Abstract
Major depression is associated with both dysregulated glutamatergic neurotransmission and fewer astrocytes in limbic areas including the prefrontal cortex (PFC). These deficits may be functionally related. Notably, astrocytes regulate glutamate levels by removing glutamate from the synapse via the glutamate transporter (GLT-1). Previously, we demonstrated that central blockade of GLT-1 induces anhedonia and c-Fos expression in the PFC. Given the role of the PFC in regulating mood, we hypothesized that GLT-1 blockade in the PFC alone would be sufficient to induce anhedonia in rats. We microinjected the GLT-1 inhibitor, dihydrokainic acid (DHK), into the PFC and examined the effects on mood using intracranial self-stimulation (ICSS). At lower doses, intra-PFC DHK produced modest increases in ICSS thresholds, reflecting a depressive-like effect. At higher doses, intra-PFC DHK resulted in cessation of responding. We conducted further tests to clarify whether this total cessation of responding was related to an anhedonic state (tested by sucrose intake), a nonspecific result of motor impairment (measured by the tape test), or seizure activity (measured with electroencephalogram (EEG)). The highest dose of DHK increased latency to begin drinking without altering total sucrose intake. Furthermore, neither motor impairment nor evidence of seizure activity was observed in the tape test or EEG recordings. A decrease in reward value followed by complete cessation of ICSS responding suggests an anhedonic-like effect of intra-PFC DHK; a conclusion that was substantiated by an increased latency to begin sucrose drinking. Overall, these results suggest that blockade of astrocytic glutamate uptake in the PFC is sufficient to produce anhedonia, a core symptom of depression.
Similar content being viewed by others
INTRODUCTION
Anhedonia and cognitive dysfunction are two of the most debilitating symptoms of major depressive disorder (MDD) (Drevets, 2001). Although brain imaging studies suggest that these symptoms may be due, in part, to dysfunction in cortical regions that control emotionality (Bremner et al, 2002; Drevets, 2000; Lorenzetti et al, 2009; Malykhin et al, 2011; Sheline, 2003), little progress has been made in identifying the underlying pathophysiology of MDD. The medications that currently treat MDD specifically target the serotonergic and noradrenergic systems and produce eventual therapeutic effects via mechanisms that are not fully understood (Duman and Monteggia, 2006; Nestler and Carlezon, 2006) and although these medications provide symptom relief for some, up to 60% of patients with unipolar depression suffer from treatment-resistant depression (Fava, 2003). Furthermore, with over 50% of suicide victims having a previous diagnosis of treatment-resistant depression (Henriksson et al, 1993), the need for improved therapeutics to better treat depression has become a global health concern. Novel insights into regional cortical abnormalities that accompany MDD have identified cellular and molecular changes in the prefrontal cortex (PFC) that may be key regulators of depression-induced anhedonia (for review, see Drevets, 2001; Hercher et al, 2009). This work is designed to model cell loss in the PFC in animals to better understand whether glial networks could represent novel treatment targets for depression.
MDD is associated with regional volumetric changes throughout a variety of limbic regions; however, all areas of the PFC consistently display volumetric reductions in imaging studies (Bremner et al, 2002; Drevets, 2000; Drevets et al, 1997; Lim et al, 2012; Malykhin et al, 2011; Salvadore et al, 2011). Decreases in PFC volume have been attributed to reductions in glial cells (Cotter et al, 2002; Hercher et al, 2009; Ongur et al, 1998; Rajkowska, 2000; Rajkowska et al, 1999) and to a lesser extent, neuronal atrophy (Cotter et al, 2002; Law and Harrison, 2003; Rajkowska, 2000; Rajkowska et al, 1999). Glial cell deficits in MDD are accompanied by a decrease in astrocytic markers in the PFC such as glial fibrillary acidic protein (Miguel-Hidalgo et al, 2000; Si et al, 2004) and glutamine synthetase (Choudary et al, 2005; Sequeira et al, 2009; Yildiz-Yesiloglu and Ankerst, 2006), as well as morphological changes including swelling of the size and shape of astrocytes (Miguel-Hidalgo and Rajkowska, 2003). Furthermore, downregulation in the high-affinity astrocytic glutamate transporters, SLC1A2 (EAAT2) and SLC1A3 (EAAT1), have been identified in prefrontal cortical areas of human post-mortem tissue; abnormalities that contribute to elevated glutamate levels in the PFC (Choudary et al, 2005). These findings may suggest defective or compromised metabolism of both neurotransmitters and brain glucose in the PFC of depressed patients. As astrocytes account for over 90% of the uptake and metabolism of the excitatory neurotransmitter glutamate (Chaudhry et al, 1995; Haugeto et al, 1996; Lehre and Danbolt, 1998; Lehre et al, 1995), deficient astrocyte function and decreased EAAT2 transporters, accompanied by increased AMPA receptors in the PFC of depressed patients (Choudary et al, 2005; Sequeira et al, 2009), may contribute to the increased activation of the PFC that is seen in depressed patients (Hashimoto et al, 2007; Kugaya and Sanacora, 2005; Milak et al, 2005; Paul and Skolnick, 2003; Sanacora et al, 2008; Valentine and Sanacora, 2009). Furthermore, increased activity in the PFC is positively associated with symptom severity in depression (Milak et al, 2005) and both deep brain stimulation (DBS) and electroconvulsive therapy, which are effective for treatment-resistant depression, are thought to normalize activity of the corticolimbic circuit (Mayberg et al, 2005; Michael et al, 2003; Pfleiderer et al, 2003).
