Abstract
Atomoxetine is a specific inhibitor of the norepinephrine transporter (NET) that has demonstrated efficacy in the treatment of children with attention-deficit hyperactivity disorder (ADHD). We investigated whether polymorphisms in the NET/SLC6A2 gene may influence atomoxetine response in ADHD. Two independent cohorts of 160 and 105 ADHD children treated for 6 weeks with atomoxetine (0.5–1.8 mg/kg per day) were genotyped on CYP2D6, which metabolizes atomoxetine, and 108 single nucleotide polymorphisms in the NET/SLC6A2 gene. Response was defined as a minimum decrease of 25% in ADHD Rating Scale IV-Parent Version and a Clinical Global Impression-Severity (CGI-S) score less than or equal to 2 at week 6. Interindividual response was independent of the genetic variants of CYP2D6. Significant (p<0.05) associations between 20 NET/SLC6A2 single nucleotide polymorphisms (SNPs) and clinical efficacy in atomoxetine responders, compared with non-responders, were observed. The genomic region across exons 4 to 9 of NET/SLC6A2, where 36 SNPs have been genotyped, was associated with treatment response in both cohorts (p<0.01, odds ratio=2.2 and p=0.026, odds ratio=6.3, respectively), in the combined cohort (p<0.01, odds ratio=1.83), and in the subgroup of Caucasians only (p=0.02, odds ratio=1.8). Clinical efficacy of atomoxetine treatment in ADHD shows potential dependence upon a series of genetic polymorphisms of its mechanistic target, the norepinephrine transporter. Taking into account the high heritability of ADHD, the significance of the present finding and replication of a similar haplotype allele sequence result in an independent cohort, it is suggested that further assessment of this region could be useful in determining response to atomoxetine in ADHD.
Similar content being viewed by others
INTRODUCTION
Attention-deficit hyperactivity disorder (ADHD) is a chronic psychiatric condition affecting 5–10% of school-age children. Symptoms of inattention, hyperactivity and impulsivity, leading to familial, social and academic dysfunction are the bases of the diagnosis (Faraone et al, 2005; Thapar et al, 2006). The risk of ADHD in additional children in families with an ADHD child is two to eight times greater than expected by chance. This familial aggregation is believed to be partially explained by genetic factors, as the heritability of ADHD has been reported to be between 75 and 91% (Faraone et al, 2005; Thapar et al, 2006; Masellis et al, 2006). Numerous vulnerability genes have been proposed in ADHD with some convergence for gene coding for the dopamine receptor D4 (Faraone et al, 2005; Gornick et al, 2007; Lasky-Su et al, 2007; Shaw et al, 2007) and the dopamine transporter (Faraone et al, 2005; Thapar et al, 2006; Masellis et al, 2006; Cook et al, 1995). The precise neurochemical pathophysiology of ADHD remains unknown. Neurobiological and pharmacological evidence points to dysregulation of the central catecholaminergic network as the underlying neurochemical pathophysiology of ADHD. Clinical studies have shown that drugs with noradrenergic and/or dopaminergic pharmacology are efficacious in ADHD. Brain regions rich in catecholamines are also consistently implicated in the pathophysiology of ADHD (Biederman and Spencer, 1999).
Atomoxetine is a highly selective noradrenergic reuptake inhibitor that has shown clinical efficacy in treating children with ADHD (Biederman and Spencer, 1999; Kelsey et al, 2004; Michelson et al, 2001, 2002, 2003). However, a significant proportion of ADHD patients remain symptomatic and refractory to treatment. Understanding the role of genetics in poor vs good response to treatment is critical to better patient care. Owing to the likely involvement of NE in the pathophysiology of ADHD and the mechanism of action of atomoxetine on norepinephrine transporter (NET), a comprehensive assessment of the norepinephrine transporter NET/SLC6A2 gene is important. The NET/SLC6A2 gene, localized on 16q12.2, is composed of 14 exons spanning 48 kb, and encodes a protein of 617 amino acids. Among the numerous single nucleotide polymorphisms (SNPs) within the SLC6A2 gene that have been studied for association with ADHD, no single SNP has been conclusively linked as a vulnerability marker and few have been tested for an association with response to treatment (Barr et al, 2002; McEvoy et al, 2002; De Luca et al, 2004; Brookes et al, 2006; Kim et al, 2008).
