Abstract
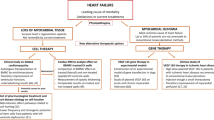
Background Studies of the transplantation of autologous bone marrow cells (BMCs) in patients with chronic ischemic heart disease have assessed effects on viable, peri-infarct tissue. We conducted a single-blinded, randomized, controlled study to investigate whether intramuscular or intracoronary administration of BMCs into nonviable scarred myocardium during CABG improves contractile function of scar segments compared with CABG alone.
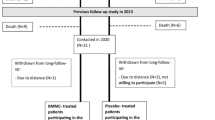
Methods Elective CABG patients (n = 63), with established myocardial scars diagnosed as akinetic or dyskinetic segments by dobutamine stress echocardiography and confirmed at surgery, were randomly assigned CABG alone (control) or CABG with intramuscular or intracoronary administration of BMCs. The BMCs, which were obtained at the time of surgery, were injected into the mid-depth of the scar in the intramuscular group or via the graft conduit supplying the scar in the intracoronary group. Contractile function was assessed in scar segments by dobutamine stress echocardiography before and 6 months after treatment.
Results The proportion of patients showing improved wall motion in at least one scar segment after BMC treatment was not different to that observed in the control group (P = 0.092). Quantitatively, systolic fractional thickening in scar segments did not improve with BMC administration. Furthermore, BMCs did not improve scar transmurality, infarct volume, left ventricular volume, or ejection fraction.
Conclusion Injection of autologous BMCs directly into the scar or into the artery supplying the scar is safe but does not improve contractility of nonviable scarred myocardium, reduce scar size, or improve left ventricular function more than CABG alone.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Tomita S et al. (1999) Autologous transplantation of bone marrow cells improves damaged heart function. Circulation 100: II247–II256
Orlic D et al. (2001) Bone marrow cells regenerate infarcted myocardium. Nature 410: 701–705
Patel AN et al. (2005) Surgical treatment for congestive heart failure with autologous adult stem cell transplantation: a prospective randomized study. J Thorac Cardiovasc Surg 130: 1631–1638
Hendrikx M et al. (2006) Recovery of regional but not global contractile function by the direct intramyocardial autologous bone marrow transplantation: results from a randomized controlled clinical trial. Circulation 114: I101–107
Stamm C et al. (2007) Intramyocardial delivery of CD133+ bone marrow cells and coronary artery bypass grafting for chronic ischemic heart disease: safety and efficacy studies. J Thorac Cardiovasc Surg 133: 717–725
Galiñanes M et al. (2004) Autotransplantation of unmanipulated bone marrow into scarred myocardium is safe and enhances cardiac function in humans. Cell Transplant 13: 7–13
Nagueh SF et al. (1999) Relation of the contractile reserve of hibernating myocardium to myocardial structure in humans. Circulation 100: 490–496
Kim RJ et al. (1999) Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 100: 1992–2002
Grothues F et al. (2002) Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol 90: 29–34
Zhang H et al. (2007) Injection of bone marrow mesenchymal stem cells in the borderline area of infarcted myocardium: heart status and cell distribution. J Thorac Cardiovasc Surg 134: 1234–1240
Schiller NB et al. (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2: 358–367
Hoffmann R et al. (1996) Analysis of interinstitutional observer agreement in interpretation of dobutamine stress echocardiograms. J Am Coll Cardiol 27: 330–336
Hoffmann R et al. (2002) Refinements in stress echocardiographic techniques improve inter-institutional agreement in interpretation of dobutamine stress echocardiograms. Eur Heart J 23: 821–829
MASS analysis (Medis, Leiden, Netherlands)
Guyatt GH et al. (1987) A controlled trial of ambroxol in chronic bronchitis. Chest 92: 618–620
SPSS version 14® (SPSS Inc., Chicago, IL, USA