It is not clear to what extent elevated glutamate levels in specific limbic areas can account for the symptoms of depression; however, preclinical studies have provided some insight into this mechanism. Cortical PFC glial ablation (Banasr and Duman, 2008), as well as pharmacological blockade of astrocytic glutamate uptake in the amygdala (Lee et al, 2007) and ventral tegmental area (Herberg and Rose, 1990), is sufficient to induce depressive-like behavior in rats. Furthermore, we have previously demonstrated that intracerebroventricular (ICV) infusion of the astrocytic glutamate reuptake inhibitor dihydrokainic acid (DHK) produces depressive-like symptoms in rats and induces c-Fos expression in cortical regions such as the infralimbic region of the PFC (Bechtholt-Gompf et al, 2010). As the PFC controls aspects of executive function and cognitive processing, in the present report we examined the effects of intra-PFC DHK infusion in rats using tests that quantify anhedonic-like behavior.
Intracranial self-stimulation (ICSS) is a powerful method used to quantify motivation (Carlezon and Chartoff, 2007). As increases in ICSS thresholds can be reflective of either diminished reward or aversion and discomfort, we chose to augment our ICSS findings with a sucrose-drinking test in order to assess if intra-PFC DHK infusion alone is sufficient to replicate the anhedonic-like symptoms found with ICV DHK infusion. Also, as increases in cortical glutamate levels can cause seizure activity and induce changes in locomotion, we chose to assess these parameters using the modified sticky tape test, a measure of forepaw coordination, and electroencephalogram (EEG) recordings to assess seizure activity. We hypothesized that intra-PFC DHK infusion would be sufficient to produce an anhedonic-like phenotype that could not be attributed to seizure activity or altered locomotion.
MATERIALS AND METHODS
Animals
A total of 23 male Sprague-Dawley rats (Charles River Laboratories) weighing 300–350 g at the time of surgery were used in these studies. After surgery, the rats were housed singly and maintained on a 12-h light/dark cycle with food and water available ad libitum. Each experiment consisted of naive cohorts of rats except for the tape test, as detailed below. Procedures were conducted between 0900 and 1800 h with the approval of the McLean Hospital Institutional Animal Care and Use Committee and within the guidelines of The National Research Council's Guide for Care and Use of Laboratory Animals.
Drugs
DHK (Tocris Bioscience, Ellisville, MO) blocks the uptake of glutamate into astrocytes (Anderson and Swanson, 2000; Arriza et al, 1994), resulting in increased extrasynaptic glutamate levels. This effect has been shown both ex vivo (Robinson et al, 1991) and in vivo (Fallgren and Paulsen, 1996). DHK does not bind to AMPA/kainite or other glutamate receptors with significant affinity (Johnston et al, 1979), indicating selectivity for glutamate transporter (GLT-1). Doses of DHK were derived from previously published behavioral data (Bechtholt-Gompf et al, 2010; Lee et al, 2007). DHK was dissolved in PBS (pH 7.4) as previously reported (Lee et al, 2007). DHK (0.0, 1.563, 3.125, or 6.25 nmol in 1 μl; 0.5 μl/side) was delivered at a rate of 0.25 μl/min and injectors were left in place for 1 min after the infusion to allow for adequate diffusion.
Surgery
Rats were implanted with monopolar stainless steel stimulating electrodes (0.25 mm diameter) aimed at the medial forebrain bundle (10° angle; from bregma 4.2 mm anterior +1.7 mm lateral, 7.9 mm ventral from the dura) and/or bilateral PFC cannulae (26 ga) aimed at the infralimbic area of the PFC (with ICSS electrode for long-term studies: from bregma 2.4 mm posterior, 0.75 mm lateral, 2.8 mm lateral; without ICSS electrode for short-term studies: from bregma 2.8 mm posterior, 0.75 mm lateral, 2.6 mm ventral from the dura with an additional 1.5 mm injector projection) (Paxinos and Watson, 2007). Rats were anesthetized with Nembutal (65 mg/kg, IP) and small burr holes were made in the skull through which an electrode and/or guide cannula was lowered to the specified depth under stereotaxic guidance. The electrodes and guide cannulae were fastened to the skull using stainless steel screws and dental acrylic. The rats were allowed 7 days of recovery before the start of experimentation.
Intracranial Self-Stimulation
ICSS was conducted to assess changes in hedonic state after DHK treatment. The rats were trained on a fixed-ratio-one (FR1) schedule of reinforcement to obtain brain stimulation as previously described (Bechtholt-Gompf et al, 2010; Carlezon and Chartoff, 2007). Briefly, rats were trained to lever press for a 0.5-s pulse train. The stimulation current (100–300 μA) was adjusted for each animal to the lowest level that sustained responding at a rate greater than 1 lever press/s. After stable responding was reached, the rats were trained to lever press for a series of 15 descending frequencies (158–32 Hz at descending 0.05 log10 units), which was termed a ‘pass’ after completion of all 15 descending frequencies. Daily training sessions consisted of 4 consecutive passes, which typically spanned 6–8 weeks. To characterize the relationship between response strength and reward magnitude, the least-squares best fit line was plotted across the frequencies that maintained responding at 20, 30, 40, 50, and 60% of the maximum response. From this function, the ICSS threshold was defined as the frequency at which the function intersects with the x-axis (θ-0; T0) (Miliaressis et al, 1986), which represents the point at which the stimulation becomes rewarding. The maximum rate of responding (Max Rate) was calculated in parallel to assess potential performance impairments. Drug test sessions began the day after mean ICSS thresholds varied by <±10% across five training sessions. On test days, rats were allowed to press through three baseline passes, infused bilaterally intra-PFC with one of four doses of DHK (total bilateral infusion: 0.0, 1.563, 3.125, or 6.25 nmol in 1 μl) and then subjected to three additional passes. Each animal was administered each dose in increasing order on separate test days with treatment days interspersed with baseline recovery days.
