Abstract
The study of human cell–cell and cell–pathogen interactions that occur in the context of complex tissue cytoarchitecture is critical for deciphering the mechanisms of many normal and pathogenic processes. This protocol describes methods for culturing and infecting explants of human tissues to study the pathogenesis of human infectious agents and their local interactions. The protocol relies on the use of fresh human tissues dissected into small blocks or biopsies that are cultured at the liquid–air interface on collagen rafts. These tissue blocks retain their cytoarchitecture and support productive infection of various pathogens without exogenous stimulation. Experimental details for setting up cultures of human tonsils, lymph nodes and cervicovaginal and rectosigmoid tissues, including protocols for their infection with HIV-1 and other pathogens, are described here. Using this protocol, culture and infections can be set up in 3–6 h and be maintained for 2–3 weeks, depending on the tissue used.
Similar content being viewed by others
Introduction
The technique of culturing cells grown under controlled laboratory conditions was developed in the United States by Ross Harrison1,2 and later was significantly improved by Alexis Carrel3. These techniques became one of the most important instruments in experimental biology and medicine and greatly contributed to the progress in understanding the structure and function of mammalian cells. Nowadays, cells attached to the surface of a culture vessel or suspended in culture medium are used in biological laboratories throughout the world. Many of the techniques used today, including light, fluorescence and electron microscopy as well as flow cytometry, virological assays and numerous methods of molecular biology, were developed or adapted for the study of such isolated cells either at the bottom of a Petri dish or floating in culture medium.
However, the very first steps in processing cells for cultures, namely tissue disruption and isolation of cells from their native microenvironment, prevent this system from faithfully reflecting important aspects of cell–cell and cell–pathogen interactions that occur in the context of complex tissue cytoarchitecture. But deciphering the mechanisms of these interactions is critical for understanding normal and pathogenic processes, including those caused by human pathogens.
Human immunodeficiency virus is one of the most studied human pathogens. Initially, it was thought, on the basis of the techniques available at that time, that after infection HIV went into almost full latency, as little or no virus was found in patients' blood soon after infection4. However, later, when lymph nodes of infected individuals were studied, it was established that HIV does not go into latency but rather replicates continuously in lymph nodes5. There, although it infects only a fraction of its main potential targets (CD4+ T cells), HIV-1 eventually either kills or renders many other cells dysfunctional, including CD8+T cells, macrophages and follicular-dendritic cells. Eventually, the entire structure of the lymph node collapses (reviewed in ref. 6). It is believed that it is this collapse, rather than the death of productively infected cells, that is the main cause of immunodeficiency, as under normal conditions the cytoarchitecture of the lymph node provides the structural context for immune cell interactions that lead to an immune response. In AIDS patients, this context is destroyed and the immune response deteriorates. It has been established that HIV replication in gut-associated lymphoid tissue is also important in HIV disease7,8. In the gut, the death of HIV-infected lymphocytes also leads to structural deterioration of this tissue, including the death of bystander (uninfected) cells. According to recent data, this deterioration results in the translocation of other microbes and/or their components through the mucosal surface7,9.
Notwithstanding the complexity of HIV pathogenesis in vivo, HIV infection is usually studied in vitro in a relatively primitive system of transfected cell lines or suspensions of peripheral blood mononuclear cells, or in blood-derived macrophages attached to the surface of a cell culture dish. Moreover, these cells need to be activated to support HIV replication. Although cell lines are activated constitutively, peripheral blood mononuclear cells need to be activated and stimulated by incubation with an exogenous activator, such as phytohaemagglutinin (PHA) and IL-2. Although such activation transforms cell cultures into efficient virus producers, it significantly changes the expression of cell surface molecules and the functioning of the intracellular machinery. This is another reason why these cells inadequately model HIV target cells in tissues. Thus, as critical events of HIV disease, as well as those of several other diseases caused by human pathogens, occur in tissues, the field requires a model for the study of disease pathogenesis in tissues under controlled laboratory conditions. In the case of HIV, this requirement is especially important because of the high cost of animal models, whose adequacy is sometimes questioned (see ref. 10).
Several years ago, we developed a system of human lymphoid tissue ex vivo to study the pathogenesis of HIV as well as that of other infectious agents11,12,13,14,15,16,17,18,19. This model is based on a technique developed by Joseph Leighton20,21 in the 1950s and further refined by Robert Hoffman in the last quarter of the previous century22. Basically, the model consists of integral blocks of tissues incubated at the liquid–air interface on a raft. We developed this model to study HIV infection in human tissue, and we initially used lymph node and tonsillar tissues for these ex vivo studies. More recently, we extended it to the culture of cervicovaginal23,24,25 and rectosigmoid tissues16,26,27, as these tissues are critical in the transmission of HIV infection and play an important role in HIV pathogenesis. In principle, this technique could also be adapted to the study of other tissues, both normal and cancerous28. More systematic studies are required to optimize this technique and to understand its limitations. As of now, we have failed to maintain ex vivo liver and kidney tissue, probably because of their complex cytoarchitecture and high metabolism.
Upon inoculation ex vivo, human lymphoid tissue supports productive HIV infection without exogenous activation and stimulation, and it retains tissue cytoarchitecture as well as the pattern of expression of key cell surface molecules relevant to HIV infection16,29,30,31. Also, some of the tissue functions are preserved ex vivo. For example, upon challenge with (recall) antigens, such as diphtheria toxoid or tetanus toxoid, ex vivo lymphoid tissue responds with a vigorous production of specific antibodies32. The critical importance of the tissue cytoarchitecture is underscored by the inability of the mixture of isolated lymphocytes to build an efficient humoral response in vitro unless cell density, culture vessel geometry, agitation, oxygenation and other factors are strictly maintained33,34. Similarly, blocks of cervical tissue ex vivo continue to secrete mucus, just as this tissue does in vivo (B. Brichacek and L.M., unpublished data).
The system of culturing human tissues ex vivo can be used to study non-HIV microbes as well. These tissues have been shown to support productive infection of the following viruses: herpesvirus (HHV)-6 see (refs. 16,35), HHV-7 see (ref. 16), HCMV (HHV-5)17, HSV-2 (HHV-2)18, vaccinia virus19, measles virus14,15 and West Nile virus (P. Murphy, unpublished data). In this ex vivo system, human tissues have also been shown to support replication of the bacterium Borrelia burgdorferi36 and of the parasite Toxoplasma gondii (A. Sassi et al., submitted).
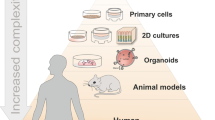
In summary, the explant system of cultured human tissues ex vivo permits the study of normal and pathogenic processes, including ones caused by human infectious agents, in the context of tissue cytoarchitecture under controlled laboratory conditions. An alternative approach is to build tissue-like structures from single cells using various scaffolds; for a detailed protocol, see reference 37. Various research teams have also used organoids formed by coculture of several cell lines or isolated primary cells in biorecators38,39,40,41. Although these strategies are valuable for many studies, and some have been successful in studying infectious agents42, such cell constructs may not faithfully represent many aspects of real tissue, including their cytoarchitectures, intercellular interactions and the presence of target cells and their locations.
Moreover, it requires isolation of cells and their maintenance without alteration of their physiology as well as a previous understanding of which cell types are essential for viral infection. On the other hand, use of cell lines or cloned primary cells for such constructs has the advantage of experimentation with highly reproducible systems overcoming the natural heterogeneity of donor tissues. However, in cases in which little is known about the contribution of various tissue cells and multicellular tissue structures in microbial pathogenesis, the use of tissue explants described in this protocol may be more adequate.
We focus our efforts on developing conditions for maintaining real tissues ex vivo. The advantage of this system is that in certain aspects it fills the gap between cultures of isolated cells and the situation in vivo. On the other hand, the system of ex vivo tissues has some limitations in the study of infection of human pathogens (Table 1). The most important of these limitations is the difficulty of applying many modern investigative tools developed for isolated cells to these tissues. For example, although microscopy gives subcellular resolution in imaging of single cells, the problem of deep tissue penetration beyond a few hundred microns is only partially solved with two photon excitation microscopy43,44.
Overcoming these limitations and developing new techniques to analyze various normal and pathological processes in the depths of the tissues under strict laboratory conditions may revolutionize biomedicine. In such a system, it will be possible to test various drugs as a preliminary step before engaging in costly and lengthy clinical trials. Those drugs that do not work in ex vivo tissues can hardly be efficient in vivo, although the opposite is not necessarily true. Also, tissue systems may reveal basic mechanisms of pathogenesis that are not recapitulated in single-cell cultures.
