Abstract
Brain iron elevation is implicated in Alzheimer’s disease (AD) pathogenesis, but the impact of iron on disease outcomes has not been previously explored in a longitudinal study. Ferritin is the major iron storage protein of the body; by using cerebrospinal fluid (CSF) levels of ferritin as an index, we explored whether brain iron status impacts longitudinal outcomes in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) cohort. We show that baseline CSF ferritin levels were negatively associated with cognitive performance over 7 years in 91 cognitively normal, 144 mild cognitive impairment (MCI) and 67 AD subjects, and predicted MCI conversion to AD. Ferritin was strongly associated with CSF apolipoprotein E levels and was elevated by the Alzheimer’s risk allele, APOE-ɛ4. These findings reveal that elevated brain iron adversely impacts on AD progression, and introduce brain iron elevation as a possible mechanism for APOE-ɛ4 being the major genetic risk factor for AD.
Similar content being viewed by others
Introduction
Cortical iron elevation is increasingly reported as a feature of Alzheimer’s disease (AD)1, and might contribute to the oxidative damage observed in AD brains2. A single-blind, 2-year trial of 48 AD patients with the iron chelator, deferoxamine, reported decreased cognitive decline3, but this has not been followed up. While evidence in animal models argue in favour of brain iron accumulation propelling atrophy and dementia4, prospective evidence about the link between brain iron status and clinical outcomes in AD is lacking.
CSF ferritin could be an index of brain iron load. Ferritin is the iron storage protein of the body and is elevated in AD brain tissue5,6,7,8. In cultured systems, ferritin expression9,10 and secretion11 by glia is dependent on cellular iron levels. Ferritin levels in CSF likely reflect iron levels in the brain and can have clinical utility. For example, in Restless Legs Syndrome, a disorder of low brain iron that is treated with iron supplementation, CSF ferritin levels are decreased12. CSF ferritin was reported to be elevated in AD in one study13, but this was not repeated in subsequent studies using larger clinical cohorts14,15.
Here, we examined the association of baseline CSF-ferritin data with biomarker, cognitive, anatomical and diagnostic outcomes over 7 years in the Alzheimer’s disease Neuroimaging Initiative (ADNI) prospective clinical cohort. We show that CSF ferritin levels have similar utility compared with more established AD CSF biomarkers, the tau/Aβ1–42 ratio and apolipoprotein E (ApoE) levels, in predicting various outcomes of AD. However, the nature of the relationship between CSF ferritin levels and cognitive performance was different from the other biomarkers, and, in contrast, CSF ferritin appears as a trait variable, and not a marker of disease.
Results
The relationship between CSF ferritin and biomarkers of AD
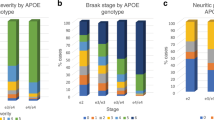
In agreement with other reports14,15, CSF ferritin levels were not different between cognitively normal (CN; n=91), mild cognitive impairment (MCI; n=144) and AD (n=67) subjects (ANCOVA: P=0.591; Table 1) in the ADNI cohort. Neither were there changes in ferritin levels when we separated the cohort according to CSF Aβ1–42 levels (192 ng l−1 cutoff; as proposed previously16) to reflect likely cerebral amyloid burden (ANCOVA: P=0.946; Supplementary Fig. 1). But in multiple regression modelling of ferritin including the established CSF biomarkers of AD17 (tau, p-tau, Aβ1–42), CSF ferritin levels were predicted by Aβ1–42 (partial R2=0.013, P=0.029) and tau (partial R2=0.086, P<0.001; model 1, Supplementary Table 1), although not by p-tau. Since the apolipoprotein E gene (APOE) alleles are the major genetic risk for AD18 and CSF apolipoprotein E protein (ApoE) levels are associated with Aβ1-42 (refs 19, 20) and tau20,21, we re-built the model to include CSF ApoE levels. This abolished the relationship between ferritin and the other biomarkers (Aβ1–42: R2<0.001, P=0.904; tau: R2=0.003, P=0.219; model 2, Supplementary Table 1). This led us to detect a surprisingly strong relationship between ApoE and ferritin (linear term partial R2=0.243, P=7.69 × 10−22), which was improved when Aβ1–42 and tau (non-significant terms) were removed from the model (linear term partial R2=0.341, P=1.52 × 10−29; model 3, Supplementary Table 1, Fig. 1a).
(a,b) Modelling ferritin in CSF (refer to, M3 of Supplementary Table 1). Minimal multiple regression contained CSF ApoE and APOE ɛ4. (a) Scatterplot of CSF ApoE and ferritin levels in APOE ɛ4 carriers and non-ɛ4 carriers. The genotype did not affect the relationship between ApoE and ferritin; however, genotype is associated with CSF ferritin levels, and thus ɛ4 carriers and non-ɛ4 carriers are plotted separately. The R2 for the linear component of the full model was 0.341 (displayed on graph). (b) CSF Ferritin levels in APOE ɛ4 carriers and non-carriers (ANCOVA: P-value=1.10 × 10−8). (c) Multiple regression of CSF ApoE. ApoE levels in APOE ɛ4 carriers and non-carriers (ANCOVA: P=2.50 × 10−9). Data are means+s.e. ‘n’ is represented in graph columns.