SAS version 9.1 (SAS® Institute Inc., Cary, IN, USA)
Seeger FH et al. (2007) Cell isolation procedures matter: a comparison of different isolation protocols of bone marrow mononuclear cells used for cell therapy in patients with acute myocardial infarction. Eur Heart J 28: 766–772
Shi Q et al. (1998) Evidence for circulating bone marrow-derived endothelial cells. Blood 92: 362–367
Quirici N et al. (2001) Differentiation and expansion of endothelial cells from human bone marrow CD133+ cells. Br J Haematol 115: 186–194
Asahara T et al. (1999) Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 85: 221–228
Balsam LB et al. (2004) Haematopoietic stem cells adopt mature haematopoietic fates in ischaemic myocardium. Nature 428: 668–673
Murry CE et al. (2004) Haematopoietic stem cells do not transdifferentiate into cardiac myocytes in myocardial infarcts. Nature 428: 664–668
Kocher AA et al. (2001) Neovascularization of ischemic myocardium by human bone-marrow-derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Nat Med 7: 430–436
Schuster MD et al. (2004) Myocardial neovascularization by bone marrow angioblasts results in cardiomyocyte regeneration. Am J Physiol Heart Circ Physiol 287: H525–H532
Ziegelhoeffer T et al. (2004) Bone marrow-derived cells do not incorporate into the adult growing vasculature. Circ Res 94: 230–238
Fukushima S et al. (2007) Direct intramyocardial but not intracoronary injection of bone marrow cells induces ventricular arrhythmias in a rat chronic ischemic heart failure model. Circulation 115: 2254–2261
Menasche P et al. (2008) The Myoblast Autologous Grafting in Ischemic Cardiomyopathy (MAGIC) trial: first randomized placebo-controlled study of myoblast transplantation. Circulation 117: 1189–1200
Hamano K et al. (2001) Local implantation of autologous bone marrow cells for therapeutic angiogenesis in patients with ischemic heart disease: clinical trial and preliminary results. Jpn Circ J 65: 845–847
Strauer BE et al. (2002) Repair of infarcted myocardium by autologous intracoronary mononuclear bone marrow cell transplantation in humans. Circulation 106: 1913–1918
Perin EC et al. (2003) Transendocardial, autologous bone marrow cell transplantation for severe, chronic ischemic heart failure. Circulation 107: 2294–2302
Assmus B et al. (2002) Transplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI). Circulation 106: 3009–3017
Menasche P et al. (2003) Autologous skeletal myoblast transplantation for severe postinfarction left ventricular dysfunction. J Am Coll Cardiol 41: 1078–1083
Acknowledgements
We thank W Rathbone and E McGlynn for their technical assistance and N Harris, A Vickers, L Middleton and S Garbett for their help. We also thank A Mathur for his valuable comments. This study was funded by the British Heart Foundation (grant PG04050).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Ang, KL., Chin, D., Leyva, F. et al. Randomized, controlled trial of intramuscular or intracoronary injection of autologous bone marrow cells into scarred myocardium during CABG versus CABG alone. Nat Rev Cardiol 5, 663–670 (2008). https://doi.org/10.1038/ncpcardio1321
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1321
This article is cited by
-
Autologous bone marrow stem cell transplantation for patients undergoing coronary artery bypass grafting: a meta-analysis of 22 randomized controlled trials
Journal of Cardiothoracic Surgery (2022)
-
Impact of Diabetes Mellitus on the Potential of Autologous Stem Cells and Stem Cell–Derived Microvesicles to Repair the Ischemic Heart
Cardiovascular Drugs and Therapy (2022)
-
Key Success Factors for Regenerative Medicine in Acquired Heart Diseases
Stem Cell Reviews and Reports (2020)
-
Intramyocardial bone marrow cell injection does not lead to functional improvement in patients with chronic ischaemic heart failure without considerable ischaemia
Netherlands Heart Journal (2019)
-
Cell therapy trials for heart regeneration — lessons learned and future directions
Nature Reviews Cardiology (2018)