Abstract
Patients with double-hit or triple-hit lymphoma have a significantly worse prognosis compared to patients with diffuse large B-cell lymphoma without MYC rearrangement. However, the prognostic importance of extra copies of MYC, BCL2, or BCL6 has not been fully explored. We studied 663 patients with de novo diffuse large B-cell lymphoma in whom the status of MYC/8q24, BCL2/18q21, and BCL6/3q27 were assessed by fluorescence in situ hybridization. Cases of double or triple extra copy lymphoma were defined by the presence of increased MYC copies and increased BCL2 and/or BCL6 copies or rearrangement. In total, 76 patients with diffuse large B-cell lymphoma had MYC extra copies including 43 cases of double or triple extra copy lymphoma; 105 patients had diffuse large B-cell lymphoma with MYC-R including 56 double- or triple-hit lymphoma; and 482 diffuse large B-cell lymphoma patients had no MYC abnormality (MYC normal). Patients with MYC extra copies, similar to MYC-R, had a worse overall survival compared with MYC normal patients (both P<0.01). The prognosis between patients with MYC extra copies and MYC-R was not statistically significantly different (P=0.086). Cell-of-origin classification failed to correlate with survival in the MYC extra copies group, similar to the MYC-R patient group. Compared with patients with double- or triple-hit lymphoma, patients with double or triple extra copy lymphoma had a higher complete remission rate (P=0.02), but there was no significant statistical difference in overall survival (P=0.089). Intensive induction chemotherapy regimens improved the overall survival of patients with double or triple extra copy lymphoma, but there was no significant improvement of overall survival in patients with MYC-R tumors. Multivariate analysis showed that MYC extra copy in diffuse large B-cell lymphoma is an independent poor prognostic factor, similar to MYC rearrangement.
Similar content being viewed by others
Main
Diffuse large B-cell lymphoma is the most common type of non-Hodgkin lymphoma worldwide. The standard frontline therapy for patients with diffuse large B-cell lymphoma is rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) and about 60% of patients are cured using this regimen. However, about 10% of patients with diffuse large B-cell lymphoma are refractory to R-CHOP and 30% of patients eventually relapse. Identifying patients with poorer prognosis who might benefit from more aggressive therapy is needed.
MYC, first identified in Burkitt lymphoma, is located on chromosome 8q24 and belongs to a family of transcription factors with either gene activating or repressing functions.1, 2, 3 Deregulation of MYC has oncogenic potential, resulting in enhanced cell proliferation, angiogenesis, apoptosis, genomic instability, and inhibition of cellular differentiation.2, 4 In addition to Burkitt lymphoma, MYC rearrangement also has been identified in 5–15% of patients with diffuse large B-cell lymphoma as well as uncommonly in other types of lymphoma.5, 6, 7, 8 In patients with diffuse large B-cell lymphoma, MYC rearrangement has been shown to be associated with a poorer prognosis.7, 9, 10, 11, 12
Double-hit lymphoma is an aggressive large B-cell lymphoma with concurrent MYC and BCL2 and/or BCL6 rearrangements. MYC/BCL2 double-hit lymphoma is the most common type of double-hit lymphoma, representing at least 65% of all double-hit lymphoma, followed by triple-hit lymphoma involving MYC, BCL2 and BCL6, and MYC/BCL6 double-hit lymphoma.13, 14, 15 The recently published revision of the World Health Organization classification of lymphoid neoplasms has designated double- or triple-hit lymphoma as a new category: high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements.16 Multiple studies in the literature have shown that patients with double- or triple-hit lymphoma have a poor prognosis with a rapidly progressive clinical course.12, 13, 17, 18, 19, 20, 21, 22 The identification of rearrangements of MYC, BCL2, and BCL6 in diffuse large B-cell lymphoma is conveniently performed by fluorescence in situ hybridization (FISH), which allows assessment of paraffin-embedded tissue biopsy specimens. In addition to identifying gene rearrangement, FISH does not uncommonly detect extra signals (or copies) of MYC, BCL2, or BCL6. The prognostic impact of extra copies of MYC, BCL2, or BCL6 has not been fully elucidated.