In model 3, APOE genotype strongly influenced CSF ferritin (P=1.10 × 10−8), with the major AD risk allele, ɛ4, inducing 22% higher levels than non-ɛ4 carriers (Fig. 1b). Reciprocally, in multiple regression modelling of CSF ApoE, APOE ɛ4-positive subjects had lower ApoE levels (-16%; P=2.50 × 10−9) compared with non-ɛ4 carriers (Fig. 1c). Plasma ferritin levels were not associated with plasma ApoE levels or APOE ɛ4 allele status (Supplementary Fig. 2), but there was a modest association between plasma ferritin and CSF ferritin levels (β=0.075, P=0.0002; Supplementary Fig. 3).
Association of ferritin with neuropsychiatric assessments
Next, we explored whether CSF ferritin was related to cognitive performance in AD. Baseline ADAS-Cog13 (The Alzheimer's Disease Assessment Scale) score was associated with CSF ferritin (P=0.006; Table 2), ApoE levels (P=0.0003) and tau/Aβ1–42 ratio (P=0.025), independently, in a multiple regression model containing the AD biomarkers and other clinical variables. In tertile analysis, high (>7.2 ng ml−1), compared with low (<5.4 ng ml−1), levels of ferritin were associated with an ≈3 point poorer ADAS-cog13 score (Fig. 2a). Similarly, in tertiles, lower levels of ApoE (Fig. 2b) were associated with a ≈4 point worse ADAS-Cog13, and higher tau/Aβ1-42 ratio was associated with a ≈2 point worse ADAS-Cog13 (Fig. 2c), as previously reported21,22.
(a–c) Multiple regression of baseline ADAS-Cog13 score expressed as tertiles of CSF (a) ferritin (L<5.5; H>7.3 ng ml−1), (b) ApoE (L< 5.8; H>7.8 μg ml−1) and (c) tau/Aβ1–42 (L<0.35; H>0.76). (d) Multiple regression of baseline RAVLT score expressed as CSF ferritin tertiles. Data are adjusted for baseline diagnosis, gender, years of education and the AD CSF biomarkers in the minimal models. Data are means+s.e. ‘n’ is shown in graph columns. CN, cognitively normal; MCI, mild cognitive impairment.
To determine whether baseline values of CSF ferritin predict longitudinal cognitive outcome, we constructed a mixed effects model of annual ADAS-Cog13 scores over 7 years (Table 2 for statistics, Supplementary Table 2 for patient numbers) and observed that both ApoE (P=0.006) and tau/Aβ1-42 ratio (P=2.70 × 10−7) were still associated with rate of cognitive change (interacted with time), as previously reported21,22. Ferritin, however, impacted on ADAS-Cog13 by a constant cross-sectional decrement (P=4.93 × 10−4 main effect only; Table 2).
We additionally modelled cognition using the Rey verbal learning test (RAVLT), which is more sensitive in distinguishing control and MCI patients23. In this model, only ferritin levels were associated with cross-sectional cognitive performance (P=0.0017; Table 2, Fig. 2d), but CSF ferritin was not associated with rate of deterioration in a longitudinal model (P=0.817; Table 2). Baseline tau/Aβ1–42 ratio was associated with rate of cognitive decline on RAVLT (P=4.8510 × 10−5), but there was only a trend for ApoE (P=0.066). Hence, in both cognitive scales, CSF ferritin impacted on performance by a constant amount, regardless of disease status, thus appearing as a trait variable and not a marker of disease.
We reasoned that if high ferritin levels worsened the cognitive performance by a constant value over time, then MCI individuals with high ferritin levels would satisfy the criteria for an AD diagnosis at a comparatively earlier interval. To investigate this, we employed a Cox proportional hazards model on 144 MCI subjects who had CSF ferritin, ApoE and tau/Aβ1-42 measurements. In a minimal model (containing only these CSF biomarkers; Table 2) of MCI conversion over 7 years, ferritin (P=0.03; Fig. 3a), ApoE (P=0.008; Supplementary Fig. 4a) and tau/Aβ1–42 (P=0.037; Supplementary Fig. 4b) were each significant predictive variables.
(a) MCI survival based on the minimal Cox proportional hazards model (Table 2), the conversion is plotted for each quintile of ferritin (applying mean values for the cohort: ApoE=7.2 μg ml−1, tau/Aβ1–42=0.69 units). The numbers on the right side of the graphs indicate the quintile boundaries. This minimal model contained only the CSF biomarkers. (b) Change in mean age of diagnosis according to CSF biomarkers. The months taken for ∼50% survival of each quintile boundary in the Cox models were graphed against the unit values of those boundaries. The gradient of the linear model was used to estimate change in age of conversion for each unit change in analyte. (refer to Fig. 3a, Supplementary Fig. 4). (c–e) Receiver operating curves of logistic regression modelling of MCI conversion to AD (refer to Table 2, Supplementary Fig. 5). (c) Base model controlling for age, gender, BMI, years of education and APOE ɛ4 status. (d) Base model plus ApoE and tau/Aβ1-42. (e) Base model plus ApoE, tau/Aβ1–42 and ferritin. AUC, area under curve.