With optimization of the protocol for ex vivo tissue cultures, it will presumably become possible to maintain ex vivo human tissues other than those described in this protocol or elsewhere22,41,45,46. Moreover, it is conceivable that a multitissue system can be developed to study tissue–tissue interactions. In particular, it may be possible to develop a system in which one tissue will affect another tissue through the soluble factors released into the common medium or through cells migrating from one tissue to another. Such a system may reproduce what happens at the organism level and simulate systemic factors associated with various pathological conditions. Another advantage of ex vivo tissues is the ability to visualize in real time the development of pathogenic conditions using confocal microscopy. Recently, such an approach was used to study green fluorescent protein-labeled HIV penetrating cervical tissue ex vivo47. HIV studies have showed important gaps in our knowledge of tissue pathogenesis. Indeed, although we know the entire genome of this virus, the proteins encoded by these genes and a great deal about molecules on the cell surface that bind the virus, and about the HIV life cycle inside infected cells, we know too little about the mechanisms of viral pathogenesis in tissues that eventually determine immunodeficiency.
In general, we believe that development of techniques for culturing integral tissues ex vivo, together with various technologies that allow monitoring of cells and of soluble factors in the depths of the tissue, will transform biomedicine in the twenty-first century in the same way as the development of techniques that allowed the culture of individual cells revolutionized biology in the twentieth century.
Although numerous articles based on the technique of maintaining human tissue ex vivo have been published, important technical details remain either unpublished or scattered in various papers addressing concrete questions of viral pathogenesis. This protocol aims to fill this gap.
The protocol in stages
Briefly, the technique of culturing human tissue ex vivo to study the pathogenesis of HIV and other infectious agents consists of the following steps (Fig. 1):
Six major stages of the protocol to set up human tissue explants to study human infectious agents: (a) Tissue (tonsils, lymph nodes, cervicovaginal, rectosigmoid) is obtained through surgery or from cadavers, and delivered to the laboratory; (b) tissue is dissected into small blocks; (c) blocks are placed at the medium–air interface on collagen rafts in appropriate culture vessels. (Note: the minimum number of wells that constitute an experimental condition is boxed in red on each culture plate and labeled with a circled star; the number of tissue blocks per well is indicated); (d) tissue is infected with a pathogen of interest (note that the modality and order of infection for cervical tissue is different from those of other tissues); (e) tissue is cultured for 2–3 weeks and samples of medium are collected periodically and analyzed for pathogen components and for various metabolites of interest; (f) at various time points, tissue blocks are collected and analyzed by use of flow cytometry or microscopy.
-
a
Tissue (tonsils, lymph nodes, cervicovaginal and rectosigmoid tissues and so on) is obtained through surgery, or from cadavers according to an Institutional Review Board (IRB)-approved protocol.
-
b
Tissue is dissected into small blocks.
-
c
Blocks are placed at the medium–air interface on collagen rafts.
-
d
Tissue is infected by a pathogen of interest.
-
e
Tissue is cultured for 12–14 d or longer; samples of medium are collected periodically and analyzed for pathogen components and/or various metabolites of interest, in particular for cytokines.
-
f
At various time points, tissue blocks are dispersed into single cells, stained with fluorescence-labeled antibodies and analyzed with flow cytometry. Also, samples of tissues can be fixed and analyzed immunohistologically.
Experimental design
Below, we emphasize elements of the technique that, in our experience, are most important to avoid failure of the experiment.
Tissues. The tissue delivered to the laboratory should be in good condition, having a 'healthy' pinkish color and lacking large blood clots and greenish necrotic centers. The state of the tissue is also dependent on how quickly it is delivered for processing. Unfortunately, it requires some experience to determine which parts of the living tissue are healthy. To visualize the selection process of tissue for histoculture, in Figure 2 we have illustrated some of the steps in the selection and preparation of tonsillar tissue. Figure 2a is a montage of pictures of (i) a tonsil as it is received after surgery, (ii) the parts of the tissue that cannot be used for culturing, (iii) usable tissue cut into large pieces (Step 10A(iv)) and (iv) the tissue strips that will be later cut into blocks (Step 10A(v)). Figure 2b shows an image of the tissue blocks before (Step 10A(v)) and after (Step 10A(vii)) being deposited on top of the Gelfoam sponge in a six-well plate. We advise beginners to isolate tissue cells and to subject them to an objective microscopic or flow cytometric viability test (e.g., with trypan blue or propidium iodide). It is important, for long-term culture, to start the experiment with a healthy tissue. However, tissues are not equal, and some are more prone to deterioration than the others. For example, tonsillar tissue is soft and prone to deterioration. According to our experience, this tissue should be delivered within 3–5 h post-surgery. Cervicovaginal tissue is much sturdier, and we successfully cultured this tissue after delivery 24 h post-surgery. The same is true of the rectosigmoid tissue that we have used. Sturdier tissues can be obtained from cadavers, whereas other tissues can be utilized only if they are procured shortly after surgery. One might think that tonsillar tissue is more vulnerable to deterioration, as tonsillectomy might have been indicated due to inflammation. However, this is not the case, as routine tonsillectomy is not performed during acute inflammation.
(a) Black arrows point to the parts of the tissue that cannot be used and should be discarded (tonsilolithes, cauterized tissue, bloody tissue and green necrotic tissue). Usable tissue parts are cut into large pieces (Step 10A(iv)) and strips (Step 10A(v)). (b) Tissue blocks before (Step 10A(v)) and after (Step 10A(vii)) being deposited on top of the gelfoam sponge in a six-well plate.
Conditions of transportation may also be important. We use RPMI 1640 as a delivery medium; however, other solutions can also be used. We have not yet optimized this step. We have noticed that, at least for tonsillar tissue, cooling on ice during delivery makes it less suitable for long-term culture; however, we have not performed a systematic study of this issue. We maintain tissues at 15–22 °C during delivery.
Tissue processing. For reproducibility of results, tissues should be dissected into blocks of uniform size. We dissect by hand with a blade or scalpel, and it takes several months for a researcher or a technician to become trained in cutting tissues into regular blocks. During this procedure, parts of the tissue that do not look healthy or that contain blood clots should be discarded. The size of the blocks should be approximately 2 mm × 2 mm × 1 mm. Smaller blocks are more difficult to prepare, and also many cells are lost during cutting, which inevitably involves compressing and squeezing of the tissue. Larger blocks are easier to cut, but they cannot be cultured for long because of necrosis at their center, which develops because of the deficit of nutrients in the middle of the block. Our attempts to use various mechanical devices for cutting did not produce satisfactory results.
Microbial contamination. After surgery, in most cases, the hospital's pathologist evaluates the samples, at least visually, before releasing them for scientific purposes. Routinely, this evaluation is performed in nonsterile conditions, often on a table contaminated by other samples. Also, tissues such as tonsils or guts are not sterile by nature. All this makes the problem of contamination serious. We use a cocktail of antibiotics to protect tissues from infection (see PROCEDURE below). However, we do not stick to one cocktail. When several tissues from different donors become contaminated, we ask our microbiology department to analyze samples for microbes and, depending on the results, we use appropriate antibiotics. There is a lesser probability of contamination if the tissues come from sterile surgery or biopsies. In these cases, the possible source of contamination is one's own laboratory, and the measures to prevent this contamination are the same as for routine cell cultures. Nevertheless, we routinely culture tissues overnight and check for contamination the following morning before using them for laborious long-term experiments.
The role of various microbes that are present in the donor tissue at the time of experimental tissue infection is complex and is not limited to the application of this protocol but rather constitutes a general biological problem. In the case of HIV infection, these coinfecting microbes may determine HIV replication by inducing cell activation, by changing the cytokine spectra and by up- or downregulating HIV receptors and coreceptors. Our analysis of tonsils from 58 patients has demonstrated that the most frequent pathogen is mycoplasma, which is found in 39% of tissues, followed by several types of Staphylococci, S. aureus, S. heamolyticus and S. werneri found in 12%, 5% and 2% of tissues, respectively. Diphteroids and Gemella are found in 7% and 3.5% of tissues, respectively. No pathogens were detected in 30% of tissues (J.-C.G. and L.M., unpublished data). In the framework of this protocol, we try to eliminate 'contaminating' pathogens with antibiotics. However, even bacterial products can signal through Toll-like receptors and thus affect HIV replication48. Also, various ubiquitous viruses, in particular herepsviruses that are present in the tissue, may also affect HIV replication. The presence of the herepsviruses can be measured with real-time PCR18. The presence of these microbes or their fragments can be considered as one of the parameters of this system that are difficult to control. On the other hand, their presence may be used to study HIV interactions with other microbes in the context of tissues ex vivo. Unlike 'sterile' cultures of isolated cells, such a system may more faithfully reproduce intermicrobial interactions that occur in vivo.
