Abstract
Epithelial to mesenchymal transition (EMT), and the reverse mesenchymal to epithelial transition (MET), are known examples of epithelial plasticity that are important in kidney development and cancer metastasis. Here we identify ASPP2, a haploinsufficient tumour suppressor, p53 activator and PAR3 binding partner, as a molecular switch of MET and EMT. ASPP2 contributes to MET in mouse kidney in vivo. Mechanistically, ASPP2 induces MET through its PAR3-binding amino-terminus, independently of p53 binding. ASPP2 prevents β-catenin from transactivating ZEB1, directly by forming an ASPP2–β-catenin–E-cadherin ternary complex and indirectly by inhibiting β-catenin’s N-terminal phosphorylation to stabilize the β-catenin–E-cadherin complex. ASPP2 limits the pro-invasive property of oncogenic RAS and inhibits tumour metastasis in vivo. Reduced ASPP2 expression results in EMT, and is associated with poor survival in hepatocellular carcinoma and breast cancer patients. Hence, ASPP2 is a key regulator of epithelial plasticity that connects cell polarity to the suppression of WNT signalling, EMT and tumour metastasis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Thiery, J. P., Acloque, H., Huang, R. Y. & Nieto, M. A. Epithelial–mesenchymal transitions in development and disease. Cell 139, 871–890 (2009).
Thiery, J. P. & Sleeman, J. P. Complex networks orchestrate epithelial–mesenchymal transitions. Nat. Rev. Mol. Cell Biol. 7, 131–142 (2006).
Sleeman, J. P. & Thiery, J. P. SnapShot: the epithelial–mesenchymal transition. Cell 145, 162–162e1 (2011).
Wang, Y. et al. Critical role for transcriptional repressor Snail2 in transformation by oncogenic RAS in colorectal carcinoma cells. Oncogene 29, 4658–4670 (2010).
Carew, R. M., Wang, B. & Kantharidis, P. The role of EMT in renal fibrosis. Cell Tissue Res. 347, 103–116 (2012).
Auersperg, N. et al. E-cadherin induces mesenchymal-to-epithelial transition in human ovarian surface epithelium. Proc. Natl Acad. Sci. USA 96, 6249–6254 (1999).
Law, M. E. et al. Glucocorticoids and histone deacetylase inhibitors cooperate to block the invasiveness of basal-like breast cancer cells through novel mechanisms. Oncogene 32, 1316–1329 (2013).
Aigner, K. et al. The transcription factor ZEB1 (δEF1) promotes tumour cell dedifferentiation by repressing master regulators of epithelial polarity. Oncogene 26, 6979–6988 (2007).
Sottocornola, R. et al. ASPP2 binds Par-3 and controls the polarity and proliferation of neural progenitors during CNS development. Dev. Cell 19, 126–137 (2010).
Cong, W. et al. ASPP2 regulates epithelial cell polarity through the PAR complex. Curr. Biol. 20, 1408–1414 (2010).
Vives, V. et al. ASPP2 is a haploinsufficient tumor suppressor that cooperates with p53 to suppress tumor growth. Genes Dev. 20, 1262–1267 (2006).
Bergamaschi, D. et al. ASPP1 and ASPP2: common activators of p53 family members. Mol. Cell. Biol. 24, 1341–1350 (2004).
Samuels-Lev, Y. et al. ASPP proteins specifically stimulate the apoptotic function of p53. Mol. Cell 8, 781–794 (2001).
Trigiante, G. & Lu, X. ASPP [corrected] and cancer. Nat. Rev. Cancer 6, 217–226 (2006).
Bergamaschi, D. et al. iASPP oncoprotein is a key inhibitor of p53 conserved from worm to human. Nat. Genet. 33, 162–167 (2003).
Zhao, J. et al. Epigenetic silence of ankyrin-repeat-containing, SH3-domain-containing, and proline-rich-region-containing protein 1 (ASPP1) and ASPP2 genes promotes tumor growth in hepatitis B virus-positive hepatocellular carcinoma. Hepatology 51, 142–153 (2010).
Sarraf, S. A. & Stancheva, I. Methyl-CpG binding protein MBD1 couples histone H3 methylation at lysine 9 by SETDB1 to DNA replication and chromatin assembly. Mol. Cell 15, 595–605 (2004).
