Abstract
Anemia is a major source of morbidity and mortality worldwide. Here we review recent insights into how red blood cells (RBCs) are produced, the pathogenic mechanisms underlying various forms of anemia, and novel therapies derived from these findings. It is likely that these new insights, mainly arising from basic scientific studies, will contribute immensely to both the understanding of frequently debilitating forms of anemia and the ability to treat affected patients. Major worldwide diseases that are likely to benefit from new advances include the hemoglobinopathies (β-thalassemia and sickle cell disease); rare genetic disorders of RBC production; and anemias associated with chronic kidney disease, inflammation, and cancer. Promising new approaches to treatment include drugs that target recently defined pathways in RBC production, iron metabolism, and fetal globin-family gene expression, as well as gene therapies that use improved viral vectors and newly developed genome editing technologies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Debbie Maizels/Nature Publishing Group

Debbie Maizels/Nature Publishing Group

Debbie Maizels/Nature Publishing Group

Debbie Maizels/Nature Publishing Group

Debbie Maizels/Nature Publishing Group
Similar content being viewed by others
References
Kassebaum, N.J. et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 123, 615–624 (2014).
Weatherall, D.J. The inherited diseases of hemoglobin are an emerging global health burden. Blood 115, 4331–4336 (2010).
Palis, J. Primitive and definitive erythropoiesis in mammals. Front Physiol. 5, 3 (2014).
Doulatov, S., Notta, F., Laurenti, E. & Dick, J.E. Hematopoiesis: a human perspective. Cell Stem Cell 10, 120–136 (2012).
Yamamoto, R. et al. Clonal analysis unveils self-renewing lineage-restricted progenitors generated directly from hematopoietic stem cells. Cell 154, 1112–1126 (2013).
Sanjuan-Pla, A. et al. Platelet-biased stem cells reside at the apex of the haematopoietic stem cell hierarchy. Nature 502, 232–236 (2013).
Sun, J. et al. Clonal dynamics of native haematopoiesis. Nature 514, 322–327 (2014).
Paulson, R.F. Targeting a new regulator of erythropoiesis to alleviate anemia. Nat. Med. 20, 334–335 (2014).
Spivak, J.L. The anaemia of cancer: death by a thousand cuts. Nat. Rev. Cancer 5, 543–555 (2005).
Dai, C.H., Price, J.O., Brunner, T. & Krantz, S.B. Fas ligand is present in human erythroid colony-forming cells and interacts with Fas induced by interferon-γ to produce erythroid cell apoptosis. Blood 91, 1235–1242 (1998).
Orkin, S.H. & Nathan, D.G. Nathan and Oski's Hematology of Infancy and Childhood, (Saunders/Elsevier, 2009).
Landowski, M. et al. Novel deletion of RPL15 identified by array-comparative genomic hybridization in Diamond–Blackfan anemia. Hum. Genet. 132, 1265–1274 (2013).
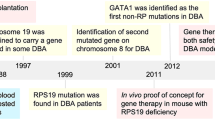
Ludwig, L.S. et al. Altered translation of GATA1 in Diamond–Blackfan anemia. Nat. Med. 20, 748–753 (2014).
Sankaran, V.G. et al. Exome sequencing identifies GATA1 mutations resulting in Diamond–Blackfan anemia. J. Clin. Invest. 122, 2439–2443 (2012).
van Wijk, R. & van Solinge, W.W. The energy-less red blood cell is lost: erythrocyte enzyme abnormalities of glycolysis. Blood 106, 4034–4042 (2005).
Perrotta, S., Gallagher, P.G. & Mohandas, N. Hereditary spherocytosis. Lancet 372, 1411–1426 (2008).
Sankaran, V.G. & Nathan, D.G. Thalassemia: an overview of 50 years of clinical research. Hematol. Oncol. Clin. North Am. 24, 1005–1020 (2010).
Khandros, E., Thom, C.S., D'Souza, J. & Weiss, M.J. Integrated protein quality-control pathways regulate free α-globin in murine β-thalassemia. Blood 119, 5265–5275 (2012).
