Abstract
Histamine H1 receptor systems have been shown in animal studies to have important roles in the reversal of sensorimotor gating deficits, as measured by prepulse inhibition (PPI). H1-antagonist treatment attenuates the PPI impairments caused by either blockade of NMDA glutamate receptors or facilitation of dopamine transmission. The current experiment brought the investigation of H1 effects on sensorimotor gating to human studies. The effects of the histamine H1 antagonist meclizine on the startle response and PPI were investigated in healthy male subjects with high baseline startle responses and low PPI levels. Meclizine was administered to participants (n=24) using a within-subjects design with each participant receiving 0, 12.5, and 25 mg of meclizine in a counterbalanced order. Startle response, PPI, heart rate response, galvanic skin response, and changes in self-report ratings of alertness levels and affective states (arousal and valence) were assessed. When compared with the control (placebo) condition, the two doses of meclizine analyzed (12.5 and 25 mg) produced significant increases in PPI without affecting the magnitude of the startle response or other physiological variables. Meclizine also caused a significant increase in overall self-reported arousal levels, which was not correlated with the observed increase in PPI. These results are in agreement with previous reports in the animal literature and suggest that H1 antagonists may have beneficial effects in the treatment of subjects with compromised sensorimotor gating and enhanced motor responses to sensory stimuli.
Similar content being viewed by others
INTRODUCTION
Motor responses in animals and humans are influenced by the subject’s ability to gate or blunt responsivity to sensory stimuli (sensorimotor gating; Swerdlow et al, 2000). Impairments in sensorimotor gating include deficits in the ability to inhibit responses to stimuli and subsequent behavioral expressions of heightened motor reactivity. Although complex and multiply determined, phenotypic expressions of motor over-reactivity in humans have been associated with impaired gating (eg, Davies et al, 2009; Miller and Fuller 2006), with deficits in sensorimotor gating being observed in neurobehavioral impairments and psychiatric disorders such as schizophrenia or obsessive-compulsive disorder. In the present study, changes in sensorimotor gating in response to a pharmacological intervention and placebo in a sample of adult humans with low baseline gating and high startle responses were examined using prepulse inhibition (PPI) of the acoustic startle response.
PPI refers to the reduction of the startle response magnitude to an intense sensory stimulus (pulse) when another less intense stimulus (prepulse) is presented shortly beforehand. This reduction in response is seen over a variety of sensory stimuli, including auditory, tactile, visual, and cross-modal, and is seen in many species ranging from rodents to humans. PPI is a neurobehavioral phenomenon that can be used as an operational measure of sensorimotor gating, where the reduced response to the pulse stimulus is thought to be caused by the momentary inhibitory gating process triggered by the prepulse to protect the earliest stages of processing of the prepulse stimulus (Dawson et al, 2000). Deficits in sensorimotor gating as measured using PPI have been observed in individuals with a range of psychiatric and neurological disorders, including schizophrenia (Braff et al, 1978), Tourette’s syndrome (Castellanos et al, 1996), obsessive-compulsive disorder (Swerdlow et al, 1993), and Huntington’s disease (Swerdlow et al, 1995).
Animal models offer a well-established method of identifying candidate interventions for sensorimotor gating deficits. Animal models of sensorimotor gating deficits include pharmacological manipulations that target specific brain areas in the animal and that cause deficits in PPI similar to those observed in human patients with some of the aforementioned psychiatric and neurobiological disorders (Geyer et al, 2001). For instance, it has been shown that dopamine agonists (such as amphetamine or apomorphine) or NMDA-receptor antagonists (dizocilpine or phencyclidine) reduce PPI (eg, Mansbach et al, 1988; Mansbach and Geyer 1989) and can elicit schizophrenia-like behavior (Kokkinidis and Anisman 1980; Olszewski et al, 2008) in rats. In addition, subsequent administration of the atypical antipsychotic clozapine (a complex drug with inhibitory effects on a variety of neurotransmitter receptors, including dopamine D4, serotonin 5-HT2, alpha-adrenergic, and histamine H1 receptors) counteracts the PPI deficits induced by these types of drugs, re-establishing PPI to normal levels (Swerdlow et al, 1991; Bakshi et al, 1994).
In a related way, it has been previously reported that a moderate dose of the histamine H1-receptor antagonist pyrilamine can effectively antagonize the PPI deficits caused by the NMDA-receptor antagonist dizocilpine (Roegge et al, 2007) in rats. It has also been shown that the same dose range of pyrilamine can effectively reverse the PPI impairment in rats caused by amphetamine (Larrauri and Levin 2010). To date, these results have not been extended to humans with PPI deficits. Accordingly, the main aim of the present study was to analyze the effects of antihistamines on PPI in healthy human subjects with reduced sensorimotor gating, who also exhibited enhanced motor responses (Miller et al, 2009, Reynolds and Lane 2008). Using a population with low-gating traits similar to those exhibited by patients with psychotic disorders may aid in the understanding of how different neurotransmitter systems targeted by atypical antipsychotics could help in restoring normal gating, and previous studies have used the translational approach of investigating the effects of antipsychotic drugs on PPI in healthy subjects with low baseline PPI levels. For instance, atypical antipsychotics (quetiapine, clozapine, sertindole) have been reported to enhance sensorimotor gating in ‘normal, low-gating’ humans (Swerdlow et al, 2006; Vollenweider et al, 2006; Holstein et al, 2011), whereas the typical antipsychotic haloperidol has not been shown effective in increasing PPI in these subjects (Csomor et al, 2008). Using this approach, and based on the observed beneficial effects of antihistamines in animal models of deficient sensorimotor gating, we hypothesized that antihistamines would increase PPI in healthy subjects with low baseline PPI levels.
