Abstract
Li–Fraumeni syndrome (LFS) is a rare cancer predisposition syndrome usually associated with TP53 germline alterations. Its genetic basis in TP53 wild-type pedigrees is less understood. Using whole-genome sequencing, we identified a germline hemizygous deletion ablating CDKN2A–CDKN2B in a TP53 wild-type patient presenting with high-grade sarcoma, laryngeal squamous cell carcinoma and a family history suggestive of LFS. Patient-derived cells demonstrated reduced basal gene and protein expression of the CDKN2A-encoded tumour suppressors p14ARF and p16INK4A with concomitant decrease in p21 and faster cell proliferation, implying potential deregulation of p53-mediated cell cycle control. Review of 13 additional patients with pathogenic CDKN2A variants suggested associations of germline CDKN2A mutations with an expanded spectrum of non-melanoma familial cancers. To our knowledge, this is the first report of a germline gross deletion of the CDKN2A–CDKN2B locus in an LFS family. These findings highlight the potential contribution of germline CDKN2A deletions to cancer predisposition and the importance of interrogating the full extent of CDKN2A locus in clinical testing gene panels.
Similar content being viewed by others
Introduction
Li–Fraumeni-like (LFL) syndrome is a variant of the Li–Fraumeni syndrome (LFS), a rare autosomal dominant cancer predisposition syndrome characterised by early onset of cancer and a broad tumour spectrum.1 Patients with LFS/LFL typically present with characteristic LFS-associated tumours (soft-tissue sarcoma, osteosarcoma, breast cancer, brain tumour, leukaemia and adrenocortical carcinoma). The majority of these patients have germline mutations in TP53, a known susceptibility gene associated with LFS/LFL.2 Studies have found that up to 20% of LFS1,2 and about 60% of LFL3 families are wild-type for TP53. Germline alterations of other genes such as CHEK2 and CDKN2A in LFS/LFL families without TP53 mutations have been reported, but their role as susceptibility genes as yet remains controversial.1,2
Here we describe a specific patient presenting with both synchronous high-grade malignant peripheral nerve sheath tumour (MPNST) and head and neck squamous cell carcinoma (HNSCC). This patient met the diagnostic criteria4 for LFS, but was wild-type for TP53. Additional sequencing and functional characterisation were performed to investigate other susceptibility genes potentially contributing to the cancers seen in this patient.
Results
Case report
Patient is a 39-year-old male initially diagnosed with moderately differentiated laryngeal squamous cell carcinoma (SCC) with subglottic extension staged as T2N2bM0. Subsequent positron emission tomography (PET) scan revealed a soft-tissue mass adjacent to the right humeral head and another large mass in the left iliopsoas extending to the left inguinal and femoral region, which was diagnosed as grade III MPNST. Apart from tobacco usage, the patient had no remarkable personal or medical record suggestive of high-risk exposure to laryngeal SCC. As his clinical presentation, together with known family history, met the Chompret criteria4 for LFS (Figure 1a), clinical genetic testing was performed for TP53. No pathogenic sequence or copy-number changes were found. However, in this test, TP53 was part of a larger gene panel, which revealed a hemizygous deletion of all three p16INK4A exons of CDKN2A. Given the absence of a personal or family history of melanoma, which might be expected in individuals with CDKN2A (specifically p16INK4A) mutations, we performed germline whole-genome sequencing (WGS) to further elucidate the basis for this patient’s disease.
(a) Family pedigree of the LFL patient. Open and filled symbols represent unaffected and affected individuals respectively, with diagnosis and age of onset indicated under the symbols. Diagonal lines represent deceased individuals. Proband is marked by the arrow. (b) Copy-number analysis of sequenced patient germline DNA revealed focal deletion of the chromosome 9 encompassing the entire CDKN2A–CDKN2B locus. Sequential zooming in of the deleted locus is visualised from top (global copy-number plot) to bottom (sequencing coverage plot at the telomeric and centromeric breakpoints of locus). Genes affected by the deletion are represented by arrows. The sequencing coverage illustrated hemizygous and homozygous loss of the region in germline (blue) and MPNST tumour (red) DNA, respectively. cen, centromeric; tel, telomeric. (c) Real-time qPCR validated the CDKN2A–CDKN2B locus deletion. Coding regions for p14ARF, p16INK4A and p15INK4B were represented by CDKN2A exon 1b, 1a and CDKN2B exon1, respectively. The reduced gene dosage ratio in patient germline and tumours (MPNST, laryngeal SCC) DNA compared with a pool of three healthy controls reflected the hemizgygous and homozygous loss of this locus. Each data point is a mean of quintuplicates with s.e. presented as error bars. P value was computed using Student’s t-test. **P<0.01, ***P<0.001, ****P<0.0001.