Arlet, J.B. et al. HSP70 sequestration by free α-globin promotes ineffective erythropoiesis in β-thalassaemia. Nature 514, 242–246 (2014).
Rees, D.C., Williams, T.N. & Gladwin, M.T. Sickle-cell disease. Lancet 376, 2018–2031 (2010).
Manwani, D. & Frenette, P.S. Vaso-occlusion in sickle cell disease: pathophysiology and novel targeted therapies. Hematology (Am. Soc. Hematol. Educ. Program) 2013, 362–369 (2013).
Gladwin, M.T., Kanias, T. & Kim-Shapiro, D.B. Hemolysis and cell-free hemoglobin drive an intrinsic mechanism for human disease. J. Clin. Invest. 122, 1205–1208 (2012).
Gladwin, M.T. & Ofori-Acquah, S.F. Erythroid DAMPs drive inflammation in SCD. Blood 123, 3689–3690 (2014).
Chou, S.T. Transfusion therapy for sickle cell disease: a balancing act. Hematology (Am. Soc. Hematol. Educ. Program) 2013, 439–446 (2013).
Locatelli, F. et al. Outcome of patients with hemoglobinopathies given either cord blood or bone marrow transplantation from an HLA-identical sibling. Blood 122, 1072–1078 (2013).
Jelkmann, W. Physiology and pharmacology of erythropoietin. Transfus. Med. Hemother. 40, 302–309 (2013).
Macdougall, I.C. New anemia therapies: translating novel strategies from bench to bedside. Am. J. Kidney Dis. 59, 444–451 (2012).
Malyszko, J. New renal anemia drugs: is there really anything new on the horizon? Expert Opin. Emerg. Drugs 19, 1–4 (2014).
Jha, V. et al. Chronic kidney disease: global dimension and perspectives. Lancet 382, 260–272 (2013).
Witmer, C.M. Hematologic manifestations of systemic disease (including iron deficiency, anemia of inflammation and DIC). Pediatr. Clin. North Am. 60, 1337–1348 (2013).
Weiss, G. & Goodnough, L.T. Anemia of chronic disease. N. Engl. J. Med. 352, 1011–1023 (2005).
Nemeth, E. et al. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J. Clin. Invest. 113, 1271–1276 (2004).
Wang, C.Q., Udupa, K.B. & Lipschitz, D.A. Interferon-γ exerts its negative regulatory effect primarily on the earliest stages of murine erythroid progenitor cell development. J. Cell. Physiol. 162, 134–138 (1995).
Birgegård, G. et al. Cancer-related anemia: pathogenesis, prevalence and treatment. Oncology 68 (suppl. 1), 3–11 (2005).
Bejar, R. & Steensma, D.P. Recent developments in myelodysplastic syndromes. Blood 124, 2793–2803 (2014).
Wrighton, N.C. et al. Small peptides as potent mimetics of the protein hormone erythropoietin. Science 273, 458–464 (1996).
Macdougall, I.C. et al. Peginesatide for anemia in patients with chronic kidney disease not receiving dialysis. N. Engl. J. Med. 368, 320–332 (2013).
Fishbane, S. et al. Peginesatide in patients with anemia undergoing hemodialysis. N. Engl. J. Med. 368, 307–319 (2013).
Bennett, C.L., Jacob, S., Hymes, J., Usvyat, L.A. & Maddux, F.W. Anaphylaxis and hypotension after administration of peginesatide. N. Engl. J. Med. 370, 2055–2056 (2014).
Schofield, C.J. & Ratcliffe, P.J. Oxygen sensing by HIF hydroxylases. Nat. Rev. Mol. Cell Biol. 5, 343–354 (2004).
Raje, N. & Vallet, S. Sotatercept, a soluble activin receptor type 2A IgG-Fc fusion protein for the treatment of anemia and bone loss. Curr. Opin. Mol. Ther. 12, 586–597 (2010).
