Abstract
Although smoking has been established as the most important cause of lung cancer, approximately 10% of patients with this malignancy have no history of smoking. The pathogenesis of tobacco-related lung carcinogenesis is becoming well characterized, but the molecular mechanisms of neoplastic transformation in never-smokers have not yet been adequately elucidated. Nevertheless, numerous recent studies have revealed a distinct biological process of malignant transformation with unique epidemiological and clinicopathological characteristics in never-smokers. The molecular pathways involved in the differential pattern of lung oncogenesis according to smoking status, however, remain fairly obscure. Researchers have studied several molecular pathways implicated in lung carcinogenesis in smokers and never-smokers, examining these processes at the genomic, epigenetic and proteomic level. The differential protein expression according to smoking status in critical signal transduction pathways has attracted scientific interest because of the possibilities of therapeutic intervention. In this Review we describe the best-characterized signaling pathways implicated in the transduction of proliferative signals and discuss the activity of these pathways in smokers and never-smokers.
Key Points
-
Numerous recent studies have revealed a distinct biological process of malignant transformation with unique epidemiological and clinicopathological characteristics in never-smokers with lung cancer
-
Almost all cases of lung cancer in never-smokers are adenocarcinomas; these tumors tend to be diagnosed at more-advanced stages and are more likely to occur in women than in men compared with tumors in smokers
-
Never-smokers have a higher probability of EGFR mutations in exons 19 and 21 and are more likely to derive clinical benefit from therapy with tyrosine kinase inhibitors than are smokers
-
It is probable that the mitogenic effects of EGFR mutations in never-smokers are mediated via mitogen-activated protein kinase and, in particular, selective activation of p38; the Ras/Raf/mitogen-activated protein kinase pathway might constitute a critical mediator of extracellular signals or growth factors in never-smokers with lung cancer
-
In smokers, tobacco-induced KRAS mutations are responsible for the transduction of proliferative signals to the nucleus, possibly via an EGFR-independent pathway
-
A better comprehension of the distinct biological entities among patients with lung cancer might help identify potential new molecular targets for a more-selective therapeutic strategy
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Thun MJ and Jemal A (2006) How much of the decrease in cancer death rates in the United States is attributable to reductions in tobacco smoking? Tob Control 15: 345–347
Subramanian J and Govindan R (2007) Lung cancer in never smokers: a review. J Clin Oncol 25: 561–570
Jemal A et al. (2007) Cancer statistics, 2007. CA Cancer J Clin 57: 43–66
[No authors listed] (2002) From the Centers for Disease Control and Prevention. State-specific prevalence of current cigarette smoking among adults, and policies and attitudes about secondhand smoke—United States, 2000. JAMA 287: 309–310
Dennis PA et al. (2005) The biology of tobacco and nicotine: bench to bedside. Cancer Epidemiol Biomarkers Prev 14: 764–767
Hecht SS (2003) Tobacco carcinogens, their biomarkers and tobacco-induced cancer. Nat Rev Cancer 3: 733–744
Akopyan G and Bonavida B (2006) Understanding tobacco smoke carcinogen NNK and lung tumorigenesis. Int J Oncol 29: 745–752
Tsurutani J et al. (2005) Tobacco components stimulate Akt-dependent proliferation and NFκB-dependent survival in lung cancer cells. Carcinogenesis 26: 1182–1195