Whole-genome sequencing
Copy-number analysis of the WGS data revealed a constitutional focal deletion on chromosome 9 of ~270 kb, resulting in a hemizygous loss of the entire CDKN2A–CDKN2B locus and partially truncating the flanking MTAP and CDKN2B-AS genes (Figure 1b). This region is homozygously deleted in the tumour, as seen by the near-loss of sequencing coverage in the MPNST tumour DNA (Figure 1b). Quantitative PCR (qPCR) validated the deletions in the patient’s germline and tumour DNA, demonstrating a gene dosage ratio of 0.5 and 0.0, respectively, compared with healthy controls (Figure 1c). In addition, analysis of WGS data and PCR detection on the laryngeal SCC tumour (using PGMY-GP consensus primers,5 data not shown) did not indicate ongoing human papillomavirus infection.
Molecular and functional analyses
Hemizygous loss of CDKN2A could affect dosage of two tumour suppressor proteins encoded by the gene, p14ARF and p16INK4A. To investigate, we compared the endogenous messenger RNA and protein expression levels in lymphoblastoid cell lines (LCLs) derived from the patient versus healthy controls. Reverse transcription qPCR analysis confirmed that basal gene expression of p14ARF and p16INK4A was 50% lower than in healthy controls (Figure 2a, P<0.001 and P<0.01, respectively). Immunoblot analysis of these two proteins in the patient LCLs did not show such a significant decrease; however, it should be noted that the p14ARF and p16INK4A levels in the LCLs of healthy controls were variable (Figure 2b). Nevertheless, immunohistochemical analysis of both MPNST and laryngeal SCC tumours were clearly null for p14ARF and p16INK4A (Figure 2c), consistent with the genomic loss observed by WGS (Figure 1b).
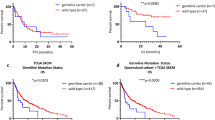
(a) Lower basal messenger RNA (mRNA) expression of CDKN2A and p53 pathway genes in LCL of the LFL patient (III-2) compared with a pool of three healthy controls. Fold change in mRNA was normalised against endogenous GAPDH and then compared against the mean of healthy controls. Each data point is a mean of triplicates with s.e. presented as error bars. P value was computed using Student’s t-test. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001. (b) Basal protein expression of p14ARF, p16INK4A, p53, MDM2 and p21 detected in whole-cell lysates derived from LCLs of the LFL patient compared with three healthy controls. GAPDH was used as loading control. N1, N2 and N3 represent healthy controls; III-2 represents LFL patient with CDKN2A–CDKN2B deletion. (c) Tumour sections of the LFL patient’s MPNST and laryngeal SCC were negatively stained for p14ARF and p16INK4A, implying loss of the protein expression in these tumours. (I–III) Immunohistochemical (IHC) for p14ARF; (IV–V) IHC for p16INK4A. III and VI are tonsil and breast specimens, respectively, used as reference for positive control of the antibody staining. (d) Cell viability assay of the LFL patient compared against a pool of three healthy controls demonstrated significantly higher rate of cell proliferation. Assay was performed in quintuplicates. For healthy controls, LCLs from three healthy volunteers were used and the averaged value from these three lines were represented. Error bars: s.e. P value was computed using Student’s t-test. *P<0.05. (e) Differential MDM2 and p21 expression profiles in MPNST and laryngeal SCC tumours. These two proteins were undetectable in MPNST but expressed in laryngeal SCC tumour, suggesting distinct mechanisms potentially involved in tumorigenesis of the two tumours. However, p53 expression was observed in both tumours. (I–III) MPNST; (IV–VI) laryngeal SCC. (f) The tumour spectrum of additionally reviewed 13 patient cases with CDKN2A pathogenic/likely pathogenic variants presented in a lollipop schematic. The frequency of each phenotype is 1, unless indicated within the lollipop.
