Mahalaxmi Aburi 
Schizophrenia is primarily believed to be a genetic disorder resulting in the chemical imbalance of certain neurotransmitters — catecholamines such as dopamine, epinephrine, and norepinephrine. Even though there is consensus that multiple genes are associated with the devastating effects of schizophrenia, COMT (catechol-O-methyltransferase), an enzyme that degrades catecholamines has been one of the most exploited molecular targets.
COMT: The most exploited target
Julius Axelrod won a Nobel Prize for his 1957 discovery of COMT at US National Institute for Health. There are two main pieces of evidence pointing to COMT as a key player in the development of schizophrenia.
Functional evidence : The classic hypothesis widely held for more than half a century is that dysfunction of dopamine signalling holds the key to the pathophysiology of schizophrenia. Therefore, COMT is especially attractive since it helps maintain appropriate levels of dopamine. However, understanding the function of COMT and its polymorphism in humans remains incomplete, though there is no shortage of elegant studies.
So far, most studies have focused on the effects of one particular common polymorphism, a variation in the amino acid sequence of the enzyme. In this variation the amino acid valine (Val) at position 108 is replaced with methionine (Met)1. This polymorphism is co-dominant and causes a 3- to 4-fold decrease in the molecular thermo-stability of the protein, which decreases its abundance in the human brain altering the enzyme's ability to break down dopamine.
Genetic evidence : The COMT gene is found in a region of the 22nd chromosome of the human genome which is shown in genetic linkage studies for harbouring schizophrenia genes. Individuals with a deletion in this region (1/ 4000 human births) have 30 times more likelihood of developing schizophrenia. Furthermore, there are studies that have indicated COMT itself to predict schizophrenia in individuals, yet these studies are highly controversial.
These studies, termed genetic association approach, involve the screening of the variability of the gene and see whether any one variation is more frequently found in schizophrenics. To date, this has been the least compelling evidence for the implication of COMT in schizophrenia and, thus, it is this aspect of the genetic association approach which has been highly debatable.
COMT research in India and abroad
A ground-breaking paper reported in 2001 that individuals with Val in place of Met showed poorer cognitive function and an elevated risk for schizophrenia. These associations, along with a multitude of other psychological and psychiatric phenotypes, have since been tested in labs across the world. Since then several key institutes in India and abroad have looked extensively at the potential connection between changes in the COMT gene and the risk of developing schizophrenia.
Labs of Ritushree Kukreti and her colleagues at the Institute of Genomics and Integrative Biology, New Delhi, have been exploring the genetic contribution of COMT in schizophrenia. Their preliminary forays into this field have been very encouraging. Their studies have indicated a weak/nominal role of individual variations but suggest interacting effects within the COMT gene polymorphisms that influence the susceptibility to schizophrenia. They intend to extend their studies to gender base as these would provide a framework for designing future epidemiological studies to identify Indian sub-populations with differential response to a given drug. Their results provide a platform for designing further prospective trials for evaluation and development of new drugs.
Diagram of human catechol-O-methyl transferase (COMT) in complex with S-adenosyl methionine and 3,5-dinitrocatechol. Credit: Wikimedia Commons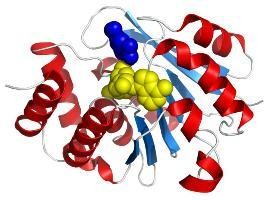
This inconsistency can be partly explained by the lack of consistent study design, low (statistical) power of studies, etiological heterogeneity and ill-defined clinical endophenotypes (a special type of biomarker for psychiatric disorder) in individual studies. There is an urgent need for maintaining inter-study homogeneity by developing clear phenotypic definitions and assaying the functional role of statistical associations.
The Department of Genetics of University of Delhi has tested the association of COMT as an influential candidates in North Indian schizophrenia subjects. However the researchers reported no significant association between the two. In another report, they claimed that contribution of dopaminergic pathway gene polymorphisms including COMT towards schizophrenia seems possible.
The Division of Psychological Medicine and Psychiatry, Institute of Psychiatry, King's College London also works on elucidating the role of COMT in schizophrenia. Its researchers feel COMT should be considered an important player while investigating gene-gene and gene-environment interactions on the etiology and pathophysiology of schizophrenia. However, they too believe that COMT alone is not sufficient to cause schizophrenia.
Joseph Gogos and Mark Slifstein at Columbia University have also been involved in COMT research. Gogos' lab has shown that COMT's polymorphic activity can play a role under conditions that increase dopamine release, especially in the prefrontal cortex. These findings were subsequently confirmed in human studies, .
Such conditions may include mutations in other genes or environmental factors. The researchers think genetic association studies of the clinical syndrome may have failed because they did not take into account gene-gene and gene-environment interactions. However to do this, one needs very large patients samples, which may be practically unattainable, and animal modelling may be the preferred way to go. COMT polymorphic activity may play a general role in schizophrenia susceptibility but this really depends on the context. However a role of COMT Val/Met variant in schizophrenia has been conclusively excluded, according to Gogos.
Mark Slifstein's lab has carried out extensive work on patients suffering from schizophrenia and COMT concluding that the high-activity Val allele was found to be slightly higher in patients with schizophrenia compared with controls in some studies but not in all. It has been suggested that the influence of this allele on schizophrenia susceptibility may vary for different ethnic populations and that other variants in COMT modulate the effect of Val/Met on dopamine function.
However, their work clearly implicates that the COMT Val/Val allele may further compromise dopamine function in individuals with schizophrenia. The evidence, Slifstein says, is that the allele is no more prevalent in schizophrenia than in the general population, so it's hard to imagine it to be global causative. However, people who already have cognitive symptoms from other causes would have their condition exacerbated if they also carried the Val/Val allele.
It is clear that a single polymorphism is certainly not the only determinant of COMT function. COMT has become one of the most studied genes in psychiatric disorders because of its function, position, and the extent to which a genetic variation can influence its function. With respect to schizophrenia, it is still unclear whether these findings can all be attributed to technical anomalies in study design and implementation or reflect an existence of a complex relationship between the genetic networks.
The fact that no robust conclusions can be drawn about the relationship between COMT and schizophrenia despite the numerous samples studied and the difficulty generated by a gene with a clear and highly plausible functional relationship with schizophrenia highlights the challenges that await investigators tackling the newer generation of potential-risk genes where they would neither have the luxury of known functional variation nor an obvious functional relationship with disease.
The COMT gene is probably not a gene for any particular mental disorder as conceptualized in contemporary classification systems. The phrase "a gene for" seems inappropriate for psychiatric disorders as many genes that influence risk for mental disorders are not diagnostically specific in their effect.
The author is an Assistant Research Scientist at the Research Foundation for Mental Hygiene (RFMH), New York and Columbia University, New York.