In this study, we attempt to address two issues. First, we assess the frequency and clinicopathologic features of patients with diffuse large B-cell lymphoma harboring extra copies of MYC, BCL2, or BCL6. Second, we sought to determine the prognostic impact of extra copies of MYC, BCL2, and BCL6 in patients with diffuse large B-cell lymphoma. As a part of the second question, we compared the outcome of patients with double or triple extra copy lymphoma to patients with double- (or triple-) hit lymphoma.
Materials and methods
Patient Selection
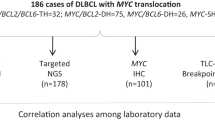
This retrospective study was approved by the institutional review board. We retrieved all cases of adult de novo diffuse large B-cell lymphoma with MYC status confirmed by FISH at The University of Texas MD Anderson Cancer Center and Vanderbilt University from 2010 to 2015. A total of 663 cases were identified. In earlier years, MYC, BCL2, and BCL6 FISH were performed together for newly diagnosed diffuse large B-cell lymphoma cases. Subsequently, guidelines were switched to perform MYC FISH initially, and if positive to add testing for BCL2 and BCL6. Therefore, BCL2 and BCL6 FISH were performed in a subset of cases. Double- or triple-hit lymphoma and double or triple extra copy lymphoma were defined by the cytogenetic status of MYC, BCL2, and BCL6 (Table 1). Patients with the following history or diagnoses were excluded: (1) history of low-grade B-cell lymphoma; (2) post-transplant lymphoproliferative disorders; (3) primary mediastinal large B-cell lymphoma; (4) primary central nervous system large B-cell lymphoma; and (5) EBV-positive diffuse large B-cell lymphoma. The choice of therapy for these patients was at the discretion of the treating physician. Overall, intensive chemotherapy regimens such as rituximab, etoposide, prednisone, cyclophosphamide, and doxorubicin (R-EPOCH) or rituximab, cyclophosphamide, vincristine, doxorubicin, dexamethasone, and cytarabine (R-Hyper-CVAD) were preferred for patients with diffuse large B-cell lymphoma who had high-risk clinical and/or pathologic features. Corresponding medical records were reviewed to obtain clinical information.
Immunophenotypic Analysis
Immunohistochemical studies were performed using antibodies specific for c-MYC (clone Y69, Epitomics, Burlingame, CA, USA), BCL2 (Leica Biosystems, Buffalo Grove, IL, USA), and BCL6 (Dako, Carpinteria, CA, USA). Testing was carried out using formalin-fixed, paraffin-embedded tissue sections, an avidin-biotin-peroxidase complex method, and an automated immunostainer (Ventana Medical Systems, Tucson, AZ, USA). Positivity of the expression for MYC, BCL2, or BCL6 was defined as >40, >50, and >30% positive cells, respectively, as has been reported previously.7, 12, 14, 18, 23, 24
Cytogenetic Analysis
All cytogenetic testing, either conventional karyotyping or FISH, was performed on diagnostic biopsy specimens obtained during the initial workup of these patients. Conventional G band karyotype analysis was performed on 48 cases. The karyotypes were reported according to the 2016 International System for Human Cytogenetic Nomenclature.25 FISH analysis was performed on all cases using a LSI MYC dual-color break-apart probe. A large subset of cases was also assessed using the LSI IGH@BCL2 dual-color, dual fusion probe set, and a smaller subset of cases was studied using the LSI BCL6 dual-color break-apart probe (Abbott Laboratories, Des Plaines, IL, USA) following the manufacturer’s instructions. The signals from 200 nuclei were analyzed. The cutoffs for considering a tumor sample to have rearrangement or extra copies of MYC, BCL2, and BCL6 were different, and cutoffs were also different in bone marrow smears vs fixed, paraffin-embedded tissue sections. Nevertheless, all cutoffs were <20% and in this study all cases considered positive for MYC, BCL2, and BCL6 extra copies or rearrangement had abnormal signals present in >20% of nuclei assessed.
Statistical Analysis
Patient survival was analyzed using the Kaplan–Meier method and compared using the log-rank test. Fisher’s exact test was used to compare clinicopathologic features. Multivariate Cox proportional hazard analysis was performed using SAS R version 3.3.1 software. A P-value of ≤0.05 was considered statistically significant.