Liu, Z. J. et al. Downregulated mRNA expression of ASPP and the hypermethylation of the 5′-untranslated region in cancer cell lines retaining wild-type p53. FEBS Lett. 579, 1587–1590 (2005).
Liu, W. K., Jiang, X. Y., Ren, J. K. & Zhang, Z. X. Expression pattern of the ASPP family members in endometrial endometrioid adenocarcinoma. Onkologie 33, 500–503 (2010).
Sgroi, D. C. et al. In vivo gene expression profile analysis of human breast cancer progression. Cancer Res. 59, 5656–5661 (1999).
Tordella, L. et al. ASPP2 suppresses squamous cell carcinoma via RelA/p65-mediated repression of p63. Proc. Natl Acad. Sci. USA 110, 17969–17974 (2013).
Lossos, I. S., Natkunam, Y., Levy, R. & Lopez, C. D. Apoptosis stimulating protein of p53 (ASPP2) expression differs in diffuse large B-cell and follicular center lymphoma: correlation with clinical outcome. Leuk. Lymphoma 43, 2309–2317 (2002).
Vandewalle, C., Van Roy, F. & Berx, G. The role of the ZEB family of transcription factors in development and disease. Cell. Mol. Life Sci. 66, 773–787 (2009).
Dressler, G. R. The cellular basis of kidney development. Annu. Rev. Cell Dev. Biol. 22, 509–529 (2006).
Sanchez-Tillo, E. et al. β-catenin/TCF4 complex induces the epithelial-to-mesenchymal transition (EMT)-activator ZEB1 to regulate tumor invasiveness. Proc. Natl Acad. Sci. USA 108, 19204–19209 (2011).
Santner, S. J. et al. Malignant MCF10CA1 cell lines derived from premalignant human breast epithelial MCF10AT cells. Breast Cancer Res. Treat. 65, 101–110 (2001).
Tang, B. et al. TGF-β switches from tumor suppressor to prometastatic factor in a model of breast cancer progression. J. Clin. Invest. 112, 1116–1124 (2003).
Stadler, S. C. & Allis, C. D. Linking epithelial-to-mesenchymal-transition and epigenetic modifications. Semin. Cancer Biol. 22, 404–410 (2012).
Gorina, S. & Pavletich, N. P. Structure of the p53 tumor suppressor bound to the ankyrin and SH3 domains of 53BP2. Science 274, 1001–1005 (1996).
Shirasawa, S., Furuse, M., Yokoyama, N. & Sasazuki, T. Altered growth of human colon cancer cell lines disrupted at activated Ki-ras. Science 260, 85–88 (1993).
Dajee, M., Tarutani, M., Deng, H., Cai, T. & Khavari, P. A. Epidermal Ras blockade demonstrates spatially localized Ras promotion of proliferation and inhibition of differentiation. Oncogene 21, 1527–1538 (2002).
Molina-Arcas, M., Hancock, D. C., Sheridan, C., Kumar, M. S. & Downward, J. Coordinate direct input of both KRAS and IGF1 receptor to activation of PI3 kinase in KRAS-mutant lung cancer. Cancer Discov. 3, 548–563 (2013).
Kim, T. et al. p53 regulates epithelial–mesenchymal transition through microRNAs targeting ZEB1 and ZEB2. J. Exp. Med. 208, 875–883 (2011).
Zeller, E., Hammer, K., Kirschnick, M. & Braeuning, A. Mechanisms of RAS/β-catenin interactions. Arch. Toxicol. 87, 611–632 (2013).
Wang, Z. et al. N terminus of ASPP2 binds to Ras and enhances Ras/Raf/MEK/ERK activation to promote oncogene-induced senescence. Proc. Natl Acad. Sci. USA 110, 312–317 (2013).
Wang, Y. et al. ASPP1 and ASPP2 bind active RAS, potentiate RAS signalling and enhance p53 activity in cancer cells. Cell Death Differ. 20, 525–534 (2013).
Lee, M. H., Koria, P., Qu, J. & Andreadis, S. T. JNK phosphorylates β-catenin and regulates adherens junctions. FASEB J. 23, 3874–3883 (2009).