Rafts. In the course of the development of explant technology, researchers have used different supports (rafts) to culture tissue on. These include filter paper, Millipore filters, wire meshes and so on. In our experience, as well as in the experience of other labs, the best-tested support is collagen gel, such as that used for surgery. We use the product Gelfoam produced by Upjohn. Other groups that use similar protocols for ex vivo tissue culture also use this product49,50. A similar product, such as Ultrafoam, is commercially available from Davol Inc. Also, different matrixes such as cytomatrix) can be used for the same purpose. However, we are not aware of a comparative study of these products as applied to ex vivo tissue culture.
Ex vivo tissue immunization. Tonsils and lymph nodes can easily mount secondary immune responses against public antigens or against vaccinal antigens, such as tetanus toxoid or diphtheria toxoid. Stimulation is achieved by addition of the antigen to the culture medium for the first 3 d of culture. It is critical to change the medium thoroughly following this stimulation, because the antigen carried-over will complex with any specific antibody produced and negate subsequent detection in immunoassays. The concentrations we have used vary from 1 to 100 ng ml−1. In our experience, roughly 80% of tonsils tested respond to challenge by either tetanus toxoid or diphtheria toxoid, which may reflect the responsiveness of the donor population.
Medium change and evaluation of the release of metabolites. Empirically, we chose a 3-d period between consecutive medium changes. When the collected medium is analyzed for viral components (in the case of HIV-1, for p24, reverse transcriptase or RNA) or for the production of cytokines, it should be taken into account that after each medium change the production of the compound of interest begins at a level of almost zero and reaches the value measured in the medium collected 3 d later. Formally, the data should be presented as a 'saw'-like graph (Fig. 3). However, we think it is more adequate to present the release of components as a cumulative curve. The graphs in Figure 3 illustrate both methods of data representation applied to the replication of R5 HIV-1 SF162. Neither of these methods is perfect: the first method is complicated and does not reflect the amount of medium retained in the gel in spite of medium change (we estimate that a 1 cm × 1 cm piece of Gelfoam of standard thickness retains ∼0.5 ml of medium); the second method does not represent primary results, as each datum for each point represents the sum of the measurement at this and all preceding time points. In spite of the fact that kinetics of viral replication for various viruses in some tissues might be different (e.g., X4 HIV-1 or X4R5 HIV), these methods of presentation are nonetheless valid. Note that the scale of the y axis has been changed between panels A and B to emphasize the difference between cumulative and differential mode of data presentation. To avoid distracting the reader of this technical article with the scientific problem of the replicative capacity of different HIV variants in different tissues, we present only one (R5) HIV-1 variant replicating in different tissues and chose experiments in which the efficiency of replication was comparable in different tissues. For the differences in the average replication of HIV variants in different tissues, see refs. 51 and 52.
Blocks of human tissues were prepared and infected with the R5 HIV-1 strain SF162 and cultured as described in the protocol. The culture media were collected and replaced at different time points following viral infection. The concentration of viral antigen p24 was measured in each sample. (a) The graphs in the blue box represent the primary data measured for each sample; the solid blue curve is the interpolation of these data points. Note: the interpolation curve does not take into account the fact that after a medium change, the concentration starts from almost zero to reach the level measured at the following time point. The dark dotted line reflects this fact. (b) The graphs in the red box represent the plots of the cumulative production of p24 obtained for each datum point by summing up the measurement at this time point with the measurement of all the preceding time points. Note that the scale of the y axis has been changed between a and b to emphasize the difference between cumulative and differential mode of data presentation. To avoid distracting the reader of this technical article with the scientific problem of the different replicative capacity of different HIV variants in different tissues, we present here only one (R5) HIV-1 variant replicating in different tissues and chose experiments in which the efficiency of replication in different tissues were comparable. For the differences in the average replication of HIV variants in different tissues, see refs. 51,52.
Comparison of results obtained under different experimental conditions: choosing controls and the appropriate statistical method. Choosing the proper controls. Unlike cell lines or tissues from genetically identical mice, samples obtained from humans are very variable in most parameters measured (e.g., relative presence of lymphocytes of different subsets, spectra of cytokines produced, activation status of cells). Accordingly, when subjected to infection by pathogens, tissues respond differently. For example, after inoculation with the same inoculum of the same HIV stock, HIV replication in tissues from different donors can differ by a factor of 20 (see ref. 51). Therefore, comparison of average parameters in the group of untreated tissues with these parameters in the experimentally treated group of donor tissues undermines the statistical power of the analysis because of donor-to-donor variability. To increase the power of the analysis, the experimental design should include the division of each donor tissue into experimental and control samples that are not experimentally treated ('donor-matched control' that are not infected, not exposed to drug and so on). Each of the measured parameters in the experimental sets should be normalized by the corresponding parameter in donor-matched control. Unfortunately, if donor-matched control tissues are not available, e.g., if one studies tissues from chronically infected patients, a large cohort of control patients should be assembled and used as a 'statistical control'53.
Statistics. The number of donors (n) needed for reproducibility of the results depends on how strong the effect is. In the absence of significance, the sample size must be increased to reach a reasonable statistical power. Among the effects of pathogens on human tissues reported so far, we have encountered effects that required a value of n from as little as 5 to as high as 83. The use of statistical analysis software with power analysis, such as StatMate (StatMate, GraphPad Software) is recommended. In the case of normalized data, namely when the parameter for control tissue is defined as 100% and therefore will have no variance, the method of statistical analysis chosen should reflect this heteroscedastic nature of the data. We usually use Prism 5.0 and its accompanying statistics guide (Harvey Motulsky 'Statistical analysis for laboratory and clinical researchers,' GraphPad Software).
Materials
Reagents
Caution
Tissues should be harvested according to an IRB-approved protocol. The protocol may reflect that, for most of the projects, tissues are collected from indicated surgeries or from cadavers and thus are not harvested for the purpose of the study. In some cases, they can be considered as 'pathological waste.' Moreover, most of the IRB-approved protocols we use require that the samples be anonymous and that the tissue containers be stripped of all identifiers at the site of collection by the hospital personnel. Tissues can be obtained from local hospitals or from the National Disease and Research Interchange. In the case of projects for which tissues are collected specifically and/or for which access to patients' records is required, a special IRB-approved protocol is needed.
-
Explant culture medium (ECM) for the initial overnight incubation (ECMON) (see REAGENT SETUP)
-
ECM for the rest of experiment (see REAGENT SETUP)
-
Fluorescence-activated cell sorting (FACS) staining buffer (see REAGENT SETUP)
-
Bead staining buffer (see REAGENT SETUP)
-
Digestion solution (see REAGENT SETUP)
-
Gelfoam 12–7 mm (adsorbable gelatin sponge; NDC, cat. no. 09-0315-03; Pharmacia and Upjohn Company, distributed by Pfizer)
-
RPMI 1640 with L-glutamine (GIBCO Invitrogen, cat. no. 11875-093)
-
Modified Eagle's medium (MEM)-nonessential amino acids, 10 mM (100 × ) (GIBCO Invitrogen, cat. no. 11140-050)
-
MEM sodium-pyruvate, 100 mM (100 × ) (GIBCO Invitrogen, cat. no. 11360-070)
-
Timentin (GlaxoSmithKline, NDC 0029-6571-26) (see REAGENT SETUP)
-
Gentamicin (50 mg ml−1, 1,000 × ) (Cellgro-Mediatech, cat. no. 30-005-CR)
-
Fungizone (250 μg ml−1, amphotericin B, 100 × ) (GIBCO Invitrogen, cat. no. 15290-018)
-
Fetal bovine serum (FBS) gem-cell (Gemini Bioproducts, cat. no. 100-500)
Critical
We advise testing several lots of serum for culture optimization, and then use of the same lot of FBS for an entire series of experiments. In the case of viral replication, we always test several lots on tissues from several donors and select the lot that gives the highest viral replication. Also, FBS is critical for the ability of tissue to secrete cytokines in culture medium: we observed (J.-C.G. and L.M., unpublished data) that different lots differ in their ability to support secretion of various cytokines upon stimulation of tissues with several polyclonal activators.