As ADHD has varied clinical presentation in addition to a lack of a clear molecular basis, another way to ascertain more homogeneous subgroups of disease pathology is to investigate response to treatment as a differentiating factor (Gorwood and Foot, 2006). Perhaps more importantly, analyzing genes related to the mechanism of action of the treatment may help clinicians identify which type of treatment would be most likely to be efficacious in certain patients. In this respect, we assessed the role of the NET/SLC6A2 gene coding for the norepinephrine transporter by genotyping 108 SNPs in children treated with the highly selective NET blocker, atomoxetine. We show an association of NET/SLC6A2 with responsiveness to atomoxetine treatment in two independent cohorts, comprised of a total of 265 ADHD patients, obtained from randomized clinical trials of atomoxetine.
MATERIALS AND METHODS
Populations
Two independent studies were performed according to ethical principles based on the Declaration of Helsinki and were approved by ethics committees for each participating site. Informed consent was obtained for participation in the main trial and a separate consent for participation in the voluntary genetic addendum according to local ethics requirements. Where customary, assent from the patient was obtained. Alternatively, informed consent from both parents or legal guardians was obtained. The first cohort (designated LYAF, n=160) comprised of patients participating in a large, previously described randomized, double-blind multinational clinical trial (Michelson et al, 2004). (Relapse Prevention After 10-Week and 52-Week Treatment with Tomoxetine Hydrochloride in Children With ADHD) which assessed responsiveness to atomoxetine vs placebo. Inclusion criteria were: individuals between the ages of 6 and 15 years at the time of study enrollment, without significant abnormalities in screening laboratory results, of normal intelligence, able to communicate with the investigator, meeting DSM-IV criteria for ADHD, and scoring at least 1.5 SD above the age norm for their diagnostic subtype using published norms for the ADHD Rating Scale IV-Parent Version: Investigator-Administered and -Scored (ADHDRS) (DuPaul et al, 1998). Only those patients on atomoxetine were included in this genetic analysis. A second unique cohort (designated LYBI, n=105) consisted of patients participating in a clinical trial in the United States of America (A Randomized, Double-Blind Comparison of Atomoxetine Hydrochloride, Extended-Release Methylphenidate Hydrochloride [Concerta], and Placebo in Pediatric Outpatients with DSM-IV ADHD), which has been described elsewhere (Newcorn et al, 2008). Inclusion criteria were similar to that of the multinational trial with the exceptions of a slight difference in the age range at the time of enrollment (increased to 16 years) and the required ability to swallow capsules. Only those patients on atomoxetine were included in these genetic analyses.
The demographic data and clinical features of each cohort at baseline tested here (Table 1) were not different from the original clinical trial populations published earlier (Michelson et al, 2004; Newcorn et al, 2008).
Design of Pharmacological Studies
Both cohorts underwent a washout period to eliminate confounds of previous therapy. The washout for the LYAF cohort was 10–20 days between treatment randomizations to accommodate the changes in treatment arms. The LYBI cohort washout was up to 33 days before treatment randomization. For the LYAF cohort, treatment of ADHD patients was initiated at a dose of 0.5 mg/kg/day and could be titrated to a maximum dose of 1.8 mg/kg per day of atomoxetine for the duration of up to 10 weeks of acute, open-label treatment, followed by approximately a year. The ADHD patients in the LYBI cohort received an acute, randomized, double-blind treatment of 0.8–1.8 mg/kg per day of atomoxetine for 6 weeks followed by an 8-month double-blind continuation phase.
Treatment Response Definition
Clinical trial efficacy measures included both the ADHDRS and the Clinical Global Impression-Severity (CGI-S) score (DuPaul et al, 1998). The ADHDRS is an 18-item scale with 1 item for each of the 18 symptoms contained in the DSM-IV diagnosis of ADHD. Each item is scored from 0 (none, never) to 3 (severe or very often). The CGI-S score is a single-item clinician rating of the severity of ADHD symptoms in relation to the clinician's total experience with ADHD patients. Severity, rated on a 7-point scale from 1 (normal, not at all ill) to 7 (among the most extremely ill patients), was obtained at baseline once a week, and at 10 and 6 weeks treatment for LYAF and LYBI, respectively. Week 6 was chosen as the end point for these analyses to represent the latest common assessment of efficacy of atomoxetine between these two clinical trials. A positive treatment response was defined a priori as having both an ADHDRS decrease of at least 25% from baseline (Gao et al, 2006) and a CGI-S score of less than or equal to 2 at week 6. To include all available informative patients in the analyses, the window method was implemented for week 6. If a patient did not have an ADHDRS score at week 6, then the averages of ADHDRS scores at weeks 5 and 7, or the score at week 5 or week 7 was used depending on availability of data. The same window methodology was applied if patients were missing a CGI-S score at week 6.