Sucrose Intake
Attenuation of sucrose consumption is a commonly used animal model of anhedonia and can be observed after a wide range of stressors (Muscat and Willner, 1992; Papp et al, 1991). Sucrose intake was assessed over a 30-min period to determine whether DHK induced behavior consistent with an anhedonic state. Rats were presented three times a week for 1 h with sucrose drinking bottles (10% solution) for 9 weeks to assess baseline intake without food and water deprivation. Drug test sessions began 1 day after mean sucrose intake varied by <±10% on previous testing day, with treatment days interspersed with baseline recovery days. On testing days, rats were bilaterally infused with vehicle or DHK (6.25 nmol in 1 μl) and then subjected to a 30-min sucrose intake test.
Modified Adhesive Removal (Sticky Tape) Test
As higher doses of intra-PFC DHK resulted in complete cessation of ICSS responding and reductions in Max Rate, motor control was assessed to determine whether DHK induces nonspecific motor effects that could account for cessation of responding. The modified sticky tape test (MST) is used as an assessment of somatosensory/fine motor coordination impairment in rats (Bouet et al, 2009; Komotar et al, 2007). Rats were tested 1 week after completion of the sucrose intake test. Before DHK testing, the MST was performed daily for 1 week to assess baseline removal times. On the test days, groups were counterbalanced for treatment order and then bilaterally infused with either vehicle or DHK (6.25 nmol in 1 μl) immediately before adhesive tape (3.0 cm long; 1.0 cm wide) was applied to both forepaws. The time required for rats to remove both pieces of tape fully from each paw was recorded and the average amount of time to remove tape from both forelimbs was calculated. On the next day, rats were subjected to the MST without intracranial treatment to confirm that no residual deviation from baseline was detected. On the second and final test day (24 h after baseline was reached following the first treatment), rats were given the opposite treatment compared with the first test day and infusion and testing procedures were executed as above.
EEG Surgery and Testing
EEG testing was performed to assess whether intra-PFC DHK can induce seizures that would interfere with ICSS responding or sucrose intake. Four EEG screw electrodes were implanted into the skull, in the frontal (two) and the parietal (two) bones of each side, and two flexible electromyogram (EMG) wire electrodes (Plastics One, Roanoke, VA) were placed into the neck muscles. The free ends of the leads were fit into a socket that was attached to the skull with dental cement. At 2 weeks after surgery, the sockets were connected via flexible recording cables and a commutator (Plastics One) to a 16-channel analog amplifier (A-M systems) and the signal was digitized using an analog to digital converter card running Vital Recorder (Kissei Comtec) on a Dell PC. Video recordings were also synchronized to the EEG/EMG traces using this software. Following 48 h of acclimation to the sound-attenuated recording chamber with the EEG/EMG cable attached, rats were recorded for a total of 24 h to assess baseline, post-vehicle injection, post-DHK injection, and recovery EEG/EMG signals at a sampling rate of 256 Hz. No filter was applied for the recording and rats were left undisturbed following injections. Wake/sleep states were automatically scored and manually checked in 4 s epochs using ‘SleepSign for Animal’ software (Kissei). Following this, the data were first visually inspected for movement-associated noise artifacts (excluded from further analyses). Then, EEG power spectra were computed for consecutive 4 s epochs between 0.75 and 50 Hz using a fast Fourier transform routine. The data were collapsed into 0.25 Hz bins (‘FFT point’=1024), power densities were summed over the entire frequency range, and each frequency bin was standardized by expressing it as a percentage relative to the total power within each 4 s epoch. The standardized data were then averaged between rats undergoing each treatment (vehicle or 6.25 nmol DHK). Additionally, the power spectral density at different frequency ranges was computed: δ (1–4.5 Hz), θ (5–8.5 Hz), α (9–13.5 Hz), β (14–31.5 Hz) and γ (lower γ or γ1: 32–58 Hz) to compare the 15 and 30 min following vehicle injections with the 15 or 30 min following DHK injections.
Histological Verification
Following the last test session, rats were anesthetized with sodium pentobarbital (130 mg/kg IP) and transcardially perfused with 0.9% NaCl followed by 4% paraformaldehyde in isotonic sodium phosphate-buffered saline (PBS). Following perfusion, brains were removed and postfixed for 24 h and then cryoprotected with 30% sucrose. Frozen 40 μm coronal sections were cut through the site of the microinjectors using a microtome and collected in PBS with 0.05% sodium azide. Sections were then mounted onto slides and stained with cresyl violet. Rats given microinjections outside of the infra-limbic PFC were eliminated from all analyses. An example photomicrograph of infra-limbic bilateral injection site is shown in Figure 1.
Intra-PFC DHK injection sites. (a) Schematic of the infralimbic region of the PFC indicating location of placements of bilateral cannulae (Paxinos and Watson, 2007). The box indicates field of view in (b). (b) Placements of bilateral cannulae of a representative rat indicating guide cannulae and obturator.