A germline hemizygous loss of CDKN2A associated with lower endogenous p14ARF suggests possible p14ARF haploinsufficiency, which may affect p53-dependent cell cycle control even in the absence of a TP53 mutation in the patient.6 The observed significantly higher rate of cell proliferation in the patient LCL supports the possibility of deregulated cell cycle control (Figure 2d). To determine the potential consequences of reduced p14ARF expression on the p53-dependent pathway, we investigated the expression levels of p53, MDM2 and one of the p53 downstream targets, p21. Whereas the messenger RNA and corresponding protein expression levels of MDM2 and p53 were inconsistent, p21 expression in the patient was significantly reduced at both messenger RNA and protein levels (Figures 2a and b). Interestingly, while all three proteins were expressed in the laryngeal SCC tumour, MDM2 and p21 were not detectable in the MPNST (Figure 2e).
Discussion
To our knowledge, this is the first report of a hemizygous CDKN2A–CDKN2B germline deletion in an LFS/LFL family, where the proband presented with MPNST–HNSCC without a personal or family history of melanoma. The CDKN2A–CDKN2B locus encodes three tumour suppressor proteins—p14ARF, p16INK4A and p15INK4B—all involved in cell cycle via p53 and retinoblastoma pathways.7 p16INK4A and p15INK4B inhibit cyclin-dependent kinase (CDK)-mediated phosphorylation of retinoblastoma, thereby promoting G1 cell cycle arrest.7 On the other hand, upon oncogenic stress, p14ARF is induced and inhibits E3 ligase activity of MDM2 towards p53, thus leading to the stabilisation of p53 and activation of p53-mediated cell cycle arrest. As p14ARF acts upstream of p53, it is conceivable that the germline hemizygous deletion of CDKN2A in our patient would phenocopy a hemizygous loss of TP53 in the impaired capacity for arresting cell proliferation. Indeed, it has been alluded that p14ARF haploinsufficiency may predispose to tumour formation.8 It has also been demonstrated that p14ARF-null and p14ARF-hemizygous mice are prone to earlier tumour development, especially of the sarcoma, lymphoma, carcinoma and neural system tumours spectrum,9–11 but to our knowledge, this patient is the first human model that includes p14ARF deficiency. The consistent observation of significantly reduced gene and protein expression of the p53 downstream target p21 in our patient LCL suggests the possible deregulation of p21 (Figures 2a and b), supporting this hypothesis. We note the variability in protein expression among the LCLs of healthy controls, probably due to the variable effects of Epstein–Barr virus in the immortalisation of cell lines12 and are thus interpreted with caution. However, the loss of p21 expression in the MPNST revealed by immunohistochemical analysis (Figure 2e) further supports our hypothesis.
The complete genomic loss of the CDKN2A locus together with ablation of p14ARF and p16INK4A expression in both tumours (Figures 1b and 2c) is consistent with the observations in p14ARF-hemizygous mice, whereby loss of the residual wild-type ARF was observed to accompany tumour development.9 Interestingly, p21 and MDM2 were also undetectable in the MPNST with only p53 staining positive in the tumour, unlike the strong presence of all the three proteins in his laryngeal SCC. This differential protein expression between the patient’s MPNST and laryngeal SCC tumours suggests the driving mechanisms in tumorigenesis of these tumours are potentially distinct. Presence of all three p53 pathway-associated proteins in the laryngeal SCC tumour suggests that tumorigenesis was probably less dependent on the p53 pathway and could potentially be more driven by deregulation in the retinoblastoma pathway associated with loss of p16INK4A.13 In contrast, in the MPNST, expression of p21 appears to be abrogated even in the presence of p53 (Figure 2e), suggesting deregulation of p21 potentially could be indirectly mediated by p14ARF via other transcriptional factors in a p53-independent manner14,15 and phenocopy LFS. Although it is known that p14ARF predominantly inhibits MDM2 thereby stabilizing p53 and promoting its activation,16 emerging body of evidences has shown that p14ARF can interact with a host of proteins that may mediate the tumour suppressor activities of p14ARF17 independent of p53.