-
Normal mouse serum (NMS) (Gemini Bioproducts, cat. no. 100-113)
-
Normal goat serum (NGS) (donor goat serum; Gemini Bioproducts, cat. no. 100-109)
-
Collagenase type IV (GIBCO Invitrogen, cat. no. 17104-019) (see REAGENT SETUP)
-
Tris-HCl, 1 M, pH 7.4 (K-D medical, cat. no. 3400-1040)
-
PBS, pH 7.4 (GIBCO Invitrogen, cat. no. 10010-023)
-
CST beads (cytometer setup and tracking beads) (BD Biosciences, cat. no. 642412)
-
Flow cytometry compensation beads (BD Biosciences, cat. nos. 552843 and 552844 for mouse and rat κ-chain-bearing antibodies, respectively, or Spherotech, cat. no. CMIgGP-50-3K for mouse κ-chain-bearing antibodies) (see REAGENT SETUP)
-
Live–Dead fixable blue fluorescent reactive dye reagent kit (Invitrogen, cat. no. L-23105), or equivalent depending on available detector channels
-
Amine-modified particles (Bangs Laboratories, cat. no. SMPLX) or equivalent (see REAGENT SETUP)
-
Fix and Perm: permeabilization reagent solution A and B (Caltag-Invitrogen, cat. no. GAAS-004)
Equipment
-
Petri dish, 100 mm × 20 mm (BD-Falcon, cat. no. 35-3003)
-
Petri dish, 150 mm × 25 mm (BD-Falcon, cat. no. 35-3025)
-
6-well plates (Costar Corning, cat. no. 3506)
-
12-well plates (Costar Corning, cat. no. 3513)
-
24-well plates (Costar Corning, cat. no. 3524)
-
Sarstedt sealed screw-cap tubes (Sarstedt, cat. no. 72-694-006, or equivalent)
-
Nalgene 0.2-μm filter cap 500-ml bottles (Nalgene, cat. no. 169-0020, or equivalent)
-
Nalgene 0.2-μm filter cap 200-ml bottles (Nalgene, cat. no. 157-0020, or equivalent)
-
12 mm × 75 mm 5-ml tubes (BD-Falcon, cat. no. 352058)
-
12 mm × 75 mm 5-ml strainer-cap tubes (BD-Falcon, cat. no. 352235)
-
40-μm strainer cap for 50-ml tubes (BD-Falcon, cat. no. 352340)
-
50-ml conical tube (BD-Falcon, cat. no. 352070)
-
Disposable pellet pestle (Sigma Aldrich, cat. no. Z359947, or equivalent)
-
Cordless motor for pellet pestle (Sigma Aldrich, cat. no. Z359971, or equivalent)
-
Thermomixer with block for 1.5-ml tubes (Eppendorf, cat. no. 022670000, or equivalent)
-
Flow cytometer (Becton Dickinson LSRII running DIVA 6.0, or equivalent)
-
Forceps
-
Scalpels, nos. 10 and 23
-
Sharp scissors
-
Flat weighing metallic spatula (see EQUIPMENT SETUP)
-
Humidified CO2 incubator set at 90% humidity to avoid dehydration of the cultures
-
Benchtop centrifuge with properly sealed buckets for aerosol containment to prevent the formation of potentially hazardous aerosols
Reagent setup
Timentin
-
Prepare a working 100 × stock solution by adding 100 ml of sterile 0.15 M NaCl to a 3.1-g vial for intravenous administration. Aliquot in 1-ml aliquots distributed in sterile screw-cap tubes. Freeze and keep all aliquots at −30 °C. Aliquots are stable for up to 30 d. Unused thawed aliquots should be discarded.
ECM
-
Open a fresh 500-ml bottle of RPMI 1640, remove 90 ml (set aside for other use) and add 75 ml of FBS, 5 ml of 100 × MEM-nonessential amino acids, 5 ml of 100 × fungizone, 5 ml of 100 × MEM–sodium pyruvate and 500 μl of 1,000 × gentamicin. Store at 4 °C.
ECMON
-
This culture medium is to be used only for the first night of culture. It is prepared freshly by adding timentin to the ECM. Dilute 1 ml of freshly thawed 100 × timentin in 100 ml of ECM. Prepare the volume needed for the experiment on the basis of the indications found in Table 2.
Table 2 Culture setup.
Collagenase IV
-
Prepare a 10 mg ml−1 2 × solution by dissolving 1 g of collagenase type IV into 100 ml of RPMI 1640 supplemented with 5% FBS (vol/vol). Filter-sterilize through a 0.20-μm filter cap bottle. Distribute 1-ml aliquots into screw-cap tubes and keep frozen at −80 °C.
FACS staining buffer
-
Prepare a staining buffer by adding 5 ml of NMS and 5 ml of NGS to 1 × PBS, pH 7.4 (1% (vol/vol) final concentration, each). Filter-sterilize through a 0.2-μm filter-cap bottle.
Bead staining buffer
-
Prepare a buffer by adding 5 ml of NGS to 1 × PBS, pH 7.4 (1% (vol/vol) final concentration). Filter-sterilize through a 0.2-μm filter cap bottle.
Critical
It is imperative to use a buffer that does not contain mouse serum, as this would prevent binding of the labeled mouse antibodies to the compensation beads.
Flow cytometry compensation beads
-
Prepare as many 12 × 75 tubes as there are fluorochrome conjugates used for cell staining. To do so, add a drop (≈40 μl) of anti-mouse κ-chain (or anti-rat κ-chain for rat monoclonal antibodies) and a drop of control microsphere per tube.
Critical
If several conjugates of the same tandem dye are used, prepare a tube for each conjugate, as the spectral properties of each tandem dye may vary between antibodies and between lots of the same conjugate.
Amine-modified particles
-
Dilute the amine-modified stock solution into PBS to a concentration of 10 × 106 beads ml−1. Transfer an aliquot of 50 μl into a 12 × 75 FACS tube and add 1 μl of Live–Dead blue fixable dye reconstituted according to the manufacturers' instructions by adding 50 μl of DMSO per dye vial (25 μg). Incubate at room temperature (19–22 °C) in the dark for 20 min. Wash with 1 ml of PBS, centrifuge at 8,000g at 16 °C for 3 min, decant the supernatant, add 100 μl of PBS, vortex, add 100 μl of a 2% (wt/vol) formaldehyde solution in PBS and allow to remain for at least 20 min.
Equipment setup
Flat weighing metallic spatula
-
Bend the flat part of the spatula to a 45–90° angle, otherwise if the angle is sharp, the spatula may damage the Gelfoam when it is used to squeeze the trapped air bubbles. We bent the spatula to a 45° rather than 90° angle to avoid having the hand right above the tissue, which might increase the risk of contamination.
Flow cytometer
-
Verify the proper function and setup of the flow cytometer lasers, fluidics and optical channels using the cytometer setup and tracking beads if running DIVA 6.0. Alternatively, use similar approaches to ensure proper function and setup of the instrument. Detailed instructions are available in reference 54.
Critical
A poorly setup flow cytometer will give unreliable data. It is imperative that the instrument be set up and verified daily. Compensation settings and LASER delays should be performed for each experiment.
Procedure
Preparation of Gelfoam sponges
Timing 30 min to 1 h depending on the size of the experiment
-
1
Prepare ECM and ECMON as described in REAGENT SETUP.
Critical Step
ECMON should be prepared freshly.
-
2
Calculate the number of Gelfoam pieces needed per experiment on the basis of the type of tissue used and the number of wells required to perform the experiment (see Table 2). For each plate necessary for the experimental design, allow 15 pieces per 6-well plate for tonsils, adenoids, appendix; allow 2 pieces per 12-well plate for cervicovaginal tissue; and allow 3 pieces per 24-well plate for rectosigmoid tissue.
-
3
Depending on the number of Gelfoam sponges required for the experiment, either fill a 100 mm × 20 mm Petri dish with 30 ml of ECM (if three sponges or fewer are required) or fill a 150 mm × 25 mm Petri dish with 50 ml of ECMON (if more than three sponges are required).
-
4
Take out the appropriate amount of 12-7 Gelfoam pieces and put them in the Petri dish.
-
5
Start the rehydration process using ethanol-sterilized forceps to push the Gelfoam pieces gently into the medium.
Critical Step
Be extremely careful in pressing on the Gelfoam. At this stage, the sponge is extremely brittle and might break apart if too much force is applied before rehydration starts.
-
6
Finish the hydration process by pressing on the Gelfoam with the bent flat spatula sterilized with ethanol. This chases the trapped air out of the sponge.
Critical Step
The Gelfoam should be as free of air as possible: the presence of air will block the capillaries through which nutrients reach the tissue.
-
7
Use ethanol-sterilized scissors to cut the rehydrated Gelfoam into pieces of the appropriate size: for 6-well plates, cut into four equal pieces; for 12-well plates, cut into six equal pieces; for 24-well plates, cut into four equal pieces and then cut each piece in half to obtain eight pieces per sponge.
-
8
Place a piece of Gelfoam into each well and add the appropriate amount of ECMFN: 3 ml per well of a 6-well plate; 1 ml per well of 12-well plate; 0.5 ml per well of 24-well plate.
-
9
Place the plates in a 37 °C, 5% CO2 incubator with high relative humidity (>83%) while the tissues are dissected.
Dissection and preparation of tissues
Timing 1–3 h for dissecting tissues and an additional hour to set up tissues on sponges for 342 blocks, i.e., six plates of tonsil explants
-
10
The dissection protocols vary slightly for each type of tissue used. If using tonsils or adenoids, follow option A; if using lymph nodes, follow option B; if using rectosigmoid tissue from surgical recession, follow option C; if using rectal biopsies, follow option D; if using cervicovaginal tissue, follow option E. See Table 2 for a synopsis of culture conditions.