Sherman, M.L. et al. Multiple-dose, safety, pharmacokinetic, and pharmacodynamic study of sotatercept (ActRIIA-IgG1), a novel erythropoietic agent, in healthy postmenopausal women. J. Clin. Pharmacol. 53, 1121–1130 (2013).
Dussiot, M. et al. An activin receptor IIA ligand trap corrects ineffective erythropoiesis in β-thalassemia. Nat. Med. 20, 398–407 (2014).
Suragani, R.N. et al. Transforming growth factor-β superfamily ligand trap ACE-536 corrects anemia by promoting late-stage erythropoiesis. Nat. Med. 20, 408–414 (2014).
Loffredo, F.S. et al. Growth differentiation factor 11 is a circulating factor that reverses age-related cardiac hypertrophy. Cell 153, 828–839 (2013).
Sinha, M. et al. Restoring systemic GDF11 levels reverses age-related dysfunction in mouse skeletal muscle. Science 344, 649–652 (2014).
Katsimpardi, L. et al. Vascular and neurogenic rejuvenation of the aging mouse brain by young systemic factors. Science 344, 630–634 (2014).
Villeda, S.A. et al. Young blood reverses age-related impairments in cognitive function and synaptic plasticity in mice. Nat. Med. 20, 659–663 (2014).
Coulon, S. et al. Polymeric IgA1 controls erythroblast proliferation and accelerates erythropoiesis recovery in anemia. Nat. Med. 17, 1456–1465 (2011).
Richardson, C.L. et al. Isocitrate ameliorates anemia by suppressing the erythroid iron restriction response. J. Clin. Invest. 123, 3614–3623 (2013).
Sankaran, V.G. & Orkin, S.H. The switch from fetal to adult hemoglobin. Cold Spring Harb. Perspect. Med. 3, a011643 (2013).
Sankaran, V.G. et al. A functional element necessary for fetal hemoglobin silencing. N. Engl. J. Med. 365, 807–814 (2011).
Sankaran, V.G. Targeted therapeutic strategies for fetal hemoglobin induction. Hematology (Am. Soc. Hematol. Educ. Program) 2011, 459–465 (2011).
Musallam, K.M. et al. Fetal hemoglobin levels and morbidity in untransfused patients with β-thalassemia intermedia. Blood 119, 364–367 (2012).
Platt, O.S. Hydroxyurea for the treatment of sickle cell anemia. N. Engl. J. Med. 358, 1362–1369 (2008).
Sankaran, V.G. et al. Human fetal hemoglobin expression is regulated by the developmental stage–specific repressor BCL11A. Science 322, 1839–1842 (2008).
Bauer, D.E. et al. An erythroid enhancer of BCL11A subject to genetic variation determines fetal hemoglobin level. Science 342, 253–257 (2013).
Xu, J. et al. Correction of sickle cell disease in adult mice by interference with fetal hemoglobin silencing. Science 334, 993–996 (2011).
Sankaran, V.G. et al. Developmental and species-divergent globin switching are driven by BCL11A. Nature 460, 1093–1097 (2009).
Wilber, A. et al. Therapeutic levels of fetal hemoglobin in erythroid progeny of β-thalassemic CD34+ cells after lentiviral vector-mediated gene transfer. Blood 117, 2817–2826 (2011).
Xu, J. et al. Corepressor-dependent silencing of fetal hemoglobin expression by BCL11A. Proc. Natl. Acad. Sci. USA 110, 6518–6523 (2013).
Suzuki, M., Yamamoto, M. & Engel, J.D. Fetal globin gene repressors as drug targets for molecular therapies to treat the b-globinopathies. Mol. Cell. Biol. 34, 3560–3569 (2014).
Sankaran, V.G. et al. MicroRNA-15a and -16-1 act via MYB to elevate fetal hemoglobin expression in human trisomy 13. Proc. Natl. Acad. Sci. USA 108, 1519–1524 (2011).
Galarneau, G. et al. Fine-mapping at three loci known to affect fetal hemoglobin levels explains additional genetic variation. Nat. Genet. 42, 1049–1051 (2010).