Due to the fluctuations of PPI during the different phases of the menstrual cycle (Swerdlow et al, 1997), we aimed to reduce the variability of the results in this study by analyzing the potential effects of the histamine antagonist only on male participants. Individual differences before administration of the intervention were examined by investigating baseline sex differences in startle amplitude, PPI, self-report measures of emotional states, and physiological responses during the baseline test session.
The widely used H1 antihistamine meclizine was tested in this study to assess its effects on the startle response and PPI. Meclizine is a safe and effective drug, approved by the FDA for over-the-counter sale. It is used in the management of nausea, vomiting, and dizziness associated with motion sickness, in many cold and flu treatments, and is also a component of some formulations of menstrual cramping and premenstrual syndrome compounds. As a first-generation antihistamine drug, meclizine crosses the blood–brain barrier and can reach histamine receptors in the brain that modulate PPI. Using a repeated-measures counterbalanced design, male participants received placebo and two doses of meclizine on different days in a counterbalanced order before each test session. In order to assess potential negative side effects of the treatment drug and/or correlated outcomes, heart rate (HR), skin response, and self-report measures (arousal, valence, and drowsiness levels) were collected throughout the different phases of the experiment.
MATERIALS AND METHODS
Participants
Recruitment
This study was conducted with the approval of the Duke University Medical Center Institutional Review Board for human subjects. All participants signed a written informed consent before enrolling in the experiment. Healthy subjects with ages ranging between 18 and 40 years were recruited from Duke University, Duke University Medical Center, and the Durham community area via newspaper advertisements, online listings, flyers, and referrals from clinics. Exclusion criteria for prospective participants included history of bipolar disorder or psychotic disorder, current substance use disorder; current use of medicines that block H1-histamine receptors, or substances known to influence psychophysiological arousal (such as alcohol) or PPI (smokers); receiving electroconvulsive shock therapy or any other treatment that may interfere with neural responses to startle probes; history of neurological disorder; significant hearing impairment; history of adverse response to antihistamines; and/or receiving medication for any psychiatric illness (SSRIs, SSNRIs, anxiolytics, or other psychotropics that cause CNS-depressant effects). Male participants who met the inclusion criteria and exhibited (a) high startle responses (>2.5 μV) and (b) overall low PPI levels (<50%) during a subsequent baseline session (Day 1) were deemed eligible to continue in the study (Days 2–4). The 2.5-μV startle response limit was selected using the median-split of the mean response amplitude of male participants to pulse-alone trials in a session from pilot data and previous studies from our laboratory (eg, Larrauri et al, 2012). The PPI threshold was also derived from these data and other experiments in the literature that used similar parameters to the ones in this study (Braff et al, 1992, Cadenhead et al, 2000; Perry et al, 2001).
Participant sample
One hundred and fifteen participants (67 males, 48 females) were recruited for the initial phase of the experiment (Day 1). Seven female and six male participants failed to meet the inclusion criteria. Thus, 102 participants (61 males, 41 females) were tested on Day 1.
After the initial assessment (Day 1), eligible male participants were asked to return to the laboratory for three additional sessions (Days 2–4) in which their startle responses were re-tested after receiving two doses of the study drug or a placebo pill. Non-eligible participants were debriefed and compensated for their participation. Twenty-eight of the 61 male participants tested on Day 1 exhibited high startle responses and low PPI and therefore were asked to continue their participation for Days 2–4. Data from four of these participants were subsequently excluded from the final analysis because of scheduling conflicts that prevented the completion of all additional test days (n=1), the presence of allergies which required medications that interfered with the study manipulation (n=1), and data artifacts during test measurements (n=2). The final sample therefore consisted of 24 male participants (mean age M=24.4 years, SD=4.9 years), composed of self-identified Caucasian (66.7%), Hispanic/Latino (12.5%), Asian (12.5%), and African-American (8.3%) participants.
Measures
Startle response
Eye-blink activity was obtained by recording electromyographic (EMG) signals from the orbicularis oculi muscle beneath the right eye. Two Ag/Ag-Cl electrodes were placed over the muscle, and a ground electrode was placed on the participant’s forehead. Raw EMG signals were amplified (5000 × ) with a BIOPAC EMG150C module, filtering frequencies <10 and >500 Hz. Data were acquired and stored with a PC computer running AcqKnowledge 4.0 software, with a sampling rate of 2000 Hz. A 60-Hz band-stop filter (to reject power-line noise) and a band-pass filter (28–500 Hz) were applied, and the resulting signal was averaged over 20 successive samples (smoothed) to determine eye-blink responses. Startle responses were then defined as those eye-blink activities whose peak amplitude values occurred between 21 and 100 ms after a pulse stimulus onset (Grillon et al, 1991). Peak responses that took place before 21 ms past the beginning of the sound were considered unrelated to the stimulus, whereas responses occurring 100 ms after the sound were deemed potentially random or consciously produced.
PPI
PPI was calculated as the difference of the average startle response to the pulse-alone trials and the average of the response to the prepulse-pulse trials and divided by the average response to the pulse-alone trials in each session, ie, PPI (%)=100 × (Pulse alone−Prepulse Pulse)/Pulse alone.