-
A
Tonsils, adenoids
-
i
Wash tissues in PBS and transfer into a 100-mm Petri dish containing 10–20 ml of PBS.
-
ii
Cut each tonsil or adenoid into several large pieces (4–5 pieces per tonsil).
-
iii
Transfer one piece into the cover of a new Petri dish filled with 5 ml of medium, just enough to cover the lid. Cover the Petri dish containing the rest of the tissues to avoid desiccation.
-
iv
With a 23-gauge blade scalpel and forceps, remove the cauterized tissue from the tonsil or adenoid and remove the capsule surrounding the tissue. Remove bloody or inflamed parts, if any, and any parts containing tonsillolithes or parts with a suspicious color (bordering on a light brown-green).
-
v
Cut the tissues into slices of ∼2 mm thickness. Remove any undesirable tissues, and recut the slices into strips of 2 mm width. Then cut the strips into 1-mm blocks. This should result in a size of roughly 2 mm × 2mm × 1 mm. Cut as many blocks as needed; at least 27 blocks are required per experimental condition. Transfer the blocks into a clean Petri dish containing ECMON.
Critical Step
Keep the medium in which the dissection was performed as well as any unused piece(s) of tissue: they might be useful for an initial flow-cytometric analysis or for archiving DNA and RNA.
-
vi
Swirl the plate to randomize the distribution of the blocks.
-
vii
Take out the six-well plate(s) containing Gelfoam from the incubator (from Step 9) and, in each well, place nine blocks of tissue on top of the Gelfoam, positioning each of them on its largest surface to maximize the contact area between the tissue and the Gelfoam.
-
viii
Return the plate(s) to the incubator for overnight culture or proceed with infection.
Pause point
It is possible to pause the protocol at this stage, before infecting with HIV-1. We prefer performing the infection after an overnight culture to make sure that no bacterial or fungal contamination develops. However, for other pathogens, the best timing for infection might be different.
Timing 30 min per plates of tissue (54 blocks)
-
i
-
B
Lymph nodes
-
i
Wash tissues in PBS and transfer into a 100-mm Petri dish containing 10–20 ml of PBS.
-
ii
Carefully remove the fat tissue surrounding the lymph node.
-
iii
Cut the lymph node into several large pieces, 2–3 pieces per node.
-
iv
Transfer one piece into the cover of a new Petri dish filled with 5 ml of medium, just enough to cover the lid. Cover the Petri dish containing the rest of the tissues to avoid desiccation.
-
v
Remove the capsule surrounding the tissue.
-
vi
Cut the tissue into slices of ∼2 mm thickness. Remove any undesirable tissue; cut the slices into strips of 2 mm width. Then cut the strips into 1-mm blocks. This should result in a size of roughly 2 mm × 2 mm × 1 mm. Cut as many blocks as needed: at least 12 blocks are required per experimental condition. Transfer the blocks into a clean Petri dish containing ECMON.
Critical Step
Keep the medium in which the dissection was performed, as well as any unused pieces of tissue: they might be useful for an initial flow-cytometric analysis or for archiving DNA and RNA.
-
vii
Swirl the plate to randomize the distribution of the blocks.
-
viii
Take out the six-well plate(s) containing Gelfoam from the incubator (from Step 9) and, in each well, place six blocks of tissue on top of the Gelfoam, positioning each of them on its largest surface to maximize the contact area between the tissue and the Gelfoam.
-
ix
Return the plate(s) into the incubator for overnight culture, or proceed with infection.
Pause point
It is possible to pause the protocol at this stage, before infecting with HIV-1. We prefer performing the infection after an overnight culture to make sure that no bacterial or fungal contamination develops. However, for other pathogens, the best timing for infection might be different.
Timing 1 h per node
-
i
-
C
Rectosigmoid (resection)
-
i
Wash tissues several times in PBS containing gentamicin (1 × ) and timentin (1 × ); if fecal matter is present in the tissue, repeat the washes extensively until the tissue takes on a light brown or pink color. Depending on the size of the tissue sample received, cut into 5-cm-long fragments and transfer them into a 150-mm Petri dish containing 30 ml of PBS and antibiotics.
-
ii
Remove the visceral fat surrounding the tissue.
-
iii
Cut the tissue lengthwise and open the lumen.
-
iv
Cut the tissue into strips that are 2 mm wide and 1–2 cm long.
-
v
Transfer several strips into the cover of a new Petri dish filled with 5 ml of medium, just enough to cover the lid. Put the tissue strips on their side and, with a 10-gauge blade scalpel and forceps, separate the mucosa from the muscular layer.
-
vi
Cut the mucosal strips to 8-mm lengths. This should result in tissue blocks with a size of roughly 8 mm × 2 mm × 1 mm. Cut as many blocks as needed to perform the experiment: at least four blocks are required per experimental condition. Transfer the blocks into a clean Petri dish containing ECMON.
Critical Step
Keep the medium in which the dissection was performed as well as any unused pieces of tissue: they might be used for an initial flow-cytometric analysis or for the purpose of archiving DNA and RNA.
-
vii
Swirl the plate to randomize the distribution of the blocks.
-
viii
Take out the 24-well plate(s) containing Gelfoam from the incubator (from Step 9) and, in each well, spread the tissue to maximize the contact area between the tissue and the Gelfoam.
-
ix
Return the plate to the incubator for overnight culture, or proceed with infection.
Pause point
It is possible to pause the protocol at this stage, before infecting with HIV-1. We prefer to perform the infection after an overnight culture to make sure that no bacterial or fungal contamination develops. However, for other pathogens, the best timing for infection might be different.
Timing 1 h per plate of tissue
-
i
-
D
Rectosigmoid biopsies
-
i
Collect biopsies (in RPMI 1640).
-
ii
Within 20–60 min, wash the tissues twice with RPMI 1640.
-
iii
Take out the 24-well plate(s) containing Gelfoam from the incubator (from Step 9) and, in each well, spread the biopsy to maximize the contact area between the tissue and the Gelfoam. At least four wells are required per experimental condition.
-
iv
Return the plate to the incubator for overnight culture, or proceed with infection.
Pause point
It is possible to pause the protocol at this stage, before infecting with HIV-1. We prefer to perform the infection after an overnight culture to make sure that no bacterial or fungal contamination develops. However, for other pathogens, the best timing for infection might be different.
Timing 20 min per 24 biopsies
-
i
-
E
Cervicovaginal tissue
-
i
Wash tissues in PBS and transfer into a 100-mm Petri dish containing 10–20 ml of PBS.
-
ii
Localize the ecto- and endocervix. Cut the cervix away from the rest of the uterus and vagina at the fornix.
-
iii
Cut radial slices 2–3 mm thick.
-
iv
Separate the ecto- and endocervix. In the received cervical samples, the endocervix is readily recognized as the part of the tissue that constitutes the lining of the lumen (it usually has a darker color and is coated by thick mucus). The ectocervix constitutes the vault of the vaginal cavity and has a clearer color.
-
v
Put the ectocervix slices on their sides, and cut away and discard as much muscular tissue as possible, leaving only the mucosal epithelium and the underlying stroma. The thickness of the dissected tissue should be ∼2 mm.
Critical Step
Keep the endocervix and ectocervix separated. They are both valuable tissues but because the endocervix usually continues to produce mucus in culture, this might interfere with subsequent assays. We prefer keeping the endocervix separate and to use it as a source of production of mucus that can be used for other studies.
-
vi
Transfer several strips into the cover of a new Petri dish filled with 5 ml of RPMI, just enough to cover the lid. Cut the strips into 2-mm lengths. This should result in tissue blocks with dimensions of roughly 2 mm × 2 mm × 2 mm. Cut as many blocks as needed to perform the experiment: at least 12 blocks are required per experimental condition (Table 2). Transfer the blocks into a clean Petri dish containing PBS.
Critical Step
Keep the medium in which the dissection was performed as well as any unused pieces of tissue: they might be used for an initial flow-cytometric analysis or for archiving DNA and RNA.
-
vii
Swirl the plate to randomize the distribution of the blocks.
-
viii
Proceed with infection.
Critical Step
Cervical explants are best infected at the time of dissection; therefore, once the desired number of blocks have been cut, they should be infected. We also recommend including an experimental condition in which both the virus and a powerful antiviral drug are combined. This is a useful control to ascertain whether the virus actually replicates rather than being adsorbed and later released by the tissue.
Timing 1.5 h per tissue
-
i
-
A
Ex vivo tissue infection
-
11
Tonsils, lymph nodes and rectosigmoid tissues can be successfully infected by direct deposit of viral suspension on top of each tissue block, whereas cervicovaginal tissue is best infected by soaking in viral suspension. For tonsils, lymph node and rectosigmoid tissue, follow option A; for cervicovaginal tissue, follow option B. These procedures are at present used in our laboratory to infect tissues with HHV-6 (see refs. 13,35), HHV-7 (see ref. 16), HCMV (HHV-5)17, HSV-2 (HHV-2)18, vaccinia virus19, measles virus14,51 and West Nile virus (P. Murphy, unpublished data).
