Abstract
Rasd2 is a thyroid hormone target gene, which encodes for a GTP-binding protein enriched in the striatum where, among other functions, it modulates dopaminergic neurotransmission. Here we report that human RASD2 mRNA is abundant in putamen, but it also occurs in the cerebral cortex, with a distinctive expression pattern that differs from that present in rodents. Consistent with its localization, we found that a genetic variation in RASD2 (rs6518956) affects postmortem prefrontal mRNA expression in healthy humans and is associated with phenotypes of relevance to schizophrenia, including prefrontal and striatal grey matter volume and physiology during working memory, as measured with magnetic resonance imaging. Interestingly, quantitative real-time PCR analysis indicated that RASD2 mRNA is slightly reduced in postmortem prefrontal cortex of patients with schizophrenia. In the attempt to uncover the neurobiological substrates associated with Rasd2 activity, we used knockout mice to analyze the in vivo influence of this G-protein on the prepulse inhibition of the startle response and psychotomimetic drug-related behavioral response. Data showed that Rasd2 mutants display deficits in basal prepulse inhibition that, in turn, exacerbate gating disruption under psychotomimetic drug challenge. Furthermore, we documented that lack of Rasd2 strikingly enhances the behavioral sensitivity to motor stimulation elicited by amphetamine and phencyclidine. Based on animal model data, along with the finding that RASD2 influences prefronto-striatal phenotypes in healthy humans, we suggest that genetic mutation or reduced levels of this G-protein might have a role in cerebral circuitry dysfunction underpinning exaggerated psychotomimetic drugs responses and development of specific biological phenotypes linked to schizophrenia.
Similar content being viewed by others
Introduction
Rasd2 (Rhes) is a GTP-binding protein (Falk et al, 1999) highly enriched in the striatum and nucleus accumbens of rodents and developmentally regulated by thyroid hormone activity (Vallortigara et al, 2008, 2009; Vargiu et al, 2001) and by dopamine (DA) innervation in adult rats (Harrison and LaHoste, 2006; Harrison et al, 2008). Rasd2 negatively modulates G protein-coupled receptor-mediated cAMP production (Vargiu et al, 2004). Consistently, targeted deletion of this gene in mice results in increased striatal cAMP/PKA signaling (Errico et al, 2008; Ghiglieri et al, 2015). Besides its well-established expression within striatal GABAergic medium spiny-projecting neurons, we recently demonstrated that Rasd2 is also virtually localized in all cholinergic interneurons in humans and mice, where it affects DA D2R-dependent firing activity and signaling (Sciamanna et al, 2015). On the other hand, Rasd2 is able to modulate AKT and mTOR signaling cascades (Harrison et al, 2013; Subramaniam et al, 2012), well known to be involved in neurological (Lee et al, 2015) and psychiatric disorders (Emamian et al, 2004). Accordingly, the interaction between mTOR and mutant Huntingtin disrupts mTORC1 function and predisposes the striatum to the early degeneration in Huntington’s disease (Lee et al, 2015). On the other hand, alterations of AKT1-GSK3β signaling in schizophrenic patients have identified AKT1 as one of the potential susceptibility genes involved in such a psychiatric disorder (Emamian et al, 2004).
Notably, the human ortholog RASD2 is located on the long arm of chromosome 22 (q12.3), a genomic region harboring several susceptibility loci for psychosis (DeLisi et al, 2002; Potash et al, 2003). This association is most robust in DiGeorge syndrome, which is caused by the deletion of a variable portion of this chromosome and characterized by about 30% increase in incidence of psychosis, as compared with the general population (Jonas et al, 2014).
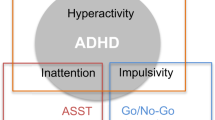
Based on this background, here we tested the hypothesis that Rasd2 may modulate in humans structural and functional prefronto-striatal systems-level phenotypes previously linked with schizophrenia. More specifically, first we evaluated the comparative pattern of fronto-striatal gene expression of Rasd2 in the human and rodent brain. Then, we explored whether RASD2 genetic variation is associated with prefrontal and striatal grey matter (GM) volume and activity during working memory (WM) processing in healthy subjects, as measured with structural and functional MRI. Later, we evaluated whether RASD2 mRNA expression levels as measured by quantitative real-time PCR analysis in postmortem human brain are altered in the prefrontal cortex (PFC) of patients with schizophrenia, when compared with non-psychiatric controls. Finally, in the attempt to uncover the neurobiological substrates linked to the influences of Rasd2, we extended our functional studies from human to rodents. To this aim, we used mutant mice with targeted deletion of Rasd2 (KO), and assessed their sensorimotor gating responses and motor activity, in both basal conditions and under administration of psychotomimetic drugs, such as amphetamine sulfate (Amph) and phencyclidine hydrochloride (PCP).
Materials and Methods
In Situ Hybridization (ISH)
ISH analysis was performed according to protocols previously described (Sciamanna et al, 2015). Mouse fresh brain tissue was embedded in Tissue Tek (Sakura) and frozen at −80 °C, and 14-μm cryostat sections were cut in the coronal plane. Human brain samples from one male (16 years, 16 h postmortem) and one female (35 years, 6 h postmortem), without history of neurological or psychiatric disorders, were dissected in the regions of dorso-lateral PFC (DLPFC) and putamen. Processing was performed as previously described (Pasqualetti et al, 1999). 35S-labelled riboprobes for ISH were as follows: Rasd2, 0.5 Kb (Spano et al, 2004); and RASD2, 2.8 Kb (nucleotides 178–2971, NM_014310.3). Mouse and human hybridized sections were exposed to Biomax MR X-ray films (Kodak) for 2–4 days. Slides with human specimens were dipped in Kodak NTB emulsion for autoradiography and counter-stained with Giemsa, as previously described (Pasqualetti et al, 1999). Sections were examined with brightfield and darkfield light microscopy.
Human Methods
Candidate RASD2 SNPs screening and RASD2 mRNA expression in the postmortem human PFC
Data from 216 brains of non-psychiatric individuals, obtained from BrainCloud (http://braincloud.jhmi.edu) (Turetsky et al, 2007) were analyzed. Samples with age at death <0 (Vargiu et al, 2001) and RNA Integrity Number (RIN) <6 were not included (Supplementary Table S1). We focused on all single-nucleotide polymorphisms (SNPs, n=66) within RASD2 (100 Kb upstream and downstream from the gene) available for this data set, and we explored their association with prefrontal RASD2 mRNA expression using Bonferroni correction for the number of independent comparisons to correct for Type I errors. We selected RASD2 intragenic SNPs—rs5750112 (UTRvariant-5′), rs6518956 (intron-variant), rs2281122 (intron-variant), rs8137058 (intron-variant), rs736211 (UTR-variant-3′), rs736210 (UTR-variant-3′)—as independent comparisons, as these SNPs may alter the rate of RASD2 mRNA expression through different mechanisms (Consortium EP, 2012). One SNP, rs6518956, survived the statistical threshold and was selected for the in vivo imaging analyses.
