Abstract
Background:
In acute cough patients, impaired lung function as present in chronic lung conditions like asthma and chronic obstructive pulmonary disease (COPD) are often thought to negatively influence course of disease, but clear evidence is lacking.
Aims:
To investigate the influence of lung function abnormalities on course of disease and response to antibiotic therapy in primary care patients with acute cough.
Methods:
A total of 3,104 patients with acute cough (⩽28 days) were included in a prospective observational study with a within-nested trial, of which 2,427 underwent spirometry 28–35 days after inclusion. Influence of the lung function abnormalities fixed obstruction (forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) ratio <0.7) and bronchodilator responsiveness (FEV1 increase of ⩾12% or 200 ml after 400 μg salbutamol) on symptom severity, duration and worsening were evaluated using uni- and multivariable regression models. Antibiotic use was defined as the reported use of antibiotics ⩾5 days in the first week. Interaction terms were calculated to investigate modifying effects of lung function on antibiotic effect.
Results:
The only significant association was the effect of severe airway obstruction on symptom severity on days 2–4 (difference=0.31, 95% confidence interval (CI)=0.03–0.60, P=0.03). No evidence of a differential effect of lung function on the effect of antibiotics was found. Prior use of inhaled steroids was associated with a 30% slower resolution of symptoms rated ‘moderately bad’ or worse (hazard ratio=0.75, 95% CI=0.63–0.90, P=0.00).
Conclusions:
In adult patients with acute cough, lung function abnormalities were neither significantly associated with course of disease nor did they modify the effect of antibiotics.
Similar content being viewed by others
Introduction
Acute cough is one of the most common reasons for people to consult their general practitioner (GP).1–3 The majority of these acute cough episodes are caused by mild and self-limiting lower respiratory tract infections (RTIs) and do not require antibiotic therapy. However, it is possible that patients with underlying lung diseases such as asthma or chronic obstructive pulmonary disease (COPD) suffer from unusually prolonged or severe illness which would benefit from targeted and adapted therapy.
Approximately 20% of the visits to the GP for lower respiratory tract symptoms are in patients with abnormal lung function as seen in asthma or COPD.4 These episodes, referred to as exacerbations of the underlying chronic lung disorder, contribute to poor quality of life, mortality and progression of lung disease.5–7 Whether these episodes, often with acute cough as one of the main symptoms, show a more severe and of prolonged duration compared with cough episodes in otherwise healthy patients is, however, unknown. More importantly, antibiotic treatment for these exacerbations of chronic lung disorders in primary care is still controversial.8–10
A better understanding of the influence of impaired lung function on course of disease and response to antibiotics could lead to improved patient education and targeted antibiotic prescribing. The aim of the present study was therefore to further evaluate influence of lung function on course of disease and response to antibiotic therapy in patients with acute cough in primary care.
Materials and Methods
Study design and patients
Data from the GRACE-09 and GRACE-10 studies (Genomics to combat Resistance against Antibiotics in Community-acquired lower RTIs in Europe; www.grace-lrti.org) were used. In this prospective observational study (GRACE-09) with a within nested randomised placebo-controlled double-blind trial (GRACE-10), data were collected in 16 primary care research networks in 12 European countries. Participating GPs recruited consecutive patients from October 2007 until April 2010.
Eligible patients were at least 18 years old, consulting their GP with a new episode of acute or worsened cough (duration ⩽28 days) as the main symptom. Previous diagnoses of asthma, COPD and other comorbid disorders were not exclusion criteria, and thus acute infective exacerbations were included. Criteria for exclusion and further details about GRACE-09 and GRACE-10 are described in detail elsewhere.11,12 The study was approved by ethics committees in all participating countries and all subjects provided written informed consent.