Maher, M. T., Mo, R., Flozak, A. S., Peled, O. N. & Gottardi, C. J. β-catenin phosphorylated at serine 45 is spatially uncoupled from β-catenin phosphorylated in the GSK3 domain: implications for signaling. PLoS ONE 5, e10184 (2010).
Sadot, E. et al. Regulation of S33/S37 phosphorylated β-catenin in normal and transformed cells. J. Cell Sci. 115, 2771–2780 (2002).
Faux, M. C., Coates, J. L., Kershaw, N. J., Layton, M. J. & Burgess, A. W. Independent interactions of phosphorylated β-catenin with E-cadherin at cell–cell contacts and APC at cell protrusions. PLoS ONE 5, e14127 (2010).
Moon, R. T., Kohn, A. D., De Ferrari, G. V. & Kaykas, A. WNT and β-catenin signalling: diseases and therapies. Nat. Rev. Genet. 5, 691–701 (2004).
Debnath, J. & Brugge, J. S. Modelling glandular epithelial cancers in three-dimensional cultures. Nat. Rev. Cancer 5, 675–688 (2005).
Yang, J. et al. Molecular cytogenetic characteristics of the human hepatocellular carcinoma cell line HCCLM3 with high metastatic potential: comparative genomic hybridization and multiplex fluorescence in situ hybridization. Cancer Genet. Cytogenet. 158, 180–183 (2005).
Tsai, J. H., Donaher, J. L., Murphy, D. A., Chau, S. & Yang, J. Spatiotemporal regulation of epithelial–mesenchymal transition is essential for squamous cell carcinoma metastasis. Cancer Cell 22, 725–736 (2012).
Ocana, O. H. et al. Metastatic colonization requires the repression of the epithelial–mesenchymal transition inducer Prrx1. Cancer Cell 22, 709–724 (2012).
Yang, J. et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell 117, 927–939 (2004).
Serres, S. et al. Molecular MRI enables early and sensitive detection of brain metastases. Proc. Natl Acad. Sci. USA 109, 6674–6679 (2012).
Carbonell, W. S., Ansorge, O., Sibson, N. & Muschel, R. The vascular basement membrane as “soil” in brain metastasis. PLoS ONE 4, e5857 (2009).
Chao, Y. L., Shepard, C. R. & Wells, A. Breast carcinoma cells re-express E-cadherin during mesenchymal to epithelial reverting transition. Mol. Cancer 9, 179 (2010).
Kim, N. G., Koh, E., Chen, X. & Gumbiner, B. M. E-cadherin mediates contact inhibition of proliferation through Hippo signaling-pathway components. Proc. Natl Acad. Sci. USA 108, 11930–11935 (2011).
Llanos, S. et al. Inhibitory member of the apoptosis-stimulating proteins of the p53 family (iASPP) interacts with protein phosphatase 1 via a noncanonical binding motif. J. Biol. Chem. 286, 43039–43044 (2011).
Liu, C. Y. et al. PP1 cooperates with ASPP2 to dephosphorylate and activate TAZ. J. Biol. Chem. 286, 5558–5566 (2011).
Bertocchi, C., Vaman Rao, M. & Zaidel-Bar, R. Regulation of adherens junction dynamics by phosphorylation switches. J. Signal Transduction 2012, 125295 (2012).
McCaffrey, L. M., Montalbano, J., Mihai, C. & Macara, I. G. Loss of the Par3 polarity protein promotes breast tumorigenesis and metastasis. Cancer Cell 22, 601–614 (2012).
Xue, B., Krishnamurthy, K., Allred, D. C. & Muthuswamy, S. K. Loss of Par3 promotes breast cancer metastasis by compromising cell–cell cohesion. Nat. Cell Biol. 15, 189–200 (2013).
Wang, X. D. et al. SUMO-modified nuclear cyclin D1 bypasses Ras-induced senescence. Cell Death Differ. 18, 304–314 (2011).
Wang, Y. et al. Autophagic activity dictates the cellular response to oncogenic RAS. Proc. Natl Acad. Sci. USA 109, 13325–13330 (2012).