Using this model we estimated how many months was required for 50% survivorship for each quintile of each biomarker. We then constructed a linear model of these values (in months; y-axis) against the values for the quintile boundaries of each analyte (in designated units; x-axis). The gradient of these functions estimates the change in mean age of conversion (in months) associated with one unit change in the baseline CSF analyte. For comparison between biomarkers, we also expressed the change in mean age of conversion associated with a s.d. change to the analyte value. One s.d. change to ferritin was associated with a 9.5-month shift in age of conversion, compared with 18.2 and 8.6 months for ApoE and tau/Aβ1–42, respectively (Fig. 3b).
In separate adjusted logistic regression models, an increase in the baseline concentration of each biomarker by its interquartile range increased the odds of converting to AD for ferritin (OR: 1.36, 95%CI: 1.17–1.58) and tau/Aβ1–42 ratio (OR: 1.13, CI: 0.95–1.35), and decreased the odds for ApoE (OR: 0.72, CI: 0.61–0.85). Including all three analytes into the one model increased the predictive value of each analyte (OR (CI): ferritin=2.32 (1.86–2.9], tau/Aβ1–42=1.45[1.16–1.8], ApoE=0.38[0.3–0.48]; Table 2).
Receiver-operating curves based on the logistic regression models determined the accuracy of these analytes to predict conversion to AD. The area under the curve (AUC) of the base model (age, gender, years of education, BMI, APOE ɛ4 genotype) was 0.6079 (Fig. 3c), which was increased by the singular inclusions of either ferritin (AUC: 0.6321; Supplementary Fig. 5b), ApoE (0.6311; Supplementary Fig. 5c) or marginally by tau/Aβ1–42 (0.6177; Supplementary Fig. 5d). When the tau/Aβ1–42 was included in the model containing ApoE, the AUC increased slightly (from 0.6311 to 0.6483; Fig. 3d). This performance, which combined the established CSF biomarkers for AD, was improved markedly by adding ferritin values (from 0.6483 to 0.6937 Fig. 3e).
Association of ferritin with brain atrophy
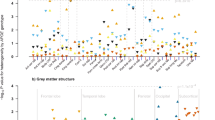
Finally, we investigated whether ferritin levels associate with neuroanatomical changes to the hippocampus and lateral ventricular area in yearly intervals over a 6-year period for CN and MCI subjects (Supplementary Table 3 for patient numbers). We explored the impact of CSF ferritin when the other biomarkers were also included in modelling, whereas CSF ferritin has previously been shown to predict atrophy of various brain structures when considered in isolation24. Baseline ApoE, ferritin and tau/Aβ1–42 values each independently predicted hippocampal volume in an adjusted longitudinal model (Table 2). The rate of atrophy of the hippocampus was greater in individuals with high CSF ferritin (P=0.02; Fig. 4a). Low CSF ApoE (P=0.008; Fig. 4b) or high tau/Aβ1–42 (P=6.80 × 10−6; Fig. 4c) also predicted atrophy, as previous reported21,25. Lateral ventricular enlargement over time was similarly associated independently with high-CSF ferritin (P=0.008; Fig. 4d), low-CSF ApoE (P=0.0002; Fig. 4e), or high tau/Aβ1–42 (P=4.19 × 10−8; Fig. 4f).
(a–c) Longitudinal hippocampal changes based on tertiles of CSF (a) ferritin (L<5.5; H>7.3 ng ml−1) (b) ApoE (L< 5.8; H>7.8 μg ml−1) and (c) tau/Aβ1–42 (L<0.35; H>0.76) tertiles (refer to Table 2). (d–f) Longitudinal lateral ventricular changes based on CSF (d) ferritin (e) ApoE and (f) tau/Aβ1–42 tertiles (refer to Table 2). These mixed effects models were adjusted for age, gender, baseline diagnosis, years of education, APOE ɛ4 status and intracranial volume. Tertiles at baseline were not significantly different for all models, therefore for visual display the baseline values were held at the adjusted means for each diagnostic group. CN, cognitively normal; H, highest tertile; M, middle tertile; MCI, mild cognitive impairment; L, lowest tertile.
Discussion
Our analyses show that CSF ferritin levels were independently related to cognitive performance in the ADNI cohort and predicted MCI conversion to AD. The magnitude impact of ferritin on these outcomes was comparable to the established biomarkers, ApoE and tau/Aβ1–42; however, the nature of the effect of ferritin was not the same. Ferritin was associated with constant shift in cognitive performance over the study period (Fig. 5a), whereas the decrements associated with the other biomarkers were exaggerated over time (Fig. 5b). A downward shift (poorer cognitive presentation) in response to high ferritin levels (1.77 RAVLT points per 1 ng ml−1 ferritin; Table 2) results in an earlier age of diagnosis (3 months per 1 ngng ml−1 ferritin; Fig. 3b). This would be consistent with findings that patients with an early age of AD onset have greater neocortical iron burden than late-onset patients1,7. Collectively these data support consideration of therapeutic strategies that lower brain iron, which have reported beneficial outcomes in Phase II trials of Alzheimer’s3 and Parkinson’s26 diseases. Lowering CSF ferritin, as might be expected from a drug like deferiprone26, could conceivably delay MCI conversion to AD by as much as 3 years.