Genotyping
At the time the study was conducted, there were 275 known NET1 SNPs. Individual SNPs were selected to provide adequate coverage of the gene, surrounding promoter and 3′ untranslated region. From this process, 150 SNPs were chosen for placement on the Sequenom MassArray analysis system (Leushner and Chiu, 2000). From those 150 SNPs, 118 were successfully converted for analysis.
Human genomic DNA was extracted from peripheral blood leukocyte nuclei and the 118 SNPs encompassing SLC6A2 gene were successfully genotyped. Of the 118 SNPs successfully genotyped, 10 were monomorphic and therefore, removed from analyses.
In addition, genotyping of CYP2D6 gene was carried out by using standard PCR–RFLP analysis on gel assays by a CLIA-certified laboratory (Cogenics Inc., Morrisville, NC). CYP2D6 gene codes for the cytochrome P450 enzyme, which metabolizes atomoxetine. Patients, homozygous or heterozygous for alleles *3, *4, *5, *6, *7, *8, were considered as poor metabolizers (Michelson et al, 2007).
Statistical Analysis
Categorical data analyses were completed using a χ2 test. Differences in continuous variables: mean age, age of onset of first symptoms and differences in overall clinical response scores between studies were analyzed using the F-test. CYP2D6 analyses were initially completed by including metabolizer status as a covariate in the χ2 analyses; however, in subsequent analyses, this was omitted because of general non-significance in the initial analyses. These analyses were completed with SAS software (Version 9.1.3, Copyright 2002–2003 SAS Institute Inc., SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA).
Genotyping quality evaluation and association analyses for response to atomoxetine were carried out using Haploview 3.32 (Barrett et al, 2005). As rare variants can be important to complex diseases and treatment response, all SNPs were included in the association analysis with only the following two quality exceptions. Each SNP was tested for Hardy–Weinberg equilibrium and those with a HWE p-value below 10−4 were excluded from analysis. In addition those SNPs, which performed below a 90% call rate were excluded from analysis. These two QC parameters resulted in an additional four SNPs removed from analysis. Haplotypes were defined using the Gabriel et al (2002) method of SNP pairwise linkage disequilibrium, which defines a linkage disequilibrium (LD) block as a contiguous set of SNPs in which 95% of pairwise SNP D′ confident values (CI 95) are considered to be in strong LD. Therefore, to properly consider the differing LD, haplotypes were defined separately in each cohort with equivalent loci, and then examined. The odds ratio for each test was calculated as a measure of effect size, with larger odds ratios corresponding to a higher chance of an individual responding.
RESULTS
Demographic Data and Clinical Features in the Cohorts
Demographic data and clinical features are listed for the LYAF cohort alone, the LYBI cohort alone, all patients from LYAF and LYBI combined (TOTAL cohort), and Caucasians only from both, LYAF and LYBI (CAUCASIAN cohort) (Table 1). CAUCASIAN and TOTAL cohorts are also presented due to a significant difference (p<0.01) in the percentage of Caucasian origin in treated ADHD patients between LYAF (96%) and LYBI (54) cohorts (Table 1). Following a 6-week treatment with atomoxetine, ADHDRS and CGI-S scores in the two cohorts were similar. Decrease in clinical symptomatology from baseline to end point for the LYAF and LYBI cohorts were as follows: ADHDRS from 41 at baseline to 20 at end point and from 41 to 25, respectively, and CGI-S score from 5.2 to 2.9 and 5.0 to 3.7, respectively, demonstrating similarity in effectiveness in symptom reduction in both cohorts.
No Effect of Cyp2d6 Metabolizer Status in the Treatment Response
Atomoxetine is metabolized through the cytochrome P450 enzyme encoded by the CYP2D6 gene. As exposure to atomoxetine is affected by a patient's CYP2D6 status, we genotyped the CYP2D6 gene in both cohorts. Based on well-established criteria for metabolizer status, extensive or poor designations were assigned. No significant difference in the treatment effect, as measured by ADHDRS end point values (p>0.05), was observed between extensive and poor metabolizers, in any cohort, LYAF, LYBI, TOTAL, or CAUCASIAN (Supplementary Table 1).