Debnath, J., Muthuswamy, S. K. & Brugge, J. S. Morphogenesis and oncogenesis of MCF-10A mammary epithelial acini grown in three-dimensional basement membrane cultures. Methods 30, 256–268 (2003).
Vooijs, M., Jonkers, J. & Berns, A. A highly efficient ligand-regulated Cre recombinase mouse line shows that LoxP recombination is position dependent. EMBO Rep. 2, 292–297 (2001).
Carretero, J. et al. Integrative genomic and proteomic analyses identify targets for Lkb1-deficient metastatic lung tumors. Cancer Cell 17, 547–559 (2010).
Notari, M. et al. Inhibitor of apoptosis-stimulating protein of p53 (iASPP) prevents senescence and is required for epithelial stratification. Proc. Natl Acad. Sci. USA 108, 16645–16650 (2011).
McAteer, M. A. et al. In vivo magnetic resonance imaging of acute brain inflammation using microparticles of iron oxide. Nat. Med. 13, 1253–1258 (2007).
Liang, B. et al. Myeloid differentiation factor 88 promotes growth and metastasis of human hepatocellular carcinoma. Clin. Cancer Res. 19, 2905–2916 (2013).
Urakami, S. et al. Epigenetic inactivation of Wnt inhibitory factor-1 plays an important role in bladder cancer through aberrant canonical Wnt/β-catenin signaling pathway. Clin. Cancer Res. 12, 383–391 (2006).
Montserrat, N. et al. Repression of E-cadherin by SNAIL, ZEB1, and TWIST in invasive ductal carcinomas of the breast: a cooperative effort? Hum. Pathol. 42, 103–110 (2011).
Rubin, M. A. et al. E-cadherin expression in prostate cancer: a broad survey using high-density tissue microarray technology. Hum. Pathol. 32, 690–697 (2001).
Theurillat, J. P. et al. NY-ESO-1 protein expression in primary breast carcinoma and metastases: correlation with CD8 + T-cell and CD79a + plasmacytic/B-cell infiltration. Int. J. Cancer 120, 2411–2417 (2007).
Acknowledgements
This work was supported mainly by the Ludwig Institute for Cancer Research Ltd (X.L.), and in part by the International Cooperation and Exchange Project of the National Natural Science Foundation of China (Y.G. and X.L.). Y.G. and J. Zhao are also supported by the National Basic Research Program of China (973 Program: 2010CB945600 and 2010CB833600). Y.W. is supported by the Medical Research Council (MR/J000930/1). S.S., J.R.L., M.S.S. and N.R.S. are funded by Cancer Research UK (grant number C5255/A12678). We thank K. Bryon-Dodd, G. Sutendra, P. Miller, M. White, L. Buti and C. Goding for critical reading of the manuscript. We are grateful to S. Shirasawa for providing HKe3 cells, F. Miller and S. Santner for the 4T1 and MCF10A series of breast cancer cell lines and Y. Fujita for the E-cadherin–Myc construct.
Author information
Authors and Affiliations
Contributions
X.L. and Y.G. coordinated and supervised the project and designed the experiments together with Y.W. and F.B.; Y.W. carried out most of the experiments, analysed data and wrote the paper with X.L.; F.B. carried out experiments and analysed data for Figs 3d, 6d, e, 7a, b, 8a–c and Supplementary Figs 6c, d, 8a; C.R. carried out experiments for Fig. 5f, g and Supplementary Figs 2k, 5b–d, f, g; S.S., J.R.L., M.S.S. and N.R.S. designed, carried out experiments and analysed data with Y.W. for Fig. 7c–e and Supplementary Fig. 7b; V.S. and F.F. carried out immunohistochemistry in breast cancer tissue microarrays designed by H.M. and analysed data for Fig. 8d, e and Supplementary Fig. 8b; C.T. carried out experiments for Fig. 1b and Supplementary Fig. 1a; S.K. carried out experiments for Fig. 1c; J. Zak and S.Z. provided materials for Supplementary Fig. 1b, c; G.W. and A.L. provided the human HCC samples; P.A.O. carried out some experiments related to this project; D.C.H. and J.D. provided HKe3–ER:HRASV12 and MCF10A–ER:HRASV12 cell lines; R.D.G. provided pathological advice; J. Zhao designed and analysed the experiments of HCC with F.B.; X.T. carried out experiments and analysed data with F.B. for Fig. 8a–c and Supplementary Fig. 8a.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 ASPP2 regulates MET in mouse kidney in vivo.