RESULTS
Effects of DHK on ICSS
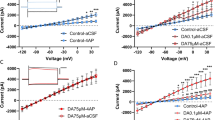
Intra-PFC DHK dose-dependently increased ICSS thresholds (Figure 2a). At the higher doses, intra-PFC DHK induced complete cessation of responding in some rats. In those cases (n=3/8; 3.125 nmol and n=5/8; 6.25 nmol), the highest stimulation frequency available was used to calculate the threshold. One-way repeated measures ANOVA revealed significant main effects of dose (F(3, 21)=9.9; p<0.0001) and time (F(1, 7)=20.3; p<0.01), and a dose × time interaction (F(7, 21)=4.7; p<0.05). Follow-up Bonferroni post hoc comparisons showed that rats treated with DHK either completely stopped responding or required significantly higher minimum stimulation frequencies to maintain responding in the first 15 min after DHK infusion compared with both vehicle-treated and 1.563 nmol-treated rats (6.25 nmol; p<0.05). Figure 2b shows the effects of intra-PFC DHK on maximum response rates (Max Rates). One-way repeated measures ANOVA revealed statistically significant main effects of dose (F(3, 21)=11.2; p<0.001) and time (F(1, 7)=9.9; p<0.05), and a dose × time interaction (F(7, 21)=6.4; p<0.05). Follow-up Bonferroni post hoc comparisons revealed that rats treated with DHK had significantly blunted Max Rates during the first 15 min after DHK infusion, with the highest dose reaching statistical significance relative to vehicle treatment (6.25 nmol; p<0.05). Decreased Max Rates can be the result of decreased hedonic value of stimulation (Do Carmo et al, 2009) or reduced performance ability (Carlezon and Chartoff, 2007). Figure 3 represents the characteristic rightward shift of the rate-frequency function (increased T0) from a representative rat that did not completely stop responding, indicating an anhedonic-like (reward decreasing) effect.
(a) Effect of intra-PFC DHK (1.563, 3.125, or 6.25 nmol) on ICSS thresholds over 45 min after infusion. Inset represents effects on T0 within the first 15 min. Follow-up comparisons showed that the effects of DHK were short in duration and dose dependent. Significant effects were observed during the first 15 min after DHK infusion and the highest dose of DHK yielded greater thresholds. Time × dose interaction: p<0.05. *Significantly different from the vehicle and 1.563 nmol-treated group, p<0.05 (n=8). (b) Effect of intra-PFC DHK (1.563, 3.125, or 6.25 nmol) on ICSS maximum response rate over 45 min after infusion. Inset represents effects on Max Rates within the first 15 min. Significant effects were observed during the first 15 min after DHK infusion with the highest dose of DHK yielding significant decreases in Max Rate. Time × dose interaction: p<0.05. *Significantly different from the vehicle group, p<0.05 (n=8).
ICSS rate-frequency functions from a representative rat at baseline and after treatment with 6.25 nmol intra-PFC DHK. Changes in motivation are indicated by lateral shifts in the frequency response curve. Shifts to the right of this frequency response curve indicate that higher frequencies of medial forebrain bundle stimulation are required to support lever pressing, suggesting an anhedonic-like state. Vertical shifts in the frequency response curve can also be indicative of changes in motivation; however, it is difficult to distinguish these effects from the effects in performance capability. These curves show that intra-PFC DHK caused both a downward vertical shift, indicative of decreased lever pressing, and a rightward shift in rate-frequency function, suggesting a depressed-like mood.
Effects of DHK on Sucrose Intake
Similar to the anhedonic-like effect of intra-PFC DHK during ICSS, a paired-samples t-test suggested that intra-PFC DHK (6.25 nmol) increased latency to begin drinking sucrose (t(7)=−2.4; p<0.05) without altering total sucrose intake (t(7)=−1.7; p=0.1; Figure 4a and b). Furthermore, rats treated with DHK did not spend more time compared with vehicle-treated rats performing behaviors other than sucrose drinking (eg, walking around, rearing, sniffing; t(7)=0.2; p=0.847).
(a) Effect of intra-PFC DHK on latency to begin drinking a 10% sucrose solution and total sucrose intake over a 30-min testing period (b). DHK in the PFC significantly increased latency to begin drinking sucrose and had no significant effect on total sucrose intake. *Significantly different from vehicle group, p<0.05 (n=8). (c) Effect of intra-PFC DHK on average tape removal time in the modified sticky tape test. Intra-PFC DHK treatment did not significantly increase overall time spent removing tape from both forepaws compared with vehicle, suggesting intact somatosensory function (n=6).
Effects of DHK on the Modified Tape Test
As shown in Figure 4c, intra-PFC DHK treatment did not significantly increase the time required for rats to remove the tape from their paws compared with vehicle treatment. A paired samples t-test indicated no significant differences in tape removal time between treatment conditions (t(5)=−1.4; p=0.24). These data suggest that somatosensory function is intact in DHK-treated rats, supporting the hypothesis that the potentially anhedonic effects of intra-PFC DHK that we observed in both ICSS and sucrose intake tests are not an artifact of motor impairment.