HR
Electrocardiography (ECG) activity was recorded using two electrodes placed on the right clavicle and the lowest rib on the participant’s left side. Raw ECG signals were amplified (500 × ) and band-pass filtered (0.5–35 Hz) with a BIOPAC ECG150C module. These data were later transformed off-line to HR (expressed in beats per minute (bpm)), and an average HR was calculated for all 5-s intervals preceding and following startle trials.
Skin response
Skin conductance electrodes were placed on the middle phalanx of the middle and index fingers of the participant’s non-dominant hand. Before placing the electrodes, Signa gel Electrode Gel was applied on the participant’s phalanxes, and afterward the electrodes were secured to the fingers with medical tape. Skin conductance signals were low-pass filtered (10 Hz) with a BIOPAC GSR150C module, which was calibrated to detect activity in the 0–20 μSiemens (μS) range. Average galvanic skin responses (GSR) were calculated for each 5-s interval preceding and following each startle trial.
Self-report ratings
Emotional states were determined with Self-Assessment Manikin scales (Bradley and Lang 1999), which assessed arousal and valence of the current affective condition using 1–9 Likert-type scales (with lower numbers indicating lower levels of arousal or valence). Similarly, levels of sedation were assessed using a 1–9 Likert-type scale, where low numbers represented a sleepy or lethargic state and high values indicated feeling alert or fully awake.
Design
For eligible male participants, the experiment took place in four sessions carried out on different days. Consecutive test sessions took place no earlier than 3 days and no longer than 21 days apart. The rest of the participants were only exposed to the initial assessment on Day 1.
Day 1
During the first session, participants were asked about their tobacco/nicotine use, medications that they were currently taking, and caffeine history use. Carbon monoxide (CO) levels were collected using a CO monitor to confirm that participants had not used tobacco products recently (CO levels >8 ppm disqualified them from continuing in the study). Urine analyses testing for the presence of oxycontin, THC, benzodiazepines, barbiturates, methadone, and amphetamines were conducted on site using a Biosite Triage Meter Plus and test strips. After this stage was complete, startle responses and PPI levels were assessed (see Procedure section below). Participants who were not eligible to continue in the study after Day 1 were de-briefed and compensated with $25.
Days 2–4
During each of the following three sessions (Days 2–4), male participants were asked to fill out a questionnaire about their tobacco or nicotine use since the previous visit and to assess any changes in their medications (specifically to verify that a participant had not used an allergy, cold/flu medication within 3 days of the last study visit). They were also asked about their caffeine use on the day of the experiment, and baseline sedation levels were assessed. Participants were instructed not to drive to the experiment location in order to avoid potential effects of meclizine interfering with their abilities to operate vehicles: on each test day, the study coordinator verified that participants walked to the laboratory, used public transportation, or arranged for somebody to drop off and pick them up from the study location. On these test days, the same startle test procedure used on Day 1 was used with the difference that 60 min before the start of each test session participants received a pill of either (a) placebo, (b) a low dose (12.5 mg), or (c) a high dose (25 mg) of meclizine. Each participant received all treatment levels randomly, with the drug order counterbalanced between subjects. Placebo and meclizine capsules were identical in shape, size, and color. The randomization and counterbalancing of the order of dosing was done by the study principal investigator (PI). In order to ensure that the double-blind procedure was not broken, identical capsules were given to the study coordinator in containers labeled only with the subject identification number and test session, who then delivered them to the participants on each test day. The PI had no contact with the participants in the study.
During the resting period between the pill intake and experimental task, participants were asked to sit in a lab room and to read or wait until the beginning of the session. At the time of drug intake, as well as 20 and 40 min later, sedation levels were assessed, and after 60-min startle responses and PPI levels were assessed (see Procedure section below). After completing each day’s session, participants were compensated with $75.
Drug
Meclizine tablets (Par Pharmaceuticals, Spring Valley, NY, USA) were placed in capsules to provide a double blind design to both the investigators and participants. The drug was administered orally to study participants in 12.5 and 25 mg doses (in addition to placebo) during different test days in a repeated measures counterbalanced design.
Stimuli
Acoustic startle stimuli (pulses) were 40-ms, 115-dBA noise bursts with instantaneous rise and fall times. Pulse-alone trials consisted only of a pulse stimulus. In prepulse-pulse trials, an 86-dBA, 20-ms noise burst (prepulse) was presented 30, 60, or 120 ms (lead interval) before the onset of the pulse. A continuous 70-dB white noise was used as the background sound throughout each test session. All auditory stimuli were generated by a PC computer running Matlab/Cogent software and delivered to the participants through headphones.
Procedure
Pre-test phase
After assessing emotional state and drowsiness levels, participants completed a hearing test to rule out potential effects of hearing problems on startle responses and PPI. In this hearing test, 3-s tones of different frequencies (500, 1000, and 6000 Hz) and intensities (35, 45, and 55 dB) were presented three times with a variable interval (8±2 s) on a 28-dB background white noise. Participants were instructed to press a key as soon as they heard a tone being played and were required to detect at least six of the nine possible sounds for each intensity level. A resting period of 5 min ensued, where participants were instructed to sit quietly with their eyes open while looking at a fixation cross at the center of the monitor screen.