Prefrontal GM volume and prefrontal–striatal physiology in healthy humans
Healthy Caucasian volunteers from the region of Puglia, Italy were genotyped for rs6518956 (see Supplementary Tables S2 and S3) and underwent the imaging protocols. All analyses were performed in Statistical Parametric Mapping 8.0 (http://www.fil.ion.ucl.ac.uk/spm) with SNP effects assessed with random-effects analyses. For the evaluation of prefrontal and striatal GM volume (n=150), we used voxel-based morphometry (VBM) performed on 3 T structural MRI images, following standardized methods (New segmentation and Diffeomorphic registration algorithms) and using appropriate covariates as described previously (Martino et al, 2011) (see Supplementary Information). For WM cortical and subcortical activity (n=160), we analyzed 3 T BOLD fMRI prefrontal and striatal physiology during performance of the 1- and 2-Back WM task (N-Back). Statistical correction for multiple comparisons within the a priori defined regions of interest (ROIs) was performed as appropriate, respectively, for VBM and fMRI data (see Supplementary Materials and Methods).
Postmortem PFC samples
Samples of postmortem PFC from patients with schizophrenia and non-psychiatric controls were obtained from the Neurodegenerative Diseases Brain Bank (King’s College London, UK). All tissue collection and processing was carried out under the regulations and licences of the Human Tissue Authority and in accordance with the Human Tissue Act of 2004. Clinical diagnosis of the samples was performed according to Diagnostic and Statistical Manual of Mental Disorders (DSMIII-R). Demographic characteristics of the samples are described in Table 1. Student’s t-test analysis was performed in order to determine whether sample characteristics (age, postmortem interval (PMI) and RIN) were comparable in the two diagnostic groups. Total RNAs extraction from PFC samples and quantitative RT-PCR protocols are described in Supplementary Information.
Animal Methods
Ten-to-12-week-old male and female wild-type (WT) and Rasd2 knockout (KO) mice without PGK-neo cassette (Ghiglieri et al, 2015; Sciamanna et al, 2015), derived from mating of heterozygous animals (Rasd2+/−), back-crossed to F11 generation to C57BL/6J strain, were used in this study. Mice were housed in groups in standard cages (29 × 17.5 × 12.5 cm3) at constant temperature (22±1 °C) and maintained on a 12/12 h light/dark cycle, with food and water ad libitum. Experiments were performed in conformity with protocols approved by the veterinary department of the Italian Ministry of Health and in accordance to the ethical and safety rules and guidelines for the use of animals in biomedical research provided by the relevant Italian laws and European Union’s directives (no. 86/609/EC). All efforts were made to minimize the animal’s suffering.
Drugs
Amph, haloperidol (Hal), and PCP were obtained from Sigma (St Louis, MO). Clozapine (Clz) was obtained from RBI (Natick, MA). Amph and PCP were dissolved in saline (0.9% NaCl). Hal was dissolved in a vehicle (Veh) composed by 10% acetic acid in saline solution. The pH was brought to 6.0 with 1 M NaOH. Clz was dissolved in a Veh composed by a solution of 2% dimethyl sulfoxide (DMSO) in saline. All drugs were administered intraperitoneally (i.p.) in a volume of 10 ml/kg.
Behavior
Prepulse inhibition (PPI) of the startle reflex. Different cohorts of animals were tested at baseline or after drug injection for PPI of the acoustic startle response, measured using the SR-Lab System (San Diego Instruments, San Diego, CA, USA). The protocol has been previously described (Errico et al, 2008). Briefly, WT and KO naïve mice were enrolled to test baseline PPI response in males and females (see Supplementary Figure S1). Whereas another cohort of male animals was divided into the following groups: Amph (10 mg/kg) or Veh, administered 5 min before starting the test session; PCP (10 mg/kg) or Veh, administered 10 min prior to the start of the test session; Hal (3 mg/kg) or Veh, injected 30 min before starting the test session; Hal (3 mg/kg) or Veh, injected 25 min before administration of 10 mg/kg Amph or Veh, and tested 5 min later; Clz (3 mg/kg) or Veh, injected 20 min before starting the test session; and Clz (3 mg/kg) or vehicle, injected 10 min before PCP treatment (10 mg/kg) or Veh, and tested 10 min later. The background noise level was 65 dB, and we chose to test 70, 74, and 78 dB prepulse sound levels corresponding to 5, 9, and 13 dB above background, respectively. Sound levels, expressed as dB(A) sound pressure levels, were measured as previously described (Swerdlow and Geyer, 1998). PPI was calculated as percentage (%) and used as a dependent variable with prepulse sound levels as repeated measure. Baseline PPI was analyzed by two-way ANOVA (genotype × prepulse sound levels) with prepulse sound levels as repeated measure. Effects of Amph or PCP at different doses, as well as those of Hal or Clz in preventing Amph- and PCP-induced PPI disruption, respectively, were analyzed by three-way ANOVA (genotype × treatment × prepulse sound levels) with prepulse sound levels as dependent variable. Effects of Hal or Clz alone were analyzed within genotypes by two-way ANOVA (treatment × prepulse sound levels) with prepulse as dependent variable. Startle magnitude was calculated as the average response (±SEM) to the startle trials (120 dB alone) presented during the test session.
Novelty-induced exploration. Novelty-induced exploratory response was used to assess spontaneous motor function in mice, as previously described (Errico et al, 2008). Locomotor activity (expressed in cm) was recorded by using a computerized video tracking system (Videotrack, Viewpoint S.A., Champagne au Mont d’Or, France). Two-way ANOVA (genotype × time) with repeated measures and Student’s t-test were used to analyze in basal condition the time course of motor activity and the total motor activity, respectively.
Motor responses induced by drugs. Amph- and PCP-induced locomotor hyperactivity was induced according to a previous protocol (Napolitano et al, 2010; Usiello et al, 2000). Briefly, WT and KO male animals were randomly assigned to the Amph (free base 1.25, 2.5 mg/kg), PCP (3.0, 6.0 mg/kg) or specific Veh-treated groups, habituated to the experimental cage (35 × 25 × 30 cm3) for 60 min, injected with drug or Veh, and replaced in the same cage. We also analyzed WT and KO female mice for motor activity following Amph (free base 1.25 mg/kg) and PCP (3.0 mg/kg) or Veh administration (Supplementary Figure S2). The horizontal motor activity was evaluated during 10-min intervals over a 1-h test session through a computerized video tracking system (Videotrack, Viewpoint S.A.). Three-way ANOVA (genotype × treatment × time) with time as repeated measures was used to analyze the time course of motor activity. Two-way ANOVA (genotype × treatment) was used to analyze locomotor activity over 60-min test session. Total motor activity was analyzed by two-way ANOVA, followed by Fisher’s post-hoc comparison.