Effects of DHK on EEG
Close visual examination (see traces in Figure 5a) revealed a typical waking EEG following injection of either vehicle or DHK. No large-amplitude spike and wave discharges, as are characteristic during ictal seizures, were noted in any of the traces. The 15 min power spectrum across the entire frequency range (0.75–58 Hz) was also typical of an awake and alert rat (Figure 5b). Moreover, the power spectra following vehicle injection did not differ significantly from those following DHK infusion. These results suggest that significant global impairments of cortical activity do not result from DHK treatment. Human studies have shown that patients with MDD display increased power in the α frequency range (9–13.5 Hz) during quiet wakefulness, which is gradually reversed in the course of antidepressant treatment (for review, see Badrakalimuthu et al, 2011). We therefore calculated the relative power in the δ (1–4.5 Hz), θ (5–8.5 Hz), α (9–13.5 Hz), β (14–31.5 Hz), and lower γ (32–58 Hz) frequency ranges and compared these values between vehicle and DHK injections. The δ power, a measure of sleepiness, was increased (169.3±56.7%), although not significantly compared with vehicle (t(3)=1.03, p=0.38), and the rats were not asleep during the 15 min following either vehicle or DHK injections. The θ and β power remained the same following DHK relative to vehicle treatment (113.7±10.3%, t(3)=1.08, p=0.36 and 97.2±6.8%, t(3)=0.76, p=0.50 respectively), whereas γ power was somewhat attenuated following DHK (80.6±6.6%, t(3)=2.64, p=0.08). Interestingly, the α power in the rats during the 30 min following DHK was strongly increased (163.0±23.0%, t(3)=3.67, p=0.03) compared with vehicle.
(a) EEG traces (15 min time scale) following injection of vehicle (top) or 6.25 nmol DHK (bottom). Rats were awake for at least 15 min. The typical wake EEG pattern depicted here was observed following either saline or DHK injection in all rats (n=5). (b) Power spectrum across the entire frequency range of 0.75–50 Hz after either vehicle or intra-PFC DHK infusion. Both power spectra are typical of what one would expect in an awake rat, suggesting no significant global impairments of cortical activity after DHK treatment.
DISCUSSION
The major finding we report is that blockade of astrocytic glutamate uptake in the PFC induces a pro-depressive phenotype in the rat. Specifically, pharmacological reduction of glial glutamate uptake diminished the rewarding effects of medial forebrain bundle stimulation and sucrose drinking. As a lack of astrocytic function can induce some signs of depression, these findings, along with previous reports, suggest that a deficit of astrocytes in the PFC of depressed patients may be a key pathophysiologic element of MDD and, specifically, the symptom of anhedonia.
Intra-PFC DHK increased ICSS thresholds (T0) and at the higher doses tested induced a complete cessation of responding in some rats, consistent with an anhedonic-like effect. This interpretation was substantiated by another measure of reward state, sucrose intake, wherein intra-PFC DHK increased the latency to begin drinking a palatable sucrose solution. These findings demonstrate that reduced astrocyte function is associated with depressive symptoms and are consistent with previous reports showing that central (Bechtholt-Gompf et al, 2010) or amygdalar (Lee et al, 2007) blockade of astrocytic glutamate uptake induces signs of depression including anhedonia (Bechtholt-Gompf et al, 2010), cognitive impairment (Bechtholt-Gompf et al, 2010), social avoidance (Lee et al, 2007), and disrupted circadian rhythms (Lee et al, 2007). These findings are also in agreement with another report wherein astrocyte ablation specifically in the PFC decreased sucrose intake and increased response to novelty and immobility in the forced swimming test (Banasr and Duman, 2008).
Intra-PFC DHK also had profound effects on maximal rates of responding (max rate) in the ICSS test. This effect can be the result of impaired motor performance (Carlezon and Chartoff, 2007), as manipulations that physically interfere with lever pressing, such as making pressing more difficult or muscle relaxants, decrease response rate (Miliaressis et al, 1986). However, this result can also be indicative of the induction of anhedonia (Bechtholt-Gompf et al, 2010), as either decreasing the intensity of the stimulation or increasing the response requirement decrease maximum response rates (Do Carmo et al, 2009). The complex ICSS outcome is shown graphically in Figure 3, which demonstrates that intra-PFC DHK caused a rightward shift (indicative of increased T0) and a downward shift (indicative of decreased max rate). DHK also decreased the latency for rats to begin drinking a palatable sucrose solution, an effect that may likewise be indicative of motor impairment or anhedonia. As either impaired performance or anhedonia could result in increased latency to drink sucrose or decreased rate of responding in the ICSS test, and because the lack of responding in the ICSS test was complete in some rats, we conducted the tape removal test to ensure that fine motor skills were intact after intra-PFC DHK infusion. In this test DHK did not significantly increase the latency to remove the tape from both paws, suggesting that the rats likely had sufficient motor skills to press the lever. Although not significant, there was a slight increase in latency to remove the tape in rats infused intra-PFC with the highest dose of DHK. We suggest that this result might also be associated with decreased motivation as the rats have to ‘want’ to remove the tape.
DHK is known to increase extracellular glutamate levels (Fallgren and Paulsen, 1996) an effect that could induce seizure activity (for review, see Bradford, 1995) and therefore potentially confound responding in the ICSS and sucrose tests. This seemed unlikely because rats were not impaired in the tape test after intra-PFC DHK, but nevertheless we sought to determine whether seizures were induced by this treatment. No seizure activity was observed, suggesting that the effects we obtained in the ICSS and the sucrose tests were likely the result of a change in mood-like state or motivation. This interpretation was indicated by normal EEG patterns lacking large-amplitude spike and wave discharges and demonstrated by overlapping power spectra for vehicle- and DHK-treated rats. We also analyzed the relative power of relevant frequency ranges. These data proved interesting in that α power was significantly increased after intra-PFC DHK treatment. This finding is consistent with results observed in depressed patients, in whom α power is increased with illness and normalized with antidepressant treatment (for review, see Badrakalimuthu et al, 2011).