Net/Slc6a2 Pharmacogenetic Dependence of Treatment Response to Atomoxetine
Using the combined ADHDRS and CGI-S scores response criteria, 79 patients were responders, 163 patients were non-responders, and 23 patients were not included in the analyses due to a missing response value. Twenty of the 108 successfully genotyped SNPs had a nominal significance for association with responder status in at least one of the two cohorts (Table 2 and Supplementary Table 2). The strongest pharmacogenetic association with responder status was found for rs12708954 (p<0.01, OR=3.1, 95% confidence interval (CI 95)=1.4−6.9) in LYBI. The A allele of rs12708954 was associated with being a good responder. The A allele of rs12708954 was also more frequently represented in responders in the LYAF sample, but did not reach significance (Table 2). Furthermore, two adjacent SNPs (rs5568 and rs1566652) to rs12708954 were significantly associated with responder status (p<0.01 and p=0.01, respectively) in the LYAF cohort (Table 2). Seven additional SNPs located within the same LD block as rs12708954 (from rs36016 to rs47958) were significantly associated with responder status in the same sample (Table 2). In the TOTAL cohort, nominal significance with response was observed for 14 SNPs. The strongest association detected was with SNP rs3785152 (p<0.01, OR=2.2, CI 95=1.2–4.0). This SNP, rs3785152, was also the most significantly associated SNP with the treatment response in the CAUCASIAN cohort (p<0.01, OR=2.7, CI 95=1.3–5.4).
Net/Slc6a2 Haplotype Analyses
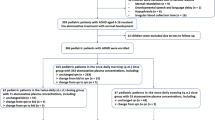
When all available patients were combined (TOTAL cohort), the pairwise linkage disequilibrium identified eight LD blocks across the NET/SLC6A2 gene (Figure 1). Independent analyses of LYAF, LYBI, and CAUCASIAN cohorts showed a similar organization of LD blocks (Figure 1).
Genomic organization of NET/SLC6A2 gene at scale displaying Haploview LD blocks. The colored bars indicate the linkage disequilibrium analysis of the 108 SNPs by cohort (LYAF, LYBI, TOTAL, and CAUCASIAN). For each cohort, significant p-values of associations between atomoxetine response and haplotype allele sequences are indicated under the colored LD bars. Similar haplotype allele sequences across exons 4 to 9 in all cohorts are boxed. The most significantly associated SNP within a cohort, rs12708954, is also boxed.
Over-representations of haplotype allele sequences were observed in the group of patients defined as responders (Table 3). More precisely in the LYAF cohort, LD blocks 2 (SNPs 5–15, p=0.02, OR=2.2, CI 95=1.1–4.6), 3 (SNPs 18–42, p=0.01, OR=2.3, CI 95=1.2–4.7) and 5 (SNPs 54–89, p<0.01, OR=2.2, CI 95=1.3–3.7) had haplotype allele sequences associated with responder status (Table 3, Figure 1). These haplotype allele sequence associations were replicated in the LYBI cohort with specific corresponding LD blocks 1 (SNPs 3–15, p=0.03, OR=6.3, CI 95=1.0–39) and 4 (SNPs 54–82, p=0.03, OR=6.27, CI 95=1.01–39.07), and a trend was observed with 2 (SNPs 18–42, p=0.051). Focusing on the CAUCASIAN cohort, we found an over-representation of haplotype allele sequences in ADHD atomoxetine responders vs non-responders for the same LD blocks 5 (SNPs 56–90, p=0.02, OR=1.8, CI 95=1.1–2.9) and 2 (SNPs 18–42, p=0.04, OR=1.9, CI 95=1.0–3.4).
However, the only region significantly (p<0.03) and systematically associated with treatment response for the LYAF, LYBI, TOTAL, and CAUCASIAN cohorts, was the region that is called LD block 6 in TOTAL cohort, from SNP 54–89. This region has parallel LD blocks in LYAF, LYBI, and CAUCASIAN cohorts, and covers exons 4–9 of NET/SLC6A2 gene and includes SNP rs12708954 (Figure 1). Furthermore, the most significant haplotype allele sequence association was in the LYAF cohort (OR=2.2, p<0.01, CI 95=1.3–3.7) (Table 3). The effect size for the associated allele sequence suggests that a carrier of this sequence would have 2.2 times the chance of responding compared with an individual without the associated sequence.