Results
Rasd2 mRNA Expression in the Human Putamen and Cerebral Cortex
Here, we first confirmed a consistent Rasd2 mRNA expression in the mouse striatum (Errico et al, 2008; Ghiglieri et al, 2015; Vargiu et al, 2001) (Figure 1a), and extended our study of Rasd2 gene expression pattern to the human brain, where we reported a highly enriched RASD2 mRNA expression in the putamen but not in the surrounding brain regions, such as globus pallidus and claustrum (Figure 1e–g). Moreover, consistent with previous findings in rodents (Vargiu et al, 2001), we found scattered Rasd2 mRNA-positive neurons distributed throughout the cortical layers, with an autoradiographic signal that appeared higher in layers (L) II–III than in deeper ones (Figure 1a and b). Conversely, RASD2 mRNA expression in humans, although detected throughout layers II–VI, showed a distinctive expression in layer V, not seen in rodents (Figure 1h–k). Interestingly, higher magnification analysis of silver grain distribution in the DLPFC showed that medium and large pyramidal-like neurons were labeled (Figure 1k, inset).
RASD2 mRNA is expressed in the putamen and in the dorso-lateral prefrontal cortex of human brain. (a–d) Radioactive ISH experiment on coronal sections of mouse brain showing Rasd2 expression in the striatum and in the cerebral cortex. (b) High magnification image of the boxed region in panel (a) showing Rasd2 mRNA distribution across cortical layers of the mouse brain. Autoradiographic signal appears higher in layers II/III as compared with deeper layers. (c, d) RNAse-treated control section and relative high magnification showing any detectable specific signal. (e–g) Nissl staining (e) and ISH autoradiographic analysis at low (f) and high (g) magnification on sections from the postmortem human brain showing expression of RASD2 in the putamen nucleus. (h–k) Nissl staining (h, j) and ISH autoradiography (i, k) of sections from the postmortem human brain highlighting the presence of RASD2 expression in the dorso-lateral prefrontal cortex with a strong autoradiographic signal in layer V. (j, k) Nissl staining (j) and darkfield photomicrograph (k) of boxed regions in panels (h) and (i) showing the layering of human prefrontal cortex and the distribution of RASD2 mRNA, respectively. Labeled neurons appear distributed across layers II–VI, with pyramidal neurons (arrows) of layer V showing a higher density of autoradiographic silver grains (see inset in panel (k)). Cl, claustrum; Gp, globus pallidus; Pu, putamen nucleus.
RASD2 is Associated with Prefrontal GM Volume As Well As Prefrontal and Striatal Activity During WM in Humans
We examined the association between functional variations in the RASD2 gene and a series of human imaging phenotypes related to schizophrenia. The first step was to determine which specific RASD2 genetic variants affected mRNA expression in postmortem PFC of non-psychiatric human subjects. Separate ANCOVAs on RASD2 mRNA expression as the dependent variable and RASD2 SNPs and race as predictors indicated that rs6518956 (G/A) within RASD2 is significantly associated with prefrontal RASD2 mRNA expression (F(2,205)=5.03, p=0.04, after Bonferroni correction). More specifically, greater RASD2 mRNA expression was predicted by GG genotype (Fisher’s post-hoc vs AG p=0.009; vs AA p=0.003) (Figure 2a). Age at death, gender, PMI, pH, and RIN were entered into the statistical model as covariates of no interest. We further investigated the in vivo association of rs6518956 with prefrontal and striatal GM volume. VBM results in healthy Caucasian subjects demonstrated a main effect of rs6518956 in the left middle frontal gyrus (x −32, y −0, z 51, k=362, Z=3.49, p=0.03 non-stationary cluster-level-corrected) (Figure 2b). In particular, the GG genotype is associated with greater prefrontal GM volume compared with the other two genotype groups (Fisher’s post-hoc vs. AG p=0.001; vs AA p=0.003). rs6518956 was not significantly associated with striatal (putamen/caudate) GM volume. Then we examined the association of rs6518956 with BOLD-fMRI brain activity of healthy Caucasian individuals during performance of the 1- and 2-Back WM task. There was no effect of genotype or interaction with WM load on behavioral performance (all p>0.2). Thus the effect of genotype on brain responses during WM processing in this sample reflected how the brain processed WM and not how individuals scored on the task. Results of the fMRI analyses indicated a main effect of rs6518956 on BOLD signal change in left middle frontal gyrus (x −34, y 0, z 42; k=110; Z=3.93; p=0.035 FWE-corrected) (Figure 2c*), with GG subjects showing greater prefrontal activity compared with GA and AA individuals (post-hoc: vs AG p=0.00007; vs AA p=0.004). fMRI results also demonstrated a RASD2 by WM load interaction in the left putamen (x −26, y 12, z 10; k=243; Z=3.88; p=0.041 FWE-corrected) (Figure 2c**). More specifically, post-hoc analysis with t-test for dependent samples of BOLD response from this cluster indicated that GG and AA subjects have greater striatal activity compared with GA individuals and that this effect is more evident at 2-Back (1-Back vs 2-Back: AA, p=0.02; AG, p=0.11; GG, p=0.007). To address whether functional results in PFC might be related to structural differences among the three RASD2 genotype subgroups, we also performed a Pearson’s test between GM and BOLD signal change in the ROIs in a subgroup of 120 subjects (35 AA, 63 AG, 22 GG) who had both structural and functional scans. Results did not show any significant correlation between GM volume and BOLD signal change both in the entire sample of healthy subjects (r=0.1, p=0.27) and within the three different RASD2 genotype subgroups (35 AA: r=−0.05, p=0.74; 63 AG: r=0.06, p=0.59; 22 GG: r=−0.0009, p=0.99, results not shown), suggesting that rs6518956 modulation of prefrontal activity during WM is not driven by local structural differences. Moreover, we did not find any relationship between prefrontal GM volume (in the same cluster as above) and striatal activity (extracted from the contrast showing RASD2 rs6518956 by WM load interaction in putamen: x −26, y 12, z 10; k=243), both in the entire sample of healthy subjects (r=−0.07, p=0.41) and within the three RASD2 genotype subgroups (AA, r=−0.18, p=0.29; AG, r=−0.05, p=0.64; GG, r=−0.33, p=0.12, results not shown).
Association of RASD2 rs6518956 with prefrontal and striatal phenotypes in healthy humans. (a) Association of RASD2 rs6518956 with RASD2 mRNA expression levels in the human postmortem prefrontal cortex. Graph depicts normalized log2 ratios (sample/reference). Data from http://braincloud.jhmi.edu/. Error bars indicate SE. (b) Association of RASD2 rs6518956 with prefrontal grey matter volume in healthy Caucasian subjects. Left panel: 3-Dimensional rendering of the cluster in prefrontal cortex associated with a main effect of RASD2 rs6518956. Image thresholded at p<0.005, non-stationary cluster extend corrected. Right panel: Graph showing mean±SE of grey matter content extracted from the cluster depicted in the left panel. (c*, c**) Association of RASD2 rs6518956 with prefrontal and striatal BOLD response during working memory in healthy Caucasian subjects: (c*) Upper panel: 3-Dimensional rendering of the cluster in the prefrontal cortex associated with a main effect of RASD2 rs6518956. Image thresholded at p<0.05, FWE corrected. Lower panel: Graph showing mean±SE of parameter estimated extracted from the cluster depicted in the upper panel. (c**) Upper panel: Coronal section of the interaction between RASD2 and WM load in left putamen. Image thresholded at p<0.05, FWE corrected. Lower panel: Graph showing mean±SE of parameter estimated extracted from the cluster depicted in the upper panel.
