Abstract
Thiopurine therapy, commonly used in autoimmune conditions, can be complicated by life-threatening leukopenia. This leukopenia is associated with genetic variation in TPMT (encoding thiopurine S-methyltransferase). Despite a lower frequency of TPMT mutations in Asians, the incidence of thiopurine-induced leukopenia is higher in Asians than in individuals of European descent. Here we performed an Immunochip-based 2-stage association study in 978 Korean subjects with Crohn's disease treated with thiopurines. We identified a nonsynonymous SNP in NUDT15 (encoding p.Arg139Cys) that was strongly associated with thiopurine-induced early leukopenia (odds ratio (OR) = 35.6; Pcombined = 4.88 × 10−94). In Koreans, this variant demonstrated sensitivity and specificity of 89.4% and 93.2%, respectively, for thiopurine-induced early leukopenia (in comparison to 12.1% and 97.6% for TPMT variants). Although rare, this SNP was also strongly associated with thiopurine-induced leukopenia in subjects with inflammatory bowel disease of European descent (OR = 9.50; P = 4.64 × 10−4). Thus, NUDT15 is a pharmacogenetic determinant for thiopurine-induced leukopenia in diverse populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Timmer, A., McDonald, J.W., Tsoulis, D.J. & Macdonald, J.K. Azathioprine and 6-mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Database Syst. Rev. 9, CD000478 (2012).
Prefontaine, E., Sutherland, L.R., Macdonald, J.K. & Cepoiu, M. Azathioprine or 6-mercaptopurine for maintenance of remission in Crohn's disease. Cochrane Database Syst. Rev. 1, CD000067 (2009).
Present, D.H., Meltzer, S.J., Krumholz, M.P., Wolke, A. & Korelitz, B.I. 6-Mercaptopurine in the management of inflammatory bowel disease: short- and long-term toxicity. Ann. Intern. Med. 111, 641–649 (1989).
Connell, W.R., Kamm, M.A., Ritchie, J.K. & Lennard-Jones, J.E. Bone marrow toxicity caused by azathioprine in inflammatory bowel disease: 27 years of experience. Gut 34, 1081–1085 (1993).
Fraser, A.G., Orchard, T.R. & Jewell, D.P. The efficacy of azathioprine for the treatment of inflammatory bowel disease: a 30 year review. Gut 50, 485–489 (2002).
Colombel, J.F. et al. Genotypic analysis of thiopurine S-methyltransferase in patients with Crohn's disease and severe myelosuppression during azathioprine therapy. Gastroenterology 118, 1025–1030 (2000).
Dewit, O. et al. Limitations of extensive TPMT genotyping in the management of azathioprine-induced myelosuppression in IBD patients. Clin. Biochem. 44, 1062–1066 (2011).
Booth, R.A. et al. Assessment of thiopurine S-methyltransferase activity in patients prescribed thiopurines: a systematic review. Ann. Intern. Med. 154, 814–823 (2011).
Kumagai, K. et al. Allelotype frequency of the thiopurine methyltransferase (TPMT) gene in Japanese. Pharmacogenetics 11, 275–278 (2001).
Cao, Q., Zhu, Q., Shang, Y., Gao, M. & Si, J. Thiopurine methyltransferase gene polymorphisms in Chinese patients with inflammatory bowel disease. Digestion 79, 58–63 (2009).
Kim, J.H. et al. Influences of thiopurine methyltransferase genotype and activity on thiopurine-induced leukopenia in Korean patients with inflammatory bowel disease: a retrospective cohort study. J. Clin. Gastroenterol. 44, e242–e248 (2010).
Takatsu, N. et al. Adverse reactions to azathioprine cannot be predicted by thiopurine S-methyltransferase genotype in Japanese patients with inflammatory bowel disease. J. Gastroenterol. Hepatol. 24, 1258–1264 (2009).
Collie-Duguid, E.S. et al. The frequency and distribution of thiopurine methyltransferase alleles in Caucasian and Asian populations. Pharmacogenetics 9, 37–42 (1999).
Lee, H.J. et al. The safety and efficacy of azathioprine and 6-mercaptopurine in the treatment of Korean patients with Crohn's disease. Intest. Res. 7, 22–31 (2009).
Lewis, J.D. et al. Timing of myelosuppression during thiopurine therapy for inflammatory bowel disease: implications for monitoring recommendations. Clin. Gastroenterol. Hepatol. 7, 1195–1201 (2009).
Fangbin, Z. et al. Should thiopurine methyltransferase genotypes and phenotypes be measured before thiopurine therapy in patients with inflammatory bowel disease? Ther. Drug Monit. 34, 695–701 (2012).
Takagi, Y. et al. Human MTH3 (NUDT18) protein hydrolyzes oxidized forms of guanosine and deoxyguanosine diphosphates: comparison with MTH1 and MTH2. J. Biol. Chem. 287, 21541–21549 (2012).
Price, A.L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909 (2006).
Howie, B.N., Donnelly, P. & Marchini, J. A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 5, e1000529 (2009).