Measurements
Symptoms
At baseline clinicians recorded signs and symptoms as well as comorbidities and use of medication. After this first visit, patients received a diary on symptoms and daily activities to complete during their illness (to a maximum of 28 days). Each symptom was rated on a scale from 0 to 6 (0=no problem, 1=very little problem, 2=slight problem, 3=moderately bad, 4=bad, 5=very bad, 6=as bad as it could be). This diary was previously validated and had been proven sensitive to change and internally reliable.13 If the diary was not returned after 4 weeks, brief information about symptom duration and severity with either a short questionnaire or a standardised telephone call.
Spirometry
Between 28 and 35 days after inclusion spirometry was performed according to a strict protocol. The aim of this timing was to obtain results during a stable phase.14,15 Staff in the participating centers underwent standardised training in spirometry. Measurements included the forced vital capacity (FVC), the forced expiratory volume in 1 s (FEV1) and the peak expiratory flow before and at least 15 min after bronchodilation with 400 μg of salbutamol. The best of a minimum of three acceptable retained flow volume curves was used to determine the post-bronchodilator FEV1/FVC ratio.14
Definition of lung function abnormalities
‘Fixed airway obstruction’ was defined as a post-bronchodilator FEV1/FVC ratio <0.7, according to the Global Initiative for Chronic Obstructive Lung Disease criteria.14 Three obstruction severity groups based on FEV1 percentage of predicted were defined: mild obstruction (FEV1⩾80% predicted), moderate obstruction (50⩽FEV1<80% predicted) and severe obstruction (FEV1<50% predicted). ‘Bronchodilator responsiveness’ was diagnosed if FEV1 increase of ⩾12% or more than 200 ml occurred after bronchodilation. In addition, we selected those patients with bronchodilator responsiveness who also reported recurrent (more than one episode) wheezing, cough or chest tightness in the past year. These patients are referred to as patients with ‘symptomatic bronchoconstriction’. Patients with both fixed airway obstruction and bronchodilator responsiveness were classified as having fixed obstruction and were not included in the analyses concerning bronchodilator responsiveness. This was decided as it is recognised that patients with COPD frequently but inconsistently exhibit modest bronchodilator responsiveness and that this does not influence response to inhaled therapy.16
Antibiotic use
Antibiotic use was defined as the reported intake of antibiotics for 5 days or more in the first week after consultation, as this is the duration of use by which bacteria should have been eradicated, and the use of antibiotics after the first week would be unlikely to influence the main outcomes under investigation. For those in the nested trial, antibiotic therapy consisted of 1 g amoxicillin three times daily. Subjects in the observational cohort reported in diaries whether they were prescribed antibiotics, the type and dose, and whether they took their medication on each day.
Outcome measures
Three key outcomes were specified as primary outcomes for the trial to capture important symptomatic outcomes for patients:17 symptom severity on days 2–4 after the index consultation, duration of symptoms rated by patients as ‘moderately bad’ or worse, and the occurrence of new or worsening symptoms, defined as a return to the physician with worsening symptoms, new symptoms or signs, or illness that made hospital admission necessary within 4 weeks after the first consultation. In addition, effects on duration of symptoms until complete resolution were assessed.
Data analysis
Data were analysed using linear regression models. Simple linear regression was used for symptom severity, Cox regression allowing for censoring for the duration of symptoms and logistic regression for the occurrence of new or worsened symptoms. In the multivariable analyses we controlled for the potentially confounding factors age, gender, baseline severity, duration of prior cough, chronic use of inhaled steroids, current smoking, the coexistence of heart disease, antibiotic use and use of inhaled bronchodilators and inhaled corticosteroids (ICSs) during this cough episode. As fixed obstruction and bronchodilator responsiveness of up to 200 ml in FEV1 are frequently seen together, the multivariable analyses concerning ‘fixed obstruction’ controlled for ‘bronchodilator responsiveness’.