Test phase
Participants were then exposed to an initial adaptation phase, in order for them to become acquainted with the auditory stimuli and for their startle responses to reach a stable level, during which five pulse-alone trials were introduced. After this phase, 64 trials were presented randomly: 16 pulse-alone and 48 prepulse-pulse trials (ie, 16 prepulse-pulse trials for each of the three lead intervals). Startle responses and PPI values were determined using the data from these trials. Finally, five additional pulse-alone trials were presented. The inter-trial interval was 20 s (±5 s). At the end of the test phase, emotional state and drowsiness levels were re-assessed. HR and GSR were recorded throughout the entire session, which lasted approximately 25 min.
Data analysis
Day 1
Paired-sample Student’s t-tests were used to assess the effect of (a) test session on self-report measures (arousal, valence, and drowsiness) and (b) startle trials on HR and GSR in male participants. A one-way repeated-measures ANOVA test was used to analyze the effects of lead interval on PPI.
Days 2–4
Startle responses were analyzed with one-way repeated-measures ANOVA tests, using Drug dose (levels: Placebo vs Low Dose vs High Dose) as the main factor. Effects on PPI were studied with two-way repeated-measures 3 × 3 ANOVA tests, using Drug and Lead interval (30 vs 60 vs 120 ms) as main factors.
Average HR and GSR levels throughout test sessions were analyzed with one-way repeated-measures ANOVA tests, with Drug as the main factor. Using the average 5-s activity immediately preceding and following all startle trials, the effects of the auditory stimuli on HR and GSR were studied with 3 × 2 (Drug × Startle trial: pre vs post) repeated-measures ANOVA tests. Self-report ratings at different times during the experimental phase (Session) were analyzed using two-way repeated-measures ANOVA tests, with Drug and Session as main factors.
Significant main effects were followed up by tests comparing the impact of the individual levels using Holm–Bonferroni corrections. Reduced degrees of freedom (Greenhouse–Geisser) were used when appropriate to offset violations of the sphericity assumption underlying repeated-measures ANOVA tests. A p-value of 0.05 was used as the threshold for significance on all statistical tests.
RESULTS
Day 1
A one-way repeated-measures ANOVA test (Lead interval: 30 vs 60 vs 120 ms) on PPI levels in male participants yielded a significant Lead interval effect (F(2,120)=28.47, p<0.0001, ɛ=0.76), indicating that PPI was lower for 30 ms than for 60 and 120 ms intervals (ps<0.001). Student’s t-tests on self-report ratings (pre-test vs post-test) revealed significant effects of test session on arousal (t(60)=4.34, p<0.001), valence (t(60)=−6.48, p<0.001), and drowsiness (t(60)=3.71, p<0.001) in male participants. In addition, t-tests on physiological responses (pre- vs post-startle trials) showed a significant effect of startling stimuli on HR (t(60)=4.34, p<0.001) and GSR (t(60)=6.47, p<0.001), indicating that the loud auditory stimuli affected both physiological measures. Female participants showed PPI levels similar to those of males, with higher startle response amplitudes. Physiological and self-report measures were similar between male and female participants, with females showing (a) lower overall skin conductance levels and (b) smaller increases in arousal than male participants (Supplementary Table S1).
During the baseline session, the median startle response for male participants in pulse-alone trials was 3.0 μV, with 57.4% of male participants showing average startle responses higher than the 2.5-μV response threshold of the study. The overall median PPI level was 35.3%, with 70% of male participants exhibiting average PPI levels lower than the 50% inhibition limit. Overall, 45.9% of male participants (n=28) met both the startle and PPI levels required to take part in the following three test sessions.
Days 2–4
Startle response
A one-way repeated-measures ANOVA test revealed no significant main effect of Drug (Placebo vs Low Dose vs High Dose) on the startle response magnitude in pulse-alone trials (F(2,46)=1.51, p>0.23), suggesting that meclizine did not cause significant changes to the amplitude of the startle response (see Table 1).
PPI
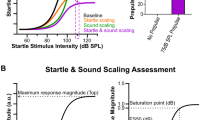
A 3 × 3 repeated-measures ANOVA (Drug: Placebo vs Low Dose vs High Dose × Lead interval: 30 vs 60 vs 120 ms) revealed significant main effects of Drug (F(2,92)=3.4, p<0.05, ɛ=0.93) and Lead interval on PPI (F(2,92)=17.32, p<0.0001, ɛ=0.78) but no interaction between these factors (F(4,92)=1.35, p>0.26). Subsequent post-hoc analyses revealed that overall PPI was higher in both Low (32.8%; p<0.03) and High Dose (33.1%; p<0.03) conditions than after placebo intake (25.3%) and that PPI was lower for 30-ms than for both 60-ms (p<0.001) and 120-ms (p<0.01) Lead intervals (Figure 1).
Meclizine effects on PPI as a function of drug dose and lead interval. Data represent mean values (±SEM). PPI was lower for the 30 ms than for the 60 and 120 ms intervals (p<0.001 and p<0.01, respectively). Meclizine administration significantly increased PPI (p<0.05) for the three lead intervals analyzed. Both low (12.5 mg) and high (25 mg) meclizine doses produced similar increases in overall PPI when compared with the control (placebo) condition (*p<0.03).