Sankaran, V.G. et al. Rare complete loss of function provides insight into a pleiotropic genome-wide association study locus. Blood 122, 3845–3847 (2013).
Stadhouders, R. et al. HBS1L-MYB intergenic variants modulate fetal hemoglobin via long-range MYB enhancers. J. Clin. Invest. 124, 1699–1710 (2014).
Zuber, J. et al. An integrated approach to dissecting oncogene addiction implicates a Myb-coordinated self-renewal program as essential for leukemia maintenance. Genes Dev. 25, 1628–1640 (2011).
Borg, J. et al. Haploinsufficiency for the erythroid transcription factor KLF1 causes hereditary persistence of fetal hemoglobin. Nat. Genet. 42, 801–805 (2010).
Giardine, B. et al. Systematic documentation and analysis of human genetic variation in hemoglobinopathies using the microattribution approach. Nat. Genet. 43, 295–301 (2011).
Arnaud, L. et al. A dominant mutation in the gene encoding the erythroid transcription factor KLF1 causes a congenital dyserythropoietic anemia. Am. J. Hum. Genet. 87, 721–727 (2010).
Campbell, A.D. et al. Forced TR2/TR4 expression in sickle cell disease mice confers enhanced fetal hemoglobin synthesis and alleviated disease phenotypes. Proc. Natl. Acad. Sci. USA 108, 18808–18813 (2011).
Bradner, J.E. et al. Chemical genetic strategy identifies histone deacetylase 1 (HDAC1) and HDAC2 as therapeutic targets in sickle cell disease. Proc. Natl. Acad. Sci. USA 107, 12617–12622 (2010).
Shi, L., Cui, S., Engel, J.D. & Tanabe, O. Lysine-specific demethylase 1 is a therapeutic target for fetal hemoglobin induction. Nat. Med. 19, 291–294 (2013).
Libani, I.V. et al. Decreased differentiation of erythroid cells exacerbates ineffective erythropoiesis in β-thalassemia. Blood 112, 875–885 (2008).
Breda, L. & Rivella, S. Modulators of erythropoiesis: emerging therapies for hemoglobinopathies and disorders of red cell production. Hematol. Oncol. Clin. North Am. 28, 375–386 (2014).
Gutsaeva, D.R. et al. Inhibition of cell adhesion by anti-P-selectin aptamer: a new potential therapeutic agent for sickle cell disease. Blood 117, 727–735 (2011).
Chang, J. et al. GMI-1070, a novel pan-selectin antagonist, reverses acute vascular occlusions in sickle cell mice. Blood 116, 1779–1786 (2010).
Chang, J., Shi, P.A., Chiang, E.Y. & Frenette, P.S. Intravenous immunoglobulins reverse acute vaso-occlusive crises in sickle cell mice through rapid inhibition of neutrophil adhesion. Blood 111, 915–923 (2008).
Jang, J.E., Hod, E.A., Spitalnik, S.L. & Frenette, P.S. CXCL1 and its receptor, CXCR2, mediate murine sickle cell vaso-occlusion during hemolytic transfusion reactions. J. Clin. Invest. 121, 1397–1401 (2011).
Wallace, K.L. et al. NKT cells mediate pulmonary inflammation and dysfunction in murine sickle cell disease through production of IFN-γ and CXCR3 chemokines. Blood 114, 667–676 (2009).
Field, J.J. et al. Sickle cell vaso-occlusion causes activation of iNKT cells that is decreased by the adenosine A2A receptor agonist regadenoson. Blood 121, 3329–3334 (2013).
Embury, S.H., Garcia, J.F., Mohandas, N., Pennathur-Das, R. & Clark, M.R. Effects of oxygen inhalation on endogenous erythropoietin kinetics, erythropoiesis, and properties of blood cells in sickle-cell anemia. N. Engl. J. Med. 311, 291–295 (1984).
Abdulmalik, O. et al. 5-hydroxymethyl-2-furfural modifies intracellular sickle haemoglobin and inhibits sickling of red blood cells. Br. J. Haematol. 128, 552–561 (2005).