Results
Patients’ Overall Characteristics
The 663 patients in the study group included 426 men and 237 women with a median age of 61 years (range, 18–96). All cases were assessed for MYC status by FISH. There were 105 (16%) cases of diffuse large B-cell lymphoma with MYC rearrangement, 76 (12%) had MYC extra copies, and 482 had no MYC abnormality (MYC normal). A total of 439 cases had BCL2 results including 110 (25%) cases with BCL2 rearrangement, 70 (16%) with BCL2 extra copies, and 259 with normal BCL2 status (BCL2 normal). Two hundred and eighty patients had BCL6 results including 68 (24%) with BCL6 rearrangement, 35 (13%) with BCL6 extra copies, and 177 with normal BCL6 status (BCL6 normal).
The patients with MYC extra copies are discussed separately below. The 105 cases of diffuse large B-cell lymphoma harboring MYC rearrangement included 28 cases with only MYC-R, 56 with concurrent MYC and BCL2 or BCL6 rearrangements (45 double- and 11 triple-hit lymphoma), and 21 cases with unknown BCL2 and/or BCL6 status. Compared to patients with diffuse large B-cell lymphoma without MYC rearrangement, those with MYC rearrangement had a significantly worse overall survival (OS) (P<0.0001).
Diffuse Large B-cell Lymphoma with MYC Extra Copies
A representative case of diffuse large B-cell lymphoma with MYC extra copy was shown in Figure 1. Twelve of 76 (16%) cases of diffuse large B-cell lymphoma showed MYC amplification (≥5 copies), with a median copy number of 7 (range, 5–20). The remaining 64 (84%) cases showed 3–4 copies of MYC. There was no difference in OS between patients with diffuse large B-cell lymphoma with 3–4 copies of MYC vs 5 or more copies (P=0.41) (Figure 2a). Therefore, both subsets were combined into one MYC extra copy group for further analysis.
Comparison of overall survival based on (a) MYC copy numbers; (b) MYC fluorescence in situ hybridization (FISH) status; (c) MYC FISH status in R-CHOP-treated patients; (d) MYC FISH status in patients who received intensive chemotherapy (R-EPOCH and R-HyperCVAD); (e) BCL2 FISH status; and (f) BCL6 FISH status.
The clinical and pathologic features of patients with MYC extra copies, in large part, were similar to patients in the MYC normal group except that the complete remission rate of patients in the MYC extra copy group was significantly lower than those patients in the MYC normal group (P=0.011; Table 2). Three patients in the MYC extra copy group had their tumors assessed by conventional cytogenetics; all showed a complex karyotype and none showed trisomy or polysomy 8.
The clinical and pathologic features of patients in the MYC extra copies group were compared to patients with diffuse large B-cell lymphoma with MYC-R. Patients in the MYC extra copies group had a lower frequency of involvement of bone marrow and other extranodal sites (P<0.01), similar to patients with diffuse large B-cell lymphoma with MYC normal. Diffuse large B-cell lymphoma with MYC extra copies, compared to diffuse large B-cell lymphoma with MYC rearrangement, less often had a germinal center B-cell immunophenotype and less frequently showed MYC expression and MYC and BCL2 coexpression (double-positive or double-expresser lymphoma) (P<0.01). Patients in the MYC extra copies group also less frequently received intensive induction chemotherapy, that is R-EPOCH or R-HyperCVAD, than patients in the MYC rearrangement group (P=0.011; Table 2). Compared to R-CHOP, intensive chemotherapy didn’t improve the OS significantly, but only a trend toward better prognosis for patients in the MYC extra copy group (P=0.13).
Patients with diffuse large B-cell lymphoma associated with either MYC extra copies or MYC rearrangement had a worse OS than patients with MYC normal diffuse large B-cell lymphoma (P<0.01). There was a trend toward better OS for patients in the MYC extra copy group vs the MYC rearrangement group; however, this was not statistically significant (P=0.086) (Figure 2b). OS was further compared among these three MYC groups based on induction chemotherapy. As shown in Figure 2c and d, the prognostic significance of MYC extra copies in patients treated with either R-CHOP or intensive chemotherapy was similar to that observed in the whole group.
The prognostic significance of BCL2 extra copies or BCL6 extra copies was evaluated in patients with FISH results available for BCL2 (n=439) or BCL6 (n=280), respectively. Extra copies of BCL2 or BCL6 were not associated with OS in patients with diffuse large B-cell lymphoma in this study (Figure 2e and f).