HR
One-way ANOVA tests showed that overall mean HR throughout test sessions was not affected by Drug (F<1). Startle trials significantly increased HR: a 3 × 2 ANOVA test comparing mean HRs before and after startling stimuli (Drug × Startle trial: Pre vs Post) revealed a significant main effect of Startle trial (F(1,46)=20.92, p<0.0002) on HR but no effect of Drug (F<1) or an interaction between factors (F<1). That is, the increase in HR caused by the startling stimuli was not affected by meclizine (Table 1).
Skin response
One-way ANOVA tests revealed that mean skin conductance levels across test sessions were not affected by Drug (F<1). A 3 × 2 ANOVA test (Drug × Startle trial: pre-auditory stimulus vs post-auditory stimulus) showed a significant main effect of startling sounds on GSR (F(1,44)=9.31, p<0.006) but no effect of Drug (F<1) or an interaction between factors (F<1). That is, the GSR increase triggered by the auditory stimuli was not influenced by meclizine (Table 1).
Self-report ratings
Arousal
Changes in self-reported arousal levels assessed before (pre) and after (post) test sessions were affected by Drug. A 3 × 2 ANOVA test (Drug × Session: pre vs post) on arousal revealed a significant main effect of Drug (F(2,46)=3.58, p<0.05, ɛ=0.9) but no effect of Session (F<1) or an interaction between factors (F<1). Subsequent analyses indicated that participants reported overall lower levels of arousal after taking Placebo than when receiving Low (p<0.05) and High (p<0.05) doses of meclizine (Figure 2, top-left panel).
Self-report ratings before and after startle probe sessions as a function of drug dose. Data represent mean values (±SEM). Overall arousal ratings were similar before and following test sessions but higher after meclizine administration (both doses) than after placebo intake (top-left panel). Mean valence ratings decreased after test sessions but were not affected by meclizine (top-right panel). Similarly, drowsiness levels increased continuously after pill intake and throughout testing but were not differentially affected by drug condition (bottom panel).
As both doses of meclizine were associated with changes in PPI and self-reported emotional arousal, correlation tests were conducted to examine whether these effects were associated. Increases in PPI caused by low doses of meclizine were not significantly correlated with the observed changes in self-reported emotional arousal (r=0.103, t(22)=0.486, p>0.31). Similarly, the increase in PPI produced by high doses of meclizine were not significantly related to the changes in self-reported emotional arousal (r=0.22, t(22)=1.06, p>0.15). These results suggest that the significant effects of meclizine on PPI and subjective appraisals of emotional arousal were independent.
Affective valence
Subjective valence ratings before and after test sessions were not affected by Drug: a 3 × 2 ANOVA test (Drug × Session) yielded a significant main effect of Session on valence scores (F(1,46)=22.96, p<0.0001), which indicated a decrease in positive affect after the test phase, but no significant main effect of Drug (F<1) or an interaction between factors (F(2,46)=1.56, p>0.22). This result suggests that the overall decrease in valence was not affected by meclizine (Figure 2, top-right panel).
Drowsiness
Participants reported an increase in drowsiness throughout the experimental session: a 3 × 5 ANOVA test (Drug × Session: 0 min after drug intake vs 20 min vs 40 min vs pre-test vs post-test) on drowsiness ratings showed a significant main effect of Session (F(4,184)=25.8, p<0.0001), indicating a linear increase in drowsiness as the session progressed (at pre-test, drowsiness was significantly lower than at 0 (p<0.008) and 20 min (p<0.03) after pill intake, and at post-test drowsiness was significantly lower than at pre-test (p<0.004)). No significant main effect of Drug (F<1) or an interaction between factors was found (F<1). These results indicate that meclizine did not affect self-reported drowsiness ratings (Figure 2, bottom panel).
DISCUSSION
Both doses of meclizine tested on Days 2–4 (12.5 and 25 mg) significantly increased PPI relative to placebo across lead intervals analyzed (30, 60, and 120 ms; ps<0.03), without altering the magnitude of the startle response in pulse-alone trials (p>0.23). That is, the two relatively low doses of meclizine administered in the study could effectively enhance PPI without affecting the participants’ response amplitude (sensitivity) to the startling stimuli. For all conditions (Placebo, Low Dose, and High Dose) PPI was lower for the shortest prepulse-pulse lead interval (30 ms) than for the other two intervals (60 and 120 ms; p<0.001 and p<0.01, respectively). This finding is consistent with previous reports showing that maximum PPI in humans usually occurs for lead intervals between 60–120 ms (Braff et al, 1978; Ison and Pinckney 1983). Furthermore, no interaction between Drug and Lead interval was found, suggesting that meclizine does not differentially improve sensorimotor gating deficits when the interval between the prepulse and pulse stimuli is changed.
The finding that an H1-receptor antagonist can enhance PPI in humans is consistent with results in the animal literature showing that pyrilamine (another H1-antagonist) antagonizes PPI deficits in rats caused by either amphetamine (Larrauri and Levin 2010) or dizocilpine (Roegge et al, 2007). In the first case, 20 mg/kg pyrilamine significantly increased PPI after it was disrupted by a 1 mg/kg dose of amphetamine, but a higher dose (40 mg/kg) only showed a non-significant trend toward an increase, and a lower dose (10 mg/kg) could not reverse the amphetamine-induced PPI disruption. Similarly, Roegge et al, (2007) showed that 10- and 20-mg/kg pyrilamine doses could reverse the PPI disruption caused by the administration of 0.05 mg/kg dizocilpine, but 40 mg/kg pyrilamine showed only a non-significant trend toward PPI restoration. The findings indicating that the PPI increase caused by pyrilamine in both animal models shows an inverted U-shape function points to the possibility of an optimal dose of meclizine to treat PPI deficits in humans, and that larger doses may be inefficient in enhancing PPI. Further experiments analyzing the effects of a wider range of meclizine doses are needed to determine optimal dosages to obtain the largest possible improvements of sensorimotor gating in humans.