DISCUSSION
Using two independent samples of patients treated with atomoxetine for ADHD, we were able to test and confirm the role of the NET/SLC6A2 gene in the prediction of response rate. We detected an LD block, covering exons 4–9, that had a haplotype allele sequence associated with nearly twice the chance of being a responder in the TOTAL cohort (OR=1.83). The associations of NET/SLC6A2 variants with response were independent of the metabolism status of CYP2D6, the enzyme that metabolizes atomoxetine. The lack of effect of CYP2D6 metabolism status seen in this study may be due to small sample size as this has been previously shown in a larger population including some patients from this genetic cohort (Michelson et al, 2007).
Although the current report represents the largest study investigating treatment response to atomoxetine reported to date and the clinical response criteria was collected under the rigorous conditions of a clinical trial, a remaining question is whether the two samples give convergent enough results to constitute a clear replication. Although none of the tests, no individual SNP, reached statistical significance at the multiple comparison threshold, this study shows evidence from two independent populations, which lends support to the association results being true as opposed to a false positive. If considering an approach based purely on each individual SNP being an independent marker that should replicate, one possible explanation is that the first results are chance findings, despite the low p-value (p<0.005) observed, and that the second negative results support an absence of association. However, it is not surprising that no individual variant was significantly associated in the two samples as the multiple genetic variants tested are assumed to be in linkage disequilibrium with the true causative variant. In examination of the data in this study, several factors support the notion of confirmation. First, all significantly associated SNPs in the replication cohort, LYBI, are located in the same LD block, close to rs12708954. Second, no SNP in any other region of the gene is significantly associated in the LYBI cohort. Third, the same allele in rs12708954 is over-represented in both samples, although in LYAF not significantly above what could be observed by chance only. Fourth, 9 of the 15 SNPs in the LYAF sample that were associated with treatment response were located in the same LD block as rs12708954. Lastly, when taking into account the variable structure of the gene in the two samples (ie, different definitions of the LD blocks), a replication may be observed within haplotype allele sequences of the same LD block. It is possible, in accordance with the heterogeneity of the two samples (LYAF and LYBI) especially regarding ethnic background, that this absence of replication regarding specific SNPs is explained by different linkage disequilibrium across the samples, that is, due to the different structure of the NET/SLC6A2 gene in the two cohorts.
Also, the genetic and phenotypic heterogeneity of ADHD disease and response to treatment is generally considered as very likely. Different etiological influences are believed to attribute to different symptomatology (Gabriel et al, 2002). DSM-IV subtypes seem to be more frequently identical in a sample of twins (Willcutt et al, 2000) and latent classes were more frequently shared by identical twins (Levy et al, 1997). Although these results were not systematically replicated (Hudziak et al, 1998), another study showed that the hyperactive–impulsive type of the disorder was found almost exclusively among relatives of hyperactive–impulsive probands (Smalley et al, 2000). The possibility that a certain gene may be a vulnerability factor in specific subtypes of ADHD therefore influencing overall genetic susceptibility and pharmacogenetic results cannot be ruled out. When taken in total, these results support the association of this region with response to atomoxetine.
In addition to the clinical phenotyping and sample size, another strength of the current report is the comprehensiveness of the genotyping. Given the complex nature of the LD observed, thorough genotyping is critical to understanding the effect of this gene on drug response or disease susceptibility. Another piece of evidence supporting this finding is the potential convergence of the SLC6A2 SNPs conferring involvement both, in ADHD disease susceptibility and in treatment response to atomoxetine. Approximately 300 SNPs, including 27 coding SNPs, have been identified within the SLC6A2 gene. The most frequently studied polymorphisms are the rs5568 (SNP 83 in this study) and rs998424 (SNP 91), which are in strong linkage disequilibrium. When examined in adults and children with ADHD, no association has been found for either SNP by case–control studies or by transmission disequilibrium test (Barr et al, 2002; McEvoy et al, 2002; De Luca et al, 2004). However, more recent analyses of additional SNPs reported an association with disease susceptibility for rs36009 (SNP 90) in a case–control study (Faraone et al, 2000) and, rs3785143 (SNP 15) in two large cohorts of ADHD families (Brookes et al, 2006; Kim et al, 2008).