The specific mechanisms through which a paucity of glia could contribute to the depressed phenotype are unknown. However, some data suggest that glutamate dysregulation, and elevated glutamate, in particular, as would be expected with reduced numbers or function of astrocytes, play a role in the expression of symptoms of anxiety and depression, including anhedonia. For example, human data from DBS in treatment-resistant depression suggests that there is a baseline increase in activation of area Cg25 that is normalized by both pharmacological antidepressant and DBS treatment (Mayberg et al, 2005). Structural and connectivity evidence implicates the infralimbic and prelimbic cortical regions of the rat as homologous to area 25 (Ongur and Price, 2000), suggesting increased activity of the infralimbic PFC could lead to anhedonic-like outcomes in animal models. Chronic unpredictable stress—a preclinical model that induces depressive-like symptoms in animals—has been shown to induce astrocytic gap junction dysfunction and consequent decreases in connexin 43, an astrocyte-specific gap junction protein, in the PFC of rats (Sun et al, 2012). The effects of these manipulations have been shown both in vitro and in vivo to be glutamate dependent (Ozog et al, 2002; Zador et al, 2008). These results suggest that depressive-like outcomes correlate with increases in glutamate and astrocyte dysregulation that may lead to increases in glutamate- changes that, therefore, probably contribute to an anhedonic phenotype.
We have shown that decreasing astrocytic glutamate uptake in the PFC can induce some of the symptoms observed in depressed patients, including anhedonia and irregular EEG patterns. This dysfunction was achieved by direct infusion of the GLT-1 inhibitor DHK into PFC, which pharmacologically mimics the dysfunction of astrocytic glutamate uptake observed in patients with depression. These data suggest that the lack of astrocytes observed in MDD patients may have a causal role in producing or mediating some of the symptoms of depression. These data add to the growing body of literature suggesting that the ability to detect alterations in astrocytic function in vivo might serve as a diagnostic criterion for MDD, and that restoration or enhancement of astrocytic function might represent a novel treatment target for some symptoms of depressive disorders.
References
Anderson CM, Swanson RA (2000). Astrocyte glutamate transport: review of properties, regulation, and physiological functions. Glia 32: 1–14.
Arriza JL, Fairman WA, Wadiche JI, Murdoch GH, Kavanaugh MP, Amara SG (1994). Functional comparisons of three glutamate transporter subtypes cloned from human motor cortex. J Neurosci 14: 5559–5569.
Badrakalimuthu R, Swamiraju R, de Waal H (2011). EEG in psychiatric practice: to do or not to do? Adv Psychiatr Treat 17: 114–121.
Banasr M, Duman RS (2008). Glial loss in the prefrontal cortex is sufficient to induce depressive-like behaviors. Biol Psychiatry 64: 863–870.
Bechtholt-Gompf AJ, Walther HV, Adams MA, Carlezon Jr WA, Ongur D, Cohen BM (2010). Blockade of astrocytic glutamate uptake in rats induces signs of anhedonia and impaired spatial memory. Neuropsychopharmacology 35: 2049–2059.
Bouet V, Boulouard M, Toutain J, Divoux D, Bernaudin M, Schumann-Bard P et al (2009). The adhesive removal test: a sensitive method to assess sensorimotor deficits in mice. Nat Protoc 4: 1560–1564.
Bradford HF (1995). Glutamate, GABA and epilepsy. Prog Neurobiol 47: 477–511.
Bremner JD, Vythilingam M, Vermetten E, Nazeer A, Adil J, Khan S et al (2002). Reduced volume of orbitofrontal cortex in major depression. Biol Psychiatry 51: 273–279.
Carlezon Jr WA, Chartoff EH (2007). Intracranial self-stimulation (ICSS) in rodents to study the neurobiology of motivation. Nat Protoc 2: 2987–2995.
Chaudhry FA, Lehre KP, van Lookeren Campagne M, Ottersen OP, Danbolt NC, Storm-Mathisen J (1995). Glutamate transporters in glial plasma membranes: highly differentiated localizations revealed by quantitative ultrastructural immunocytochemistry. Neuron 15: 711–720.
Choudary PV, Molnar M, Evans SJ, Tomita H, Li JZ, Vawter MP et al (2005). Altered cortical glutamatergic and GABAergic signal transmission with glial involvement in depression. Proc Natl Acad Sci USA 102: 15653–15658.
Cotter D, Mackay D, Chana G, Beasley C, Landau S, Everall IP (2002). Reduced neuronal size and glial cell density in area 9 of the dorsolateral prefrontal cortex in subjects with major depressive disorder. Cereb Cortex 12: 386–394.
Do Carmo GP, Folk JE, Rice KC, Chartoff E, Carlezon Jr WA, Negus SS (2009). The selective non-peptidic delta opioid agonist SNC80 does not facilitate intracranial self-stimulation in rats. Eur J Pharmacol 604: 58–65.
Drevets WC (2000). Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res 126: 413–431.
Drevets WC (2001). Neuroimaging and neuropathological studies of depression: implications for the cognitive-emotional features of mood disorders. Curr Opin Neurobiol 11: 240–249.