-
A
Direct deposit of pathogen
-
i
If the tissues were dissected the previous night, aspirate the culture medium with a pipette. Then tilt the plate and gently push the Gelfoam back to the high part of each well to allow the medium to gather at the lower part. Aspirate and discard this medium before proceeding from Step 11A(ii). For freshly dissected tissues, start at Step 11A(iii).
-
ii
Add 3 ml of fresh medium to each well.
-
iii
Dilute viral stocks to an appropriate concentration. It is preferable to have a dilution such that the desired inoculum is contained in 5 μl of medium or less.
Critical Step
Volumes larger than 5 μl do not remain on the tissue block and end up diluted in the culture medium shortly after being applied.
-
iv
Pipette 5 μl of the inoculum and delicately deposit this volume on top of each block.
-
v
Let the plate stand under the hood for at least 15 min, and then return it to the incubator until the first medium change, which in our protocol is usually 3 d.
Timing 10 min per plate (54 blocks)
-
i
-
B
Tissue incubation in pathogen suspension
-
i
Prewarm the Thermomixer to 37 °C.
-
ii
Transfer the number of tissue blocks (no more than 15) to be infected into a 1.5-ml Eppendorf conical tube containing 0.5 ml of viral stock diluted appropriately. If more blocks are needed, use several tubes with an equal number of blocks per tube.
-
iii
Transfer the tubes to the 37 °C prewarmed Thermomixer and set mixing to 300 r.p.m.
-
iv
Shake or incubate for 2 h.
-
v
Fill the wells of a 6-well plate (or more if more than six tubes were used for infection) with 3 ml of PBS.
-
vi
Transfer the blocks from each tube to one well, swirl gently with a pipette tip and wait for 1 min.
-
vii
Aspirate the PBS while taking care not to aspirate the blocks.
-
viii
Add 3 ml of PBS, swirl gently with a pipette tip and wait for 1 min.
-
ix
Repeat Steps B(vii) and (viii) three times.
Critical Step
These wash steps are necessary when cervical tissues are used or in cases in which viral replication is not expected to be vigorous and can be masked by carry-over from the viral inoculum.
-
x
Take a 12-well plate out of the incubator and transfer four blocks onto the top of each Gelfoam piece.
-
xi
Return to the incubator until the first medium change.
Timing 3 h
-
i
-
A
Culture of tissues
Timing 20 min per plate
-
12
Three days after the infection, take two aliquots of medium from each of the replicate wells and distribute them into two labeled cryotubes. Repeat for all the experimental conditions.
-
13
With a pipette, aspirate the entire medium from the well, proceeding with one experimental condition at a time. Keep the same pipette for the next step.
-
14
Tilt the tissue culture plate, gently bring the Gelfoam to the top of the well and let the medium flow down to the bottom; aspirate.
-
15
Take a new pipette tip and add an adequate volume of fresh ECM. See Table 2 for the appropriate volume.
-
16
Repeat Steps 13–15 for the remaining experimental conditions.
-
17
Sample and change the medium (Steps 12–16) every 3 d until the end of the experiment: for tonsils and rectosigmoid tissue explants, the experiment will last 12–15 d; for lymph nodes, up to 21 d; and for cervicovaginal tissue, up to 18 d.
Critical Step
Inspect the Gelfoam for quality: if the Gelfoam is digested and the tissue blocks sink into the culture medium and the experiment has to be continued, prepare a new culture plate with new Gelfoam and transfer the dissolved Gelfoam-with-tissue block onto this new Gelfoam.
Pause point
Store samples at −80 °C, until ready to measure viral replication by the appropriate assay.
Digestion and preparation of single-cell suspension for flow cytometry
Timing 30–50 min per plate for collection and processing, and 30 min for tissue digestion
-
18
If the study is limited to cells residing in the tissue blocks, follow option A. If cells that have migrated from the tissue into the Gelfoam are to be studied, follow option B. If migrated cells are to be studied together with the cells remaining in the blocks, follow option C.
-
A
Study of tissue block cells only
-
i
Set a Thermomixer at 37 °C.
-
ii
With forceps, pick up the tissue blocks from the Gelfoam and, into a 1.7-ml Eppendorf tube containing 0.5 ml of RPMI–5% FBS, transfer up to 27 blocks of tonsils or lymph nodes, up to 8 rectosigmoid tissue biopsies or up to 8 cervicovaginal tissue blocks.
-
iii
Thaw as many aliquots of collagenase IV as necessary: one aliquot per two tubes for digestion.
-
iv
Add 500 μl of collagenase IV solution per tube containing the blocks to be digested.
-
v
Place the tubes in the Thermomixer and agitate at 400 r.p.m. for 30 min.
-
vi
Prewet and label one strainer-cap 12 × 75 tube per experimental condition for analysis by addition of 500 μl of PBS.
-
vii
With a pipette, remove 500 μl of medium from the digestion tube and transfer to the appropriate strainer tube.
-
viii
Carefully insert a disposable pellet pestle into the digestion tube and rotate the pestle while pulling it up and down without removing it from the tube. Proceed to two series of 20 rotations.
Caution
This procedure should be executed in a proper biosafety level 3 cabinet with the sash adjusted to the proper height to provide maximum protection to the operator. We do not encourage the use of the cordless motor on infected samples, and its use on noninfected tissue should be considered with caution because of the aerosol produced during this procedure.
-
ix
Transfer the content of the tube to the corresponding prewet strainer-cap tube.
-
x
Rinse the tube with 500 μl of PBS; pass through the strainer.
-
xi
Centrifuge at 400g for 5 min at 16 °C; decant the supernatant.
Caution
To avoid exposure to aerosols, use centrifuge buckets that can be sealed tightly. Load and unload the buckets under a biosafety cabinet.
-
xii
Resuspend the pellet in 1 ml of PBS, centrifuge at 400g for 5 min at 16 °C. Decant the supernatant.
-
xiii
Resuspend the pellet in PBS. The volume of PBS used to resuspend the pellet varies from 0.5 to 1 ml. For 27 tonsil blocks, a volume of 1 ml works well. For cervicovaginal explants, 0.5 ml is adequate for 12 blocks. For rectosigmoid biopsies, 0.5 ml is adequate for eight biopsies.
Timing 20 min sample collection per plate
-
i
-
B
Study of tissue block cells and migrated cells separately
-
i
Remove the tissue blocks from the Gelfoam and prepare cell suspensions as described in Step 18A.
-
ii
Label and prepare as many 50-ml conical tubes with strainer caps as there are experimental conditions.
-
iii
In each culture well, use forceps to squeeze the cells out of the Gelfoam.
-
iv
Strain the cells over the appropriate 50-ml conical tube.
-
v
Transfer the Gelfoam sponge pieces from the corresponding wells and squeeze them on the strainer over the corresponding conical tube.
-
vi
Centrifuge at 400g for 5 min at 16 °C; decant the supernatant.
Caution
To avoid exposure to aerosols, use centrifuge buckets that can be sealed tightly. Load and unload the buckets under a biosafety cabinet.
-
vii
Resuspend the pellet in 1 ml of PBS; centrifuge at 400g for 5 min at 16 °C. Decant the supernatant.
-
viii
Resuspend the pellet in 0.5 ml of PBS.
-
i
-
C
Study of tissue block cells and migrated cells together
-
i
Prepare tissue block cells as described for Steps 18A(i–viii).
-
ii
Strain the cells in a 50-ml conical tube equipped with a 40-μm strainer cap.
-
iii
Rinse the tube with 500 μl of PBS, and pass this rinse through the strainer.
-
iv
Follow Steps 18B(iii–vi) with the same strainer tube used to strain the tissue blocks.
-
v
Resuspend in 1 ml of PBS.
-
i
-
A
Cell surface staining
Timing 1 h for preparing tubes and staining and 1 h for fixation (Step 31A)
-
19
Prepare and label 12 × 75 tubes by adding 50 μl of cell surface antibody mix (previously titered).
Critical Step
You must include fluorescence-minus-one control tubes. These tubes sequentially contain all fluorochromes minus one; they are used to define proper gates and to control the compensation process. A nonstained tube is also required.
-
20
Take an aliquot (50–100 μl) of cell suspension (from Step 18) and keep it on ice.
-
21
Add 1 or 2 μl of Live–Dead fixable blue stain solution (see REAGENTS) to the remaining 500-μl or 1-ml cell suspension, respectively.
-
22
Incubate at room temperature for 15 min.
-
23
Add an equal volume of staining buffer.