(a) Immunohistochemical staining of ZEB1 in kidney tissues from ASPP2+/+ or ASPP2Δ3/Δ3 mice. Scale bar: 40 μm. (b) Immunofluorescence staining of ZEB1 (green) and E-cadherin (red) in kidney tissues from ASPP2loxP/loxP Cre–ER mice with indicated treatment. TO-PRO-3 (blue) was used to stain nuclei. Scale bar: 40 μm. (c) Protein expression of ZEB1, E-cadherin and β-catenin in kidney tissues from ASPP2loxP/loxP Cre–ER mice with indicated treatment. Scores under the bands are relative levels against control group (1.0). β-Tubulin was used as a loading control. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 2 N-terminal ASPP2 is required and sufficient to induce MET.
(a) Immunofluorescence staining of ASPP2 (green), E-cadherin (green), ZEB1 (red) or Vimentin (green) in a panel of MCF10A cells. Arrows indicate junctional ASPP2 or E-cadherin. Scale bar: 10 μm. (b) Protein expression of ASPP2, E-cadherin, ZEB1, Vimentin and β-catenin in a panel of MCF10A cell lines. WT: wild-type β-Tubulin was used as a loading control. Scores under the bands are relative levels against WT (1.0). (c) Fold change in mRNA levels of ASPP2, E-cadherin and ZEB1 in a panel of MCF10A cell lines. (d) Protein expression of ASPP2 in a panel of MCF10A cell lines treated with or without 5-AZ. Scores under the bands are relative levels against untreated WT (1.0). (e) Fold change in mRNA levels of ASPP2, ZEB1 and E-cadherin following 5-AZ treatment in MCF10A-M3 cells. (f) Schematic representation of truncated ASPP2 mutants. (g) Immunofluorescence staining of V5-ASPP2 (green) and ZEB1 (red) in MCF10A-M3 cells transfected with V5-tagged full-length or ASPP2 fragments. DAPI (blue) was used to stain nuclei. Scale bar: 10 μm. Triangles indicate ZEB1 expression in V5 + cells. The percentage of V5 + /ZEB1 down-regulated cells in indicated transfected samples and the percentage of V5 + /with MET morphology change in indicated transfected samples are shown as graphs. Error bars indicate SD. n = 3 samples. 100 V5 positive cells were counted per sample. (h and i) Immunofluorescence staining of V5-ASPP2 (green) and ZEB1 (red) (h) or V5-ASPP2 (green) and E-cadherin (red) (i) in U2OS cells transfected with V5-tagged full-length or ASPP2 fragments. TO-PRO-3 (blue) was used to stain nuclei. Scale bar: 10 μm. Arrows indicate junctional staining of ASPP2 or E-cadherin. Triangles indicate ZEB1 expression in V5 + cells. The percentage of V5 + /E-cadherin + cells or V5 + /ZEB1 down-regulated cells in indicated transfected samples are shown as graphs. Error bars indicate SD. n = 3 samples. 100 V5 positive cells were counted per sample. (j) Immunofluorescence staining of E-cadherin (green) or ZEB1 (red) in MCF10A-M3 cells transfected with E-cadherin-myc plasmid. TO-PRO-3 (blue) was used to stain nuclei. Scale bar: 10 μm. (k) Immunofluorescence staining of E-cadherin (red) or ASPP2 (green) in MDA-MB-231 cells transfected with or without E-cadherin-myc plasmid. Scale bar: 10 μm. (l) Immunofluorescence staining of V5-ASPP2 (green) in MDA-MB-231 cells transfected with full-length V5-tagged ASPP2. TO-PRO-3 (blue) was used to stain nuclei. Scale bar: 10 μm. Data in c and e are the mean of 2 independent experiments performed in duplicate. For source data, see Supplementary Table 1. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 3 ASPP2 depletion promotes EMT and sensitises cells to oncogenic RAS-induced EMT.