Yang Y et al. (2004) Increased susceptibility of mice lacking Clara cell 10-kDa protein to lung tumorigenesis by 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, a potent carcinogen in cigarette smoke. J Biol Chem 279: 29336–29340
Schuller HM and Cekanova M (2005) NNK-induced hamster lung adenocarcinomas over-express β2-adrenergic and EGFR signaling pathways. Lung Cancer 49: 35–45
Schuller HM et al. (2000) Interaction of tobacco-specific toxicants with the neuronal alpha(7) nicotinic acetylcholine receptor and its associated mitogenic signal transduction pathway: potential role in lung carcinogenesis and pediatric lung disorders. Eur J Pharmacol 393: 265–277
Jin Z et al. (2004) Tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone promotes functional cooperation of Bcl2 and c-Myc through phosphorylation in regulating cell survival and proliferation. J Biol Chem 279: 40209–40219
Xu L and Deng X (2004) Tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone induces phosphorylation of mu- and m-calpain in association with increased secretion, cell migration, and invasion. J Biol Chem 279: 53683–53690
Stringer KA et al. (2004) Particulate phase cigarette smoke increases MnSOD, NQO1, and CINC-1 in rat lungs. Free Radic Biol Med 37: 1527–1533
Shopland DR et al. (1996) Cigarette smoking among U.S. adults by state and region: estimates from the current population survey. J Natl Cancer Inst 88: 1748–1758
Toh CK et al. (2006) Never-smokers with lung cancer: epidemiologic evidence of a distinct disease entity. J Clin Oncol 24: 2245–2251
Keohavong P et al. (1996) Detection of K-ras mutations in lung carcinomas: relationship to prognosis. Clin Cancer Res 2: 411–418
Siegfried JM (2001) Women and lung cancer: does oestrogen play a role? Lancet Oncol 2: 506–513
Ferguson MK et al. (1990) Sex-associated differences in presentation and survival in patients with lung cancer. J Clin Oncol 8: 1402–1407
Zeka A et al. (2006) Lung cancer and occupation in nonsmokers: a multicenter case-control study in Europe. Epidemiology 17: 615–623
Donington JS et al. (2006) Lung cancer in women: exploring sex differences in susceptibility, biology, and therapeutic response. Clin Lung Cancer 8: 22–29
Stabile LP and Siegfried JM (2004) Estrogen receptor pathways in lung cancer. Curr Oncol Rep 6: 259–267
Gills JJ et al. (2004) Targeting aberrant signal transduction pathways in lung cancer. Cancer Biol Ther 3: 147–155
Bain C et al. (2004) Lung cancer rates in men and women with comparable histories of smoking. J Natl Cancer Inst 96: 826–834
Franklin WA et al. (2002) Epidermal growth factor receptor family in lung cancer and premalignancy. Semin Oncol 29 (Suppl 4): S3–S14
Shigematsu H et al. (2005) Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst 97: 339–346
Lynch TJ et al. (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350: 2129–2139
Paez JG et al. (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304: 1497–1500
Shepherd FA et al. (2005) Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 353: 123–132
Tsao MS et al. (2005) Erlotinib in lung cancer—molecular and clinical predictors of outcome. N Engl J Med 353: 133–144
Thatcher N et al. (2005) Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet 366: 1527–1537
Hirsch FR et al. (2006) Molecular predictors of outcome with gefitinib in a phase III placebo-controlled study in advanced non-small-cell lung cancer. J Clin Oncol 24: 5034–5042
Engelman JA et al. (2007) MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316: 1039–1043
Pham D et al. (2006) Use of cigarette-smoking history to estimate the likelihood of mutations in epidermal growth factor receptor gene exons 19 and 21 in lung adenocarcinomas. J Clin Oncol 24: 1700–1704
Tang X et al. (2005) EGFR tyrosine kinase domain mutations are detected in histologically normal respiratory epithelium in lung cancer patients. Cancer Res 65: 7568–7572