-
24
Centrifuge at 400g for 5 min at 16 °C; decant the supernatant.
Caution
To avoid exposure to aerosols, use centrifuge buckets that can be sealed tightly. Load and unload the buckets under a biosafety cabinet.
-
25
Resuspend the pellet in 0.5 or 1 ml of staining buffer as per Step 21.
-
26
Distribute 50-μl aliquots of cells into 12 × 75 FACS tubes containing 50 μl of the various antibody mixes or staining buffer (unstained control).
-
27
Prepare compensation tubes by adding to each tube one drop each of flow cytometry compensation beads (see REAGENTS); add the same amount of each individual antibody used in the staining.
Critical Step
Do not dilute the antibody in the staining buffer; use the bead-staining buffer for this purpose. The presence of mouse antibodies in the mouse serum will prevent binding of the labeled antibodies to the beads.
-
28
Incubate at room temperature for 20 min.
-
29
Add 2 ml of staining buffer to the tubes containing cells to be stained. Add 2 ml of bead buffer to the compensation control bead tubes.
-
30
Centrifuge at 400g for 5 min at 16 °C; decant the supernatant.
-
31
If performing cell surface staining only, follow option A; if performing intracellular staining, follow option B.
-
A
Surface staining
-
i
Add 100 μl of PBS to each tube, including compensation bead control tubes.
-
ii
Vortex gently.
-
iii
Add 100 μl of a 2% (wt/vol) formaldehyde solution in PBS.
-
iv
Vortex gently.
-
v
Incubate at room temperature for 1 h (to inactivate virus).
Timing Fixation 1 h
-
i
-
B
Intracellular staining
-
i
Gently vortex the pellet to separate cell aggregates.
-
ii
Add 100 μl of Fix and Perm solution A to each tube, including compensation beads.
-
iii
Incubate at room temperature for 15 min.
-
iv
Add 3 ml of staining buffer.
-
v
Centrifuge at 400g for 5 min at 16 °C.
-
vi
To the tubes containing cells, add 100 μl of Fix and Perm solution B (see REAGENTS).
-
vii
Add 30 μl of intracellular staining antibody cocktail (previously tittered) and 15 μl of NMS.
-
viii
Incubate at room temperature for 20 min.
-
ix
Add 2 ml of staining buffer.
-
x
Centrifuge at 400g for 5 min at 16 °C; decant the supernatant.
-
xi
Repeat Steps 31B(ix) and (x).
-
xii
Resuspend in 100 μl of PBS; vortex gently.
-
xiii
Add 100 μl of 2% (wt/vol) formaldehyde solution in PBS; vortex.
Timing 50 min
-
i
-
A
-
32
Keep samples in the dark at 4 °C and acquire samples on flow cytometer within 48 h.
-
33
Set up the flow cytometer with adequate quality control using cytometer setup and tracking beads (see REAGENTS) or equivalent if you are not running DIVA 6.0.
Critical Step
If you are using a multi-LASER instrument, verify that the LASER delays are properly set up. This step is often omitted, and an improper setting will ruin your experiment.
-
34
Run and record the appropriate compensation controls and nonstained controls.
-
35
Acquire data for experimental samples.
-
36
Analyze data using Flowjo, Winlist or Diva software, or an equivalent.
Analysis of viral replication and culture media
Timing Depends on the number and type of assays
-
37
Thaw the frozen media samples and perform the assay designed to measure viral replication.
-
38
On the thawed samples, perform the assays designed to measure proteins secreted by the cultured tissues, such as cytokines and chemokines.
Troubleshooting
Troubleshooting advice can be found in Table 3.
Timing
The timing will depend very much on the size of the experiment. The preparation of Gelfoam and culture medium takes 30 min to 1 h for up to four plates of culture. Dissecting tissue blocks is the most time-consuming phase of the work. Allow 3 h for cutting the 342 blocks of tissue that are required to set up three plates of tonsil explants. For lymph nodes, consider dissecting for 1 h per node; for rectosigmoid resection, consider spending 1 h per patient to set up one or two plates of culture. For rectosigmoid biopsies, consider spending 20 min per patient, once the biopsies are collected. Finally, for cervicovaginal tissue, the tissue preparation and dissection take around 1.5 h per patient. Allow an additional hour to set up the blocks on the Gelfoam sponges (10 min per plate). The time required to perform infection is also dependent on the number of plates to infect and the mode of infection. It takes 10 min for a skilled experimenter to infect 54 tissue blocks (one plate of tonsils); for someone with less experience, it will take much longer. Infection by incubation in viral suspension, as for cervicovaginal tissue, takes around 3 h. When working with tissues that do not require immediate infection, such as tonsils, lymph nodes and rectosigmoid tissues, it is possible to pause after the dissection and explants set up since the infection can be performed the following day. In experiments with cervicaovaginal tissue, everything should be done in one phase; count on spending 2.5 h to prepare the Gelfoam plates and dissect the blocks. The infection and washing of the blocks should take an additional 3 h. Setting the blocks on the Gelfoam takes an additional 30 min. Altogether, setting up cervicovaginal tissue will take around 6 h from start to finish. Changing and sampling the medium takes around 20 min per plate. Sample collection and tissue digestion for flow cytometry takes 20 min per plate plus 30 min for digestion and 15 min for straining. Once the cell suspensions are prepared, the whole flow cytometry staining process takes around 3 h from start to finish.
Anticipated results
Tissues cultured for up to 12 d under this protocol should retain their typical cell subset distribution, continue to release cytokines and be able to support infection by HIV-1 or other pathogens of interest without the need to activate cells. Also, they retain their gross cytoarchitecture, although a significant loss of cells is inevitable during long-term culture. Only if the parameters of control tissue are relatively stable can the effect of pathogen infection or other experimental treatment be revealed. Upon culture setup, there is a noticeable egress of cells from the explants. In the case of tonsils, we estimate that in the first 2 d, 60% of the cells have left the tissue blocks, compared with the number of cells present in the tissue blocks at the time of dissection. On average, at day 0, we have ∼1.2 × 105 ± 1.9 × 104 CD4 T cells and 2.25 × 104 ± 3.6 × 103 CD8 T cells per tissue block.
References
Harrison, R. Observations on the living developing nerve fiber. Anat. Rec. 1, (1907).
Harrison, R. The outgrowth of the nerve fiber as a mode of protoplasmic movement. J. Exp. Zool. 9, 787–846 (1910).
Carrel, A. On the permanent life of tissues outside of the organism. J. Exp. Med. 15, 516–528 (1912).
Pantaleo, G. & Fauci, A.S. Tracking HIV during disease progression. Curr. Opin. Immunol. 6, 600–604 (1994).
Pantaleo, G. et al. HIV infection is active and progressive in lymphoid tissue during the clinically latent stage of disease [see comments]. Nature 362, 355–358 (1993).
Fauci, A.S. Host factors in the pathogenesis of HIV disease. Antibiot. Chemother. 48, 4–12 (1996).
Brenchley, J.M. et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat. Med. 12, 1365–1371 (2006).
Brenchley, J.M. et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J. Exp. Med. 200, 749–759 (2004).
Estes, J. et al. Collagen deposition limits immune reconstitution in the gut. J. Infect. Dis. (2008).
Brown, C.R. et al. Unique pathology in simian immunodeficiency virus-infected rapid progressor macaques is consistent with a pathogenesis distinct from that of classical AIDS. J. Virol. 81, 5594–5606 (2007).
Glushakova, S., Baibakov, B., Margolis, L.B. & Zimmerberg, J. Infection of human tonsil histocultures: a model for HIV pathogenesis. Nat. Med. 1, 1320–1322 (1995).
Glushakova, S., Baibakov, B., Zimmerberg, J. & Margolis, L. Experimental HIV infection of human lymphoid tissue: correlation of CD4+ T cell depletion and virus syncytium-inducing/non-syncytium-inducing phenotype in histoculture inoculated with laboratory strains and patient isolates of HIV type 1. AIDS Res. Retroviruses 13, 461–471 (1997).
Grivel, J.C. et al. Suppression of CCR5- but not CXCR4-tropic HIV-1 in lymphoid tissue by human herpesvirus 6. Nat. Med. 7, 1232–1235 (2001).
Condack, C., Grivel, J.C., Devaux, P., Margolis, L. & Cattaneo, R. Measles virus vaccine attenuation: suboptimal infection of lymphatic tissue and tropism alteration. J. Infect. Dis. 196, 541–549 (2007).
Grivel, J.C., Garcia, M., Moss, W. & Margolis, L. Measles virus inhibits HIV-1 replication in human lymphoid tisue ex vivo . J. Inf. Dis. 192, 71–78 (2005).
Lisco, A. et al. Viral interactions in human lymphoid tissue: human herpesvirus 7 suppresses the replication of CCR5-tropic human immunodeficiency virus type 1 via CD4 modulation. J. Virol. 81, 708–717 (2007).