RASD2 mRNA Expression in the Postmortem Brains of Patients with Schizophrenia
Based on its cortical localization and considering the potential involvement of RASD2 in prefrontal phenotypes that might be of relevance to psychiatric disorders, we then assessed whether the mRNA expression levels of this GTPase might be altered in the postmortem PFC from patients with schizophrenia. Quantitative real-time PCR analysis revealed an average 30% reduction of RASD2 transcript in patients with schizophrenia, when compared with controls, although not statistically significant (ANCOVA with diagnosis as predictor and PMI as covariate of no interest; PFC: F(1,17)=1.429, p=0.2483, Cohen’s d=0.44; Figure 3).
RASD2 mRNA expression in postmortem samples from patients with schizophrenia and non-psychiatric controls (n=10 SCZ, n=12 NC). All studies were performed by quantitative reverse transcription-PCR. Quantity means of transcript were normalized to the geometric mean of three housekeeping genes. All values are expressed as mean±SEM.
Rasd2 Modulates Sensorimotor Gating
In order to assess the influence of Rasd2 in modulating sensorimotor gating, known to be altered in patients and in preclinical model of schizophrenia (Braff et al, 2001), we analyzed the PPI of the acoustic startle reflex under basal conditions in Rasd2 KO male mice (n=15/genotype). Statistical analysis showed a significant PPI reduction in mutants compared with control littermates (two-way ANOVA with prepulse sound levels as repeated measures: genotype effect, F(1,56)=4.968, p=0.0340; Figure 4a). Differently from what observed in males, we failed to find any PPI alteration in female KO mice (Supplementary Figure S1). Then, to investigate whether Rasd2 deletion may affect the sensitivity of the disruptive effect induced by the DA-releaser Amph on PPI, we tested this drug at the doses of 5 (n=9/genotype), 7.5 (n=10/genotype), and 10 mg/kg (n=24/genotype) or vehicle (n=30 WT, n=32 KO). Three-way ANOVA showed an overall significant effect of genotype (F(1,280)=10.351, p=0.0016) and treatment (F(3,280)=5.441, p=0.0014), but no genotype × treatment interaction (F(3,280)=0.258, p=0.8558) or genotype × treatment × prepulse levels interaction (F(6,280)=0.834, p=0.5448) (Figure 4b).
Evaluation of PPI in drug-free and psychotomimetic-treated Rasd2 mutant mice. (a) Baseline PPI in naïve Rasd2 mutant and control mice (n=15/genotype). (b) PPI in mice treated with 5 mg/kg (n=9/genotype), 7.5 mg/kg (n=10/genotype), and 10 mg/kg (n=24/genotype) Amph or Veh (WT, n=30; KO, n=32). (c) PPI values for 5 mg/kg (n=10/genotype) and 10 mg/kg (WT, n=18; KO, n=20) PCP or Veh (WT, n=30; KO, n=32) treatment. (d) Effect of 3 mg/kg Hal (n=9/genotype) on PPI in KO and WT mice. Veh-treated group (n=11/genotype) was used as control. (e) PPI response in mice treated with 3 mg/kg Hal plus 10 mg/kg Amph (WT, n=8; KO, n=9), 10 mg/kg Amph (WT, n=14; KO, n=16) or Veh (WT, n=13; KO, n=12). (f) Effect of 3 mg/kg Clz (n=10/genotype) on PPI in KO and WT mice. Veh-treated group (n=10/genotype) was used as control. (g) PPI response in mice treated with 3 mg/kg Clz plus 10 mg/kg PCP (WT, n=10; KO, n=12), 10 mg/kg PCP (n=10/genotype), or Veh (WT, n=9; KO, n=10). PPI was measured at three different prepulse intensities (5, 9, and 13 dB(A) above background). Percentage of the PPI was used as a dependent variable. All values are expressed as the mean±SEM. Genotypes and treatment are as indicated.
Further, we evaluated the involvement of Rasd2 in regulating the severity of PPI disruption in mice treated with the NMDAR antagonist PCP, also known to promote striatal DA release (Javitt, 2007; Svensson, 2000). Here, we tested this hallucinogenic at the doses of 5 (n=10/genotype) and 10 (n=18 WT, n=20 KO) mg/kg or vehicle (n=30 WT, n=32 KO). Three-way ANOVA showed a significant genotype (F(1,228)=9.339, p=0.0028) and treatment (F(2,228)=8.527, p=0.0004) effect, with no effect of genotype × treatment interaction (F(2,228)=0.206, p=0.8140). Notably, we found a trend, although not significant, towards a genotype × treatment × prepulse interaction (F(4,228)=2.361, p=0.0541; Figure 4c).
Hal and Clz Prevent Amph- and PCP-Induced PPI Deficits in Rasd2 Knockouts
Later, we evaluated the ability of the antipsychotics Hal or Clz to prevent the prominent sensorimotor gating deficits induced in mutants by high doses of Amph or PCP, respectively. When administered at the dose of 3 mg/kg, Hal failed to induce any significant effect on PPI responses both in KO and WT mice (Hal, n=9/genotype; Veh, n=11/genotype), as indicated by the two-way ANOVA with prepulse sound levels as repeated measure (WT: F(1,36)=0.394, p=0.5381; KO: F(1,36)=0.012, p=0.9123; Figure 4d). On the other hand, pretreatment with 3 mg/kg Hal fully prevented the PPI deficits induced by Amph administration in both genotypes (Hal+Amph, n=8 WT, n=9 KO; Veh, n=13 WT, n=12 KO). Accordingly, the three-way ANOVA indicated no significant treatment effect (Veh vs Hal/Amph: F(1,76)=0.027, p=0.8701) and no significant genotype × treatment interaction (F(1,76)=0.128, p=0.7222; Figure 4e). Conversely, Amph at 10 mg/kg (n=14 WT, n=16 KO), as expected, triggered a significant PPI disruption in both genotypes (Veh vs Amph: F(1,102)=20.555, p<0.0001).
Administration of 3 mg/kg Clz alone failed to cause any significant effect on PPI in both genotypes, compared with their respective Veh-treated group (n=10/genotype and treatment), as indicated by the two-way ANOVA with prepulse sound levels as repeated measure (WT: F(1,36)=0.546, p=0.4696; KO: F(1,36)=0.055, p=0.8166; Figure 4f). However, pretreatment with 3 mg/kg Clz, both in mutant and control mice, completely prevented the PPI deficits induced by PCP (Clz+PCP, n=10 WT, n=12 KO; PCP, n=10/genotype, Veh, n=9 WT, n=10 KO), as revealed by the three-way ANOVA (Veh vs Clz/PCP: F(1,74)=1.744, p=0.1947; genotype × treatment: F(1,74)=0.717, p=0.4026), which alone caused severe sensorimotor gating alteration (three-way ANOVA, Veh vs PCP, F(1,70)=24.442, p<0.0001; Figure 4g).