(a) CSF ferritin has a qualitatively different impact to (b) CSF tau/Aβ1–42 and ApoE on cognitive performance over time in cognitively normal (dotted lines) and in subjects who develop AD (solid lines). Higher CSF ferritin levels are associated with poorer baseline cognitive status (for example, RAVLT) by [α] points, where [α]=Ln[ferritin (ng ml−1)]*1·77 (refer to Table 2). This effect is constant over time, such that [α]=[β,χ]. Consequently, ferritin causes a shift to the left in age of conversion to AD by [δ] months, where [δ]=ferritin (ng ml−1)*3 (refer to Fig. 3b). Levels of tau/Aβ1–42 or ApoE are associated with both baseline cognitive status [ɛ] and the rate of cognitive deterioration, such that [ɛ]<[φ,γ]. The effect causes a shift in age of diagnosis by [η] months where [η]=ApoE (μg ml−1)*8 or tau/Aβ1–42 (units)*17 (refer to Fig. 3b).
An unresolved question arising from this study is why are CSF ferritin levels not elevated in AD, where brain iron levels are reported as elevated2? We hypothesize that ferritin levels in the CSF reflect global brain iron burden, whereas iron elevation in AD has only been reported in affected regions (for example, frontal cortical tissue27). Possibly, iron elevation in brain regions affected by AD is too confined regionally to be reflected in CSF. An altered relationship between tissue and CSF ferritin in AD, however, cannot yet be excluded.
Our data also provide exploratory insights into iron in AD aetiopathogenesis, identifying an unexpected interaction of ApoE with ferritin. That ferritin levels are increased by the APOE-ɛ4 allele argues that ApoE influences ferritin levels, rather than the reverse. Our current findings indicate that APOE genotype should influence constitutive brain iron burden. However, to our knowledge, a post mortem study of iron or ferritin in brain tissue, stratified according to APOE genotype, has not been reported. Focal changes to iron and ferritin have been observed in AD brains post mortem1,2,5,6,7,8, and on the basis of our findings we propose that the ɛ4 genotype raises the baseline iron load of the brain, thus lowering the threshold for iron-mediated neuronal loss in disease. This proposal awaits experimental confirmation, but it is possible that increased plaque pathology associated with the APOE ɛ4 isoform28 might be a consequence of interactions between Aβ and iron29, leading to oxidative stress and Aβ aggregation12,13. Elevated iron could likewise contribute to tau pathology by causing its aggregation30, indeed iron is co-localized in neurofibrillary tangles in AD, and such co-localization is also observed in a primary disease of brain iron overload, neurodegeneration with brain iron accumulation2,31. Superficial CNS siderosis is also characterized by brain iron deposition, and tau is elevated in the CSF in this condition32. A relationship between brain iron and tau is supported by the results in our study, where CSF ferritin levels correlated with tau levels (Model 1 of Supplementary Table 1; when ApoE is excluded from the analysis).
How, then, could ApoE impact on brain iron homeostasis? To our knowledge, no previous study has directly explored this, but synaptic zinc was reported to be lowered in APOE KO mice,33 and in a closed head injury model, iron accumulation was shown to be exaggerated in APOE-KO mice34. The mechanism for ApoE in iron regulation could involve the trafficking of lipoproteins by ApoE. Treatment of macrophages with high-density lipoprotein (HDL; the lipoprotein of CSF) has been shown to lower intracellular iron levels and to promote ferritin release35. APOE ɛ4 carriers have less CSF ApoE, and the ɛ4 isoform has comparatively lower affinity for HDL36, so reduced delivery of HDL in APOE ɛ4 carriers could result in iron retention in the brain. Notably, the iron accumulation mutation of HFE (associated with hemochromatosis) has an epistatic interaction with APOE ɛ4 to increase AD risk and accelerates disease onset by 5.5 years (reviewed in ref. 37). We therefore introduce the concept that APOE ɛ4 status confers susceptibility to AD by increasing ferritin levels. The association between ApoE and brain iron status will warrant further investigation.
Methods
ADNI description
Data used in the preparation of this article were downloaded on 15 July 2014 from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). The ADNI study has been previously described in detail38. The ADNI was launched in 2003 by the National Institute on Aging (NIA), the National Institute of Biomedical Imaging and Bioengineering (NIBIB), the Food and Drug Administration (FDA), private pharmaceutical companies and non-profit organizations, as a $60 million, five-year public-private partnership. The primary goal of ADNI has been to test whether serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of mild cognitive impairment (MCI) and early Alzheimer’s disease (AD). Determination of sensitive and specific markers of very early AD progression is intended to aid researchers and clinicians to develop new treatments and monitor their effectiveness, as well as lessen the time and cost of clinical trials.