Germline mutations in CDKN2A are associated with familial melanoma and pancreatic cancer, and infrequently with neurofibroma,18 HNSCC19 and neural system tumours (astrocytoma and glioma).20 To date, CDKN2A deletions have been reported in only a handful of kindreds displaying clustering of specific tumour spectrum, all of which feature melanoma: cutaneous malignant melanoma-neural system tumour,20–22 melanoma-HNSCC,19 melanoma-neurofibroma18 and malignant melanoma.23,24 We reviewed the clinical records for a series of cancer patients who were found to be positive through gene panel testing for germline CDKN2A mutations to better understand the phenotypic and mutation spectrum. In this series, there were a total of 29 cancers reported among the 14 patients from 12 unique families with germline CDKN2A mutations. The most common cancer was melanoma occurring in seven patients followed by sarcoma, pancreatic and breast cancers each occurring in two patients (Figure 2f, Supplementary Table 1). The overall average age at first cancer diagnosis was 34 years (age range 9–60 years) and the average age at diagnosis of first melanoma was 27 years. Three patients had a history of multiple melanomas and one developed pancreatic cancer 25 years after a melanoma diagnosis. One homozygous individual presented with Hodgkin’s lymphoma at age 12 years and had family history of early-onset lymphoma, jaw tumours, pancreatic, breast and lung cancers. A family history that would suggest hereditary cancer risk was reported in 13 out of 14 patients. Importantly, 2 out of 14 patients met the Chompret criteria and 11 out of 14 reported a family history of cancers characteristic of LFS/LFL spectrum. A review by Baker et al. highlighted a rare contiguous deletion in chromosome 9p21.3 obliterating ~25 genes including CDKN2A, CDKN2B and MTAP in a melanoma-prone family with additional tumour spectrum (neural system tumours, leukaemia, chondrosarcoma, pontomedullary PNET and cervical cancer),25 supporting our findings that genetic alterations involving CDKN2A could potentially underlie hereditary predisposition to cancers beyond melanoma. In our patient with hemizygous germline deletion of CDKN2A, it is prudent to extend melanoma screening given the increased risk of melanoma in families with CDKN2A alterations.
Recent reports revealed that loss of MTAP, a gene flanking and frequently co-deleted with CDKN2A, can render cancer cells sensitive to PRMT5 inhibition, thus opening up opportunities to exploit this vulnerability for treating tumours with MTAP–CDKN2A co-deletion.26 For affected individuals with large deletions involving CDKN2A and MTAP, such as our patient and the family described by Baker et al.,25 the possibility of targeting this PRMT5 dependence raises potential for therapeutic strategies.
Currently, not all clinical testing panels include the entire CDKN2A locus (encompassing both p14ARF and p16INK4A genes). Our study suggests the importance of interrogating the full extent of this locus as alterations to p14ARF may account for a small subset of germline TP53 wild-type LFS/LFL cases and should be included in clinical testing gene panels.
In summary, our study highlights the contribution of CDKN2A germline deletion to cancer predisposition in LFS/LFL patients and expands the non-melanoma phenotypic spectrum of cancers associated with germline CDKN2A mutations. Clinicians should consider genetic testing, including the entire CDKN2A locus, in their patients with LFS/ LFL or those with personal history of sarcoma, and family history of cancers beyond the traditional spectrum of CDKN2A. To the best of our knowledge, this is also the first report of a human p14ARF deficiency model, providing insights into the potential role of p14ARF and deregulation of the p53 pathway in sarcoma tumour development.
Materials and methods
This study was approved by the SingHealth Centralised Institutional Review Board (IRB 2011/826/B). Signed informed consent was given by the patient.
Genetic analysis
Clinical genetic testing was performed at Invitae as previously described.27 WGS of patient genomic DNA purified from peripheral blood and MPNST tissue was performed on an Illumina Hiseq2000 (Illumina Inc., San Diego, CA, USA) to a mean coverage of 72×, data analysed by in-house pipeline and deposited in the European Nucleotide Archive (accession no. PRJEB13761). The genomic deletion was validated by qPCR. For detailed methods, refer to Supplementary Information.