Double/Triple Extra Copy Lymphoma vs Double-/Triple-Hit Lymphoma
Some diffuse large B-cell lymphoma cases had MYC extra copies with concomitant extra copies of BCL2 and/or BCL6. Other cases of diffuse large B-cell lymphoma had MYC extra copies with concomitant rearrangements of BCL2 and/or BCL6. There was no statistical difference in the OS of patients with diffuse large B-cell lymphoma associated with MYC extra copy and extra copies BCL2 and/or BCL6 vs diffuse large B-cell lymphoma associated with MYC extra copies and rearrangement of BCL2 and/or BCL6 (Figure 3a; P=0.80). We therefore grouped these patients together as double or triple extra copy lymphoma. A total of 43 patients had either double extra copy lymphoma (n=21) or triple extra copy lymphoma (n=22). The double extra copy lymphoma and triple extra copy lymphoma patient subgroups had a similar OS (P=0.69) and therefore they were combined to compare with patients who had double- or triple-hit lymphoma and those with MYC normal diffuse large B-cell lymphoma.
Overall survival comparison based on (a) BCL2 and BCL6 rearrangement vs extra copies in patients with MYC extra copies; (b) in patients with MYC normal, double/triple extra copy lymphoma, and double-/triple-hit lymphoma; (c) different induction regimens within double/triple extra copy lymphoma; (d) different induction regimens within double-/triple-hit lymphoma.
Patients with double or triple extra copy lymphoma showed a lower frequency of extranodal involvement and less often had high stage disease compared to patients with double- or triple-hit lymphoma. In addition, diffuse large B-cell lymphoma with MYC extra copies was less often of germinal center B-cell immunophenotype and less often showed BCL2, BCL6, and MYC expression or coexpression of MYC and BCL2 (Table 3; P<0.05). All other clinicopathologic features were similar between patients with double- or triple-hit lymphoma and those with double or triple extra copy lymphoma (Table 3).
Overall, patients with double or triple extra copy lymphoma or double- or triple-hit lymphoma had significantly worse OS than patients with MYC normal diffuse large B-cell lymphoma (P<0.0001) (Figure 3b). The OS in the double or triple extra copy lymphoma patient group was not significantly different from the double- or triple-hit lymphoma patient group, although there might be a trend toward a better OS for patients with double or triple extra copy lymphoma (P=0.089). Patients with double or triple extra copy lymphoma received similar induction chemotherapy as did patients with double- or triple-hit lymphoma. Intensive induction chemotherapy vs R-CHOP therapy correlated with improved OS of double or triple extra copy lymphoma patients (Figure 3c; P=0.047), but did not significantly correlate with better OS in double- or triple-hit lymphoma patients (Figure 3d; P=0.24).
Cell of Origin Classification
All cases were examined for cell-of-origin classification using the Hans’ algorithm. In total, 380 (57%) cases of diffuse large B-cell lymphoma had a germinal center B-cell immunophenotype and 283 (43%) cases had a non-germinal center B-cell immunophenotype. In the MYC extra copies group, 47 (62%) diffuse large B-cell lymphoma had a germinal center B-cell and 29 (38%) tumors had a non-germinal center B-cell immunophenotype. Cell-of-origin failed to predict OS in the MYC extra copies patient group (P=0.19). In the double or triple extra copy lymphoma group, 58% of patients had diffuse large B-cell lymphoma with a germinal center B-cell immunophenotype. Cell-of-origin also failed to predict OS in the double or triple extra copy lymphoma group.
We compared the MYC extra copies group to patients with diffuse large B-cell lymphoma with MYC rearrangement or MYC normal. MYC rearranged diffuse large B-cell lymphoma (85%) more often had a germinal center B-cell-like immunophenotype as compared to either MYC extra copies (62%) or MYC normal (51%) (Table 2; P<0.01). Similarly, double- or triple-hit lymphoma more often were of germinal center B-cell type when compared to patients with double or triple extra copy lymphoma (Table 3; 93% vs 58%; P=0.02). Cell-of-origin also failed to predict OS in the MYC rearrangement group (P=0.16) in this study.