The principal investigator of this initiative is Michael W. Weiner, MD, VA Medical Center and University of California, San Francisco. ADNI is the result of efforts of many co-investigators from a broad range of academic institutions and private corporations, and subjects have been recruited from over 50 sites across the United States and Canada. The initial goal of ADNI was to recruit 800 subjects but ADNI has been followed by ADNI-GO and ADNI-2. To date these three protocols have recruited over 1,500 adults, ages 55 to 90, to participate in the research, consisting of cognitively normal older individuals, people with early or late MCI, and people with early AD. The follow-up duration of each group is specified in the protocols for ADNI-1, ADNI-2 and ADNI-GO. Subjects originally recruited for ADNI-1 and ADNI-GO had the option to be followed in ADNI-2. For up-to-date information, see www.adni-info.org.
Recruitment inclusion and exclusion criteria for ADNI 1
Inclusion criteria were as follows: (1) Hachinski Ischaemic Score ≤4; (2) permitted medications stable for 4 weeks before screening; (3) Geriatric Depression Scale score<6; (4) visual and auditory acuity adequate for neuropsychological testing; good general health with no diseases precluding enrolment; (5) six grades of education or work history equivalent; (6) ability to speak English or Spanish fluently; (7) a study partner with 10 h per week of contact either in person or on the telephone who could accompany the participant to the clinic visits.
Criteria for the different diagnostic groups are summarized in Supplementary Table 1. Groups were age-matched. Cognitively normal (CN) subjects must have no significant cognitive impairment or impaired activities of daily living. Clinical diagnosed AD patients must have had mild AD and had to meet the National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association criteria for probable AD39, whereas mild cognitive impairment subjects (MCI) could not meet these criteria, have largely intact general cognition as well as functional performance, but meet defined criteria for MCI.
CSF biomarker collection and analysis
CSF was collected once in a subset of ADNI participants at baseline. Aβ1–42 and tau levels in CSF were measured using the Luminex platform. ApoE and ferritin protein levels were determined using a Myriad Rules Based Medicine platform (Human Discovery MAP, v1.0; see ADNI materials and methods). CSF Factor H (FH) levels were measured using a multiplex human neurodegenerative kit (HNDG1-36K; Millipore, Billerica, MA) according to the manufacturer’s overnight protocol with minor modifications.
CSF was collected into polypropylene tubes or syringes provided to each site, and then be transferred into polypropylene transfer tubes without any centrifugation step followed by freezing on dry ice within 1 h after collection for subsequent shipment overnight to the ADNI Biomarker Core laboratory at the University of Pennsylvania Medical Center on dry ice. Aliquots (0.5 ml) were prepared from these samples after thawing (1 h) at room temperature and gentle mixing. The aliquots were stored in bar code-labelled polypropylene vials at −80 °C. Fresh, never before thawed, 0.5 ml aliquots for each subject’s set of longitudinal time points were analysed on the same 96-well plate in the same analytical run for this study to minimize run to run and reagent kit lot sources of variation. Within run coefficient of variation (%CV) for duplicate samples ranged from 2.5 to 5.9% for Aβ1–42, 2.2–6.3% for tau and the inter-run %CV for CSF pool samples ranged from 5.1 to 14% for Aβ1–42, 2.7–11.2% for tau.
Apolipoprotein E (ApoE) and ferritin protein levels were determined using Rules Based Medicine (Human Discovery MAP, v1.0).
Further information on the procedures and standard operating procedures can be found in previous publications40,41 and online ( http://www.adni-info.org/).
Structural MRI acquisition and processing
Subjects with a 1.5-T MRI and a sagittal volumetric 3D MPRAGE with variable resolution around the target of 1.2 mm isotropically were included in the analysis. See ( www.loni.ucla.edu/ADNI) and for detail42. The hippocampal and ventral volumes utilized were those in the ADNIMERGE primary table as part of the ADNIMERGE R package, downloaded on the 15 July 2014. Only CN and MCI subjects were included in the MRI analysis. MRI scans were performed at baseline, 6 months, 1 year and then yearly for six years.
Statistical analysis
All statistical work was conducted with R (version 3.1.0)43, using packages ggplot2 (ref. 44), nlme45, car46 and Deducer47. We tested the conditions necessary to apply the regression models, normal distribution of the residuals and the absence of multicolinearity. All models satisfied these conditions. Minimal models were obtained via step down regression using Akaike information criterion (AIC), and Bayesian information criterion (BIC), ensuring that the central hypotheses were maintained. Subjects were excluded from analysis if they had one or more covariates missing. Where subjects prematurely left the study, their data were included in modelling to the point at which they left. The following variables were natural log-transformed to ensure normality: CSF ferritin, Factor H, tau and haemoglobin, while ADAS-cog13 was square-root transformed.
ANCOVA models assessing the differences in each of the CSF biomarkers across the diagnostic groups initially contained age, gender, BMI, APOE genotype, and levels of CSF haemoglobin (Hb) and Factor H (FH). CSF Hb was included as a proxy for blood contamination, to control for the possibility of a traumatic tap introducing plasma ferritin into the CSF samples. FH was used to control for inflammation, since ferritin levels are known to be elevated in certain inflammatory conditions (for example, bacterial meningitis48).