Functional studies
LCLs established by Epstein–Barr virus immortalisation of peripheral blood mononuclear cells of patient and healthy volunteers were used for cell proliferation and expression studies. Cell proliferation was assessed by viability assay using the CellTiter-Glo Luminescent Cell Viability Assay kit (Promega, Madison, WI, USA), whereas gene expression was quantitated using messenger RNA extracted from LCLs by reverse transcription qPCR. Protein expression was assessed by immunoblotting of whole-cell lysates from LCLs. Detailed methods including reverse transcription qPCR primers and immunoblotting antibodies are described in Supplementary Information. Immunohistochemical analysis was performed on 2-μm-thick slides sectioned from patient tumours and scored by a pathologist.
Statistical analysis
P values were computed using two-tailed Student’s t-test and were not adjusted for multiple testing.
References
Malkin, D. Li-fraumeni syndrome. Genes Cancer 2, 475–484 (2011).
Olivier, M. et al. Li-Fraumeni and related syndromes: correlation between tumor type, family structure, and TP53 genotype. Cancer Res. 63, 6643–6650 (2003).
Varley, J. M. Germline TP53 mutations and Li-Fraumeni syndrome. Hum. Mutat. 21, 313–320 (2003).
Tinat, J. et al. 2009 version of the Chompret criteria for Li Fraumeni syndrome. J. Clin. Oncol. 27, e108–e109 (2009).
Voorhoeve, P. M. & Agami, R. The tumor-suppressive functions of the human INK4A locus. Cancer Cell 4, 311–319 (2003).
Kim, W. Y. & Sharpless, N. E. The Regulation of INK4/ARF in Cancer and Aging. Cell 127, 265–275 (2006).
Hewitt, C. et al. Germline mutation of ARF in a melanoma kindred. Hum. Mol. Genet. 11, 1273–1279 (2002).
Kamijo, T., Bodner, S., van de Kamp, E., Randle, D. H. & Sherr, C. J. Tumor spectrum in ARF-deficient mice. Cancer Res. 59, 2217–2222 (1999).
Sharpless, N. E., Ramsey, M. R., Balasubramanian, P., Castrillon, D. H. & DePinho, R. A. The differential impact of p16(INK4a) or p19(ARF) deficiency on cell growth and tumorigenesis. Oncogene 23, 379–385 (2004).
Moore, L. et al. Cooperativity of p19ARF, Mdm2, and p53 in murine tumorigenesis. Oncogene 22, 7831–7837 (2003).
Maruo, S. et al. Epstein-Barr virus nuclear antigens 3C and 3A maintain lymphoblastoid cell growth by repressing p16 INK4A and p14 ARF expression. Proc. Natl Acad. Sci. USA 108, 1919–1924 (2011).
Lechner, M. et al. Targeted next-generation sequencing of head and neck squamous cell carcinoma identifies novel genetic alterations in HPV+ and HPV− tumors. Genome Med. 5, 49 (2013).
Abbas, T. & Dutta, A. p21 in cancer: intricate networks and multiple activities. Nat. Rev. Cancer 9, 400–414 (2009).
Phalke S. et al. p53-Independent regulation of p21Waf1/Cip1 expression and senescence by PRMT6. Nucleic Acids Res. 2012; 40: 9534–9542.
Sherr, C. J. & Weber, J. D. The ARF/p53 pathway. Curr. Opin. Genet. Dev. 10, 94–99 (2000).
Sherr, C. J. Divorcing ARF and p53: an unsettled case. Nat. Rev. Cancer 6, 663–673 (2006).
Petronzelli, F. et al. CDKN2A germline splicing mutation affecting both p16(ink4) and p14(arf) RNA processing in a melanoma/neurofibroma kindred. Genes. Chromosomes Cancer 31, 398–401 (2001).
Cabanillas, R. et al. Novel germline CDKN2A mutation associated with head and neck squamous cell carcinomas and melanomas. Head Neck 35, E80–E84 (2013).