Influence of variation in genes involved in the metabolism, transport, or mechanism of action of a drug on variability in treatment response and tolerability has been demonstrated for antidepressants and antipsychotics (Guan et al, 2008; Kirchheiner et al, 2004). Current pharmacogenetic studies of ADHD investigating response or tolerability to medication have mainly focused on methylphenidate response and dopaminergic genes (Tomalik-Scharte et al, 2008; Kereszturi et al, 2008; Polanczyk et al, 2005, 2007). Polymorphisms in NET/SLC6A2 gene can have a specific effect as proposed on methylphenidate response (Yang et al, 2004; Kooij et al, 2008; Mick et al, 2008).To date, our pharmacogenetic evidence that NET/SLC6A2 polymorphisms modulate the effectiveness of atomoxetine treatment is the first report. Given the increased usage of noradrenergic medications in the treatment of ADHD symptomatology, including non-responders to methylphenidate (Newcorn et al, 2008), further investigation of genes involved in norepinephrine neurotransmission or metabolism of noradrenergic drugs is critical to our understanding of treatment response.
References
Barr CL, Kroft J, Feng Y, Wigg K, Roberts W, Malone M et al (2002). The norepinephrine transporter gene and attention-deficit hyperactivity disorder. Am J Med Genet 114: 255–259.
Barrett JC, Fry B, Maller J, Daly MJ (2005). Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21: 263–265.
Biederman J, Spencer T (1999). Attention-deficit/hyperactivity disorder (ADHD) as a noradrenergic disorder. Biol Psychiatry 46: 1234–1242 .2.
Brookes K, Xu X, Chen W, Zhou K, Neale B, Lowe N et al (2006). The analysis of 51 genes in DSM-IV combined type attention deficit hyperactivity disorder: association signals in DRD4, DAT1 and 16 other genes. Mol Psychiatry 11: 934–953.
Cook Jr EH, Stein MA, Krasowski MD, Cox NJ, Olkon DM, Kieffer JE et al (1995). Association of attention-deficit disorder and the dopamine transporter gene. Am J Hum Genet 56: 993–998.
De Luca V, Muglia P, Jain U, Kennedy JL (2004). No evidence of linkage or association between the norepinephrine transporter (NET) gene Mnll polymorphism and adult ADHD. Am J Med Genet B Neuropsychiatr Genet 124B: 38–40.
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R (1998). ADHD Rating Scale-IV: Checklists, Norms, and Clinical Interpretation. The Guilford Press: New York.
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA et al (2005). Molecular genetics of attention-deficit hyperactivity disorder. Biol Psychiatry 57: 1313–1323.
Faraone S, Biederman J, Friedman D (2000). Validity of DSM-IV subtypes of attention-deficit hyperactivity disorder: a family study perspective. J Am Acad Child Adolesc Psychiatry 39: 300–307.
Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B et al (2002). The Structure of Haplotype Blocks in the Human Genome. Science 296: 2225–2229.
Gao H, Zhao Y, Levine L, Allen A 2006. Determining cut-points for clinically meaningful improvement: an ROC approach. Presented at: The 53rd Annual Meeting of The American Academy of Child and Adolescent Psychiatry; October 24–29 San Diego, CA. American Academy of Child and Adolescent Psychiatry: Washington, DC, p 201.
Gornick MC, Addington A, Shaw P, Bobb AJ, Sharp W, Greenstein D et al (2007). Association of the dopamine receptor D4 (DRD4) gene 7-repeat allele with children with attention-deficit/hyperactivity disorder (ADHD): an update. Am J Med Genet B Neuropsychiatr Genet 144B: 379–382.
Gorwood P, Foot E (2006). Introduction on psychopharmacogenetics. In:Gorwood G and Hamon M eds Psychopharmacogenetics 1st ed Springer Science: New York, USA. : pp 1–24.
Guan L, Wang B, Chen Y, Yang L, Li J, Qian Q et al (2008). A high-density single-nucleotide polymorphism screen of 23 candidate genes in attention deficit hyperactivity disorder: suggesting multiple susceptibility genes among Chinese Han population. Mol Psychiatry e-pub ahead of print 8 January 2008 8.