Biancotto, A. et al. Upregulation of human cytomegalovirus by HIV type 1 in human lymphoid tissue ex vivo . AIDS Res. Hum. Retroviruses 24, 453–462 (2008).
Lisco, A. et al. Acyclovir is activated into a HIV-1 reverse transcriptase inhibitor in herpesvirus-infected human tissues. Cell Host Microbe 4, 260–270 (2008).
Vanpouille, C., Biancotto, A., Lisco, A. & Brichacek, B. Interactions between human immunodeficiency virus type 1 and vaccinia virus in human lymphoid tissue ex vivo . J. Virol. 81, 12458–12464 (2007).
Leighton, J. A sponge matrix method for tissue culture; formation of organized aggregates of cells in vitro . J. Natl. Cancer Inst. 12, 545–561 (1951).
Leighton, J. A method for the comparison of the fate of intravascular tumor-cell emboli in vivo and in organ culture. Natl. Cancer Inst. Monogr. 11, 157–195 (1963).
Hoffman, R.M. Three-dimensional histoculture: origins and applications in cancer research. Cancer Cells 3, 86–92 (1991).
Cummins, J.E. Jr . et al. Preclinical testing of candidate topical microbicides for anti-human immunodeficiency virus type 1 activity and tissue toxicity in a human cervical explant culture. Antimicrob. Agents Chemother. 51, 1770–1779 (2007).
Palacio, J. et al. In vitro HIV1 infection of human cervical tissue. Res. Virol. 145, 155–161 (1994).
Shattock, R.J., Griffin, G.E. & Gorodeski, G.I. In vitro models of mucosal HIV transmission. Nat. Med. 6, 607–608 (2000).
Abner, S.R. et al. A human colorectal explant culture to evaluate topical microbicides for the prevention of HIV infection. J. Infect. Dis. 192, 1545–1556 (2005).
Fletcher, P.S. et al. Ex vivo culture of human colorectal tissue for the evaluation of candidate microbicides. AIDS 20, 1237–1245 (2006).
Olbina, G., Miljkovic, D., Hoffman, R.M. & Geller, J. New sensitive discovery histoculture model for growth-inhibition studies in prostate cancer and BPH. Prostate 37, 126–129 (1998).
Grivel, J.C. et al. Human immunodeficiency virus type 1 coreceptor preferences determine target T-cell depletion and cellular tropism in human lymphoid tissue. J. Virol. 74, 5347–5351 (2000).
Grivel, J.C. & Margolis, L.B. CCR5- and CXCR4-tropic HIV-1 are equally cytopathic for their T-cell targets in human lymphoid tissue. Nat. Med. 5, 344–346 (1999).
Grivel, J.C., Malkevitch, N. & Margolis, L. Human immunodeficiency virus type 1 induces apoptosis in CD4(+) but not in CD8(+) T cells in ex vivo-infected human lymphoid tissue. J. Virol. 74, 8077–8084 (2000).
Glushakova, S. et al. Evidence for the HIV-1 phenotype switch as a causal factor in acquired immunodeficiency. Nat. Med. 4, 346–349 (1998).
Lane, H.C., Volkman, D.J., Whalen, G. & Fauci, A.S. In vitro antigen-induced, antigen-specific antibody production in man. Specific and polyclonal components, kinetics, and cellular requirements. J. Exp. Med. 154, 1043–1057 (1981).
Volkman, D.J., Allyn, S.P. & Fauci, A.S. Antigen-induced in vitro antibody production in humans: tetanus toxoid-specific antibody synthesis. J. Immunol. 129, 107–112 (1982).
Grivel, J.C. et al. Pathogenic effects of human herpesvirus 6 in human lymphoid tissue ex vivo . J. Virol. 77, 8280–8289 (2003).
Duray, P.H. et al. Invasion of human tissue ex vivo by Borrelia burgdorferi . J. Infect. Dis. 191, 1747–1754 (2005).
Nelson, C.M., Inman, J.L. & Bissell, M.J. Three-dimensional lithographically defined organotypic tissue arrays for quantitative analysis of morphogenesis and neoplastic progression. Nat. Protoc. 3, 674–678 (2008).
Giese, C. et al. A human lymph node in vitro—challenges and progress. Artif. Organs 30, 803–808 (2006).
Saito, M. et al. Reconstruction of liver organoid using a bioreactor. World J. Gastroenterol. 12, 1881–1888 (2006).
Kim, S.S., Penkala, R. & Abrahimi, P. A perfusion bioreactor for intestinal tissue engineering. J. Surg. Res. 142, 327–331 (2007).
Margolis, L. et al. Long term organ culture of human prostate tissue in a NASA-designed rotating wall bioreactor. J. Urol. 161, 290–297 (1999).
Straub, T.M. et al. In vitro cell culture infectivity assay for human noroviruses. Emerg. Infect. Dis. 13, 396–403 (2007).
Rubart, M. Two-photon microscopy of cells and tissue. Circ. Res. 95, 1154–1166 (2004).
Helmchen, F. & Denk, W. Deep tissue two-photon microscopy. Nat. Methods 2, 932–940 (2005).
Marshall, D. et al. T cell generation including positive and negative selection ex vivo in a three-dimensional matrix. J. Hematother Stem Cell Res. 12, 565–574 (2003).
Geller, J., Sionit, L., Connors, K., Youngkin, T. & Hoffman, R.M. Expression of prostate-specific antigen in human prostate specimens in in vitro three-dimensional histoculture. In Vitro Cell Dev. Biol. Anim. 29A, 523–524 (1993).
Fox-Canale, A.M. et al. Human cytomegalovirus and human immunodeficiency virus type-1 co-infection in human cervical tissue. Virology 369, 55–68 (2007).
Bafica, A., Scanga, C.A., Schito, M., Chaussabel, D. & Sher, A. Influence of coinfecting pathogens on HIV expression: evidence for a role of Toll-like receptors. J. Immunol. 172, 7229–7234 (2004).
Robbins, K.T., Connors, K.M., Storniolo, A.M., Hanchett, C. & Hoffman, R.M. Sponge-gel-supported histoculture drug-response assay for head and neck cancer. Correlations with clinical response to cisplatin. Arch. Otolaryngol. Head Neck Surg. 120, 288–292 (1994).
Chishima, T. et al. Use of histoculture and green fluorescent protein to visualize tumor cell host interaction. In Vitro Cell Dev. Biol. Anim. 33, 745–747 (1997).
Karlsson, I. et al. Differential pathogenesis of primary CCR5-using human immunodeficiency virus type 1 isolates in ex vivo human lymphoid tissue. J. Virol. 79, 11151–11160 (2005).
Grivel, J.C. et al. HIV-1 pathogenesis differs in rectosigmoid and tonsillar tissues infected ex vivo with CCR5- and CXCR4-tropic HIV-1. AIDS 21, 1263–1272 (2007).
Biancotto, A. et al. Abnormal activation and cytokine spectra in lymph nodes of people chronically infected with HIV-1. Blood 109, 4272–4279 (2007).
Perfetto, S.P., Ambrozak, D., Nguyen, R., Chattopadhyay, P. & Roederer, M. Quality assurance for polychromatic flow cytometry. Nat. Protoc. 1, 1522–1530 (2006).
Acknowledgements
We are grateful to the past and present members of the laboratory who contributed to the development of these techniques. These are (in alphabetical order) Massimo Alfano, Naomi Amichay, Boris Baibakov, Angelique Biancotto, Beda Brichacek, Silvia Chen, Cristian Condak, Wendy Fitzgerald, Svetlana Glushakova, Ingrid Karlsson, Rosangela Lima da Gomez, Andrea Lisco, Nina Malkevitch, Lucia Pinto da Silva, Atfa Sassi, Andrew Sylwester, Christophe Vanpouille and Joshua Zimmerberg. This work was supported by the intramural program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grivel, JC., Margolis, L. Use of human tissue explants to study human infectious agents. Nat Protoc 4, 256–269 (2009). https://doi.org/10.1038/nprot.2008.245
Published:
Issue Date:
DOI: https://doi.org/10.1038/nprot.2008.245
This article is cited by
-
Rapid, efficient and activation-neutral gene editing of polyclonal primary human resting CD4+ T cells allows complex functional analyses
Nature Methods (2022)
-
Adenovirus vector vaccination reprograms pulmonary fibroblastic niches to support protective inflating memory CD8+ T cells
Nature Immunology (2021)
-
Labeling and tracking of immune cells in ex vivo human skin
Nature Protocols (2021)
-
Extracellular vesicles from symbiotic vaginal lactobacilli inhibit HIV-1 infection of human tissues
Nature Communications (2019)
-
Reduced Basal Nitric Oxide Production Induces Precancerous Mammary Lesions via ERBB2 and TGFβ
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.