(a) Immunofluorescence staining of E-cadherin (red) or ZEB1 (green) in HCT116 cells with indicated RNAi transfections. TO-PRO-3 was used to stain nuclei. Scale bar: 10 μm. (b) Q-RT-PCR analysis of E-cadherin, Snail1, Snail2, ZEB1 and TWIST expression in HCT116 cells transfected with control or ASPP2 RNAi. (c) Immunofluorescence staining of E-cadherin (green) in HCT116 cells with indicated RNAi transfections. TO-PRO-3 (blue) was used to stain nuclei. Scale bar: 10 μm. (d) Immunofluorescence staining of ZEB1 (green) in MCF10A ER:HRAS V12 cells with indicated treatments. TO-PRO-3 (blue) was used to stain nuclei. Scale bar: 10 μm. (e) Q-RT-PCR and western blot of samples from MCF10A-ER:HRASV12 cells with indicated treatments showing effects on ZEB1 and ASPP2. β-Tubulin was used as a loading control. Data in b and e are the mean of 2 independent experiments performed in duplicate. For source data, see Supplementary Table 1. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 4 ASPP2 knockdown induces ZEB1 expression via β-catenin, not p53.
(a) Western blot of lysates from HKe3-ER:HRASV12 cells with indicated treatments showing effects on ZEB1 and p53. GAPDH was used as a loading control. (b) ChIP assays of β-catenin’s ability to bind the ZEB1 promoter in HKe3 ER:HRAS V12 cells with the indicated treatments. qPCR of fragments of the ZEB1 promoter immunoprecipitated in ChIP assays from HKe3 ER:HRAS V12 cells with an antibody against β-catenin and control IgG. Amplified ZEB1 promoter region (−325∼−101) contains β-catenin/TCF binding sites at −161. (c) Protein expression of ZEB1, ASPP2, ASPP1 and β-catenin in HKe3-ER:HRASV12 cells with indicated treatments. β-Tubulin was used as a loading control. (d) Western blot showing the knockdown of β-catenin in MCF10A-WT or M3 cells. GAPDH was used as a loading control. (e) Protein expression of ZEB1, ASPP2 and β-catenin in 4-OHT-treated MCF10A-ER:HRASV12 cells with indicated RNAi transfections. β-Tubulin was used as a loading control. (f) Protein expression of ZEB1, ASPP2 and β-catenin in HepG2 cells with indicated RNAi transfections. β-Tubulin was used as a loading control. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 5 ASPP2 binds β-catenin and negatively regulates the WNT/β-catenin pathway.
(a) Immunofluorescence staining of V5-ASPP2 or β-catenin in MCF10A-M3 cells transfected with control plasmid (Vector) or V5-ASPP2. DAPI (blue) was used to stain nuclei. Scale bar: 10 μm. Arrows indicate junctional staining of ASPP2 or β-catenin. (b) Immunofluorescence staining of ASPP2 (green) and E-cadherin or β-catenin (magenta) in MCF7 cells. Scale bar: 10 μm. (c) Co-immunoprecipitation experiment using in vitro-translated (IVT) β-catenin and V5-tagged ASPP2. A rabbit polyclonal antibody against ASPP2 was used to immunoprecipitate ASPP2. β-catenin and ASPP2 levels were then analysed by western blot. (d) Different amount of total cell lysates from MCF7 and MDA-MB-231 cells, 30 μg or 60 μg used as input respectively, were immunoprecipitated with a rabbit polyclonal anti-ASPP2 antibody or control IgG. β-catenin, E-cadherin and ASPP2 levels are indicated. β-Tubulin was used as a loading control. (e) ASPP2 binds β-catenin and the binding does not require PAR3. Total cell lysates from HKe3 cells transfected with control or PAR3 RNAi were immunoprecipitated with a rabbit polyclonal antibody against ASPP2 or control IgG. β-catenin, PAR3 and ASPP2 levels were then analysed by western blot. IgGL indicates IgG light chain. (f) Immunofluorescence staining showing the effect of WNT3a on endogenous β-catenin in wild-type and ASPP2Δ3/Δ3 MEFs, respectively. Green and red arrows indicate nuclei containing β-catenin in wild-type or ASPP2Δ3/Δ3 MEFs, respectively. Scale bar: 50 μm. (g) Immunofluorescence staining showing the effect of LiCl on endogenous β-catenin in wild-type or ASPP2Δ3/Δ3 MEFs, respectively. Green and red arrows indicate nuclei containing β-catenin in wild-type and ASPP2Δ3/Δ3 MEFs, respectively. Scale bar: 50 μm. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 6 ASPP2 deficiency promotes cell migration and invasion.