Hudziak JJ, Heath AC, Madden PF, Reich W, Bucholz KK, Slutske W et al (1998). Latent class and factor analysis of DSM-IV ADHD: a twin study of female adolescents. J Am Acad Child Adolesc Psychiatry 37: 848–857.
Kelsey DK, Sumner CR, Casat CD, Coury DL, Quintana H, Saylor KE et al (2004). Once-daily atomoxetine treatment for children with attention-deficit hyperactivity disorder, including an assessment of evening and morning behavior: a double-blind, placebo-controlled trial. Pediatrics 114: e1–e8.
Kereszturi E, Tarnok Z, Bognar E, Lakatos K, Farkas L, Gadoros J et al (2008). Catechol-O-methyltransferase Val158Met polymorphism is associated with methylphenidate response in ADHD children. Am J Med Genet B Neuropsychiatr Genet 147B: 1431–1435.
Kim JW, Biederman J, McGrath CL, Doyle AE, Mick E, Fagerness J et al (2008). Further evidence of association between two NET single-nucleotide polymorphisms with ADHD. Mol Psychiatry 13: 624–630.
Kirchheiner J, Nickchen K, Bauer M, Wong ML, Licinio J, Roots I et al (2004). Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol Psychiatry 9: 442–473.
Kooij JS, Boonstra AM, Vermeulen SH, Heister AG, Burger H, Buitelaar JK et al (2008). Response to methylphenidate in adults with ADHD is associated with a polymorphism in SLC6A3 (DAT1). Am J Med Genet B Neuropsychiatr Genet 147B: 201–208.
Lasky-Su J, Banaschewski T, Buitelaar J, Franke B, Brookes K, Sonuga-Barke E et al (2007). Partial replication of a DRD4 association in ADHD individuals using a statistically derived quantitative trait for ADHD in a family-based association test. Biol Psychiatry 62: 985–990.
Leushner J, Chiu NH (2000). Automated mass spectrometry: a revolutionary technology for clinical diagnostics. Mol Diagn 5: 341–348.
Levy F, Hay DA, McStephen M, Wood C, Waldman I (1997). Attention-deficit hyperactivity disorder: a category or a continuum? Genetic analysis of a large-scale twin study. J Am Acad Child Adolesc Psychiatry 36: 737–744.
Masellis M, Basile VS, Kennedy JL (2006). Neuropsychopharmacogenetics: ‘Stimulating’ rationale therapy in attention-deficit hyperactivity disorder (ADHD): Pharmacogenetics of psychostimulants in ADHD. In:Gorwood P and Hamon M (eds) Psychopharmacogenetics 1st ed Springer Science: New York, USA. pp 231–248.
McEvoy B, Hawi Z, Fitzgerald M, Gill M (2002). No evidence of linkage or association between the norepinephrine transporter (NET) gene polymorphisms and ADHD in the Irish population. Am J Med Genet 114: 665–666.
Michelson D, Allen AJ, Busner J, Casat C, Dunn D, Kratochvil C et al (2002). Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry 159: 1896–1901.
Michelson D, Adler L, Spencer T, Reimherr FW, West SA, Allen AJ et al (2003). Atomoxetine in adults with ADHD: two randomized, placebo-controlled studies. Biol Psychiatry 53: 112–120.
Michelson D, Buitelaar JK, Danckaerts M, Gillberg C, Spencer TJ, Zuddas A et al (2004). Relapse prevention in pediatric patients with ADHD treated with atomoxetine: a randomized, double-blind, placebo-controlled study. J Am Acad Child Adolesc Psychiatry 43: 896–904.
Michelson D, Faries D, Wernicke J, Kelsey D, Kendrick K, Sallee FR et al (2001). Atomoxetine ADHD Study Group. Atomoxetine in the treatment of children and adolescents with attention-deficit hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics 108: E83.
Michelson D, Read HA, Ruff DD, Witcher J, Zhang S, McCracken J (2007). CYP2D6 and clinical response to atomoxetine in children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry 46: 242–251.
Mick E, Neale B, Middleton FA, McGough JJ, Faraone SV (2008). Genome-wide association study of response to methylphenidate in 187 children with attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 147B: 1412–1418.