Drevets WC, Price JL, Simpson Jr JR, Todd RD, Reich T, Vannier M et al (1997). Subgenual prefrontal cortex abnormalities in mood disorders. Nature 386: 824–827.
Duman RS, Monteggia LM (2006). A neurotrophic model for stress-related mood disorders. Biol Psychiatry 59: 1116–1127.
Fallgren AB, Paulsen RE (1996). A microdialysis study in rat brain of dihydrokainate, a glutamate uptake inhibitor. Neurochem Res 21: 19–25.
Fava M (2003). Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 53: 649–659.
Hashimoto K, Sawa A, Iyo M (2007). Increased levels of glutamate in brains from patients with mood disorders. Biol Psychiatry 62: 1310–1316.
Haugeto O, Ullensvang K, Levy LM, Chaudhry FA, Honore T, Nielsen M et al (1996). Brain glutamate transporter proteins form homomultimers. J Biol Chem 271: 27715–27722.
Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsa ET, Kuoppasalmi KI et al (1993). Mental disorders and comorbidity in suicide. Am J Psychiatry 150: 935–940.
Herberg LJ, Rose IC (1990). Excitatory amino acid pathways in brain-stimulation reward. Behav Brain Res 39: 230–239.
Hercher C, Turecki G, Mechawar N (2009). Through the looking glass: examining neuroanatomical evidence for cellular alterations in major depression. J Psychiatr Res 43: 947–961.
Johnston GA, Kennedy SM, Twitchin B (1979). Action of the neurotoxin kainic acid on high affinity uptake of L-glutamic acid in rat brain slices. J Neurochem 32: 121–127.
Komotar RJ, Kim GH, Sughrue ME, Otten ML, Rynkowski MA, Kellner CP et al (2007). Neurologic assessment of somatosensory dysfunction following an experimental rodent model of cerebral ischemia. Nat Protoc 2: 2345–2347.
Kugaya A, Sanacora G (2005). Beyond monoamines: glutamatergic function in mood disorders. CNS Spectr 10: 808–819.
Law AJ, Harrison PJ (2003). The distribution and morphology of prefrontal cortex pyramidal neurons identified using anti-neurofilament antibodies SMI32, N200 and FNP7. Normative data and a comparison in subjects with schizophrenia, bipolar disorder or major depression. J Psychiatr Res 37: 487–499.
Lee Y, Gaskins D, Anand A, Shekhar A (2007). Glia mechanisms in mood regulation: a novel model of mood disorders. Psychopharmacology 191: 55–65.
Lehre KP, Danbolt NC (1998). The number of glutamate transporter subtype molecules at glutamatergic synapses: chemical and stereological quantification in young adult rat brain. J Neurosci 18: 8751–8757.
Lehre KP, Levy LM, Ottersen OP, Storm-Mathisen J, Danbolt NC (1995). Differential expression of two glial glutamate transporters in the rat brain: quantitative and immunocytochemical observations. J Neurosci 15 (3 Pt 1): 1835–1853.
Lim HK, Jung WS, Ahn KJ, Won WY, Hahn C, Lee SY et al (2012). Regional cortical thickness and subcortical volume changes are associated with cognitive impairments in the drug-naive patients with late-onset depression. Neuropsychopharmacology 37: 838–849.
Lorenzetti V, Allen NB, Fornito A, Yucel M (2009). Structural brain abnormalities in major depressive disorder: a selective review of recent MRI studies. J Affect Disord 117: 1–17.
Malykhin NV, Carter R, Hegadoren KM, Seres P, Coupland NJ (2011). Fronto-limbic volumetric changes in major depressive disorder. J Affect Disord 36: 1104–1113.
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C et al (2005). Deep brain stimulation for treatment-resistant depression. Neuron 45: 651–660.
Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B (2003). Metabolic changes within the left dorsolateral prefrontal cortex occurring with electroconvulsive therapy in patients with treatment resistant unipolar depression. Psychol Med 33: 1277–1284.
Miguel-Hidalgo JJ, Baucom C, Dilley G, Overholser JC, Meltzer HY, Stockmeier CA et al (2000). Glial fibrillary acidic protein immunoreactivity in the prefrontal cortex distinguishes younger from older adults in major depressive disorder. Biol Psychiatry 48: 861–873.
Miguel-Hidalgo JJ, Rajkowska G (2003). Comparison of prefrontal cell pathology between depression and alcohol dependence. J Psychiatr Res 37: 411–420.
Milak MS, Parsey RV, Keilp J, Oquendo MA, Malone KM, Mann JJ (2005). Neuroanatomic correlates of psychopathologic components of major depressive disorder. Arch Gen Psychiatry 62: 397–408.
Miliaressis E, Rompre PP, Laviolette P, Philippe L, Coulombe D (1986). The curve-shift paradigm in self-stimulation. Physiol Behav 37: 85–91.
Muscat R, Willner P (1992). Suppression of sucrose drinking by chronic mild unpredictable stress: a methodological analysis. Neurosci Biobehav Rev 16: 507–517.
Nestler EJ, Carlezon Jr WA (2006). The mesolimbic dopamine reward circuit in depression. Biol Psychiatry 59: 1151–1159.
Ongur D, Drevets WC, Price JL (1998). Glial reduction in the subgenual prefrontal cortex in mood disorders. Proc Natl Acad Sci USA 95: 13290–13295.