Multivariate Analysis
To further explore if MYC extra copies, MYC rearrangement, double- or triple-hit lymphoma, and double or triple extra copy lymphoma were independent prognostic factors in diffuse large B-cell lymphoma patients, these variables were entered into multivariate Cox proportional hazard analysis together with other factors that also predict OS in univariate analysis, including extranodal sites of involvement >1, elevated serum LDH level, high stage (III/IV) disease, International Prognostic Index, and complete remission. Induction chemotherapy was also considered to exclude therapy effect. As shown in Table 4, MYC extra copies, MYC rearrangement, double- or triple-hit lymphoma, and double or triple extra copy lymphoma were all independent prognostic factors for OS in this cohort of diffuse large B-cell lymphoma patients.
Discussion
Multiple studies have described the frequency and prognostic significance of MYC rearrangement in diffuse large B-cell lymphoma. However, the role of MYC extra copies in diffuse large B-cell lymphoma is less well elucidated. Earlier retrospective studies that have assessed the prognostic importance of MYC extra copies have yielded conflicting results.11, 26, 27, 28, 29, 30 In a study by Yoon et al,30 11 of 154 (7%) diffuse large B-cell lymphoma patients with MYC extra copies showed an inferior OS in univariate analysis, similar to patients with MYC rearrangement; however, MYC aberrancy failed to predict OS in multivariate analysis. Mossafa et al27 studied 344 cases of non-Hodgkin lymphoma and showed that 16 (5%) cases had MYC extra copies and were associated with a poor prognosis: 9 patients died during a median follow-up of 11 months, but these included different types of lymphomas. Another study of 141R-CHOP treated de novo diffuse large B-cell lymphoma patients showed 10 (7%) cases with MYC extra copy, which correlated with a poorer prognosis.26 However, the authors included some MYC rearrangement cases in the MYC extra copies group. In contrast, Testoni et al29 found that MYC extra copies predicted a poorer prognosis only when concomitant del(8p) was present in a series of 166 patients, with diffuse large B-cell lymphoma received R-CHOP. In the study by Landsburg et al,31 22 patients with MYC amplification (>4 copies) were included and had a similar 2-year OS compared to MYC normal patients. Another study suggested that patients with diffuse large B-cell lymphoma associated with MYC amplification (≥5 copies), but not those with 3–4 copies of MYC was associated with poorer prognosis, although only three patients had MYC amplification.11 In general, the limited number of cases with MYC extra copies as well as non-uniform approach taken by the authors in various studies hampers the interpretation of the above findings. The underlying patient characteristics in different patient cohorts may also contribute to the different outcomes. In the current study, we present a large cohort of 663 de novo diffuse large B-cell lymphoma patients in which 76 (12%) had MYC extra copies. Our results show that patients with diffuse large B-cell lymphoma associated with 3–4 copies of MYC showed a similar OS to those with ≥5 copies of MYC, and that MYC extra copies predicts worse OS by both univariate and multivariate analysis.
In this study, patients with double or triple extra copy lymphoma had a worse prognosis than patients with MYC normal diffuse large B-cell lymphoma. In addition, the OS of patients with double or triple extra copy lymphoma was not statistically significantly different from patients with double- or triple-hit lymphoma, an acknowledged poor prognostic group. However, our data suggest that patients with double or triple extra copy lymphoma may have trend toward a better OS than patients with double- or triple-hit lymphoma (P=0.089). Although two studies have compared the prognosis of patients with double extra copy lymphoma and double-hit lymphoma, and found that they had a similarly poor prognosis, one study26 included a few MYC rearrangement cases in the double extra copy lymphoma group, and the other32 included transformed diffuse large B-cell lymphoma as well as high-grade B-cell lymphoma unclassifiable in the double extra copy lymphoma and double-hit lymphoma groups. In contrast, in this study we included only de novo diffuse large B-cell lymphoma and no cases with MYC rearrangement were included in the double or triple extra copy lymphoma group. In the current cohort, patients with double or triple extra copy lymphoma received similar induction chemotherapy regimens as did patients with double- or triple-hit lymphoma. Intensive induction chemotherapy (R-EPOCH or R-Hyper-CVAD) failed to significantly improve the OS of patients with double- or triple-hit lymphoma; however, patients with double or triple extra copy lymphoma did appear to benefit from intensive chemotherapy.