Newcorn JH, Kratochvil CJ, Allen AJ, Casat CD, Ruff DD, Moore RJ et al (2008). Atomoxetine/Methylphenidate Comparative Study Group. Atomoxetine and osmotically Released Methylphenidate for the Treatment of Attention Deficit Hyperactivity Disorder: acute Comparison and Differential Response. Am J Psychiatry 165: 721–730.
Polanczyk G, Zeni C, Genro JP, Guimarães AP, Roman T, Hutz MH et al (2007). Association of the adrenergic alpha2A receptor gene with methylphenidate improvement of inattentive symptoms in children and adolescents with attention-deficit hyperactivity disorder. Arch Gen Psychiatry 64: 218–224.
Polanczyk G, Zeni C, Genro JP, Roman T, Hutz MH, Rohde LA (2005). Attention-deficit hyperactivity disorder: advancing on pharmacogenomics. Pharmacogenomics 6: 225–234.
Shaw P, Gornick M, Lerch J, Addington A, Seal J, Greenstein D et al (2007). Polymorphisms of the dopamine D4 receptor clinical outcome, and cortical structure in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 64: 921–931.
Smalley SL, McGough JJ, Del’Homme M, NewDelman J, Gordon E, Kim T et al (2000). Familial clustering of symptoms and disruptive behaviors in multiplex families with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 39: 1135–1143.
Thapar A, Langley K, O’Donovan M, Owen M (2006). Refining the attention deficit hyperactivity disorder phenotype for molecular genetic studies. Mol Psychiatry 11: 714–720.
Tomalik-Scharte D, Lazar A, Fuhr U, Kirchheiner J (2008). The clinical role of genetic polymorphisms in drug-metabolizing enzymes. Pharmacogenomics J 8: 4–15.
Willcutt EG, Pennington BF, DeFries JC (2000). Etiology of inattention and hyperactivity/impulsivity in a community sample of twins with learning difficulties. J Abnorm Child Psychol 28: 149–159.
Yang L, Wang YF, Li J, Faraone SV (2004). Association of norepinephrine transporter gene with methylphenidate response. J Am Acad Child Adolesc Psychiatry 43: 1154–1158.
Acknowledgements
We acknowledge Ms. Shuyu Zhang of Eli Lilly and Company for sharing her statistical expertise.
Author information
Authors and Affiliations
Corresponding author
Additional information
CONFLICT OF INTEREST
Both clinical trials, LYAF and LYBI, and pharmacogenetic analysis were funded by Eli Lilly and Company, Indianapolis, IN, USA. AMD, SLC, and AJA are employees of Eli Lilly and Company. AMP is a current and SLP is a former employee of BioStat Solutions that Eli Lilly and Company paid for services and other than receiving compensation from their employer, have no other conflicts of interest to report. PG received grants from Eli Lilly; honoraria from Lundbeck, Servier, UCB-Pharma and participated in advisory boards for Janssen, Servier, and Wyeth. He has a paid position from University of Paris VII. NR, CB, MH, and DPO declare no conflicts of interest.
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Supplementary information
Rights and permissions
About this article
Cite this article
Ramoz, N., Boni, C., Downing, A. et al. A Haplotype of the Norepinephrine Transporter (Net) Gene Slc6a2 is Associated with Clinical Response to Atomoxetine in Attention-Deficit Hyperactivity Disorder (ADHD). Neuropsychopharmacol 34, 2135–2142 (2009). https://doi.org/10.1038/npp.2009.39
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2009.39
Keywords
This article is cited by
-
Personalizing atomoxetine dosing in children with ADHD: what can we learn from current supporting evidence
European Journal of Clinical Pharmacology (2023)
-
Atomoxetine Decreases Mitochondrial Biogenesis, Fission and Fusion In Human Neuron-like Cells But Does Not Alter Antioxidant Defences
Cell Biochemistry and Biophysics (2023)
-
Genetic Influence on Efficacy of Pharmacotherapy for Pediatric Attention-Deficit/Hyperactivity Disorder: Overview and Current Status of Research
CNS Drugs (2020)
-
The Efficacy of Atomoxetine for the Treatment of Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Comprehensive Review of Over a Decade of Clinical Research
CNS Drugs (2015)
-
No association of the norepinephrine transporter gene (SLC6A2) and cognitive and behavioural phenotypes of patients with autism spectrum disorder
European Archives of Psychiatry and Clinical Neuroscience (2014)