Multiple regression models of CSF ferritin and ApoE initially contained age, gender, BMI, APOE genotype, and levels of CSF Hb and FH, plus various inclusions of CSF tau, Aβ1–42 and either ferritin or ApoE. The minimal models are described in the table legend.
Associations between the baseline Alzheimer’s Disease Assessment Scale Cognition (ADAS-cog13) and Rey Auditory Verbal Learning Test (RAVLT) scores with CSF ferritin, the CSF tau/Aβ1–42 ratio and CSF ApoE were tested with a covariate-adjusted multiple regression for each cogntive scale. For these analyses, age, gender, BMI, years of education, APOE-ɛ4 allele and baseline diagnosis were initially included as covariates. To assess the association of baseline CSF ferritin levels with the longitudinal clinical outcomes (ADAS-cog13 and RAVLT scores over 7 years), linear mixed effects models were used. These models were adjusted for the same variables as the baseline models of cognition, and additionally included time as interacting variable with each of the CSF biomarkers. AD subjects were excluded from the longitudinal analysis because of low rate of follow up (Supplementary Table 2). A significant value for any of these interaction terms would indicate that the variable affected the rate of cognitive change. For the ADAS-cog13, longitudinal analysis, the minimal model included years of education, gender and APOE-ɛ4 allele. For the longitudinal analysis with RAVLT, the minimal model included years of education and gender.
Cox proportional hazards model was used to assess the impact of CSF analytes on the time to AD conversion. The initial model contained age at baseline, gender, years of education and APOE-ɛ4 genotype as confounding variables together with CSF ApoE, tau/Aβ1–42 and ferritin. A minimal model containing only the CSF biomarkers was identified via BIC step down procedure and log likelihood test.
Logistic regression analysis was used to assess the impact of CSF analytes on risk of conversion to AD. Combinations of CSF ferritin, ApoE and tau/Aβ1–42 analytes were included in logistic regression models of MCI conversion to AD that were adjusted for age at baseline, gender, years of education, APOE genotype and BMI. These models determined the predictive performance of these analytes in identifying stable MCI participants from MCI participants who, up to 102 months, had a diagnosis change to AD. The receiver-operator curves and the area under the curve were derived from the predictive probabilities of the logistic regression models.
The relationships between CSF ferritin, ApoE, tau/Aβ1–42 with longitudinal structural (MRI) changes to hippocampus and lateral ventricle were analysed using linear mixed models adjusted for age, years of education, BMI, gender and APOE genotype and intracranial volume. For all models, CSF ferritin, ApoE, tau/Aβ1–42 and baseline diagnosis were included as fixed effects and were not removed from a minimal model. Two random effects were also included, intercepts and slope (time). An interaction between time and diagnosis, time and CSF ferritin, time and CSF ApoE, as well as time and CSF tau/Aβ1–42 were also included for all models. All the AD subjects were excluded from MRI analyses due to low numbers and short follow-up. PET imaging data from ADNI were not included in the analysis because there were too few patients who had CSF ferritin measured and who also underwent PET imaging at baseline.
Additional information
How to cite this article: Ayton, S. et al. Ferritin levels in the cerebrospinal fluid predict Alzheimer’s disease outcomes and is regulated by APOE. Nat. Commun. 6:6760 doi: 10.1038/ncomms7760 (2015).
References
van Rooden, S. et al. 7T T2-weighted magnetic resonance imaging reveals cortical phase differences between early- and late-onset Alzheimer’s disease. Neurobiol. Aging 36, 20–26 (2014).
Smith, M. A., Harris, P. L., Sayre, L. M. & Perry, G. Iron accumulation in Alzheimer disease is a source of redox-generated free radicals. Proc. Natl Acad. Sci. USA 94, 9866–9868 (1997).
Crapper McLachlan, D. R. et al. Intramuscular desferrioxamine in patients with Alzheimer's disease. Lancet 337, 1304–1308 (1991).
Lei, P. et al. Tau deficiency induces parkinsonism with dementia by impairing APP-mediated iron export. Nat. Med. 18, 291–295 (2012).
Jellinger, K., Paulus, W., Grundke-Iqbal, I., Riederer, P. & Youdim, M. B. Brain iron and ferritin in Parkinson's and Alzheimer's diseases. J. Neural Transm. Park. Dis. Dement. Sect. 2, 327–340 (1990).
Connor, J. R., Menzies, S. L., St Martin, S. M. & Mufson, E. J. A histochemical study of iron, transferrin, and ferritin in Alzheimer's diseased brains. J. Neurosci. Res. 31, 75–83 (1992).
Bartzokis, G., Tishler, T. A., Shin, I. S., Lu, P. H. & Cummings, J. L. Brain ferritin iron as a risk factor for age at onset in neurodegenerative diseases. Ann. N. Y. Acad. Sci. 1012, 224–236 (2004).
Quintana, C. et al. Study of the localization of iron, ferritin, and hemosiderin in Alzheimer's disease hippocampus by analytical microscopy at the subcellular level. J. Struct. Biol. 153, 42–54 (2006).