As observed in the current study, the frequency of aggressive clinicopathologic features was lower in patients with MYC extra copies vs patients with MYC rearrangement. The frequencies of MYC expression and MYC/BCL2 coexpression, assessed by immunohistochemistry, were lower in patients in the MYC extra copies group compared with the MYC rearrangement group, similar to a previous study.23 Of note, the number of cases evaluated for MYC and BCL2 expression was limited in both the MYC extra copies and MYC rearrangement groups in this study. Correspondingly, we also appreciated from Figure 2b that normal MYC status has the best OS and MYC rearrangement has the worst OS, while the OS of MYC extra copies is in between. Thus, MYC extra copies appears to have a less profound prognostic impact than MYC rearrangement, although this difference is small and didn’t reach statistical significance (P=0.086). In addition, more patients with MYC extra copies received R-CHOP than those with MYC rearrangement. However, the prognostic relationship of different MYC status was the same for subsets of patients treated with the same induction therapy (Figure 2c and d) as compared to the whole group (Figure 2b).
Similar to the study by Yoon et al, we found that MYC extra copies diffuse large B-cell lymphoma less often had a germinal center B-cell-like immunophenotype than MYC rearrangement diffuse large B-cell lymphoma, more similar to MYC normal (P<0.01). This is of interest because patients with germinal center B-cell-like diffuse large B-cell lymphoma are considered to have a better prognosis than patients with non-germinal center B-cell diffuse large B-cell lymphoma. However, the survival advantage of germinal center B-cell type appears to be totally abrogated in the context of altered MYC gene status. Furthermore, we found no difference in survival between diffuse large B-cell lymphoma of germinal center B-cell vs non-germinal center B-cell type in either the MYC extra copy or MYC-R patient groups. Using different methology, a newly published study by Ennishi et al33 also found worse outcome in germinal center B-cell-like diffuse large B-cell lymphoma in the presence of gains or amplifications of MYC. These data suggest that the prognostic impact of cell-of-origin classification in DBLCL seems to be overshadowed by the genetic and molecular abnormalities.
Although this is a retrospective study with limitations inherent to the approach, to date this study represents the largest and most comprehensive study focused on the significance of the increased MYC copies in diffuse large B-cell lymphoma. MYC extra copy, MYC rearrangement, double- or triple-hit lymphoma, and double or triple extra copy lymphoma were all independent prognostic factors in patients with diffuse large B-cell lymphoma. Intensive chemotherapy improved the OS of patients with double or triple extra copy lymphoma, but only showed a trend toward better OS in patients with double- or triple-hit lymphoma. The results of this study suggest that incorporating MYC extra copies into the standard prognostic systems may be helpful. The implications of these findings also stress the need for novel therapeutic approaches for patients with diffuse large B-cell lymphoma associated with MYC abnormalities.
Single-nucleotide polymorphism, comparative genomic hybridization, high-throughput genomic sequencing, and other molecular techniques could also be used to detect extra copies of genes such as MYC. Each of these techniques has its advantages and drawbacks, which is beyond the scope of this manuscript. However, these techniques are typically more expensive, less readily available, and not commonly used for routine lymphoma diagnostic practice. In addition, some of them may not be suitable to detect rearrangement. FISH remains a sensitive and cost effective tool for detecting targeted gene rearrangements and copy number increases in daily practice.
Our current study showed that by limiting FISH testing to only high MYC expression cases or GCB type, a substantial number of MYC extra copies cases will be missed. Our previous study also demonstrated that using 40% as cutoff for positive MYC expression has a sensitivity of 81% and specificity of 61% to predict MYC rearrangement.23 In other words, if FISH was only performed in those cases with >40% of MYC expression, ~20% of cases with MYC rearrangement may be missed. Therefore we recommend performing MYC FISH in every newly diagnosed large B-cell lymphoma to catch all cases with MYC rearrangement or/and extra copies, which predict a poor prognosis.
OS was also compared among different patient groups according to BCL2 or BCL6 status. On the basis of the results of earlier studies, the reported prognostic significance of BCL2 extra copies is controversial. In one study, BCL2 extra copies did not predict OS,30 whereas in another study BCL2 extra copies did correlate with prognosis.26 In the current study, ~16% of diffuse large B-cell lymphoma cases had BCL2 extra copies, which did not predict OS. No earlier study has evaluated the frequency and prognostic significance of BCL6 extra copies in diffuse large B-cell lymphoma. In this study, BCL6 extra copies was observed in ~13% of patients assessed and was not associated with prognosis.