Other studies have previously shown that atypical antipsychotics such as clozapine (Vollenweider et al, 2006) and quetiapine (Swerdlow et al, 2006) can enhance PPI in healthy subjects with low baseline sensorimotor gating. Histamine is one of the neurotransmitter systems targeted by these antipsychotics (Coward 1992, Richelson and Souder 2000). By targeting a wider range of neurotransmitter systems, atypical antipsychotics are better suited to reverse sensorimotor gating deficits in animal models where typical antipsychotics are not effective. For example, clozapine has been shown to reverse both apomorphine- (Swerdlow et al, 1991) and dizocilpine-induced (Bakshi et al, 1994) PPI disruptions, whereas haloperidol can reverse the former (Mansbach et al, 1988) but not the latter (Geyer et al, 1990). Hence, analyzing specific subcomponents of antipsychotic drug actions that are effective for reversing PPI impairments can help to elucidate therapies for treating sensorimotor gating impairments, as was the case in this study.
The tuberomammillary nucleus is the source of histamine in the brain and has efferent connections, among others, to the cortex, basal ganglia, and nucleus accumbens (NAc) (Panula et al, 1984), all brain regions involved in the modulation of PPI (Koch 1999). Thus it is possible that the results observed in the present study could be caused by the effects of H1-receptor antagonists in the NAc, which is the main center of convergence of several neurotransmitter systems that modulate PPI, including the cortex (Koch 1999). It has been shown that infusions of pyrilamine in the NAc decrease extracellular dopamine levels (Galosi et al, 2001), though the mechanism by which this is done is not clear (ie, presynaptic, indirectly through output neurons of the NAc, indirectly through hippocampal glutamatergic neurons, or interfering with the dopamine uptake). Increased concentrations of extracellular dopamine in the NAc have been associated with lower PPI levels (Goto et al, 2004), suggesting that the observed increase in PPI in this study could have been caused by a decrease in extracellular NAc dopamine after the meclizine intake.
Drowsiness is a known side effect of meclizine (eg, Manning et al, 1992, Raymond et al, 2000). Even when PPI is not affected during sleep (Silverstein et al, 1980), it could be posited that drowsiness may have led to a general lower level of alertness after meclizine administration, which could have affected PPI levels (Grillon and Davis 1997; van der Linden et al, 2006). In order to address this potential confounding factor, during each test day participants were asked to rate their alertness levels five times throughout each session: 0, 20, 40 min after pill intake, pre- (60 min), and post-test (85 min). Participants reported an overall increase in drowsiness as the test sessions progressed (Figure 2, bottom panel), but this effect was not significantly affected by meclizine (p>0.88). Therefore, these data do not support the view that the observed meclizine-induced increases in PPI were related to changes in drowsiness or alertness. Furthermore, the doses used in the study (12.5 and 25 mg; one measure per day) were substantially lower than others reported in the literature to cause increases in drowsiness (⩾50 mg/dose).
Changes in emotional states can affect the magnitude of the startle response. Lang et al, (1990) reported that eye-blink responses when looking at emotionally aversive images are larger than when watching neutral images and smaller than when looking at emotionally positive images. Therefore, it could be hypothesized that variations in emotional states may have influenced the changes in PPI triggered by meclizine. It has been previously reported that in some patients antihistamines produce paradoxical stimulatory effects (Zlott and Byrne 2010), and self-reported emotional arousal in this study was higher after participants were given meclizine than after receiving placebo, even when low doses of meclizine were administered to avoid sedative effects. It is not uncommon for drugs with sedative effects at higher doses to exhibit non-monotonic dose-effect functions with increases in self-reported stimulation at lower doses (eg, ethanol; Addicott et al, 2007). However, no significant effect of drug on the magnitude of the startle response was found (p>0.23), and the changes in arousal after low and high meclizine intake (compared with placebo) were not significantly correlated with the increases in PPI (p>0.31 and p>0.15, respectively) found in the study. Therefore, these results suggest that the observed increase in PPI was independent of the changes in self-reported emotional arousal following meclizine administration. Furthermore, valence ratings were not affected by either drug dose, providing additional evidence that affective state did not significantly influence the observed PPI changes.
In order to reduce variability in PPI associated with possible sex differences, data from males and females at baseline (Day 1) were collected, but only male participants continued on Days 2–4 of the experiment. In line with previous studies, results from the baseline test session (Supplementary Table S1) showed that female participants exhibited larger startle response amplitudes than male participants (eg, Blumenthal and Gescheider 1987; Kofler et al, 2001) with similar overall PPI levels (Della Casa et al, 1998; cf. Swerdlow et al, 1997). Future studies analyzing the efficacy of meclizine in enhancing PPI should include women, carefully controlling the phase of the menstrual cycle to avoid potential confounding effects.
In conclusion, our results show that two relatively low doses of the H1 histamine antagonist meclizine can effectively increase PPI in a population of male subjects who show high startle responses and low PPI, without affecting the startle response amplitude or sympathetic responses (HR or GSR). These findings may be useful in helping to inform the development of pharmacological interventions for individuals with reduced sensorimotor gating and enhanced motor responses to sensory stimuli.