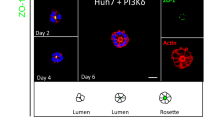
(a) Representative phase contrast images of MCF10A-ER:HRASV12 cells cultured in Matrigel with indicated treatments. Scale bar: 40 μm. (b) Protein expression of ASPP2 in MCF10A-ER:HRASV12 cells transfected with control or ASPP2 RNAi for the indicated time. iASPP was used as a loading control. (c) Hep3B or HCC-LM3 cells were infected with ASPP2 shRNA or shNon for 72 h. Cells were then seeded in 96-well plates for MTS assay. (d) Hep3B or HepG2 cells infected with ASPP2 shRNA or shNon were subjected to transwell migration assay or Matrigel invasion assay. ∗P < 0.05. The expressions of ASPP2 were detected by western blot. Data in c and d are the mean from a representative experiment, and error bars indicate SEM. n = 6 wells in c and n = 5 random fields in d. Statistical significance was determined by a two-tailed, unpaired Student’s t-test. The experiments were repeated 5 times. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 7 ASPP2 expression inhibits metastasis in vivo.
(a) Western blot of V5 in 4T1-GFP cells transfected with control plasmids or V5-tagged full-length (1-1128) or N terminal (1-360) ASPP2. (b) Visible tumours were counted in the 4T1-GFP model by virtue of the H&E staining; graph showing total tumour number per mouse brain for each group. Data in b are individual values with mean, and error bars indicate SD. n = 3 mice per group. For source data, see Supplementary Table 1. Uncropped images of blots are shown in Supplementary Fig. 9.
Supplementary Figure 8 ASPP2 expression correlates with EMT status in human HCC, and the ASPP2 expression pattern in breast cancer is also shown.
(a) The relationships between ASPP2 expression and protein expression of β-catenin, ZEB1 and E-cadherin were analysed (Mann–Whitney U-test: P < 0.001). Nuclear β-catenin negative n = 133 and nuclear β-catenin positive n = 40; nuclear ZEB1 negative n = 126 and nuclear ZEB1 positive n = 53; junctional E-cadherin positive n = 69 and junctional E-cadherin negative n = 117. Spread of data denoted by box-and-whisker plot, the central box represents the value from the lower to upper quartile (25th–75th percentile). The middle line represents the median. The whisker ends 1 and 99 percentiles. (b) Representative ASPP2 staining pattern (High or Low ASPP2) in 275 human breast cancer tissue microarray cores. Scale bar: 50 μm. For source data, see Supplementary Table 1.
Supplementary information
Supplementary Information
Supplementary Information (PDF 7092 kb)
Rights and permissions
About this article
Cite this article
Wang, Y., Bu, F., Royer, C. et al. ASPP2 controls epithelial plasticity and inhibits metastasis through β-catenin-dependent regulation of ZEB1. Nat Cell Biol 16, 1092–1104 (2014). https://doi.org/10.1038/ncb3050
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncb3050
This article is cited by
-
Integrated network pharmacology and cellular assay reveal the biological mechanisms of Limonium sinense (Girard) Kuntze against Breast cancer
BMC Complementary Medicine and Therapies (2023)
-
The role of the ZEB1–neuroinflammation axis in CNS disorders
Journal of Neuroinflammation (2022)
-
Enhanced CHOLESTEROL biosynthesis promotes breast cancer metastasis via modulating CCDC25 expression and neutrophil extracellular traps formation
Scientific Reports (2022)
-
Knockout of ASPP2 promotes DEN-induced hepatocarcinogenesis via the NF-κB pathway in mice
Cancer Gene Therapy (2022)
-
ASPP2 maintains the integrity of mechanically stressed pseudostratified epithelia during morphogenesis
Nature Communications (2022)