Safo, M.K. & Kato, G.J. Therapeutic strategies to alter the oxygen affinity of sickle hemoglobin. Hematol. Oncol. Clin. North Am. 28, 217–231 (2014).
Finberg, K.E. Striking the target in iron overload disorders. J. Clin. Invest. 123, 1424–1427 (2013).
Tanno, T. et al. High levels of GDF15 in thalassemia suppress expression of the iron regulatory protein hepcidin. Nat. Med. 13, 1096–1101 (2007).
Kautz, L. et al. Identification of erythroferrone as an erythroid regulator of iron metabolism. Nat. Genet. 46, 678–684 (2014).
Ganz, T. Systemic iron homeostasis. Physiol. Rev. 93, 1721–1741 (2013).
Schmidt, P.J. et al. An RNAi therapeutic targeting Tmprss6 decreases iron overload in Hfe−/− mice and ameliorates anemia and iron overload in murine β-thalassemia intermedia. Blood 121, 1200–1208 (2013).
Guo, S. et al. Reducing TMPRSS6 ameliorates hemochromatosis and beta-thalassemia in mice. J. Clin. Invest. 123, 1531–1541 (2013).
Preza, G.C. et al. Minihepcidins are rationally designed small peptides that mimic hepcidin activity in mice and may be useful for the treatment of iron overload. J. Clin. Invest. 121, 4880–4888 (2011).
Ramos, E. et al. Minihepcidins prevent iron overload in a hepcidin-deficient mouse model of severe hemochromatosis. Blood 120, 3829–3836 (2012).
Gardenghi, S. et al. Hepcidin as a therapeutic tool to limit iron overload and improve anemia in β-thalassemic mice. J. Clin. Invest. 120, 4466–4477 (2010).
Li, H. et al. Transferrin therapy ameliorates disease in β-thalassemic mice. Nat. Med. 16, 177–182 (2010).
Kohn, D.B., Pai, S.Y. & Sadelain, M. Gene therapy through autologous transplantation of gene-modified hematopoietic stem cells. Biol. Blood Marrow Transplant. 19, S64–S69 (2013).
May, C. et al. Therapeutic haemoglobin synthesis in β-thalassaemic mice expressing lentivirus-encoded human β-globin. Nature 406, 82–86 (2000).
Pawliuk, R. et al. Correction of sickle cell disease in transgenic mouse models by gene therapy. Science 294, 2368–2371 (2001).
Cavazzana-Calvo, M. et al. Transfusion independence and HMGA2 activation after gene therapy of human β-thalassaemia. Nature 467, 318–322 (2010).
Hacein-Bey-Abina, S. et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J. Clin. Invest. 118, 3132–3142 (2008).
Stein, S. et al. Genomic instability and myelodysplasia with monosomy 7 consequent to EVI1 activation after gene therapy for chronic granulomatous disease. Nat. Med. 16, 198–204 (2010).
Deng, W. et al. Reactivation of developmentally silenced globin genes by forced chromatin looping. Cell 158, 849–860 (2014).
Flygare, J., Olsson, K., Richter, J. & Karlsson, S. Gene therapy of Diamond–Blackfan anemia CD34+ cells leads to improved erythroid development and engraftment following transplantation. Exp. Hematol. 36, 1428–1435 (2008).
Bedel, A. et al. Metabolic correction of congenital erythropoietic porphyria with iPSCs free of reprogramming factors. Am. J. Hum. Genet. 91, 109–121 (2012).
Robert-Richard, E. et al. Effective gene therapy of mice with congenital erythropoietic porphyria is facilitated by a survival advantage of corrected erythroid cells. Am. J. Hum. Genet. 82, 113–124 (2008).
Rovira, A. et al. Stable in vivo expression of glucose-6-phosphate dehydrogenase (G6PD) and rescue of G6PD deficiency in stem cells by gene transfer. Blood 96, 4111–4117 (2000).
Meza, N.W. et al. Rescue of pyruvate kinase deficiency in mice by gene therapy using the human isoenzyme. Mol. Ther. 17, 2000–2009 (2009).