FUNDING AND DISCLOSURE
The authors declare no conflict of interest.
References
Addicott MA, Marsh-Richard DM, Mathias CW, Dougherty DM (2007). The biphasic effects of alcohol: comparisons of subjective and objective measures of stimulation, sedation, and physical activity. Alcohol Clin Exp Res 31: 1883–1890.
Bakshi VP, Swerdlow NR, Geyer MA (1994). Clozapine antagonizes phencyclidine-induced deficits in sensorimotor gating of the startle response. J Pharmacol Exp Ther 271: 787–794.
Blumenthal TD, Gescheider GA (1987). Modification of the acoustic startle reflex by a tactile prepulse: the effects of stimulus onset asynchrony and prepulse intensity. Psychophysiology 24: 320–327.
Bradley MM, Lang PJ (1999) Affective Norms for English Words (ANEW): Instruction Manual and Affective Ratings Technical Report C-1, The Center for Research in Psychophysiology, University of Florida.
Braff D, Stone C, Callaway E, Geyer M, Glick I, Bali L (1978). Prestimulus effects on human startle reflex in normals and schizophrenics. Psychophysiology 15: 339–343.
Braff DL, Grillon C, Geyer MA (1992). Gating and habituation of the startle reflex in schizophrenic patients. Arch Gen Psychiatry 49: 206–215.
Cadenhead KS, Swerdlow NR, Shafer KM, Diaz M, Braff DL (2000). Modulation of the startle response and startle laterality in relatives of schizophrenic patients and in subjects with schizotypal personality disorder: evidence of inhibitory deficits. Am J Psychiatry 157: 1660–1668.
Castellanos FX, Fine EJ, Kaysen D, Marsh WL, Rapoport JL, Hallett M (1996). Sensorimotor gating in boys with Tourette's syndrome and ADHD: preliminary results. Biol Psychiatry 39: 33–41.
Coward DM (1992). General pharmacology of clozapine. Br J Psychiatry 160 (Suppl 17): 5–11.
Csomor PA, Stadler RR, Feldon J, Yee BK, Geyer MA, Vollenweider FX (2008). Haloperidol differentially modulates prepulse inhibition and p50 suppression in healthy humans stratified for low and high gating levels. Neuropsychopharmacology 33: 497–512.
Davies PL, Chang WP, Gavin WJ (2009). Maturation of sensory gating performance in children with and without sensory processing disorders. Int J Psychophysiol 72: 187–197.
Dawson ME, Schell AM, Hazlett EA, Nuechterlein KH, Filion DL (2000). On the clinical and cognitive meaning of impaired sensorimotor gating in schizophrenia. Psychiatry Res 96: 187–197.
Della Casa V, Hofer I, Weiner I, Feldon J (1998). The effects of smoking on acoustic prepulse inhibition in healthy men and women. Psychopharmacology (Berl) 137: 362–368.
Galosi R, Lenard L, Knoche A, Haas H, Huston JP, Schwarting RK (2001). Dopaminergic effects of histamine administration in the nucleus accumbens and the impact of H1-receptor blockade. Neuropharmacology 40: 624–633.
Geyer MA, Krebs-Thomson K, Braff DL, Swerdlow NR (2001). Pharmacological studies of prepulse inhibition models of sensorimotor gating deficits in schizophrenia: a decade in review. Psychopharmacology (Berl) 156: 117–154.
Geyer MA, Swerdlow NR, Mansbach RS, Braff DL (1990). Startle response models of sensorimotor gating and habituation deficits in schizophrenia. Brain Res Bull 25: 485–498.
Goto K, Ueki A, Iso H, Morita Y (2004). Involvement of nucleus accumbens dopaminergic transmission in acoustic startle: observations concerning prepulse inhibition in rats with entorhinal cortex lesions. Psychiatry Clin Neurosci 58: 441–445.
Grillon C, Ameli R, Woods SW, Merikangas K, Davis M (1991). Fear-potentiated startle in humans: effects of anticipatory anxiety on the acoustic blink reflex. Psychophysiology 28: 588–595.
Grillon C, Davis M (1997). Effects of stress and shock anticipation on prepulse inhibition of the startle reflex. Psychophysiology 34: 511–517.
Holstein DH, Csomor PA, Geyer MA, Huber T, Brugger N, Studerus E et al (2011). The effects of sertindole on sensory gating, sensorimotor gating, and cognition in healthy volunteers. J Psychopharmacol 25: 1600–1613.
Ison JR, Pinckney LA (1983). Reflex inhibition in humans: sensitivity to brief silent periods in white noise. Percept Psychophys 34: 84–88.
Koch M (1999). The neurobiology of startle. Prog Neurobiol 59: 107–128.
Kofler M, Muller J, Reggiani L, Valls-Sole J (2001). Influence of gender on auditory startle responses. Brain Res 921: 206–210.
Kokkinidis L, Anisman H (1980). Amphetamine models of paranoid schizophrenia: an overview and elaboration of animal experimentation. Psychol Bull 88: 551–579.
Lang PJ, Bradley MM, Cuthbert BN (1990). Emotion, attention, and the startle reflex. Psychol Rev 97: 377–395.