The effects of antibiotics were analysed both in the observational study and in the within-nested randomised clinical trial. To investigate the effect of antibiotics in patients with abnormal lung function test results, interaction terms between antibiotic use and fixed obstruction and antibiotic use and bronchodilator responsiveness were calculated and used as an independent factor in the statistical models. To forestall confounding by indication for patients in the observational cohort, propensity scores were calculated and included in the multivariate models to control for. All data analyses were performed using SPSS version 20.0 for Windows (IBM Corporation, Armonk, NJ, USA). The significance level was set at 5%.
Results
Patient characteristics
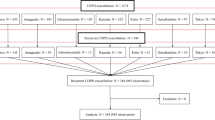
A total of 3,104 eligible patients with acute cough were recruited, of which 2,581 (83%) underwent spirometry. Patients with incomplete spirometry results (n=154) were excluded, resulting in 2,427 subjects for analysis (Figure 1). The mean age of the total study population (n=2,427) was 50.8 (s.d.=16.5) and 59.5% (n=1,454) of the patients were female. Table 1 shows the baseline characteristics of all patients, sorted by lung function abnormality after 4 weeks and by antibiotic use.
Lung function abnormalities
Patients with fixed lung function obstruction of any severity category were older, more often male, more often current smokers and more often chronic inhaled medication users. Of the patients that met the criteria for fixed obstruction (n=323), only 12.4% (mild obstruction) to 37.2% (severe obstruction) were previously diagnosed with COPD, suggesting that significant numbers of patients presenting to GPs with an acute cough may have previously undiagnosed COPD. On the other hand, of the patients with previously diagnosed COPD (n=157), only 79 (50.3%) showed a fixed obstruction during the present spirometry, suggesting overdiagnosis.
Patients with bronchodilator responsiveness were more often male and current smokers, but otherwise did not differ significantly from the patients without this abnormality. Patients with lung function abnormalities, both fixed obstruction and responsiveness, did not present with more severe or longer-existing symptoms at baseline than people without (Table 1).
Antibiotic use
Of all 2,427 patients, 1,626 were included in the randomised controlled trial with 821 patients in the amoxicillin group and 805 patients in the placebo group. All the other patients (n=801) were part of the observational study, of which 394 patients were prescribed antibiotics by their GP. When analysed together and regarding actual use of antibiotics (per protocol analysis), 896 patients (36.9%) used antibiotics for 5 days or more in the first week compared with 1,327 (54.7%) patients who did not. In 204 patients (8.4%) actual antibiotic use was not reported.
Course of disease
Only in the outcome measure mean symptom severity on days 2–4, there was a significant difference between patients with and without severe airway obstruction in the multivariable analysis (difference=0.31, 95% confidence interval (CI)=0.03–0.60, P=0.03). A similar effect was seen for ‘symptomatic bronchoconstriction’ (difference=0.12, 95% CI=0.01–0.23, P=0.03) (Table 2). For all other outcome parameters, no significant effects of any of the lung function abnormality groups were seen after controlling for confounders (Tables 3, 4 and 5).
We found that 231 patients (9.5%) were receiving maintenance treatment with ICSs at the time of presentation. Long-term use of inhaled steroids was associated with a 30% slower resolution of symptoms rated ‘moderately bad’ or worse (12.2 days versus 9.2 days in patients without inhaled steroids, hazard ratio (HR)=0.75, 95% CI=0.63–0.90, P<0.001) and a 15% slower resolution of symptoms until complete resolution (18.3 days versus 15.9 days, HR=0.65, 95% CI=0.52–0.83, P<0.001) in multivariate regression models. Similarly, a prior physician diagnosis of COPD (n=157, 6.5%) was associated with a slower resolution of symptoms rated ‘moderately bad’ or worse (12.4 days in patients with this diagnosis versus 9.3 days in patients without, HR=0.77, 95% CI=0.62–0.95, P=0.02).