Acknowledgements
We would like to thank all participants who provided the DNA and clinical information necessary for this study. J.L. and W.Z. are supported by the Biomedical Research Council, the Agency for Science, Technology and Research (A*STAR; BMRC SPF2014/001), Singapore. D.P.B.M., T.H. and M.D. are supported by the US National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (P01DK046763, U01DK062413, U01AI067068, R01HS021747), the European Union (IBD-BIOM 305479), the Leona M. and Harry B. Helmsley Charitable Trust (2011PG-MED004, 2014PG-IBD014) and internal funding from the F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute. This work was supported by a Mid-Career Researcher Program grant through NRF (National Research Foundation of Korea) to K.S. (2010-0015648, 2014R1A2A1A09005824) funded by the Ministry of Science, Information and Communication Technology (ICT) and Future Planning and by a Korean Health Technology R&D Project grant to S.-K.Y. (A120176) from the Ministry of Health and Welfare, the Republic of Korea.
Author information
Authors and Affiliations
Contributions
K.S. and S.-K.Y. obtained financial support and conceived and designed the study. K.S. supervised genotyping, data analysis and interpretation, and S.-K.Y. supervised all the sample collection, data analysis and interpretation. J.L. supervised data analysis and interpretation. S.-K.Y., B.D.Y., K.-J.K., S.H.P., S.-K.P., D.-H.Y. and I.L. recruited subjects and participated in diagnostic evaluation. S.-K.Y., S.H.P. and S.-K.P. assessed clinical features. T.H., M.D. and D.P.B.M. supervised the Immunochip genotyping and provided their data. M.H., W.Z., Y.J. and H.C. performed data analyses. M.H., J.B. and H.C. prepared DNA samples and performed genotyping. J.B. performed in vitro transfection experiments and data analysis. K.S. and S.-K.Y. drafted the manuscript. K.S., S.-K.Y., D.P.B.M. and J.L. revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
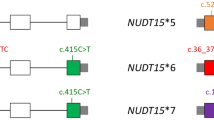
Supplementary Figure 1 Study design.
Leukopenia was classified as 'early' when it occurred within the first 8 weeks of thiopurine therapy and as 'late' when it occurred more than 8 weeks after the start of therapy. The discovery and replication analyses were initially focused on early leukopenia. The SNPs identified from the initial analyses were confirmed in patients with late leukopenia.
Supplementary Figure 2 Quantile-quantile plot for the Immunochip association P values of SNPs in 33 cases and 307 controls.
–log10 P values are plotted against the expected null distribution. Black data points and red data points represent the results of 95,405 genotyped SNPs and 531,416 genotyped + imputed SNPs in the Immunochip set, respectively.
Supplementary Figure 3 Manhattan plot for the discovery Immunochip association analysis in 33 cases and 307 controls.
Data represent the trend test result of 531,416 genotyped + imputed SNPs. –log10 P values are shown according to chromosomal location. SNPs within the SUCLA2-NUDT15-MED4 locus at 13q14 achieve genome-wide significance. The red horizontal line indicates SNPs at a genome-wide significance level (here P = 9.41 × 10–8). The blue horizontal line indicates SNPs with P < 1.0 × 10–5.
Supplementary Figure 4 Regional association plots after conditional analysis of the SUCLA2-NUDT15-MED4 locus at 13q14.
(a,b) Regional association plots after conditional analysis was performed to control for the association at rs116855232 (a) and rs7320366 (b).
Supplementary Figure 5 Receiver operating characteristic curve for an additive prediction model of early leukopenia using NUDT15 SNP rs116855232.
The area under the curve with 95% CI = 0.88–0.97 is 0.92. Overall sensitivity is 89.4%, whereas specificity is 93.2%.
Supplementary Figure 6 Sensitivity of Jurkat cells to 7.5 μM 6-MP following transfection with wild-type or mutant NUDT15.
(a) NUDT15 mRNA levels in Jurkat cells transfected with wild-type or mutant NUDT15, as determined by RT-PCR analysis. (b) The number of viable mutant NUDT15-transfected cells decreases compared to wild type–transfected control cells. (c) Cytotoxicity assay with annexin V and propidium iodide staining showing that cells are more sensitive to 6-MP when they have been transfected with mutant NUDT15, compared to cells transfected with wild-type NUDT15. Data are presented as mean ± s.d. of three independent experiments.
Supplementary Figure 7 Principal-component analysis (PCA).
(a) PCA of 340 samples and 194 reference DNA samples from HapMap. (b) Plots of first eight principal components from the principal-component analysis using 340 samples (33 cases, 307 controls).
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7, Supplementary Tables 1–7 and Supplementary Note. (PDF 3352 kb)
Rights and permissions
About this article
Cite this article
Yang, SK., Hong, M., Baek, J. et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat Genet 46, 1017–1020 (2014). https://doi.org/10.1038/ng.3060
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.3060
This article is cited by
-
Therapeutic drug monitoring in inflammatory bowel disease: A practical approach
Indian Journal of Gastroenterology (2024)
-
Thiopurines exert harmful effects on spermatogenesis in Nudt15R138C knock-in mice
Journal of Gastroenterology (2024)
-
Analysis of the NUDT15 gene and metabolites of azathioprine in Japanese patients with inflammatory bowel disease
BMC Gastroenterology (2023)
-
Mammalian Nudt15 hydrolytic and binding activity on methylated guanosine mononucleotides
European Biophysics Journal (2023)
-
Inflammatory Bowel Disease: Pathophysiology, Treatment, and Disease Modeling
BioChip Journal (2023)