Shigematsu H et al. (2005) Somatic mutations of the HER2 kinase domain in lung adenocarcinomas. Cancer Res 65: 1642–1646
Stephens P et al. (2004) Lung cancer: intragenic ERBB2 kinase mutations in tumours. Nature 431: 525–526
Papadimitrakopoulou V and Adjei AA (2006) The Akt/mTOR and mitogen-activated protein kinase pathways in lung cancer therapy. J Thorac Oncol 1: 749–751
Adjei AA and Hidalgo M (2005) Intracellular signal transduction pathway proteins as targets for cancer therapy. J Clin Oncol 23: 5386–5403
Sato M et al. (2007) A translational view of the molecular pathogenesis of lung cancer. J Thorac Oncol 2: 327–343
Downward J (2003) Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer 3: 11–22
Eberhard DA et al. (2005) Mutations in the epidermal growth factor receptor and in KRAS are predictive and prognostic indicators in patients with non-small-cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J Clin Oncol 23: 5900–5909
Ahrendt SA et al. (2001) Cigarette smoking is strongly associated with mutation of the K-ras gene in patients with primary adenocarcinoma of the lung. Cancer 92: 1525–1530
Brose MS et al. (2002) BRAF and RAS mutations in human lung cancer and melanoma. Cancer Res 62: 6997–7000
Erman M et al. (2005) Epidermal growth factor receptor, HER-2/neu and related pathways in lung adenocarcinomas with bronchioloalveolar features. Lung Cancer 47: 315–323
Vicent S et al. (2004) ERK1/2 is activated in non-small-cell lung cancer and associated with advanced tumours. Br J Cancer 90: 1047–1052
Heusch WL and Maneckjee R (1998) Signalling pathways involved in nicotine regulation of apoptosis of human lung cancer cells. Carcinogenesis 19: 551–556
Kuo WH et al. (2005) Induction of apoptosis in the lung tissue from rats exposed to cigarette smoke involves p38/JNK MAPK pathway. Chem Biol Interact 155: 31–42
Mazieres J et al. (2005) Wnt signaling in lung cancer. Cancer Lett 222: 1–10
Vicent S et al. (2004) Mitogen-activated protein kinase phosphatase-1 is overexpressed in non-small cell lung cancer and is an independent predictor of outcome in patients. Clin Cancer Res 10: 3639–3649
Greenberg AK et al. (2002) Selective p38 activation in human non-small cell lung cancer. Am J Respir Cell Mol Biol 26: 558–564
Tsai JR et al. (2006) Mitogen-activated protein kinase pathway was significantly activated in human bronchial epithelial cells by nicotine. DNA Cell Biol 25: 312–322
Olson JM and Hallahan AR (2004) P38 MAP kinase: a convergence point in cancer therapy Trends Mol Med 10: 125–129
Shin I et al. (2005) H-Ras-specific activation of Rac-MKK3/6-p38 pathway: its critical role in invasion and migration of breast epithelial cells. J Biol Chem 280: 14675–14683
Bradham C and McClay DR (2006) p38 MAPK in development and cancer. Cell Cycle 5: 824–828
Turkson J et al. (1999) Requirement for Ras/Rac1-mediated p38 and c-Jun N-terminal kinase signaling in Stat3 transcriptional activity induced by the Src oncoprotein. Mol Cell Biol 19: 7519–7528
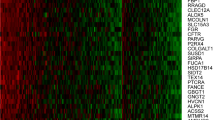
Mountzios G et al.: Mitogen-activated protein kinase activation in lung adenocarcinoma: a comparative study between ever smokers and never smokers. Clin Cancer Res, (in press)
Schmelzle T and Hall MN (2000) TOR, a central controller of cell growth. Cell 103: 253–262
Baselga J and Arribas J (2004) Treating cancer's kinase 'addiction'. Nat Med 10: 786–787
Brognard J et al. (2001) Akt/protein kinase B is constitutively active in non-small cell lung cancer cells and promotes cellular survival and resistance to chemotherapy and radiation. Cancer Res 61: 3986–3997
Moore SM et al. (1998) The presence of a constitutively active phosphoinositide 3-kinase in small cell lung cancer cells mediates anchorage-independent proliferation via a protein kinase B and p70s6k-dependent pathway. Cancer Res 58: 5239–5247