Hansen, T. M., Nielsen, H., Bernth, N. & Moos, T. Expression of ferritin protein and subunit mRNAs in normal and iron deficient rat brain. Brain Res. Mol. Brain Res. 65, 186–197 (1999).
Malecki, E. A., Cable, E. E., Isom, H. C. & Connor, J. R. The lipophilic iron compound TMH-ferrocene [(3,5,5-trimethylhexanoyl)ferrocene] increases iron concentrations, neuronal L-ferritin, and heme oxygenase in brains of BALB/c mice. Biol. Trace Elem. Res. 86, 73–84 (2002).
Zhang, X., Surguladze, N., Slagle-Webb, B., Cozzi, A. & Connor, J. R. Cellular iron status influences the functional relationship between microglia and oligodendrocytes. Glia 54, 795–804 (2006).
Earley, C. J. et al. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology 54, 1698–1700 (2000).
Kuiper, M. A., Mulder, C., van Kamp, G. J., Scheltens, P. & Wolters, E. C. Cerebrospinal fluid ferritin levels of patients with Parkinson’s disease, Alzheimer’s disease, and multiple system atrophy. J. Neural Transm. Park. Dis. Dement. Sect. 7, 109–114 (1994).
Craig-Schapiro, R. et al. Multiplexed immunoassay panel identifies novel CSF biomarkers for Alzheimer's disease diagnosis and prognosis. PloS ONE 6, e18850 (2011).
Paterson, R. W. et al. Cerebrospinal fluid markers including trefoil factor 3 are associated with neurodegeneration in amyloid-positive individuals. Transl. Psychiatry 4, e419 (2014).
Mattsson, N. et al. Effects of cerebrospinal fluid proteins on brain atrophy rates in cognitively healthy older adults. Neurobiol. Aging 35, 614–622 (2014).
Mattsson, N. et al. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA 302, 385–393 (2009).
Corder, E. H. et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science 261, 921–923 (1993).
Cruchaga, C. et al. Cerebrospinal fluid APOE levels: an endophenotype for genetic studies for Alzheimer’s disease. Hum. Mol. Genet. 21, 4558–4571 (2012).
Martinez-Morillo, E. et al. Total apolipoprotein E levels and specific isoform composition in cerebrospinal fluid and plasma from Alzheimer's disease patients and controls. Acta Neuropathol. 127, 633–643 (2014).
Toledo, J. B. et al. CSF Apo-E levels associate with cognitive decline and MRI changes. Acta Neuropathol. 127, 621–632 (2014).
Kester, M. I. et al. CSF biomarkers predict rate of cognitive decline in Alzheimer disease. Neurology 73, 1353–1358 (2009).
Estevez-Gonzalez, A., Kulisevsky, J., Boltes, A., Otermin, P. & Garcia-Sanchez, C. Rey verbal learning test is a useful tool for differential diagnosis in the preclinical phase of Alzheimer's disease: comparison with mild cognitive impairment and normal aging. Int. J. Geriatr. Psychiatry 18, 1021–1028 (2003).
Mattsson, N. et al. CSF protein biomarkers predicting longitudinal reduction of CSF beta-amyloid42 in cognitively healthy elders. Transl. Psychiatry 3, e293 (2013).
Apostolova, L. G. et al. 3D PIB and CSF biomarker associations with hippocampal atrophy in ADNI subjects. Neurobiol. Aging 31, 1284–1303 (2010).
Devos, D. et al. Targeting chelatable iron as a therapeutic modality in Parkinson’s disease. Antioxid. Redox Signal. 21, 195–210 (2014).
Duce, J. A. et al. Iron-export ferroxidase activity of beta-amyloid precursor protein is inhibited by zinc in Alzheimer’s disease. Cell 142, 857–867 (2010).
Christensen, D. Z., Schneider-Axmann, T., Lucassen, P. J., Bayer, T. A. & Wirths, O. Accumulation of intraneuronal Abeta correlates with ApoE4 genotype. Acta Neuropathol. 119, 555–566 (2010).
Huang, X. et al. The A beta peptide of Alzheimer's disease directly produces hydrogen peroxide through metal ion reduction. Biochemistry 38, 7609–7616 (1999).
Yamamoto, A. et al. Iron (III) induces aggregation of hyperphosphorylated tau and its reduction to iron (II) reverses the aggregation: implications in the formation of neurofibrillary tangles of Alzheimer's disease. J. Neurochem. 82, 1137–1147 (2002).
Tofaris, G. K., Revesz, T., Jacques, T. S., Papacostas, S. & Chataway, J. Adult-onset neurodegeneration with brain iron accumulation and cortical alpha-synuclein and tau pathology: a distinct clinicopathological entity. Arch. Neurol. 64, 280–282 (2007).
Kondziella, D. & Zetterberg, H. Hyperphosphorylation of tau protein in superficial CNS siderosis. J. Neurol. Sci. 273, 130–132 (2008).
Lee, J. Y. et al. Apolipoprotein E ablation decreases synaptic vesicular zinc in the brain. Biometals 23, 1085–1095 (2010).
