kim, T. H. & Shivdasani, R. A. Notch signaling in stomach epithelial stem cell homeostasis. J. Exp. Med. 208, 677–688 (2011).
Que, J. et al. Multiple dose-dependent roles for Sox2 in the patterning and differentiation of anterior foregut endoderm. Development 134, 2521–2531 (2007).
Yang, A. et al. p63 is essential for regenerative proliferation in limb, craniofacial and epithelial development. Nature 398, 714–718 (1999).
Gao, N., White, P. & Kaestner, K. H. Establishment of intestinal identity and epithelial–mesenchymal signaling by Cdx2. Dev. Cell 16, 588–599 (2009).
Hryniuk, A., Grainger, S., Savory, J. G. & Lohnes, D. Cdx function is required for maintenance of intestinal identity in the adult. Dev. Biol. 363, 426–437 (2012).
Grainger, S., Savory, J. G. & Lohnes, D. Cdx2 regulates patterning of the intestinal epithelium. Dev. Biol. 339, 155–165 (2010).
Simmini, S. et al. Transformation of intestinal stem cells into gastric stem cells on loss of transcription factor Cdx2. Nat. Commun. 5, 5728 (2014).
Stringer, E. J. et al. Cdx2 determines the fate of postnatal intestinal endoderm. Development 139, 465–474 (2012).
Mutoh, H. et al. Conversion of gastric mucosa to intestinal metaplasia in Cdx2-expressing transgenic mice. Biochem. Biophys. Res. Commun. 294, 470–479 (2002).
Silberg, D. G. et al. Cdx2 ectopic expression induces gastric intestinal metaplasia in transgenic mice. Gastroenterology 122, 689–696 (2002).
Hryniuk, A., Grainger, S., Savory, J. G. & Lohnes, D. Cdx1 and Cdx2 function as tumor suppressors. J. Biol. Chem. 289, 33343–33354 (2014).
Seno, H. et al. CDX2 expression in the stomach with intestinal metaplasia and intestinal-type cancer: prognostic implications. Int. J. Oncol. 21, 769–774 (2002).
Fan, Z., Li, J., Dong, B. & Huang, X. Expression of Cdx2 and hepatocyte antigen in gastric carcinoma: correlation with histologic type and implications for prognosis. Clin. Cancer Res. 11, 6162–6170 (2005).
Abrams, J. A., Gonsalves, L. & Neugut, A. I. Diverging trends in the incidence of reflux-related and Helicobacter pylori-related gastric cardia cancer. J. Clin. Gastroenterol. 47, 322–327 (2013).
Islami, F. & Kamangar, F. Helicobacter pylori and esophageal cancer risk: a meta-analysis. Cancer Prev. Res. (Phila) 1, 329–338 (2008).
Boulton-Jones, J. R. & Logan, R. P. An inverse relation between cagA-positive strains of Helicobacter pylori infection and risk of esophageal and gastric cardia adenocarcinoma. Helicobacter 4, 281–283 (1999).
Rubenstein, J. H. et al. Association between Helicobacter pylori and Barrett's esophagus, erosive esophagitis, and gastroesophageal reflux symptoms. Clin. Gastroenterol. Hepatol. 12, 239–245 (2014).
Zang, Z. J. et al. Exome sequencing of gastric adenocarcinoma identifies recurrent somatic mutations in cell adhesion and chromatin remodeling genes. Nat. Genet. 44, 570–574 (2012).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Correa pathway
-
A cascade that describes the sequential steps during disease progression from superficial chronic gastritis, gastric atrophy and intestinal metaplasia to gastric dysplasia and cancer, proposed by Correa and colleagues.
- Goblet cells
-
Columnar cells in the intestinal glands that secrete mucins such as MUC2 into the gut lumen.
- Hypochlorhydria
-
A decrease or lack of hydrochloric acid in the gastric juice. Hypochlorhydria is accompanied by a gastric atrophy and intestinal metaplasia sequence, in which the number of acid-secreting parietal cells is decreased.