In summary, we show that ~12% of patients with diffuse large B-cell lymphoma have extra copies of MYC and that about 55% of these patients also have extra copies of BCL2 and/or BCL6, designated here as double or triple extra copy lymphoma. Patients with diffuse large B-cell lymphoma associated with MYC extra copies had a worse OS compared with MYC normal patients (P<0.01). Cell-of-origin classification failed to correlate with survival in patients with MYC extra copies diffuse large B-cell lymphoma. Intensive induction chemotherapy regimens improved the OS of patients with double or triple extra copy lymphoma, but there was no significant improvement in patients with double- or triple-hit lymphoma. Compared with patients with double- or triple-hit lymphoma, patients with double or triple extra copy lymphoma had a higher complete remission rate, but there was no significant statistical difference in OS. Multivariate analysis showed that MYC extra copies in diffuse large B-cell lymphoma is an independent prognostic factor, similar to MYC rearrangement.
References
Dang CV . MYC on the path to cancer. Cell 2012;149:22–35.
Meyer N, Penn LZ . Reflecting on 25 years with MYC. Nat Rev Cancer 2008;8:976–990.
Dalla-Favera R, Bregni M, Erikson J et al. Human c-myc onc gene is located on the region of chromosome 8 that is translocated in Burkitt lymphoma cells. Proc Natl Acad Sci USA 1982;79:7824–7827.
Nesbit CE, Tersak JM, Prochownik EV . MYC oncogenes and human neoplastic disease. Oncogene 1999;18:3004–3016.
Hao S, Sanger W, Onciu M et al. Mantle cell lymphoma with 8q24 chromosomal abnormalities: a report of 5 cases with blastoid features. Mod Pathol 2002;15:1266–1272.
Hu Z, Medeiros LJ, Chen Z et al. Mantle cell lymphoma with MYC rearrangement: a report of 17 Patients. Am J Surg Pathol 2017;41:216–224.
Wang XJ, Jeffrey Medeiros L, Bueso-Ramos CE et al. P53 expression correlates with poorer survival and augments the negative prognostic effect of MYC rearrangement, expression or concurrent MYC/BCL2 expression in diffuse large B-cell lymphoma. Mod Pathol 2017;30:194–203.
Huh YO, Lin KI, Vega F et al. MYC translocation in chronic lymphocytic leukaemia is associated with increased prolymphocytes and a poor prognosis. Br J Haematol 2008;142:36–44.
Aukema SM, Kreuz M, Kohler CW et al. Biological characterization of adult MYC-translocation-positive mature B-cell lymphomas other than molecular Burkitt lymphoma. Haematologica 2014;99:726–735.
Savage KJ, Johnson NA, Ben-Neriah S et al. MYC gene rearrangements are associated with a poor prognosis in diffuse large B-cell lymphoma patients treated with R-CHOP chemotherapy. Blood 2009;114:3533–3537.
Valera A, Lopez-Guillermo A, Cardesa-Salzmann T et al. MYC protein expression and genetic alterations have prognostic impact in patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Haematologica 2013;98:1554–1562.
Li S, Weiss VL, Wang XJ et al. High-grade B-cell lymphoma with MYC rearrangement and without BCL2 and BCL6 rearrangements is associated with high P53 expression and a poor prognosis. Am J Surg Pathol 2016;40:253–261.
Li S, Lin P, Young KH et al. MYC/BCL2 double-hit high-grade B-cell lymphoma. Adv Anat Pathol 2013;20:315–326.
Li S, Saksena A, Desai P et al. Prognostic impact of history of follicular lymphoma, induction regimen and stem cell transplant in patients with MYC/BCL2 double hit lymphoma. Oncotarget 2016;7:38122–38132.
Aukema SM, Siebert R, Schuuring E et al. Double-hit B-cell lymphomas. Blood 2011;117:2319–2331.
Swerdlow SH, Campo E, Pileri SA et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016;127:2375–2390.
Sarkozy C, Traverse-Glehen A, Coiffier B . Double-hit and double-protein-expression lymphomas: aggressive and refractory lymphomas. Lancet Oncol 2015;16:e555–e567.
Johnson NA, Slack GW, Savage KJ et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 2012;30:3452–3459.
Johnson NA, Savage KJ, Ludkovski O et al. Lymphomas with concurrent BCL2 and MYC translocations: the critical factors associated with survival. Blood 2009;114:2273–2279.
Hu S, Xu-Monette ZY, Tzankov A et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood 2013;121:4021–4031; quiz 4250.