Effect of antibiotics
Antibiotic use was included in regression models of all four main outcomes, and was not an independent predictive factor for severity of symptoms on days 2–4, duration of symptoms or occurrence of new or worsened symptoms. In addition, there was no evidence for an interaction between fixed airway obstruction and the use of antibiotics on mean severity of symptoms (B interaction term coefficient=0.05, 95% CI=−0.13 to 0.24, P=0.58), duration of symptoms rated ‘moderately bad’ or worse (HR=0.87, 95% CI=0.71–1.05, P=0.15), duration of symptoms until resolution (HR=0.84, 95% CI=0.66–1.07, P=0.15) or the occurrence of new or worsened symptoms (odds ratio=1.26, (0.81–1.95, P=0.31). No interaction between ‘bronchodilator responsiveness’ and antibiotic use was seen on these four outcomes. The results after controlling for propensity score for the observational study participants confirmed that the interaction term was not significant in any model (see Supplementary Appendix Tables 1–4). Therefore no further subgroup analysis was performed. No different results were found in trial patients only (data not shown).
Discussion
Main findings
In adult patients who consulted for acute cough in primary care and who underwent pre- and post-bronchodilator spirometry 4 weeks later, lung function abnormalities defined as ‘fixed airway obstruction’, ‘bronchodilator responsiveness’ and ‘symptomatic bronchoconstriction’ did not influence course of disease in a clinically meaningful way. Neither fixed airway obstruction nor bronchodilator responsiveness influenced the effect of antibiotics. The use of ICSs was independently associated with prolonged illness, as was a prior diagnosis of COPD.
Interpretation of findings in relation to previously published work
The general presumption, although lacking a firm evidence-base, is that patients with abnormal lung function and with pre-existing airways disease will suffer from more severe symptoms and a longer duration of illness. However, as asthma and COPD patients are usually regarded as separate groups in medical research, we are aware of no studies directly comparing healthy individuals with patients with asthma or COPD.
Hopstaken et al.10 reported physician-diagnosed asthma to be an independent predictor of delayed symptom resolution in RTI. This finding was not confirmed by our study. Neither measured bronchodilator responsiveness, with or without reported complaints of recurrent cough, wheezing or chest tightness, nor a prior diagnosis of asthma, were found to be independent predictors of a prolonged disease in our study. Comparison between our study and Hopstaken’s is, however, hampered by differences in study size, definitions and use of measurements. In our larger study, neither a prior diagnosis of asthma nor recurrent episodes of respiratory symptoms combined with bronchodilator responsiveness were associated with length or severity of illness nor with a response to antibiotics.
While lung function abnormalities as measured by spirometry were no independent predictors of course of disease, both long-term use of ICSs and a prior diagnosis of COPD were independent predictors of duration of symptoms rated ‘moderately bad’ or worse. These two characteristics were probably markers for a more severe underlying disorder or risk for a more serious course of disease. In the case of a diagnosis of COPD, this is somewhat remarkable since spirometry results were normal in half of these patients. A possible explanation could be that the physician diagnosis of ‘COPD’ included a subgroup that did not meet the physiological criteria required for COPD diagnosis but previously had suffered from frequent and prolonged episodes for other, perhaps, immunological reasons. Further research to understand this finding is needed.
In the existing literature ICS use is associated with an increased risk of pneumonia in patients with COPD,18 and new evidence shows similar results for asthma patients.19 However, the effects on RTI severity and duration have not been studied in a large representative group of patients treated in the community such as those in our study. There is biological plausibility in the contention that long-term inhaled steroid use could have effects on RTI, and our data suggest that it might be an independent predictor of a prolonged course of disease, regardless of lung function. This finding also warrants further research.
Regarding antibiotic use in patients with abnormal lung function, our findings are consistent with other studies. A recent Cochrane review shows effects of antibiotics for exacerbations of COPD in patients admitted to an ICU, but in patients with mild and moderate exacerbations, more likely to be seen by the GP, there is limited evidence of the effectiveness of currently available antibiotics.9 In asthma, two studies including 97 participants included in a Cochrane review show insufficient evidence to support the use of antibiotics.20
Strengths and limitations of this study
A major strength of this study is the large sample size. In addition, as this study recruited patients consulting their GP with acute cough in 12 European countries using broad inclusion criteria, these findings are based on a clinically relevant population and therefore are highly generalisable.