Xie, F. et al. Seamless gene correction of β-thalassemia mutations in patient-specific iPSCs using CRISPR/Cas9 and piggyBac. Genome Res. 24, 1526–1533 (2014).
Sun, N. & Zhao, H. Seamless correction of the sickle cell disease mutation of the HBB gene in human induced pluripotent stem cells using TALENs. Biotechnol. Bioeng. 111, 1048–1053 (2014).
Sankaran, V.G. & Orkin, S.H. Genome-wide association studies of hematologic phenotypes: a window into human hematopoiesis. Curr. Opin. Genet. Dev. 23, 339–344 (2013).
Ulirsch, J.C. et al. Altered chromatin occupancy of master regulators underlies evolutionary divergence in the transcriptional landscape of erythroid differentiation. PLoS Genet. 10, e1004890 (2014).
Pishesha, N. et al. Transcriptional divergence and conservation of human and mouse erythropoiesis. Proc. Natl. Acad. Sci. USA 111, 4103–4108 (2014).
An, X. et al. Global transcriptome analyses of human and murine terminal erythroid differentiation. Blood 123, 3466–3477 (2014).
Bunn, H.F. Erythropoietin. Cold Spring Harb. Perspect. Med. 3, a011619 (2013).
Naldini, L. Ex vivo gene transfer and correction for cell-based therapies. Nat. Rev. Genet. 12, 301–315 (2011).
Hsu, P.D., Lander, E.S. & Zhang, F. Development and applications of CRISPR-Cas9 for genome engineering. Cell 157, 1262–1278 (2014).
Gupta, R.M. & Musunuru, K. Expanding the genetic editing tool kit: ZFNs, TALENs, and CRISPR-Cas9. J. Clin. Invest. 124, 4154–4161 (2014).
Holt, N. et al. Human hematopoietic stem/progenitor cells modified by zinc-finger nucleases targeted to CCR5 control HIV-1 in vivo. Nat. Biotechnol. 28, 839–847 (2010).
Lombardo, A. et al. Gene editing in human stem cells using zinc-finger nucleases and integrase-defective lentiviral vector delivery. Nat. Biotechnol. 25, 1298–1306 (2007).
Genovese, P. et al. Targeted genome editing in human repopulating haematopoietic stem cells. Nature 510, 235–240 (2014).
Acknowledgements
We apologize for being unable to cite numerous papers and studies in this field due to space limitations. We are grateful to N. Mohandas, A. Nienhuis, and D. Nathan for comments and suggestions on this Review. V.G.S. received support from the US National Institutes of Health (NIH; R01 DK103794, R21 HL120791, U01 HL117720), a March of Dimes Basil O'Connor Scholar Award and an award from the Diamond–Blackfan Anemia Foundation. M.J.W. received support from the NIH (R01 DK0923128, R01 DK61692, R01 HL088554). We are grateful to the many patients with anemia and their families, who have advanced the field by participating in clinical studies and advocating research.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
M.J.W. is a consultant for GlaxoSmithKline and receives research funding for studies on erythropoiesis from Biogen Idec.
Rights and permissions
About this article
Cite this article
Sankaran, V., Weiss, M. Anemia: progress in molecular mechanisms and therapies. Nat Med 21, 221–230 (2015). https://doi.org/10.1038/nm.3814
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3814
This article is cited by
-
NGS-basierte Molekulargenetik der Leukämie – ein leistungsfähiger und dezentraler Lösungsansatz
Die Pathologie (2023)
-
A rare mutation (p.F149del) of the NT5C3A gene is associated with pyrimidine 5′-nucleotidase deficiency
Cellular & Molecular Biology Letters (2022)
-
Genome-based therapeutic interventions for β-type hemoglobinopathies
Human Genomics (2021)
-
Iron control of erythroid microtubule cytoskeleton as a potential target in treatment of iron-restricted anemia
Nature Communications (2021)
-
Advances in genome editing: the technology of choice for precise and efficient β-thalassemia treatment
Gene Therapy (2021)