Lomnitski, L., Nyska, A., Shohami, E., Chen, Y. & Michaelson, D. M. Increased levels of intracellular iron in the brains of A poE-deficient mice with closed head injury. Exp. Toxicol. Pathol. 52, 177–183 (2000).
Yuan, X. M., Li, W., Baird, S. K., Carlsson, M. & Melefors, O. Secretion of ferritin by iron-laden macrophages and influence of lipoproteins. Free Radic. Res. 38, 1133–1142 (2004).
Dong, L. M. et al. Human apolipoprotein E. Role of arginine 61 in mediating the lipoprotein preferences of the E3 and E4 isoforms. J. Biol. Chem. 269, 22358–22365 (1994).
Ali-Rahmani, F., Schengrund, C. L. & Connor, J. R. HFE gene variants, iron, and lipids: a novel connection in Alzheimer's disease. Front. Pharmacol. 5, 165 (2014).
Weiner, M. W. et al. The Alzheimer's Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimer's Dement. 8, S1–68 (2012).
McKhann, G. et al. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 34, 939–944 (1984).
Shaw, L. M. et al. Qualification of the analytical and clinical performance of CSF biomarker analyses in ADNI. Acta Neuropathol. 121, 597–609 (2011).
Shaw, L. M. et al. Cerebrospinal fluid biomarker signature in Alzheimer's disease neuroimaging initiative subjects. Ann. Neurol. 65, 403–413 (2009).
Jack, C. R. Jr. et al. The Alzheimer's disease neuroimaging initiative (ADNI): MRI methods. J. Magn. Reson. Imag. 27, 685–691 (2008).
Team, R.C. R. A Language and Environment for Statistical Computing R Foundation for Statistical Computing (2014).
Wickham, H. Ggplot2: Elegant Graphics for Data Analysis Springer New York (2009).
Pinheiro, J., Bates, D., DebRoy, S., Sarkar, D. & Team, R. C. nlme: Linear and Nonlinear Mixed Effects Models (2014).
Fox, J. & Weisberg, S. An R Companion to Applied Regression Sage (2011).
Fellows, I. Deducer: a data analysis GUI for R. J. Stat. Softw. 48, 1–15 (2012).
Kim, Y. O., Kang, J. S., Youm, M. H. & Jong Woo, Y. Diagnostic capability of CSF ferritin in children with meningitis. Pediatr. Neurol. 28, 271–276 (2003).
Acknowledgements
Data collection and sharing for this project was funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defence award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; BioClinica; Biogen Idec; Bristol-Myers Squibb Company; Eisai; Elan Pharmaceuticals; Eli Lilly and Company; F. Hoffmann-La Roche and its affiliated company Genentech; GE Healthcare; Innogenetics, N. V.; IXICO; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Medpace; Merck & Co.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Novartis Pharmaceuticals Corporation; Pfizer; Piramal Imaging; Servier; Synarc; and Takeda Pharmaceutical Company. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health ( www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer's Disease Cooperative Study at the University of California, San Diego. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. Analysis supported by funds from the Australian Research Council, the Australian National Health & Medical Research Council (NHMRC), the CRC for Mental Health (the Cooperative Research Centre (CRC) programme is an Australian Government Initiative), the Yulgilbar foundation, and Operational Infrastructure Support from the Victorian State Government.
Author information
Authors and Affiliations
Consortia
Contributions
S.A. provided-scientific concept, modelling of data and wrote manuscript. N.G.F. helped in modelling of data and wrote manuscript. A.I.B. supervised modelling, wrote manuscript and funded analysis project.
Corresponding author
Ethics declarations
Competing interests
A.I.B. is a shareholder in Prana Biotechnology, Cogstate, Eucalyptus, Mesoblast, Brighton Biotech, LLC, and a payed consultant for Collaborative Medicinal Developments, LLC and Brighton Biotech, LLC. S.A. and N.G.F. declare no competing financial interests.
Additional information
A full list of members and their affiliations appear at the end of the paper.
Supplementary information
Supplementary Information
Supplementary Figures 1-5 and Supplementary Tables 1-3 (PDF 757 kb)
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Ayton, S., Faux, N., Bush, A. et al. Ferritin levels in the cerebrospinal fluid predict Alzheimer’s disease outcomes and are regulated by APOE. Nat Commun 6, 6760 (2015). https://doi.org/10.1038/ncomms7760
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/ncomms7760
This article is cited by
-
Brain pathological changes during neurodegenerative diseases and their identification methods: How does QSM perform in detecting this process?
Insights into Imaging (2022)
-
Apolipoprotein E potently inhibits ferroptosis by blocking ferritinophagy
Molecular Psychiatry (2022)
-
Mercury levels in hair are associated with reduced neurobehavioral performance and altered brain structures in young adults
Communications Biology (2022)
-
Ventricular enlargement caused by aducanumab
Nature Reviews Neurology (2022)
-
Selective ferroptosis vulnerability due to familial Alzheimer’s disease presenilin mutations
Cell Death & Differentiation (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.