Lung function was assessed using the spirometers already available in the participating primary care practices. Because of this, measurements were obtained by a range of different spirometer models. However, spirometry was performed according to a strict protocol at all study sites and participating staff were adequately trained to perform spirometry and analyse curves. It has been shown that spirometry tests in primary care conducted by appropriately skilled and trained staff are comparable in quality to pulmonary function laboratory measurements.21
Lung function was measured 4 weeks after the index consultation to avoid temporary airway obstruction or responsiveness caused by the RTI. However, some of the patients may still have had a prolonged temporary airway hyperreactivity due to their infection.15 It is, however, not likely that this will have biased results significantly in patients without asthma or COPD. In addition, spirometry results of patients with asthma vary over time and may be completely normal at any given moment and in the absence of exposure to triggers.22 Consequently, it is possible that a proportion of the patients with normal spirometry may have had asthma, which could have been detected by more sophisticated tests such as measures of bronchial hyperreactivity or airways inflammation.
Patients with a pre-existing diagnosis of asthma or COPD were included in this analysis. How these diagnostic labels were given was not recorded and thus should be assumed to be varying as is the case in routine daily primary care. When interpreting the relations between previous diagnosis of asthma and COPD, this should be taken into account. The same applies for the treatments at baseline that patients used. These baseline characteristics all reflect daily routine in primary care and were not given according to a study protocol or standardised guidelines.
For this study it was decided to combine data from a nested trial and an observational part of a study cohort. These two groups of patients are not completely comparable as some patients were deliberately withheld from randomisation for several possible reasons, raising the possibility of bias. In addition, the antibiotic used in the trial was amoxicillin 1 g three times daily while in the observational study the type and dose of antibiotics varied. However, this potential limitation was controlled for by adjusting for possible differences in baseline characteristics in our regression models. In addition, we calculated propensity scores for all observational patients to control for confounding by indication. The same results were found with these scores included in the multivariable statistical models. A subanalysis of trial patients only showed similar results.
Conclusion and implications for future research, policy and practice
Overall, this study found little influence of lung function on course of disease in adult patients presenting in primary care with acute cough. In addition, no effect of antibiotics was apparent in patients with fixed airflow obstruction or bronchodilator reversibility. This suggests that undetected lung function abnormalities pose no relevant short-term clinical problems for GPs while diagnosing and treating patients with acute cough. The course of disease in these patients is usually mild, self-limiting and not improved by antibiotics. No extensive diagnostic procedures are warranted immediately, and monitoring of recurrent and prolonged signs and symptoms within a somewhat larger timeframe still seems a good approach.
References
Schappert SM, Burt CW . Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001-02. Vital Health Stat 13 2006; 1–66.
MacFarlane J, Holmes W, Gard P, MacFarlane R, Rose D, Weston V et al. Prospective study of the incidence, aetiology and outcome of adult lower respiratory tract illness in the community. Thorax 2001; 56: 109–114.
Burt CW, Schappert SM . Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1999–2000. Vital Health Stat 13 2004; 1–70.
MacFarlane J, Colville A, Guion A, MacFarlane R, Rose D . Prospective study of aetiology and outcome of adult lower respiratory tract infections in the community. Lancet 1993; 341: 511–514.
Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC . Chronic obstructive pulmonary disease surveillance—United States, 1971-2000. MMWR Surveill Summ 2002; 51: 1–16.
Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA . Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002; 57: 847–852.
Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F et al. for the IMPAC study group. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax 2004; 59: 387–395.
Anthonisen NR, Manfreda J, Warren CPW, Herschfield ES, Harding GMK, Nelson NA . Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987; 106: 196–204.
Vollenweider DJ, Jarret H, Sterurer-Stey CA, Garcia-Aymerich J, Puhan MA . Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 12: CD010257.