Mukohara T et al. (2003) Expression of epidermal growth factor receptor (EGFR) and downstream-activated peptides in surgically excised non-small-cell lung cancer (NSCLC). Lung Cancer 41: 123–130
Blackhall FH et al. (2003) Expression and prognostic significance of kit, protein kinase B, and mitogen-activated protein kinase in patients with small cell lung cancer. Clin Cancer Res 9: 2241–2247
David O et al. (2004) Phospho-Akt overexpression in non-small cell lung cancer confers significant stage-independent survival disadvantage. Clin Cancer Res 10: 6865–6871
Cappuzzo F et al. (2005) Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer Inst 97: 643–655
Shah A et al. (2005) Phospho-akt expression is associated with a favorable outcome in non-small cell lung cancer. Clin Cancer Res 11: 2930–2936
Tang JM et al. (2006) Phosphorylated Akt overexpression and loss of PTEN expression in non-small cell lung cancer confers poor prognosis. Lung Cancer 51: 181–191
Tsurutani J et al. (2005) Tobacco components stimulate Akt-dependent proliferation and NFκB-dependent survival in lung cancer cells. Carcinogenesis 26: 1182–1195
West KA et al. (2003) Rapid Akt activation by nicotine and a tobacco carcinogen modulates the phenotype of normal human airway epithelial cells. J Clin Invest 111: 81–90
Lim WT et al. (2007) PTEN and phosphorylated AKT expression and prognosis in early- and late-stage non-small cell lung cancer. Oncol Rep 17: 853–857
Dutu T et al. (2005) Differential expression of biomarkers in lung adenocarcinoma: a comparative study between smokers and never-smokers. Ann Oncol 16: 1906–1914
Yu H and Jove R (2004) The STATs of cancer—new molecular targets come of age. Nat Rev Cancer 4: 97–105
Buettner R et al. (2002) Activated STAT signaling in human tumors provides novel molecular targets for therapeutic intervention. Clin Cancer Res 8: 945–954
Alvarez JV et al. (2006) Signal transducer and activator of transcription 3 is required for the oncogenic effects of non-small-cell lung cancer-associated mutations of the epidermal growth factor receptor. Cancer Res 66: 3162–3168
Akca H et al. (2006) Activation of the AKT and STAT3 pathways and prolonged survival by a mutant EGFR in human lung cancer cells. Lung Cancer 54: 25–33
Haura EB et al. (2005) Activated epidermal growth factor receptor-Stat-3 signaling promotes tumor survival in vivo in non-small cell lung cancer. Clin Cancer Res 11: 8288–8294
Wright JG and Christman JW (2003) The role of nuclear factor kappa B in the pathogenesis of pulmonary diseases: implications for therapy. Am J Respir Med 2: 211–219
Lemjabbar H et al. (2003) Tobacco smoke-induced lung cell proliferation mediated by tumor necrosis factor alpha-converting enzyme and amphiregulin. J Biol Chem 278: 26202–26207
Yang P et al. (2004) Glutathione pathway genes and lung cancer risk in young and old populations. Carcinogenesis 25: 1935–1944
Han CH et al. (2006) Clinical significance of insulin receptor substrate-I down-regulation in non-small cell lung cancer. Oncol Rep 16: 1205–1210
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Mountzios, G., Fouret, P. & Soria, JC. Mechanisms of Disease: signal transduction in lung carcinogenesis—a comparison of smokers and never-smokers. Nat Rev Clin Oncol 5, 610–618 (2008). https://doi.org/10.1038/ncponc1181
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncponc1181
This article is cited by
-
Imperatorin sensitizes anoikis and inhibits anchorage-independent growth of lung cancer cells
Journal of Natural Medicines (2013)
-
Vacuolated cell pattern of pancreatobiliary adenocarcinoma: a clinicopathological analysis of 24 cases of a poorly recognized distinctive morphologic variant important in the differential diagnosis
Virchows Archiv (2010)
-
Hallmarks for senescence in carcinogenesis: novel signaling players
Apoptosis (2009)