Lack of Rasd2 Triggers Greater Sensitivity to Amph- and PCP-Induced Motor Stimulation in Mice
Here, we aimed at exploring the involvement of Rasd2 deletion in stimulating motor effects elicited by the DA-releaser Amph and the NMDAR antagonist PCP. In this regard, we first measured the basal motor activity in mutants, compared with controls (n=10/genotype). Two-way ANOVA, with time as repeated measure, indicated that both naïve WT and KO animals display comparable locomotion and habituation profile to the novel cage (genotype effect: F(1,90)=0.235, p=0.6339; genotype × time: F(5,90)=0.262, p=0.9325; time effect: F(5,90)=17.086, p<0.0001; Figure 5a). Then, we assessed the effect of Amph on motor activity at the doses of 1.25 and 2.5 mg/kg (n=12/genotype and treatment) or vehicle (n=14/genotype). Statistical analysis showed that Amph produces differential motor effects in the two genotypes along the test session, as indicated by the three-way ANOVA with time as repeated measure (genotype × treatment, F(2,350)=7.503, p=0.0011; Figure 5b). The genotype × treatment interaction was also confirmed by total locomotor activity measured in KO and WT Amph-treated animals, when compared with their matched-vehicle groups (two-way ANOVA: genotype × treatment, F(2,70)=7.503, p<0.01; Figure 5b′). Analysis at each dose showed that 1.25 mg/kg Amph evokes substantial motor hyperactivity in KO but not in WT animals, compared with their respective Veh-treated groups (three-way ANOVA, genotype × treatment interaction: F(1,250)=17.713, p=0.0001; two-way ANOVA, treatment effect, WT: F(1,125)=0.014, p=0.9064; KO: F(1,125)=18.151, p=0.0003). On the other hand, 2.5 mg/kg Amph administration similarly enhanced horizontal motor activity in both genotypes, compared with their respective Veh-treated groups (three-way ANOVA, treatment effect: F(1,240)=49.109, p<0.0001; genotype × treatment: F(1,240)=1.084, p=0.3030). Then, we evaluated the influence of Rasd2 on hyperlocomotion induced by the NMDAR antagonist PCP at the doses of 3 (n=7/genotype) and 6 (n=7/genotype) mg/kg or vehicle (n=12 WT, n=10 KO). Similar to Amph treatment, PCP triggered a different motor stimulation between genotypes, as indicated by the three-way ANOVA with time as repeated measure (genotype × treatment, F(2,220)=3.957, p=0.0263) (Figure 5c). In particular, administration of a low dose of PCP (3 mg/kg) produced motor hyperactivity only in KO mice, compared with Veh-treated animals. Accordingly, our data indicated a significant genotype × treatment interaction (three-way ANOVA F(1,155)=8.172 p=0.0075; two-way ANOVA, treatment effect, WT: F(1,80)=0.068, p=0.7980; KO: F(1,75)=25.517, p=0.0001). Moreover, administration of 6 mg/kg PCP increased horizontal locomotion in both genotypes, compared with the Veh-treated group, although with a higher magnitude in KOs (three-way ANOVA, treatment effect: F(1,155)=77.308, p<0.0001; genotype × treatment interaction: F(1,155)=5.674, p=0.0235). The differential motor effect of PCP between genotypes is also indicated by a significant difference in total distance travelled, as shown by the two-way ANOVA (genotype × treatment, F(2,44)=3.957 p<0.05; Figure 5c′). As seen in male mutants, we also found in female KOs a greater hyperlocomotion induced either by Amph or PCP (Supplementary Figure S2).
Amphetamine and PCP trigger motor stimulation in mice. (a, a’) Basal motor activity in naïve WT and KO mice (n=10/per genotype). (b, b’) Horizontal motor activity induced by administration of 1.25 mg/kg Amph (n=12/genotype) and 2.5 mg/kg Amph (n=12/genotype) or Veh (n=14/genotype). (c, c’) Locomotor activity induced by 3.0 mg/kg PCP (n=7/genotype) and 6.0 mg/kg PCP (n=7/genotype) or Veh (WT, n=12; KO, n=10) administration. Locomotion is expressed as distance travelled (cm), measured every 10 min over a 60-min test session (a–c) and as total motor activity (a’–c’). All values are expressed as mean±SEM. **p<0.01, ***p<0.0001 vs Veh-treated group within genotype. Genotypes and treatments are as indicated.
Discussion
It is documented that Rasd2 is developmentally regulated by thyroid hormone (Manzano et al, 2003). Accordingly, hypothyroid rodents display a significant reduction of striatal Rasd2 mRNA expression, restored by T3 administration (Vallortigara et al, 2008; Vargiu et al, 2001). Importantly, this transcriptional regulation is most likely mediated by thyroid receptor α (TRα) as, differently from what observed in TRα knockout mice, T3 supplementation induces an upregulation of Rasd2 mRNA in hypothyroid TRβ mutants (Vallortigara et al, 2008). Rasd2 encodes for a small GTP-binding protein highly expressed in the striatum and nucleus accumbens of rodents (Errico et al, 2008; Vargiu et al, 2004), where it affects neuronal processes associated with cAMP/PKA and AKT signaling transduction cascades (Ghiglieri et al, 2015; Harrison and Lahoste, 2013). Furthermore, Rasd2 also influences DA D1R- and D2R-related processes within striatal GABAergic projection neurons and cholinergic interneurons (Errico et al, 2008; Ghiglieri et al, 2015; Sciamanna et al, 2015). On the other hand, recent studies have suggested that Rasd2, through SUMO and mTOR pathway regulation, has a pivotal role in the genesis of neurological disorders involving the striatum, such as Huntington’s disease (Lee et al, 2015; Subramaniam et al, 2010) and L-DOPA-induced dyskinesia (Subramaniam et al, 2012).
In the present study, we documented not only that RASD2 mRNA is highly expressed in human putamen but also, even more interestingly, we found for the first time its expression throughout layers II–VI of PFC, with stronger levels in pyramidal neurons of layer V, not found in the rodent brain. Layer V pyramidal neurons of the DLPFC are involved in WM processing (Goldman-Rakic, 1995), and their dysfunction has been reported in patients with schizophrenia. Although further studies are required, we cannot exclude that the prominent localization of RASD2 mRNA in human layer V pyramidal neurons might suggest a modulatory role of this GTPase on neuronal activity within this cortical layer.