Larrauri JA, Levin ED (2010). PPI deficit induced by amphetamine is attenuated by the histamine H1 antagonist pyrilamine, but is exacerbated by the serotonin 5-HT2 antagonist ketanserin. Psychopharmacology (Berl) 212: 551–558.
Larrauri JA, Rosenthal MZ, Levin ED, McClernon FJ, Schmajuk NA (2012). Effects of unexpected changes in visual scenes on the human acoustic startle response and prepulse inhibition. Behav Process 89: 1–7.
Manning C, Scandale L, Manning EJ, Gengo FM (1992). Central nervous system effects of meclizine and dimenhydrinate: evidence of acute tolerance to antihistamines. J Clin Pharmacol 32: 996–1002.
Mansbach RS, Geyer MA (1989). Effects of phencyclidine and phencyclidine biologs on sensorimotor gating in the rat. Neuropsychopharmacology 2: 299–308.
Mansbach RS, Geyer MA, Braff DL (1988). Dopaminergic stimulation disrupts sensorimotor gating in the rat. Psychopharmacology (Berl) 94: 507–514.
Miller LJ, Fuller DA (2006) Sensational Kids: Hope and Help for Children with Sensory Processing Disorder (SPD) G.P. Putnam’s Sons: New York, NY, USA.
Miller LJ, Nielsen DM, Schoen SA, Brett-Green BA (2009). Perspectives on sensory processing disorder: a call for translational research. Front Integr Neurosci 3: 22.
Olszewski RT, Wegorzewska MM, Monteiro AC, Krolikowski KA, Zhou J, Kozikowski AP et al (2008). Phencyclidine and dizocilpine induced behaviors reduced by N-acetylaspartylglutamate peptidase inhibition via metabotropic glutamate receptors. Biol Psychiatry 63: 86–91.
Panula P, Yang HY, Costa E (1984). Histamine-containing neurons in the rat hypothalamus. Proc Natl Acad Sci USA 81: 2572–2576.
Perry W, Minassian A, Feifel D, Braff DL (2001). Sensorimotor gating deficits in bipolar disorder patients with acute psychotic mania. Biol Psychiatry 50: 418–424.
Raymond EG, Creinin MD, Barnhart KT, Lovvorn AE, Rountree RW, Trussell J (2000). Meclizine for prevention of nausea associated with use of emergency contraceptive pills: a randomized trial. Obstet Gynecol 95: 271–277.
Reynolds S, Lane SJ (2008). Diagnostic validity of sensory over-responsivity: a review of the literature and case reports. J Autism Dev Disord 38: 516–529.
Richelson E, Souder T (2000). Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds. Life Sci 68: 29–39.
Roegge CS, Perraut C, Hao X, Levin ED (2007). Histamine H1 receptor involvement in prepulse inhibition and memory function: relevance for the antipsychotic actions of clozapine. Pharmacol Biochem Behav 86: 686–692.
Silverstein LD, Graham FK, Calloway JM (1980). Preconditioning and excitability of the human orbicularis oculi reflex as a function of state. Electroencephalogr Clin Neurophysiol 48: 406–417.
Swerdlow NR, Benbow CH, Zisook S, Geyer MA, Braff DL (1993). A preliminary assessment of sensorimotor gating in patients with obsessive compulsive disorder. Biol Psychiatry 33: 298–301.
Swerdlow NR, Braff DL, Geyer MA (2000). Animal models of deficient sensorimotor gating: what we know, what we think we know, and what we hope to know soon. Behav Pharmacol 11: 185–204.
Swerdlow NR, Hartman PL, Auerbach PP (1997). Changes in sensorimotor inhibition across the menstrual cycle: implications for neuropsychiatric disorders. Biol Psychiatry 41: 452–460.
Swerdlow NR, Keith VA, Braff DL, Geyer MA (1991). Effects of spiperone, raclopride, SCH 23390 and clozapine on apomorphine inhibition of sensorimotor gating of the startle response in the rat. J Pharmacol Exp Ther 256: 530–536.
Swerdlow NR, Paulsen J, Braff DL, Butters N, Geyer MA, Swenson MR (1995). Impaired prepulse inhibition of acoustic and tactile startle response in patients with Huntington's disease. J Neurol Neurosurg Psychiatry 58: 192–200.
Swerdlow NR, Talledo J, Sutherland AN, Nagy D, Shoemaker JM (2006). Antipsychotic effects on prepulse inhibition in normal ‘low gating' humans and rats. Neuropsychopharmacology 31: 2011–2021.
van der Linden D, Massar SA, Schellekens AF, Ellenbroek BA, Verkes RJ (2006). Disrupted sensorimotor gating due to mental fatigue: preliminary evidence. Int J Psychophysiol 62: 168–174.
Vollenweider FX, Barro M, Csomor PA, Feldon J (2006). Clozapine enhances prepulse inhibition in healthy humans with low but not with high prepulse inhibition levels. Biol Psychiatry 60: 597–603.
Zlott DA, Byrne M (2010). Mechanisms by which pharmacologic agents may contribute to fatigue. PM R 2: 451–455.
Acknowledgements
This research was funded by the Wallace Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Larrauri, J., Kelley, L., Jenkins, M. et al. Meclizine Enhancement of Sensorimotor Gating in Healthy Male Subjects with High Startle Responses and Low Prepulse Inhibition. Neuropsychopharmacol 39, 651–659 (2014). https://doi.org/10.1038/npp.2013.248
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2013.248