- Proton pump inhibitors
-
(PPIs). Drugs commonly used for patients with gastric ulcer that inhibit gastric acid secretion by binding to the H+/K+-ATPase.
- Hypergastrinaemia
-
Elevated levels of serum gastrin. As gastrin promotes gastric acid secretion from parietal cells, hypergastrinaemia occurs in a negative feedback manner when acid secretion is suppressed by certain drugs such as proton pump inhibitors (PPIs).
- Hiatal hernia
-
A condition in which part of the stomach, including the cardia, slides up towards the oesophageal hiatus in the chest cavity.
- Stratified squamous epithelium
-
Consists of several layers of keratin-expressing squamous cells on a basal membrane, and it is seen in the skin, mouth, oesophagus and vagina.
- LGR5
-
A receptor that can bind to R-spondin and activate the WNT–β-catenin pathway.
- Parietal cells
-
Gastric epithelial cells that reside in the corpus and secrete gastric acid.
- Chief cells
-
Gastric epithelial cells that reside in the base of corpus glands and secrete digestive enzymes such as pepsin.
- Enterochromaffin-like (ECL) cells
-
Gastric epithelial neuroendocrine cells that promote acid secretion from parietal cells by producing histamine.
- LRIG1
-
Expressed in intestinal and epidermal stem cells and regulates quiescence of these cells.
- SOX2
-
Expressed in multiple stem cells including embryonic stem cells and adult tissue stem cells, and is essential for maintaining self-renewal and pluripotency.
- LGR5–DTR mouse
-
A mouse in which diphtheria toxin receptor (DTR) is expressed in leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5)+ cells. Given that cells in mice do not normally express DTR, only LGR5+ cells are killed and ablated when diphtheria toxin (DT) is given. In the stomach, mature chief cells express LGR5, thus DT administration causes specific cell death in the chief cell population.
- Signet ring cancer cells
-
Cancer cells that contain a large quantity of mucins in the cytoplasm and have a thin nucleus in the cell periphery.
- G-cells
-
Gastric epithelial cells in the antrum that secrete gastrin.
- D-cells
-
Gastric epithelial cells in the antrum that secrete somatostatin.
- +4 position
-
The cell position in a gastrointestinal gland is usually counted and numbered from the base of the gland (that is, the cell at the bottom of the gland is called position +1). Until leucine-rich repeat- containing G protein-coupled receptor 5 (LGR5)+ stem cells were discovered, it was thought that major gastrointestinal stem cells resided at the +4 position, based on label-retaining assays.
- CCKBR
-
A receptor for the gastrin peptide. It has been thought to be involved in gastric acid secretion in CCKBR+ neuroendocrine cells and parietal cells.
- Residual embryonic cells
-
(RECs). Potential precursors of Barrett oesophagus; these cells are most evident in the gastric cardia in the embryonic stage, but some can persist in adult mice.
Rights and permissions
About this article
Cite this article
Hayakawa, Y., Sethi, N., Sepulveda, A. et al. Oesophageal adenocarcinoma and gastric cancer: should we mind the gap?. Nat Rev Cancer 16, 305–318 (2016). https://doi.org/10.1038/nrc.2016.24
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc.2016.24
This article is cited by
-
Lymphangiogenesis in gastric cancer: function and mechanism
European Journal of Medical Research (2023)
-
In vivo assessment of Lauren classification for gastric adenocarcinoma using diffusion MRI with a fractional order calculus model
European Radiology (2021)
-
Gastric squamous-columnar junction contains a large pool of cancer-prone immature osteopontin responsive Lgr5−CD44+ cells
Nature Communications (2020)
-
Paradox of age-specific incidence rates of second primary cancer in individuals with esophageal cancer
Journal of Gastroenterology (2020)
-
Tumor-specific genetic aberrations in cell-free DNA of gastroesophageal cancer patients
Journal of Gastroenterology (2019)