Furthermore, in line with its neuroanatomical localization, our imaging findings also provide evidence for a role of RASD2 in modulating prefrontal and striatal phenotypes in humans. Consistently, a non-coding variation in the RASD2 gene (rs6518956), which affects RASD2 mRNA levels in human prefrontal postmortem tissue, also predicts in vivo phenotypes of prefrontal GM volume, as well as prefrontal and striatal activity during WM processing in healthy subjects. Our results also indicate that the GG genotype of rs6518956 is associated with greater prefrontal RASD2 mRNA expression relative to the A allele, and suggest a functional role of this SNP on modulation of prefrontal RASD2 protein levels. Consistently, the GG genotype also predicts greater prefrontal GM volume relative to the AG and AA genotypes in healthy individuals, thus leading to the hypothesis that RASD2 may be implicated in prefrontal plasticity, likely through the modulation of key neurodevelopmental pathways, such as AKT1 and mTOR (Costa-Mattioli and Monteggia, 2013; Tan et al, 2008). Surprisingly, we did not find any effect of rs6518956 on striatal (putamen/caudate) GM volume. One speculation is that this SNP, which was selected on the basis of its association with prefrontal mRNA expression, affects primarily GM volume in the cortex, as also supported by results of the uncorrected whole brain exploratory analysis (Supplementary Table S4). Additional studies on postmortem striatal tissues of healthy humans might elucidate the importance of rs6518956 in modulating RASD2 mRNA in this region.
Furthermore, in spite of similar WM performance, our fMRI results indicate that the GG genotype is associated with greater PFC activity during WM relative to AG and AA genotypes in healthy subjects, and that this effect is not driven by local structural differences. These findings suggest that GG subjects are inefficient in performing the WM task, because they need to recruit more neural resources to achieve a similar level of performance. Interestingly, RASD2 by WM load interaction was found in putamen such that both homozygous genotypes have greater activity at 2-Back. One possible explanation is that rs6518956 effect on putamen activity only becomes manifest when greater putamen engagement is required by the more difficult task (2-Back), which might require additional neuronal resources beyond PFC. This interpretation is consistent with the results of the association in prefrontal activity, which is instead manifest at both 1- and 2-Back. Further studies are warranted to investigate how RASD2 genetic variation interacts with diagnosis of schizophrenia in affecting imaging phenotypes related to the disorder.
Quantitative real-time PCR studies in the postmortem PFC of patients with schizophrenia indicate a mild reduction of prefrontal RASD2 mRNA, when compared with non-psychiatric controls. However, given the small number of brain samples here analyzed, future studies are necessary to establish ‘whether’ and ‘to which extent’ changes in prefrontal RASD2 mRNA expression occur in patients with schizophrenia.
Modeling endophenotypes of psychiatric disorders in animal models represents a preclinical approach helpful to shed light on the pathophysiology of these disorders in humans (Jones et al, 2011). Within this framework, the PPI of the startle reflex is one of the most frequently used cross-species paradigm to evaluate the sensorimotor gating response, known to be disrupted in schizophrenia, and proposed as a candidate neurophysiological endophenotype of this psychiatric disorder (Gottesmann, 2003). In line with the evidence that psychotomimetic drugs, such as Amph and PCP, trigger PPI deficits in both animals and humans, administration of these drugs represents the most widely validated experimental strategy to model schizophrenia-like symptoms in rodents (Braff et al, 2001; Brisch et al, 2014; Gargiulo and Landa De Gargiulo, 2014; Jones et al, 2011). Based on this consideration, in the attempt to move Rasd2 functional characterization from human to mouse, we evaluated whether lack of this GTPase in mutants influences sensorimotor gating responses in drug-free condition and after Amph or PCP treatment.
Considering the pivotal role of DA system in regulating PPI response (Braff et al, 2001), and coherently with an involvement of Rasd2 in the modulation of this neurotransmission (Errico et al, 2008; Harrison and LaHoste, 2006; Sciamanna et al, 2015), our behavioral data indicate that targeted deletion of this gene induces significant sensorimotor gating deficits in naïve male mutants. Moreover, we also documented that administration of both Amph and PCP triggers prominent PPI deficits in mutants, when compared with their matched-treated controls. Nevertheless, in light of the significant basal sensorimotor gating disturbance of naïve mutants, we argue that the greater PPI alterations found in treated knockouts are most likely due to an additive effect of the drugs, rather than to a different sensitivity of the genotypes to Amph and PCP. In line with this interpretation, we failed to find in KO mice a significant left-shift in the dose–response curve of psychotomimetic drug-induced PPI deficits.
Pharmacological and genetic studies in mice have indicated a consistent role of striatal DA transmission at D2 receptor (D2R) sites in regulating sensorimotor gating responses (Mansbach et al, 1988; Ralph et al, 2001; Xu et al, 2002). In agreement with these findings, we argue that defective basal gating processes, along with the exacerbated magnitude of psychotomimetic drug-induced PPI deficits found in Rasd2 mutants, might be linked to an altered striatal transmission.
Consistently, pretreatment with the DAergic D2R antagonist Hal in Rasd2 knockouts completely prevents the dramatic PPI alterations triggered by high dose of Amph.
On the other hand, the finding that Clz prevented the PPI deficits seen in PCP-treated KO mice is consistent with the pharmacodynamic profile of Clz, which binds to D2R and blocks 5HT2A receptors with high affinity, thus preventing further dopamine release within the striatum (Seeman, 2014; Vauquelin et al, 2012). However, as Clz is a broad-spectrum ligand (Wenthur et al, 2014), at present its specific mechanism of action in Rasd2 KOs is still unclear. One possibility is that Clz could normalize DAergic-mediated signaling in these mice, thereby preventing their abnormal gating disturbances.
Intriguingly, despite normal spontaneous locomotion, we found that lack of Rasd2 triggers a striking hypersensitivity to the Amph- and PCP-induced motor stimulation in mutants, indicating an inhibitory role exerted by this GTPase on striatal DA-mediated transmission under phasic conditions, possibly via inhibition of cAMP/PKA signaling cascade (Kelly et al, 2007; Pascoli et al, 2005; Svenningsson et al, 2003).
In a recent work, we reported that the lack of Rasd2 triggers higher responsiveness to caffeine and, more intriguingly, specific gender-sensitive electrophysiological, biochemical, and behavioral phenotypes (Ghiglieri et al, 2015). Here, we further confirmed a relevant interaction between the gender and the appearance of peculiar sex-sensitive phenotypes in Rasd2 mutants. Consistently, while we demonstrated that Rasd2-targeted deletion prominently enhanced Amph- and PCP-induced motor stimulation in both genders, we found that knockout females were protected against PPI dysfunction, seen in males. Given the established role of estrogen hormones in regulating the onset and severity of symptoms in patients with schizophrenia (Kulkarni et al, 2012), the gender-dependent PPI responses found in Rasd2 mutants represent an intriguing translational feature to decipher in future experiments. Accordingly, this preclinical model may provide a valuable in vivo tool to unveil the molecular determinants underlying the obscure interaction among sexual hormones and sensorimotor gating processes reported in humans (Kumari, 2011). Importantly, in support of previous clinical findings pointing to an association between RASD2 and schizophrenia in a subgroup of Taiwanese patients (Liu et al, 2008), present data provided neuroanatomical evidence that RASD2 mRNA is expressed in the putamen, as well as in the cortical layer V.