Hopstaken RM, Coenen S, Butler CC, Nelemans P, Muris JW, Rinkens PE et al. Prognostic factors and clinical outcome in acute lower respiratory tract infections: a prospective study in general practice. Fam Pract 2006; 23: 512–519.
Vugt van SF, Verheij TJ, Jong de PA, Butler CC, Hood K, Coenen D et al. Diagnosing pneumonia in patients with acute cough: clinical judgment compared to chest radiography. Eur Respir J 2013; 42: 1076–1082.
Little P, Stuart B, Moore M, Coenen S, Butler CC, Godycki-Cwirko M et al. Amoxicillin for acute lower-respiratory-tract infection in primary care when pneumonia is not suspected: a 12-country, randomised, placebo-controlled trial. Lancet Infect Dis 2013; 13: 123–129.
Watson L, Little P, Williamson I, Moore M, Warner G . Validation study of a diary for use in acute lower respiratory tract infection. Fam Pract 2001; 18: 553–554.
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007; 176: 532–555.
Boldy DA, Skidmore SJ, Ayres JG . Acute bronchitis in the community: clinical features, infective factors, changes in pulmonary function and bronchial reactivity to histamine. Respir Med 1990; 84: 377–385.
Albert P, Agusti A, Edwards L, Tal-Singer R, Yates J, Bakke P et al. Bronchodilator responsiveness as a phenotypic characteristic of established chronic obstructive pulmonary disease. Thorax 2012; 67: 701–708.
Little P, Rumsby K, Kelly J, Watson L, Moore M, Warner G et al. Information leaflet and antibiotic prescribing strategies for acute lower respiratory tract infection: a randomized controlled trial. JAMA 2005; 293: 3029–3035.
Crim C, Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C et al. Pneumonia risk in COPD patients receiving inhaled corticosteroids alone or in combination: TORCH study results. Eur Respir J 2009; 34: 641–647.
McKeever T, Harrison TW, Hubbard R, Shaw D . Inhaled corticosteroids and the risk of pneumonia in people with asthma: a case control stud. Chest 2013; 144: 1788–1794.
Graham V, Lasserson TJ, Rowe BH . Antibiotics for acute asthma. Cochrane database Syst Rev 2009; 2: CD002741.
Schermer TR, Jacobs JE, Chavannes NH, Hartman J, Folgering HT, Bottema BJ et al. Validity of spirometric testing in a general practive population of patients with chronic obstructive pulmonary disease (COPD). Thorax 2003; 58: 861–866.
Thiadens HA, de Bock GH, Dekker FW, Huysman JA, van Houwelingen JC, Springer MP et al. Identifying asthma and chronic obstructive pulmonary disease in patients with persisting cough presenting to general practitioners: descriptive study. BMJ 1998; 316: 1286–1290.
Author information
Authors and Affiliations
Consortia
Contributions
NvE reorganised existing data, performed statistical analyses supervised by BS and wrote the main text. BS supervised statistical analyses and performed the propensity score analyses. PL and TJMV (guarantor) came up with the idea for the present study and were main contributors to design, analyses and writing of the paper. MT as an expert in asthma and COPD in primary care had an important contribution to the design, analyses and reporting of the study. PL, TJMV, MM, BS, CCB, KH, SC, HG, Ml, as part of the GRACE consortium, had main roles in the design and data gathering of the GRACE studies, and contributed to the text of the present study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest. MT is an Associate Editor of npjPCRM, but was not involved in the editorial review of, nor the decision to publish, this article.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
van Erp, N., Little, P., Stuart, B. et al. Influence of lung function on course of disease and response to antibiotic therapy in adult primary care patients with acute cough: a post hoc analysis of patients enrolled in a prospective multicentre study. npj Prim Care Resp Med 24, 14067 (2014). https://doi.org/10.1038/npjpcrm.2014.67
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjpcrm.2014.67