Green TM, Nielsen O, de Stricker K et al. High levels of nuclear MYC protein predict the presence of MYC rearrangement in diffuse large B-cell lymphoma. Am J Surg Pathol 2012;36:612–619.
Li S, Lin P, Fayad LE et al. B-cell lymphomas with MYC/8q24 rearrangements and IGH@BCL2/t(14;18)(q32;q21): an aggressive disease with heterogeneous histology, germinal center B-cell immunophenotype and poor outcome. Mod Pathol 2012;25:145–156.
Wang XJ, Medeiros LJ, Lin P et al. MYC cytogenetic status correlates with expression and has prognostic significance in patients with MYC/BCL2 protein double-positive diffuse large B-cell lymphoma. Am J Surg Pathol 2015;39:1250–1258.
Wang XJ, Seegmiller AC, Reddy NM et al. CD30 expression and its correlation with MYC rearrangement in de novo diffuse large B-cell lymphoma. Eur J Haematol 2016;97:39–47.
McGowan JSA, Schmid M, An International System for Human Cytogenetic Nomenclature (2016), 1st edn. Karger: Basel, Switzerland, 2016.
Lu TX, Fan L, Wang L et al. MYC or BCL2 copy number aberration is a strong predictor of outcome in patients with diffuse large B-cell lymphoma. Oncotarget 2015;6:18374–18388.
Mossafa H, Damotte D, Jenabian A et al. Non-Hodgkin’s lymphomas with Burkitt-like cells are associated with c-Myc amplification and poor prognosis. Leuk Lymphoma 2006;47:1885–1893.
Stasik CJ, Nitta H, Zhang W et al. Increased MYC gene copy number correlates with increased mRNA levels in diffuse large B-cell lymphoma. Haematologica 2010;95:597–603.
Testoni M, Kwee I, Greiner TC et al. Gains of MYC locus and outcome in patients with diffuse large B-cell lymphoma treated with R-CHOP. Br J Haematol 2011;155:274–277.
Yoon SO, Jeon YK, Paik JH et al. MYC translocation and an increased copy number predict poor prognosis in adult diffuse large B-cell lymphoma (DLBCL), especially in germinal centre-like B cell (GCB) type. Histopathology 2008;53:205–217.
Landsburg DJ, Falkiewicz MK, Petrich AM et al. Sole rearrangement but not amplification of MYC is associated with a poor prognosis in patients with diffuse large B cell lymphoma and B cell lymphoma unclassifiable. Br J Haematol 2016;175:631–640.
Li S, Seegmiller AC, Lin P et al. B-cell lymphomas with concurrent MYC and BCL2 abnormalities other than translocations behave similarly to MYC/BCL2 double-hit lymphomas. Mod Pathol 2015;28:208–217.
Ennishi D, Mottok A, Ben-Neriah S et al. Genetic profiling of MYC and BCL2 in diffuse large B-cell lymphoma determines cell of origin-specific clinicalimpact. Blood 2017;129:2760–2770.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Quesada, A., Medeiros, L., Desai, P. et al. Increased MYC copy number is an independent prognostic factor in patients with diffuse large B-cell lymphoma. Mod Pathol 30, 1688–1697 (2017). https://doi.org/10.1038/modpathol.2017.93
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2017.93
This article is cited by
-
High-grade B-cell lymphoma (HGBL)-NOS is clinicopathologically and genetically more similar to DLBCL/HGBL-DH than DLBCL
Leukemia (2023)
-
High performance of multiplex fluorescence in situ hybridization to simultaneous detection of BCL2 and BCL6 rearrangements: useful application in the characterization of DLBCLs
Virchows Archiv (2021)
-
Evolving insights into the genomic complexity and immune landscape of diffuse large B-cell lymphoma: opportunities for novel biomarkers
Modern Pathology (2020)
-
Somatic copy number gains in MYC, BCL2, and BCL6 identifies a subset of aggressive alternative-DH/TH DLBCL patients
Blood Cancer Journal (2020)
-
Patients with double/triple copy number gains on C-MYC, BCL2, and/or BCL6 treated with standard chemotherapy have a similarly poor prognosis than those with high-grade B cell lymphoma with C-MYC and BCL2 and/or BCL6 rearrangements: a single-center experience on a consecutive cohort of large B cell lymphomas
Annals of Hematology (2020)