In addition, we demonstrated that variation in the gene coding for RASD2 (rs6518956) affects in vivo prefrontal and striatal phenotypes in healthy human subjects that are relevant to schizophrenia. However, the different cortical Rasd2 expression pattern between humans and mice represents a main concern for our cross-species studies and, in turn, could explain the absence of gross cognitive impairment in mutants (Supplementary Figure S3).
Taken together, the reported deficits in sensorimotor gating and the exaggerated behavioral responses to Amph and PCP found in KOs prompt us to suggest that Rasd2 mutants may represent a novel genetic mouse model recapitulating the relationship between altered striatal neurotransmission and the emergence of specific subgroup of schizophrenia-like symptoms.
Finally, considering the transcriptional regulation of Rasd2 by thyroid hormone (Vargiu et al, 2001), and the ability of this G-protein to act as a physiological ‘brake’ on striatal DA neurotransmission, we speculate that potential endocrine dysfunctions altering Rasd2 mRNA expression could influence central DA signaling and indirectly impact on the vulnerability to develop psychiatric disorders, including schizophrenia.
FUNDING AND DISCLOSURE
Alessandro Usiello was supported by NARSAD Independent Investigator Grant from the Brain and Behavior Research Foundation (Grant no: 20353). Alessandro Bertolino is a full-time employee of Hoffmann-La Roche Ltd. The authors declare no conflict of interest.
References
Braff DL, Geyer MA, Swerdlow NR (2001). Human studies of prepulse inhibition of startle: normal subjects, patient groups, and pharmacological studies. Psychopharmacology (Berl) 156: 234–258.
Brisch R, Saniotis A, Wolf R, Bielau H, Bernstein HG, Steiner J et al (2014). The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Front Psychiatry 5: 47.
Consortium EP (2012). An integrated encyclopedia of DNA elements in the human genome. Nature 489: 57–74.
Costa-Mattioli M, Monteggia LM (2013). mTOR complexes in neurodevelopmental and neuropsychiatric disorders. Nat Neurosci 16: 1537–1543.
DeLisi LE, Shaw SH, Crow TJ, Shields G, Smith AB, Larach VW et al (2002). A genome-wide scan for linkage to chromosomal regions in 382 sibling pairs with schizophrenia or schizoaffective disorder. Am J Psychiatry 159: 803–812.
Emamian ES, Hall D, Birnbaum MJ, Karayiorgou M, Gogos JA (2004). Convergent evidence for impaired AKT1-GSK3beta signaling in schizophrenia. Nat Genet 36: 131–137.
Errico F, Santini E, Migliarini S, Borgkvist A, Centonze D, Nasti V et al (2008). The GTP-binding protein Rhes modulates dopamine signalling in striatal medium spiny neurons. Mol Cell Neurosci 37: 335–345.
Falk JD, Vargiu P, Foye PE, Usui H, Perez J, Danielson PE et al (1999). Rhes: a striatal-specific Ras homolog related to Dexras1. J Neurosci Res 57: 782–788.
Gargiulo PA, Landa De Gargiulo AI (2014). Glutamate and modeling of schizophrenia symptoms: review of our findings: 1990-2014. Pharmacol Rep 66: 343–352.
Ghiglieri V, Napolitano F, Pelosi B, Schepisi C, Migliarini S, Di Maio A et al (2015). Rhes influences striatal cAMP/PKA-dependent signaling and synaptic plasticity in a gender-sensitive fashion. Sci Rep 5: 10933.
Goldman-Rakic PS (1995). Cellular basis of working memory. Neuron 14: 477–485.
Gottesmann C (2003). Inhibitory processes in the brain. Drug Discov Today 8: 1020–1021.
Harrison LM, Lahoste GJ (2013). The role of Rhes, Ras homolog enriched in striatum, in neurodegenerative processes. Exp Cell Res 319: 2310–2315.
Harrison LM, LaHoste GJ (2006). Rhes, the Ras homolog enriched in striatum, is reduced under conditions of dopamine supersensitivity. Neuroscience 137: 483–492.
Harrison LM, Lahoste GJ, Ruskin DN (2008). Ontogeny and dopaminergic regulation in brain of Ras homolog enriched in striatum (Rhes). Brain Res 1245: 16–25.
Harrison LM, Muller SH, Spano D (2013). Effects of the Ras homolog Rhes on Akt/protein kinase B and glycogen synthase kinase 3 phosphorylation in striatum. Neuroscience 236: 21–30.
Javitt DC (2007). Glutamate and schizophrenia: phencyclidine, N-methyl-D-aspartate receptors, and dopamine-glutamate interactions. Int Rev Neurobiol 78: 69–108.
Jonas RK, Montojo CA, Bearden CE (2014). The 22q11.2 deletion syndrome as a window into complex neuropsychiatric disorders over the lifespan. Biol Psychiatry 75: 351–360.
Jones CA, Watson DJ, Fone KC (2011). Animal models of schizophrenia. Br J Pharmacol 164: 1162–1194.
Kelly MP, Isiegas C, Cheung YF, Tokarczyk J, Yang X, Esposito MF et al (2007). Constitutive activation of Galphas within forebrain neurons causes deficits in sensorimotor gating because of PKA-dependent decreases in cAMP. Neuropsychopharmacology 32: 577–588.
Kulkarni J, Hayes E, Gavrilidis E (2012). Hormones and schizophrenia. Curr Opin Psychiatry 25: 89–95.
Kumari V (2011). Sex differences and hormonal influences in human sensorimotor gating: implications for schizophrenia. Curr Top Behav Neurosci 8: 141–154.
Lee JH, Tecedor L, Chen YH, Monteys AM, Sowada MJ, Thompson LM et al (2015). Reinstating aberrant mTORC1 activity in Huntington's disease mice improves disease phenotypes. Neuron 85: 303–315.
Liu YL, Fann CS, Liu CM, Chen WJ, Wu JY, Hung SI et al (2008). RASD2, MYH9, and CACNG2 genes at chromosome 22q12 associated with the subgroup of schizophrenia with non-deficit in sustained attention and executive function. Biol Psychiatry 64: 789–796.
Mansbach RS, Geyer MA, Braff DL (1988). Dopaminergic stimulation disrupts sensorimotor gating in the rat. Psychopharmacology (Berl) 94: 507–514.
Manzano J, Morte B, Scanlan TS, Bernal J (2003). Differential effects of triiodothyronine and the thyroid hormone receptor beta-specific agonist GC-1 on thyroid hormone target genes in the b ain. Endocrinology 144: 5480–5487.
Martino D, Di Giorgio A, D'Ambrosio E, Popolizio T, Macerollo A, Livrea P et al (2011). Cortical gray matter changes in primary blepharospasm: a voxel-based morphometry study. Mov Disord 26: 1907–1912.
Napolitano F, Bonito-Oliva A, Federici M, Carta M, Errico F, Magara S et al (2010). Role of aberrant striatal dopamine D1 receptor/cAMP/protein kinase A/DARPP32 signaling in the paradoxical calming effect of amphetamine. J Neurosci 30: 11043–11056.