Ongur D, Price JL (2000). The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex 10: 206–219.
Ozog MA, Siushansian R, Naus CC (2002). Blocked gap junctional coupling increases glutamate-induced neurotoxicity in neuron-astrocyte co-cultures. J Neuropathol Exp Neurol 61: 132–141.
Papp M, Willner P, Muscat R (1991). An animal model of anhedonia: attenuation of sucrose consumption and place preference conditioning by chronic unpredictable mild stress. Psychopharmacology (Berl) 104: 255–259.
Paul IA, Skolnick P (2003). Glutamate and depression: clinical and preclinical studies. Ann NY Acad Sci 1003: 250–272.
Paxinos G, Watson C (2007). The Rat Brain in Stereotaxic Coordinates. Academic Press: New York.
Pfleiderer B, Michael N, Erfurth A, Ohrmann P, Hohmann U, Wolgast M et al (2003). Effective electroconvulsive therapy reverses glutamate/glutamine deficit in the left anterior cingulum of unipolar depressed patients. Psychiatry Res 122: 185–192.
Rajkowska G (2000). Postmortem studies in mood disorders indicate altered numbers of neurons and glial cells. Biol Psychiatry 48: 766–777.
Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY et al (1999). Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biol Psychiatry 45: 1085–1098.
Robinson MB, Hunter-Ensor M, Sinor J (1991). Pharmacologically distinct sodium-dependent L-[3H]glutamate transport processes in rat brain. Brain Res 544: 196–202.
Salvadore G, Nugent AC, Lemaitre H, Luckenbaugh DA, Tinsley R, Cannon DM et al (2011). Prefrontal cortical abnormalities in currently depressed versus currently remitted patients with major depressive disorder. NeuroImage 54: 2643–2651.
Sanacora G, Zarate CA, Krystal JH, Manji HK (2008). Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat Rev Drug Discov 7: 426–437.
Sequeira A, Mamdani F, Ernst C, Vawter MP, Bunney WE, Lebel V et al (2009). Global brain gene expression analysis links glutamatergic and GABAergic alterations to suicide and major depression. PloS One 4: e6585.
Sheline YI (2003). Neuroimaging studies of mood disorder effects on the brain. Biol Psychiatry 54: 338–352.
Si X, Miguel-Hidalgo JJ, O′Dwyer G, Stockmeier CA, Rajkowska G (2004). Age-dependent reductions in the level of glial fibrillary acidic protein in the prefrontal cortex in major depression. Neuropsychopharmacology 29: 2088–2096.
Sun JD, Liu Y, Yuan YH, Li J, Chen NH (2012). Gap junction dysfunction in the prefrontal cortex induces depressive-like behaviors in rats. Neuropsychopharmacology 37: 1305–1320.
Valentine GW, Sanacora G (2009). Targeting glial physiology and glutamate cycling in the treatment of depression. Biochem Pharmacol 78: 431–439.
Yildiz-Yesiloglu A, Ankerst DP (2006). Review of 1H magnetic resonance spectroscopy findings in major depressive disorder: a meta-analysis. Psychiatry Res 147: 1–25.
Zador Z, Weiczner R, Mihaly A (2008). Long-lasting dephosphorylation of connexin 43 in acute seizures is regulated by NMDA receptors in the rat cerebral cortex. Mol Med Report 1: 721–727.
Acknowledgements
Funding for this work was provided by the Jerome Lyle Rappaport Charitable Foundation, the National Alliance for Research on Schizophrenia and Depression, and the National Institute of Mental Health MH087695 (to AJB); the Shervert Frazier Research Institute (to BMC and DO); Englehard Foundation (to BMC); and MH063266 (to WAC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest. Dr Carlezon has a US patent covering the use of κ antagonists in the treatment of depression (Assignee: McLean Hospital) and is a member of a collaborative group, including Dr Cohen, that has submitted a patent application covering the synthesis and use of salvinorin derivatives (Assignees: McLean Hospital and Temple University). In the past 3 years, Dr Carlezon has received compensation for professional services from The American College of Neuropsychopharmacology and Myneurolab.com. Dr Öngür is a Principal Investigator on a research contract with Rules Based Medicine, and has received income from Archives of General Psychiatry for services in 2012. Dr Cohen has three additional pending patents on Pyrimidines to treat bipolar disorders, κ agonists in bipolar mania, and Mitochondrial replacement therapy, and a book on bipolar disorder that has been published by Jossey-Bass/Wiley.
Rights and permissions
About this article
Cite this article
John, C., Smith, K., Van'T Veer, A. et al. Blockade of Astrocytic Glutamate Uptake in the Prefrontal Cortex Induces Anhedonia. Neuropsychopharmacol 37, 2467–2475 (2012). https://doi.org/10.1038/npp.2012.105
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.105
Keywords
This article is cited by
-
A unified model of the biology of peripartum depression
Translational Psychiatry (2023)
-
Astrocyte regulation of synaptic signaling in psychiatric disorders
Neuropsychopharmacology (2023)
-
Dysfunctional serotonergic neuron-astrocyte signaling in depressive-like states
Molecular Psychiatry (2023)
-
Dysregulation of adult hippocampal neuroplasticity in major depression: pathogenesis and therapeutic implications
Molecular Psychiatry (2022)
-
High-fat diet induces depression-like phenotype via astrocyte-mediated hyperactivation of ventral hippocampal glutamatergic afferents to the nucleus accumbens
Molecular Psychiatry (2022)