Randerson-Moor, J. A. et al. A germline deletion of p14(ARF) but not CDKN2A in a melanoma-neural system tumour syndrome family. Hum. Mol. Genet. 10, 55–62 (2001).
Bahuau, M. et al. Germ-line deletion involving the INK4 locus in familial proneness to melanoma and nervous system tumors. Cancer Res. 58, 2298–2303 (1998).
Tachibana, I. et al. Investigation of germline PTEN, p53, p16(INK4A)/p14(ARF), and CDK4 alterations in familial glioma. Am. J. Med. Genet. 92, 136–141 (2000).
Knappskog, S., Geisler, J., Arnesen, T., Lillehaug, J. R. & Lønning, P. E. A novel type of deletion in the CDKN2A gene identified in a melanoma-prone family. Genes. Chromosomes Cancer 45, 1155–1163 (2006).
Laud, K. et al. Comprehensive analysis of CDKN2A (p16INK4A/p14ARF) and CDKN2B genes in 53 melanoma index cases considered to be at heightened risk of melanoma. J. Med. Genet. 43, 39–47 (2006).
Baker, M. J. et al. An interstitial deletion within 9p21.3 and extending beyond CDKN2A predisposes to melanoma, neural system tumours and possible haematological malignancies. J. Med. Genet. (e-pub ahead of print 21 January 2016; doi:10.1136/jmedgenet-2015-103446).
Shipman, L. Genetics: common co-deletion isn’t a silent passenger. Nat. Rev. Cancer 16, 197–197 (2016).
Lincoln, S. E. et al. A systematic comparison of traditional and multigene panel testing for hereditary breast and ovarian cancer genes in more than 1000 patients. J. Mol. Diagn. 17, 533–544 (2015).
Winder, D. M. et al. Sensitive HPV detection in oropharyngeal cancers. BMC Cancer 9, 440 (2009).
Acknowledgements
We thank our patients and research participants for their contribution to this study. We would also like to thank the TP53 lab at A*STAR for their kind gifts of antibodies and reagents. We also acknowledge Magdalene Koh of SingHealth Advanced Molecular Pathology Laboratory for her valuable assistance in pathological analyses. We are grateful to Sir David Lane, David Virshup and the Reversade lab at A*STAR for helpful comments. J.N. is the recipient of the NMRC Singapore Transition Award.
Author information
Authors and Affiliations
Contributions
S.H.C. and J.N. conceived and designed the study. M.K.A., M.F., J.W., S.A. and J.N. consulted the patient and M.M.-D. provided genetic counselling. S.H.C., W.K.L., J.Q.L., N.D.B.I., M.M.-D., C.N.C.Y., K.S. and K.I. contributed to data acquisition, analysis and interpretation. S.T.M., K.V., E.D.E., J.F. and S.E.L. performed the clinical genetic testing and analysis of additional patients. S.H.C., W.K.L. and J.N. drafted the manuscript. All authors contributed to critical revision of the manuscript for intellectual content and final approval of the manuscript. T.B.T. and J.N. are the guarantors of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the npj Genomic Medicine website (http://www.nature.com/npjgenmed)
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chan, S., Lim, W., Michalski, S. et al. Germline hemizygous deletion of CDKN2A–CDKN2B locus in a patient presenting with Li–Fraumeni syndrome. npj Genomic Med 1, 16015 (2016). https://doi.org/10.1038/npjgenmed.2016.15
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjgenmed.2016.15
This article is cited by
-
Hereditary oral squamous cell carcinoma associated with CDKN2A germline mutation: A case report
Journal of Otolaryngology - Head & Neck Surgery (2022)
-
CDKN2A germline alterations and the relevance of genotype-phenotype associations in cancer predisposition
Hereditary Cancer in Clinical Practice (2021)
-
Germinal GLT8D1, GATAD2A and SLC25A39 mutations in a patient with a glomangiopericytal tumor and five different sarcomas over a 10-year period
Scientific Reports (2021)
-
The functional property of royal jelly 10-hydroxy-2-decenoic acid as a melanogenesis inhibitor
BMC Complementary and Alternative Medicine (2017)