Pascoli V, Valjent E, Corbille AG, Corvol JC, Tassin JP, Girault JA et al (2005). cAMP and extracellular signal-regulated kinase signaling in response to d-amphetamine and methylphenidate in the prefrontal cortex in vivo: role of beta 1-adrenoceptors. Mol Pharmacol 68: 421–429.
Pasqualetti M, Ori M, Castagna M, Marazziti D, Cassano GB, Nardi I (1999). Distribution and cellular localization of the serotonin type 2C receptor messenger RNA in human brain. Neuroscience 92: 601–611.
Potash JB, Zandi PP, Willour VL, Lan TH, Huo Y, Avramopoulos D et al (2003). Suggestive linkage to chromosomal regions 13q31 and 22q12 in families with psychotic bipolar disorder. Am J Psychiatry 160: 680–686.
Ralph RJ, Paulus MP, Fumagalli F, Caron MG, Geyer MA (2001). Prepulse inhibition deficits and perseverative motor patterns in dopamine transporter knock-out mice: differential effects of D1 and D2 receptor antagonists. J Neurosci 21: 305–313.
Sciamanna G, Napolitano F, Pelosi B, Bonsi P, Vitucci D, Nuzzo T et al (2015). Rhes regulates dopamine D2 receptor transmission in striatal cholinergic interneurons. Neurobiol Dis 78: 146–161.
Seeman P (2014). Clozapine, a fast-off-D2 antipsychotic. ACS Chem Neurosci 5: 24–29.
Spano D, Branchi I, Rosica A, Pirro MT, Riccio A, Mithbaokar P et al (2004). Rhes is involved in striatal function. Mol Cell Biol 24: 5788–5796.
Subramaniam S, Mealer RG, Sixt KM, Barrow RK, Usiello A, Snyder SH (2010). Rhes, a physiologic regulator of sumoylation, enhances cross-sumoylation between the basic sumoylation enzymes E1 and Ubc9. J Biol Chem 285: 20428–20432.
Subramaniam S, Napolitano F, Mealer RG, Kim S, Errico F, Barrow R et al (2012). Rhes, a striatal-enriched small G protein, mediates mTOR signaling and L-DOPA-induced dyskinesia. Nat Neurosci 15: 191–193.
Svenningsson P, Tzavara ET, Carruthers R, Rachleff I, Wattler S, Nehls M et al (2003). Diverse psychotomimetics act through a common signaling pathway. Science 302: 1412–1415.
Svensson TH (2000). Dysfunctional brain dopamine systems induced by psychotomimetic NMDA-receptor antagonists and the effects of antipsychotic drugs. Brain Res Brain Res Rev 31: 320–329.
Swerdlow NR, Geyer MA (1998). Using an animal model of deficient sensorimotor gating to study the pathophysiology and new treatments of schizophrenia. Schizophr Bull 24: 285–301.
Tan HY, Nicodemus KK, Chen Q, Li Z, Brooke JK, Honea R et al (2008). Genetic variation in AKT1 is linked to dopamine-associated prefrontal cortical structure and function in humans. J Clin Invest 118: 2200–2208.
Turetsky BI, Calkins ME, Light GA, Olincy A, Radant AD, Swerdlow NR (2007). Neurophysiological endophenotypes of schizophrenia: the viability of selected candidate measures. Schizophr Bull 33: 69–94.
Usiello A, Baik JH, Rouge-Pont F, Picetti R, Dierich A, LeMeur M et al (2000). Distinct functions of the two isoforms of dopamine D2 receptors. Nature 408: 199–203.
Vallortigara J, Alfos S, Micheau J, Higueret P, Enderlin V (2008). T3 administration in adult hypothyroid mice modulates expression of proteins involved in striatal synaptic plasticity and improves motor behavior. Neurobiol Dis 31: 378–385.
Vallortigara J, Chassande O, Higueret P, Enderlin V (2009). Thyroid hormone receptor alpha plays an essential role in the normalisation of adult-onset hypothyroidism-related hypoexpression of synaptic plasticity target genes in striatum. J Neuroendocrinol 21: 49–56.
Vargiu P, De Abajo R, Garcia-Ranea JA, Valencia A, Santisteban P, Crespo P et al (2004). The small GTP-binding protein, Rhes, regulates signal transduction from G protein-coupled receptors. Oncogene 23: 559–568.
Vargiu P, Morte B, Manzano J, Perez J, de Abajo R, Gregor Sutcliffe J et al (2001). Thyroid hormone regulation of rhes, a novel Ras homolog gene expressed in the striatum. Brain Res Mol Brain Res 94: 1–8.
Vauquelin G, Bostoen S, Vanderheyden P, Seeman P (2012). Clozapine, atypical antipsychotics, and the benefits of fast-off D2 dopamine receptor antagonism. Naunyn Schmiedebergs Arch Pharmacol 385: 337–372.
Wenthur CJ, Bennett MR, Lindsley CW (2014). Classics in chemical neuroscience: fluoxetine (Prozac). ACS Chem Neurosci 5: 14–23.
Xu R, Hranilovic D, Fetsko LA, Bucan M, Wang Y (2002). Dopamine D2S and D2L receptors may differentially contribute to the actions of antipsychotic and psychotic agents in mice. Mol Psychiatry 7: 1075–1082.
Acknowledgements
We are grateful to Neurodegenerative Diseases Brain Bank (King’s College London, UK) for providing us postmortem prefrontal cortex samples. We thank Dr P Krashia and S Subramanian for his critical discussion and M Squillace, G Aceto, T Nuzzo, and V Lucignano for their excellent technical support. We also thank R Masellis, P Selvaggi, R Romano, and S Trizio for their contribution to data analysis.
Author contributions
AU and AB designed the research and approved the final version of the paper. ADM, DV, FN, ADG, MP, VM, BP, FE, MTA, BG, LF, and PT performed the research. ADG, GB, FE, AU, MP, and AB analyzed the data. DV, FN, ADG, AB, and AU wrote the paper.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Vitucci, D., Di Giorgio, A., Napolitano, F. et al. Rasd2 Modulates Prefronto-Striatal Phenotypes in Humans and ‘Schizophrenia-Like Behaviors’ in Mice. Neuropsychopharmacol 41, 916–927 (2016). https://doi.org/10.1038/npp.2015.228
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2015.228
This article is cited by
-
Matrix Metalloproteinase 1 as a Marker of Tonsil-Derived Mesenchymal Stem Cells to Assess Bone Marrow Cell Migration
Tissue Engineering and Regenerative Medicine (2023)
-
Patterns of neuronal Rhes as a novel hallmark of tauopathies
Acta Neuropathologica (2021)
-
The mammalian target of rapamycin (mTOR) kinase mediates haloperidol-induced cataleptic behavior
Translational Psychiatry (2020)
-
Genome-wide DNA methylation meta-analysis in the brains of suicide completers
Translational Psychiatry (2020)
-
The striatal-enriched protein Rhes is a critical modulator of cocaine-induced molecular and behavioral responses
Scientific Reports (2019)